CLIN PATH I: EXAM #2 (PULM - Obstructive Lung Dz)
1/158
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
159 Terms
What are the main physiologic roles of the lungs?
1. make o2 available to tissues
2. remove CO2 (metabolic byproduct)
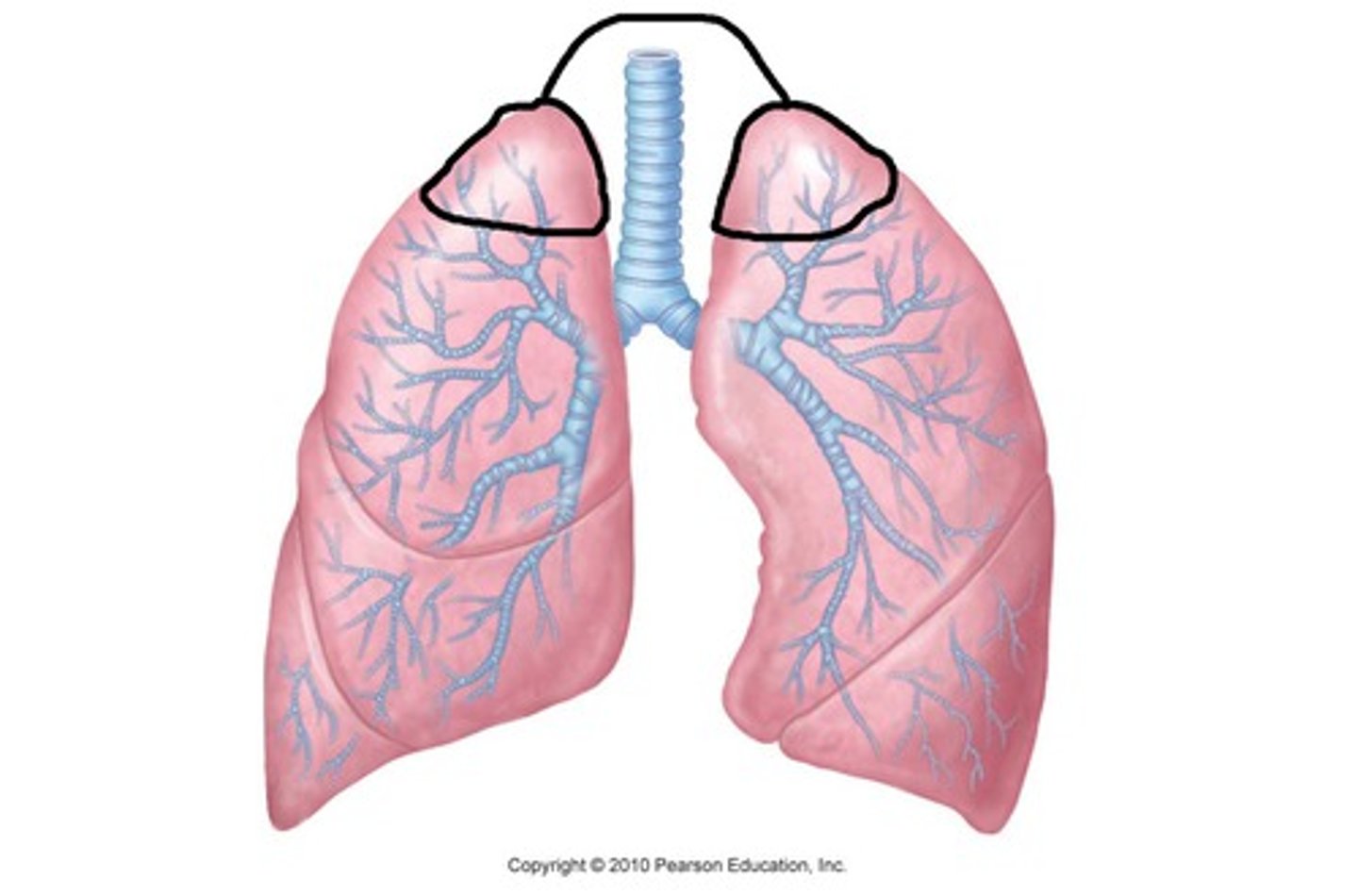
Each lobe is demarcated by:
visceral pleura
Difference between pleural effusion and pulmonary edema:
pleural effusion - pleura
pulmonary edema - alveoli
Inspiration is _____ and expiration is ________
active; passive (due to recoil - except w/ exercise)
What maintains the anatomic integrity of the lungs?
connective tissue (collagen/elastic structures - supports and maintains patency)
surfactant (reduces surface tension allowing for expansion)
Proximal conducting airways are:
ciliated pseudostratified columnar epithelial (cilia beat in unison to transport FB out)
As airways further branch, smooth muscle and secretory glands are:
reduced
Smallest conducting, non respiratory airways are:
bronchioles (cuboidal epithelium - may or may not be ciliated)
What causes asthma?
bronchial smooth muscle constriction (closes up airways)
Where do lymphatic vessels arise from?
beneath visceral pleural and in deep plexuses at junction of terminal bronchioles and alveoli
Where should the alveolar fluid move to gain access to draining lymphatics?
terminal bronchioles
Where do the lymphatic ducts travel?
peribroncovascular sheath to hilar and mediastinal lymph nodes (before going to the left or right thoracic ducts)
There is no _______ in lymph
protein
Lymphatic drainage of the pleural space occurs through plexuses that are:
anatomically separate from pulmonary lymphatics
What do efferent parasympathetic (muscarinic cholinergic) fibers of the lungs cause?
bronchoconstriction
pulmonary vasodilation
mucous gland secretion
What do efferent sympathetic fibers of the lungs cause?
