meat hygiene labs | Quizlet
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
characteristics enterobacteria
gram neg
rods
faculatitive anaerobic
catalase pos
oxidase neg
grows well at 37 degress, some better at 25-30
some motile
worlwide- soil, water, plants, animals
name the bacteria included in enter-bacteria
E. coli
salmonella
Yesenia
shigella
pneumoniae
what's special about the salmonella bacteria
most are motile except s. typhi
most produce hydrogen sulphide
except s.paratyphi
and s. typo produces less than normal
what special about E. coli
capsulated with a k ag
many produce enterotoxin or have other virulence t
factor that increase their invasiveness
what's special about klebsiella
grow on ordinary agar
non-motile
capsulated
what special about shigella
non motile
highly infected
species of shigella
s. dystenteria
s. flexneri
s. boydii
s. sonnei
steps of testing for salmonella
inoculate on mediums XLD and BGA
XLD
can ferment xylose = decre pH => yellow
metabolise thiosulfate to H2S => black colonies
BGA
white —>red
opaque colonies surrounded by red
selective for salmonella except typhi
test serology
what does XLD mean
xylose lysine deoxycholate agar
what is XLD used for
selective media for salmonella and shigella
has pH 7.4
contains phenol red so agar is red
how to read results of XLD
if there is sugar fermentation the pH drops
turns agar red to yellow
uses xylose which shigella can't use
yellow= salmonella
what does the salmonella colonies on the XLD agar look like
there are round black colonies because salmonella turns thiosulfate to hydrogen sulphide
what grows on BGA and what inhibited
gram positive INHIBITED
most gram negative bacilli INHIBITED
gram negative rods GROW
what does BGA tell about the colonies that grow
contains phenol red
turns yellow from red when sugar is fermented
lactose non-fermenting is are pink
what does salmonella look like on BGA
white/red colonies w red zone around
what does E. coli and klebsilla look like on BGA
yellow and green w green zone around
what does pseudomonas look like on BGA
red and pink
how to do serology confirmation on salmonella
slide w colony of bacteria and appropriate sera and rock
clumping is a pos reaction
what ag does the agglutination test for
o
h
vi
characteristics of pseudomonas of aerginosa
gram negative aerobic rods
most are motile
free living in water and soil
opportunistic pathogens
optiumum 37-42
produce pigments
what are the 2 pigment of pseudomonas aerginosa
pyoverdin: fluorescent
pyocyanin: blue = blue pus
what agars to use for pyorubin and pyocyanin
king A medium
what agar to use for pyoverdin
king B agar
what happens to p. aerginosa on blood agar
turns red to marine blue
small like jasmine poets
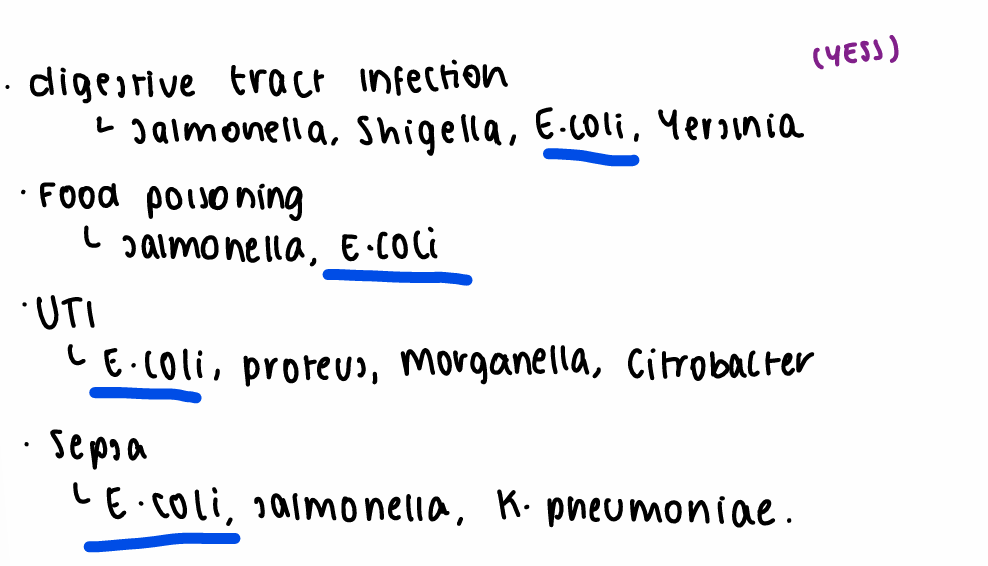
zoonotic infection of p. aerginosa
enteric infection
food poisoning
UTI
resp infcetions
dermatitis and soft tissue infection
affects bones and joints
characteristics of burkholderia
gram - rods
aerobic
non motile
characteristics of b. mullei
gram neg aerobic
coccibacillus
grow on macconkey
non motile
characteristics of b. mpseudomallei
infects humans and plants
causes meliodosis
characteristics of bacillaceae
gram positive bacilli
motile/non-motile
aerobic/non-aerobic
produce ENDOSPORES
colonies of b subtilus
rough creamy white elevated and entire edges
what is caused by B. cereus
food Bourne illnesses
zoonotic problems caused by baccilaceae
cause GIT issues
diarrhea or emetic
the bacteria produce toxins which irritate the mucosa
characterise clostridium
gram positive rods
in pairs or chains
pointed, round, square end
often pleomorphic
aerolotolerant or obligate anaerobes
characterise c. perfringens
aerobic
spore forming
5 types a-e
produce lethal toxin
characterise c. botulism
obligate anaerobic
spore forming
produce neurotoxin- a,b,e
subtypes a-g
incubate of c .perfringens
6-24hrs
how does c. perfringens last in cooked food and symptoms and how long do last
spores are heat stable
symptoms: cramps, diarrhea, vomiting and fever
gone in 24hrs
fatal cases on clostridial necrotising enteritis caused by
types c producing beta toxin
c. sporogens cause what
food spoilage through putrefaction
what is botulism
flaccid paralysis of ANS and motor beginning with the cranial nerves which occurs when the neuromuscular transmission is interrupted by a protein botulism neurotoxin
movement pattern of botulism
cranial nerves
resp muscles
lower extremities
symptoms of botulism
nausea, vomiting, cramps and diarrhoea