bronchial relaxation
pulmonary vasoconstriction
inhibition of secretory glands
What should you stimulate during asthmatic rxns?
sympathetic nerve fibers
What does the efferent non-adrenergic non-cholinergic system do in the lungs?
inhibition of events (including bronchodilation)
**ATP, NO, peptide NT
Afferent pulmonary nerve functions:
1. bronchopulmonary stretch receptors
2. irritant receptors
3. C fibers/juxtacapillary receptors
1. bronchopulmonary stretch receptors (lung inflation, bronchodilation, inc HR)
2. irritant receptors (cough, mucus secretion, bronchoconstriction)
3. C fibers/juxtacapillary receptors (response to chemical/mechanical stimuli causing a rapid shallow breath pattern, mucus secretion, cough, and decreased HR w/ inspiration)
Pulmonary arteriole system runs adjacent to:
bronchial tree
Pulmonary venous system found distant from:
airways
Lymphatics found adjacent to both:
arteriole and venous systems
**remove fluid (especially near alveoli sac where pulmonary edema will occur)
**do not penetrate alveolar wall
The ability of the lungs to relate changes in volume to changes in pressure
compliance
Which dz has a problem with recoil?
Emphysema
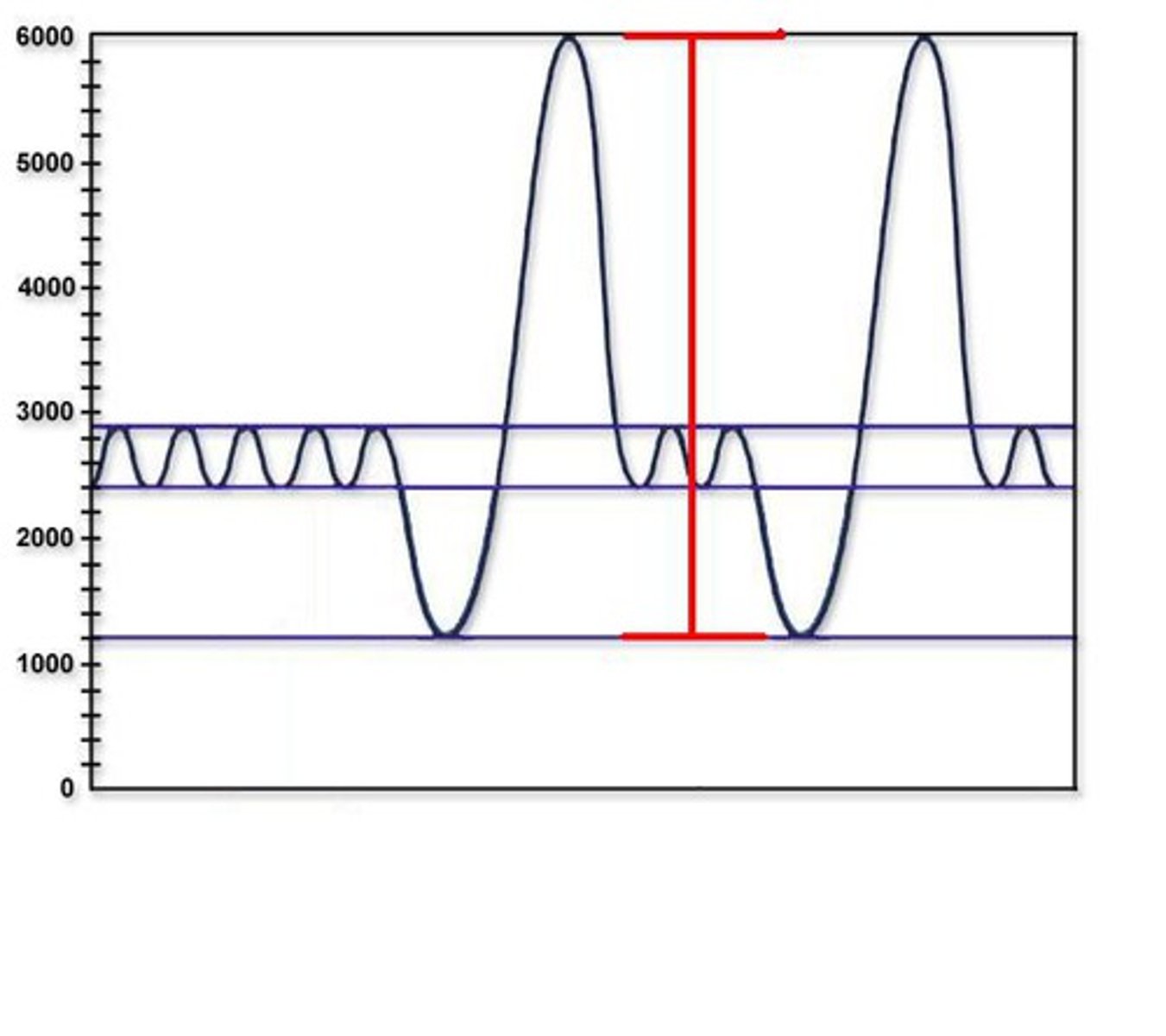
What do pulmonary function tests do?
identify abnormalities in respiratory function and determine the extent of those abnormalities
Types of pulmonary function tests:
spirometry
air flow rates
calculation of lung volumes/capacities
Spirometry is ____ and measures ______.
Indirect; Air
**Used to re-inflate the lungs (especially after surgery)
Tidal volume
inhaled and exhaled air each normal breath
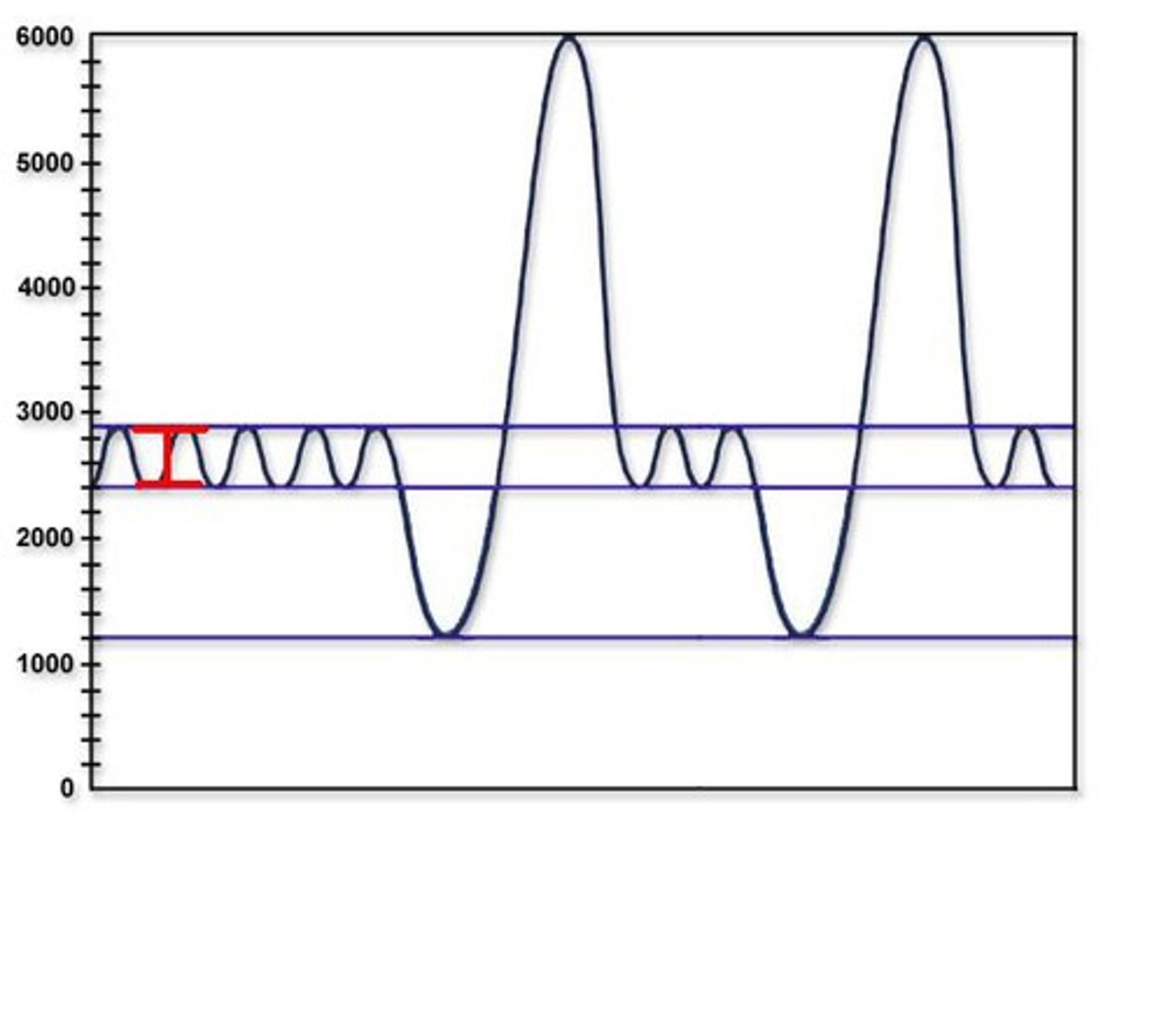
inspiratory reserve volume
the maximum amount of air inhaled above a normal TV
expiratory reserve volume
the maximum amount of air exhaled below a normal TV
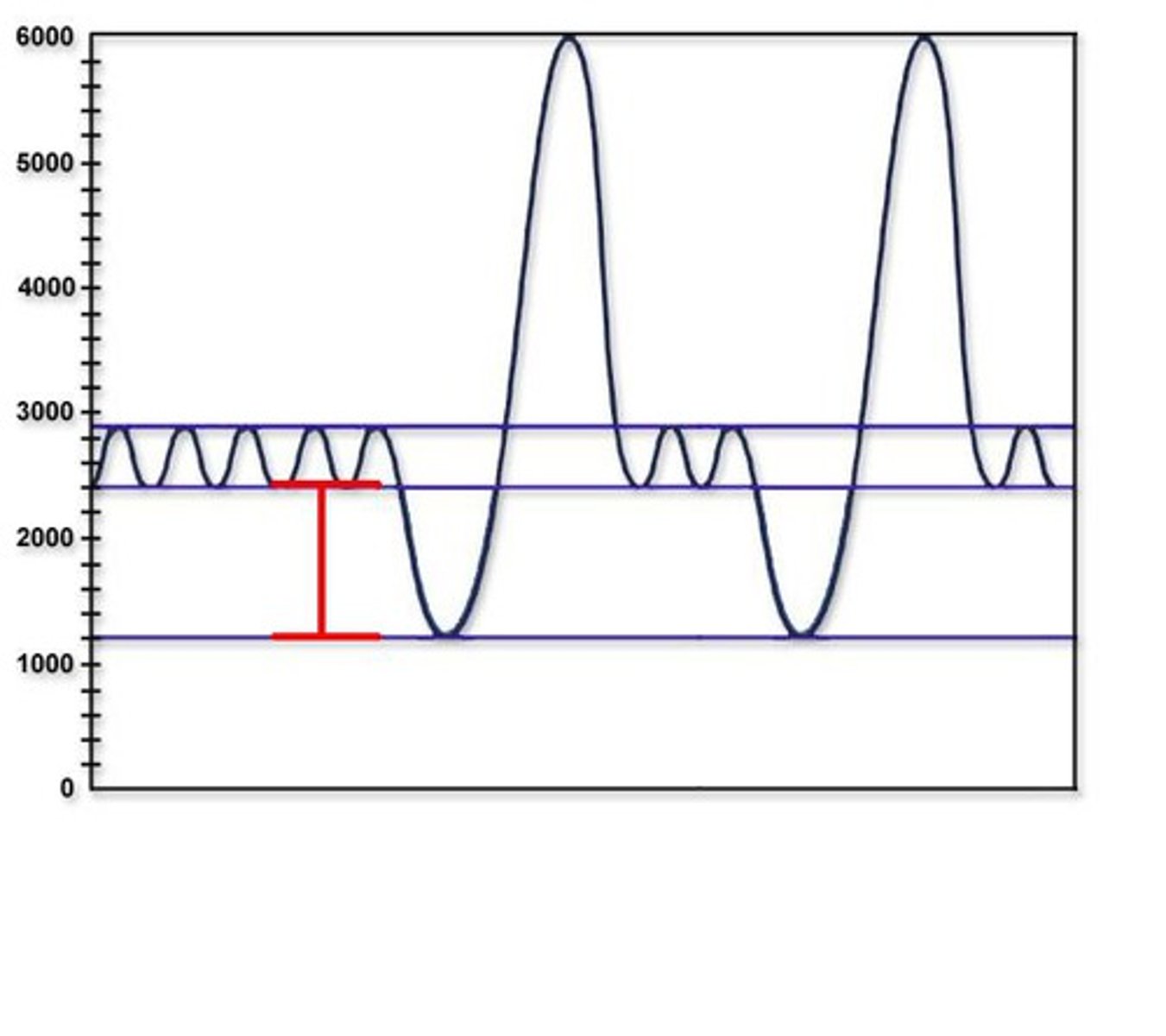
residual volume
amount of air left in lungs after maximum exhalation
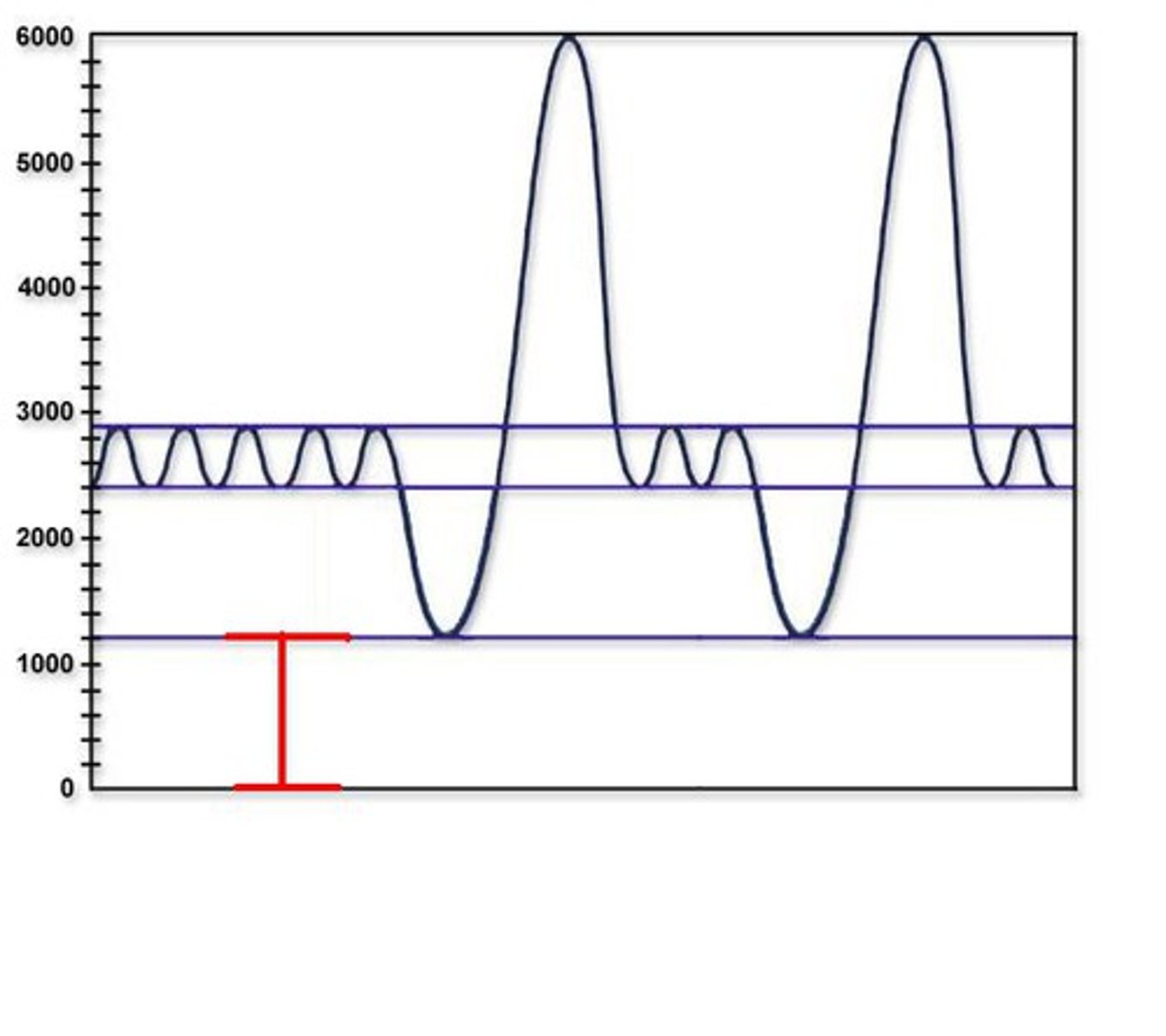
Vital capacity
IRV + TV + ERV
Total lung capacity
VC (IRV + TV + ERV) + RV
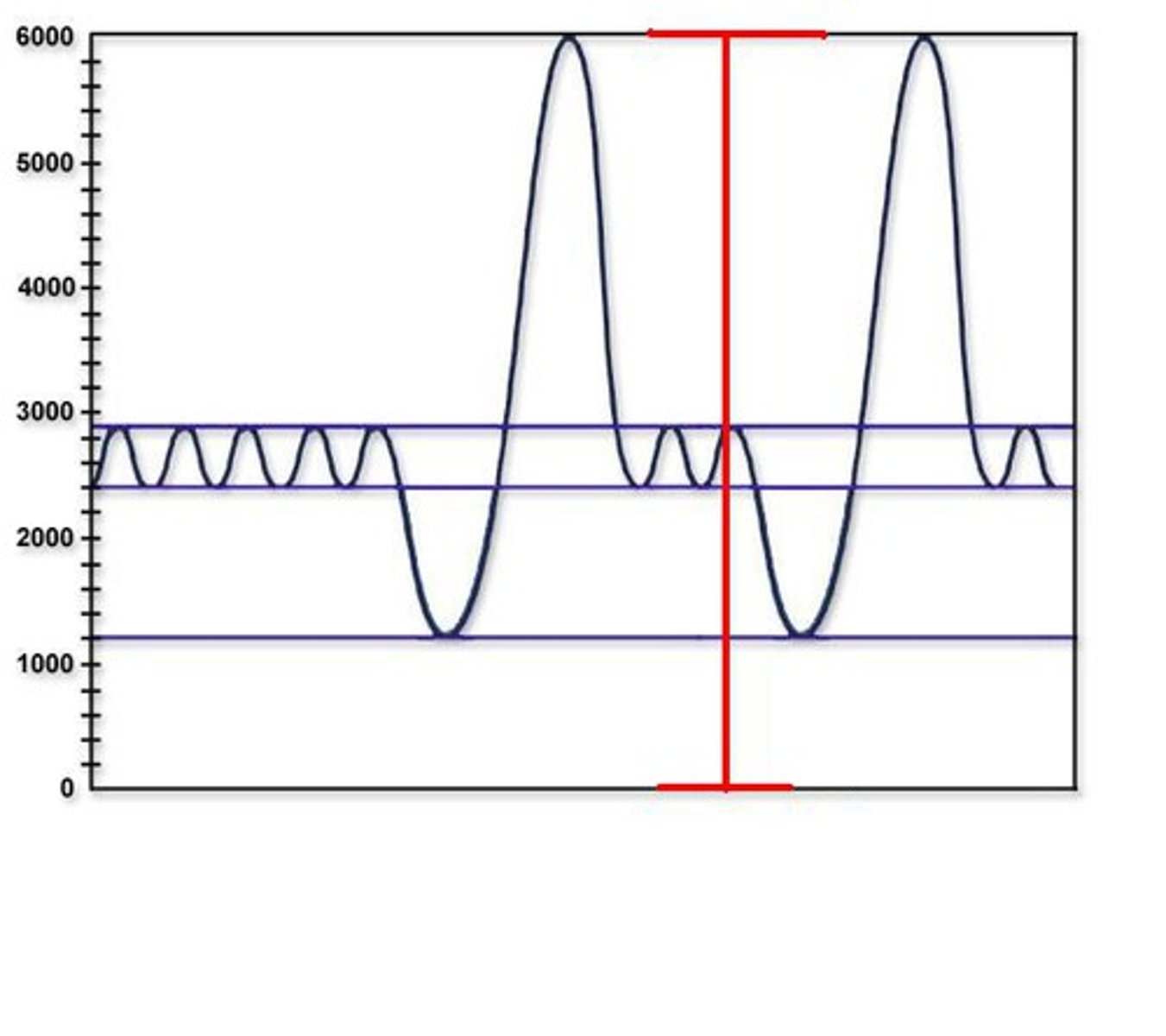