neurological symptoms
dry mouth and blurred vision
peripheral muscle weakness, dysphagia and dysarthia
how is the beta toxin stable
pH 3.5-6.5
dissociates at alkaline conditions
spores are heat stable
how to kill botulism spores
30mins @80
10mins @ 100
what is the 12-D process
heating botulism spores to 121.1. for 2.8 mins
detection of aerobic spore forming
heat serial dilution at 80 for 10mins
inoculate .5ml on 2 plates
incubate
gram stain
examine
Schaeffer fultor method
examination of spores
fix to the slide
malachite green het 3 times
wash
add safranin for 30 secs
observe
endospores are bright green
detection of botulism toxins
detected on mice and gineua pigs
present give antitoxin
detection of anaerobic spore forming
inoculate 2 Wrzosek broth w 1g meat
heat 80 for 10mins
inoculate both and gram stain
up until now same as aerobic
postive for gram + rods
put 1 drop from 1 broth to WILSON BLAIRE
heat @ 45
mix leave and add water
will be black colonies = + for anaerobic spores
characteristics of staphylococcus
gram + cocci
catalase +
oxidase negative
types of staphylococcus
s. aureus
s. epidermis
s. saprophyticus
characteristics of s. aureus
potential pathogen
produces coagulase
yellow and large colonies
hemolytica
what are the properties of a pathogenic strain of staphylococcus
beta hemolysis
liquefaction of coagulataive serum
increase fibrinolysis
hematoxin
dermatoxin
lathaltoxin
zoonotic of staphylococcus
important cause of food Borne illnesses as it produces enterotoxin
human carrier
food product and animal origin
characteristic of s. epidermidis
can't produce coagulase
white small colonies
non-hemolyitca
charcterise streptococcus
gram + in chains and pairs
types of hemolysis
types of hemolysis of streptococcus
alpha hemolysis: oxidation of iron in the haemoglobin green
bete hemolysis: complete rupture of RBCs clear
gamma hemolysis: no hemolysis
characterise s. pyrogens
gram +
non motile
non spore forming
catalase +
facultative anaerobes
how to identify staphylococcus
liquid medium: Giolitti- cantoni used to enrich stay aureus
causes blackening of the medium is +
then subculture to Baird Parker
characteristics of enterococcus
facultative anaerobes
tolerant to extreme temp, pH and chloride conc.
characterise nocardia
gram + rods
smooth moist colonies that have a powdery appearance and have a mildew odour
causes progressive pneumonia
what are under the fungi bracket
moulds
yeast
higher fungi- saprophytes
characterise fungi
chemoterotrophs
aerobic
contain chitin in the wall
produce mycotoxins
most important mycotoxins
aflatoxin
ochratoxins A
fumonisms
trichthecenes
zearalenones
types of diseases caused by fungi
superficial
subcutaneous
systemic
oppourtunistics
agars to detect fungi
sabouruda
synthetic
czapeks medium
2 forms of catalase
enzyme bound: clumping factor
free enzyme: converts prothrombin causing fibrinogen to fibrin-clot
where will bacteria be present and least likely
organs w no contact to the exterior may be regarded as sterile
a slaughter if bacteria/septicemia present bacteria are likely to be found in the spleen, lymph node and muscular tissue
intestinal bacteria could migrate to systemic migration when the barrier is down
examination of animals and meat for slaughter and food
ante-mortem
gross post-mortem
lab tests
when will bacteriology lab not be required
when they exhibit marked pathological changes but not required when they show pathological changes of non-infectious nature= condemned without bacteriology
when will bacteriology be necessary
slaughtered in emergency
excreting food poisoning organisms
slaughtered without antemortem
haven't been eviserated within 1hr of slaughter
slaughtered due to systemic disturbances
pathological changes in the the post mortem
list of material submitted for examination
2 complete muscles w faces
(1 from hinquarter/ 1 from forequarter and then cubes 8cm from opposite each side)
prescapilular/auxiallry lymph nodes or iliac node
spleen if ENLARGED
kidney
SM:whole liver and gallbladder
LM:2 fists of liver, portal veins, gallbladder and lymph nodes
parts of pathological changes and LN
portion of small intestine w mesenteric lymph nodes
what happens with received samples in the lab
examined immediately
put on sterile plate
visible changes noted
burn surface
cut with sterile knife and inoculate
solid mediums used for bacteriology
nutritive agar
baird parker agar
brilliant green agar
blood Agar
liquid mediums used for bacteriology
MRSV
wrzoseks broth