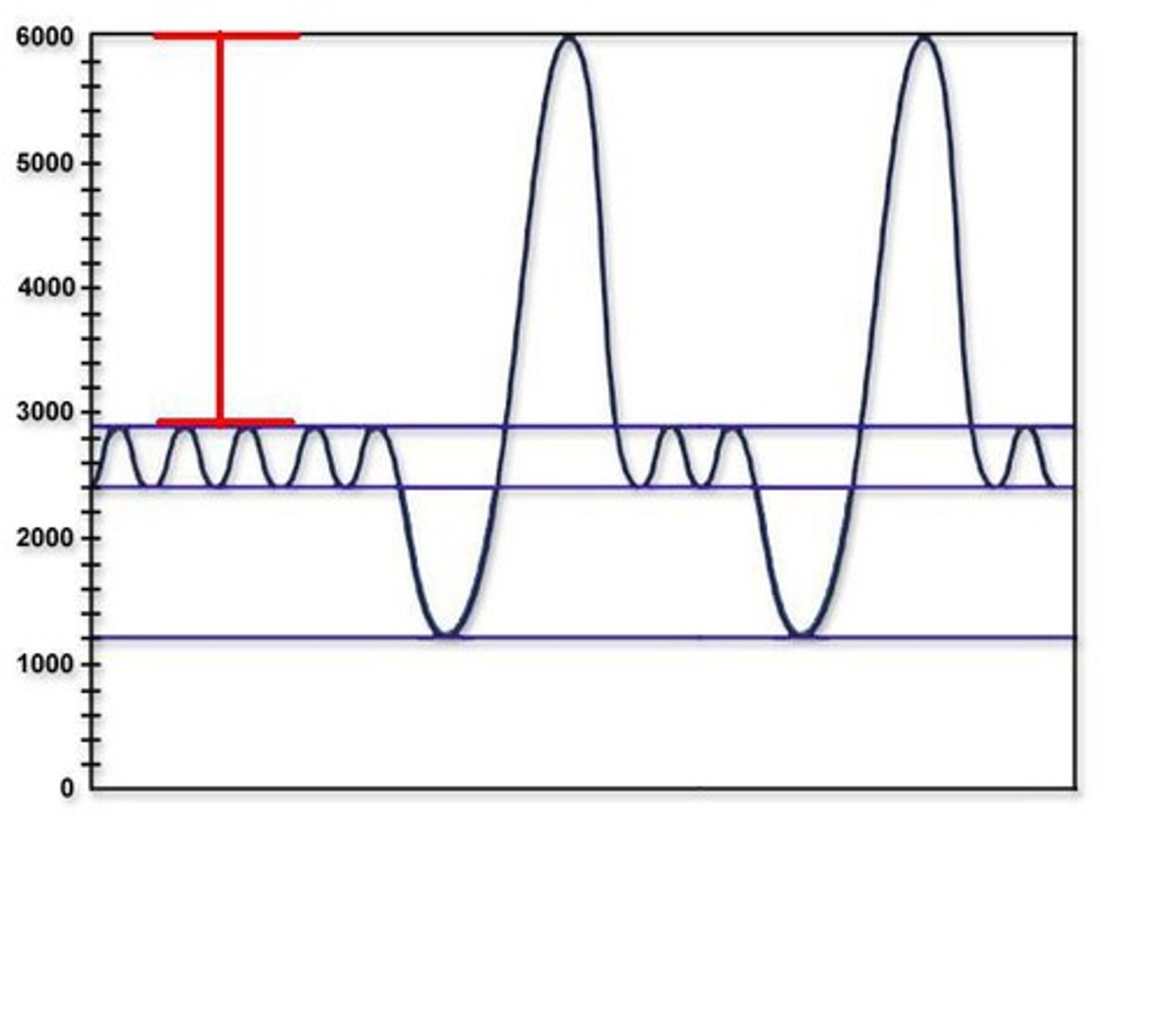
Force vital capacity
begins with an inhalation from FRC (functional residual capacity) to TLC (total lung capacity) followed by a forceful exhalation from TLC to FV
Forced expiratory volume in 1 second (FEV1)
amount of gas exhaled during the first second of the FCV maneuver
Normal FEV1/FCV ratio
80%
Diminished FEV1/FCV ratio in patients with:
obstructive lung disease
**cannot get air out as quickly (but normal lung volume); low FEV1 but normal FVC
Increased or normal FEV1/FCV ratio in patients with:
restrictive lung disease
**high FEV1 but low FVC (volume is restricted, but flow is more because recoil is faster)
Major categories of pulmonary defense:
1. nonspecific (clearance, secretions, cell or biochemical defenses)
2. chemical (antibody mediated, antigen presentation, cell mediated)
Oxygen in blood is either ________ or ________
bound to hemoglobin
dissolved in plasma
Oxygen content in the blood depends on:
1. arterial PO2 (pressure of air we breath in)
2. hemoglobin level
Tissue oxygen delivery depends on:
1. oxygen content in the blood (O2 saturation)
2. CO
What determines blood O2 saturation
how much o2 is in environment?
how much are we breathing?
is our airway open?
Determinants of CO
SV and HR
Determinants of stroke volume
preload, afterload, contractility
CO2 is carried in the blood as:
HCO3- (dissolved in plasma)
carbaminohemoglobin
CO2 is _____ soluble than O2
more
In pts with lung disease, energy requirements are _________ at rest
greater
**and increases dramatically w/ exercise
Two components of breathing
1. elasticity (recoil to get air out)
2. resistance (obstruction)
Which lung segments have the greatest perfusion?
gravity-dependent segments (ex. Zone III)
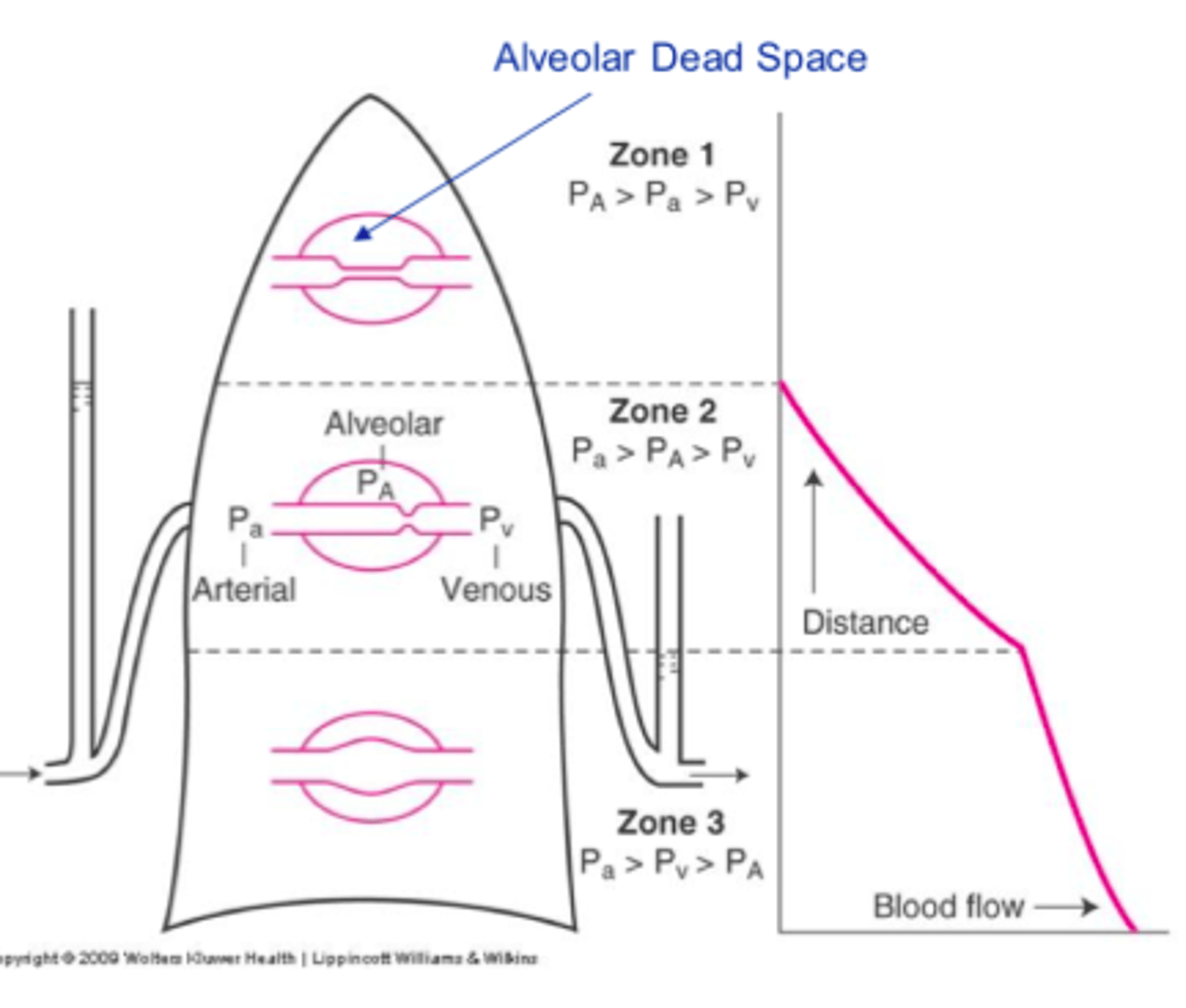
Exercise allows for more:
perfusion of the lungs (to allow for more oxygenation of blood)
The ratio of ventilation to perfusion is highest at the:
apex
What is the reason for most abnormalities in O2 and CO2 exchange?
V/Q mismatch
Normal V/Q ration
0.8
When the V/Q ratio is high, it means:
ventilation > perfusion (ex. PE, cardiac arrest)
**dead space ventilation
When the V/Q ratio is low, it means:
ventilation < perfusion (ex. CF, asthma, effusion)
**shunt perfusion
When can you not give contrast (V/Q scan > CT)?
renal failure, pregnancy, allergy
Tests for pulmonary emboli are done with:
nucelar medicine
Which muscles manage breathing?
diaphragm, abdominal muscles, and intercostal muscles
Breathing originates in:
brainstem (medulla)
Major driving force of breathing
CO2 levels
What causes spontaneous breathing
output signals of the phrenic nerve (diaphragm) and spinal nerves (intercostals/abdominal muscles)
Sensory input for breathing is through:
carotid bodies and aortic bodies (arterial oxygenation)
**increases ventilation w/ hypoxia
Integrated responses of breathing:
arterial pH changes affect PaCO²
Global Initiative for Chronic Obstructive Lung Disease (GOLD)
improve prevention and treatment of COPD worldwide
airflow limitation of COPD is usually ___________ and associated with _________________ to noxious particles or gases
progressive; an abnormal inflammatory response of the lungs
Gold 1: Mild
FEV1 > 80% predicted
FEV1/FVC < 0.7
Gold 2: Moderate
FEV1 is between 50-80%
FEV1/FVC < 0.7
Gold 3: Severe
FEV1 is between 30-50%
FEV1/FVC < 0.7
Gold 4: Very Severe
FEV1 < 30% predicted
FEV1/FVC < 0.7
Fundamental issue of obstructive lung disease:
resistance to airflow
What causes increased resistance to airflow
1. decreased lumen size (obstructive secretions - asthma/chronic bronchitis)
2. airway wall thickening/narrowing from inflammation or constriction (asthma/chronic bronchitis)
3. structures supporting airway (ex. elastic tissue destroyed in emphysema)
What is the difference between asthma and emphysema/chronic bronchitis?
asthma is reversible and emphysema/chronic bronchitis are not
Asthma can be caused by:
environmental factors or genetics
Asthma is a disease of airway ____________ and airflow _____________. Symptoms are ___________.
inflammation; obstruction
intermittent
Symptoms of asthma
wheezing, SOB, chest tightness, cough
Symptoms of asthma indicate:
bronchial hyper-responsiveness
What will release of mediators do?
alter airway smooth muscle tone/responsiveness
cause mucus hyper-secretion
damage airway epithelium
What is the most common chronic pulmonary disease?
asthma
Epidemiology of asthma
more common in men, African Americans, inner-city dwellers, and premature babies
Why are premature babies more at risk for asthma?
lungs are the last to develop
Intrinsic vs. Extrinsic asthma
Intrinsic asthma is NOT related to allergies, has later age of onset, and is often more severe
Extrinsic is related to allergy and IgE mediated, appears mostly in childhood, and is often mild
Physiologic or pharmacologic mediators that trigger asthm
Histamine, Methacholine, Adenosine triphosphate
Exogenous physiochemical agents that produce airway hyperactivity
exercise, pollutants, viral respiratory infections, propranolol, ASA/NSAIDs, cold air
Why you do not want to give beta blockers to asthmatics?
affects B2 (lungs) and causes bronchoconstriction
Asthma is often associated with what?
atopy (Type I)
Atopy
A hypersensitivity or allergic state (production of IgE antibodies in response to an allergy)
Status asthmaticus
a severe, life-threatening asthma attack that is refractory to usual treatment
**complete airway lumen obstruction
Common manifestations of atopy
allergic rhinitis
allergic asthma
atopic dermatitis (eczema)
What begins an asthma exacerbation?
Activation of local inflammatory cells, principally mast cells and eosinophils
What do the mediators cause?
smooth muscle contraction
mucus hypersecretion
vasodilation (with endothelial leakage and edema)
During an asthma exacerbation, some of the preformed & rapidly acting mediators recruit additional:
inflammatory cells (eosinophils and neutrophils)
What aids in perpetuating local airway inflammation and hyper-responsiveness?
cytokines and chemokines
What do mast cells do?
secrete histamine
Function of B cells in asthma pathogenesis
differentiate into IgE and IgA producing plasma cells
What drives tissue remodeling & submucosal airway fibrosis?
Production of growth factors and fibroblasts
**can cause fixed airway obstructino
Elements of a normal bronchus
thin layer of mucus on top
normal epithelial basement membrane
small smooth muscle layer
Elements of a asthmatic bronchus
thick mucus
epithelial basement
membrane makes goblet cells (makes more mucus) and have increased macrophages
increase size of smooth muscle layer
IgEs, mast cells, lymphocytes, neutrophils, and eosinophils are within the bronchus
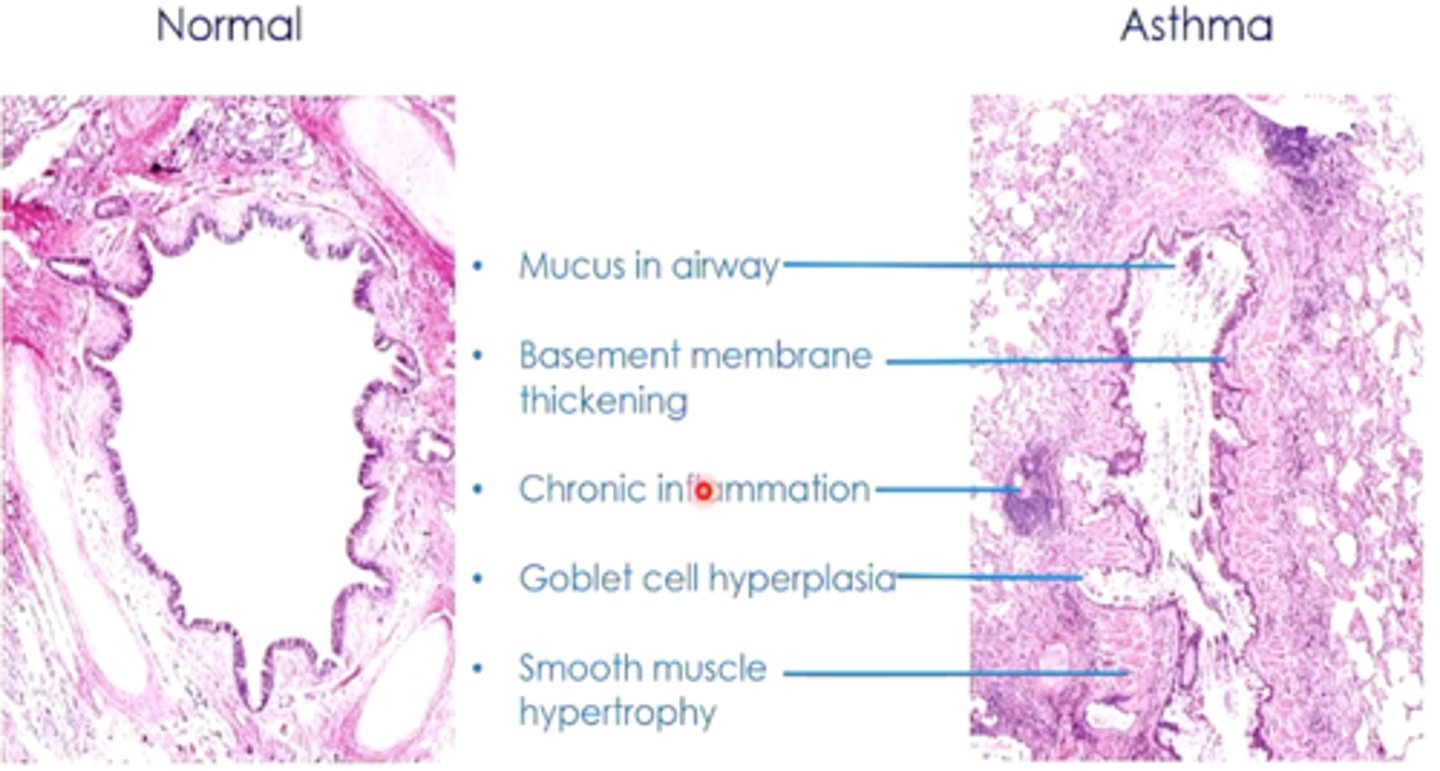
What causes increased airflow resistance in asthmatic patients?
airway inflammation, smooth muscle hypersensitivity, and narrowing of airways
Which elements exacerbate airway obstruction?
mucus hypersecretion and bronchoconstrictor stimuli