Clin Path LN units 3-4
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Where does normal white blood cell (WBC) production occur?
All normal white blood cell production occurs in the bone marrow.
What are the two main functional groups of white blood cells?
Granulocytes – contain granules, capable of phagocytosis
Lymphocytes – lack granules, involved in immune response
What are the two major subgroups of myelopoiesis?
Granulopoiesis – production of granulocytes
Lymphopoiesis – production of lymphocytes
What does granulopoiesis produce?
WBCS- neutrophils, basophils, eosinophils, and monocytes.
Do monocytes follow the same maturation path as granulocytes?
No — monocytes come from the same committed cell pool but have a different maturation sequence.
How is specific granulocyte production regulated?
If a specific granulocyte is needed, leukopoietins direct bone marrow to produce that specific type (e.g., neutrophils, eosinophils, etc.).
What triggers the granulocyte maturation sequence?
A signal indicating which WBC production pathway is required triggers granulocyte maturation, leading to:
a) Increased cell division
b) Cellular differentiation
c) Enhanced cell function
When would a metamyelocyte appear in circulation?
Normally confined to the bone marrow
may appear in blood during severe acute infection or inflammation, when the bone marrow cannot keep up with neutrophil demand.
What is a metamylocyte?
MOVES FROM PROLIFERATING POOL TO MATURATION POOL- intermediate stage in the granulocyte maturation process, typically confined to the bone marrow but can enter circulation during severe acute infections or inflammation when the bone marrow's production capacity is overwhelmed.
What is a band cell?
A band cell is an immature neutrophil with a U-shaped or deeply indented nucleus, seen when the marrow releases early cells to meet demand.
Are band cells normally found in circulation?
Yes, but only in small numbers (1–2%). Increased numbers indicate infection or inflammation and are a sign the bone marrow is working to meet neutrophil demand.
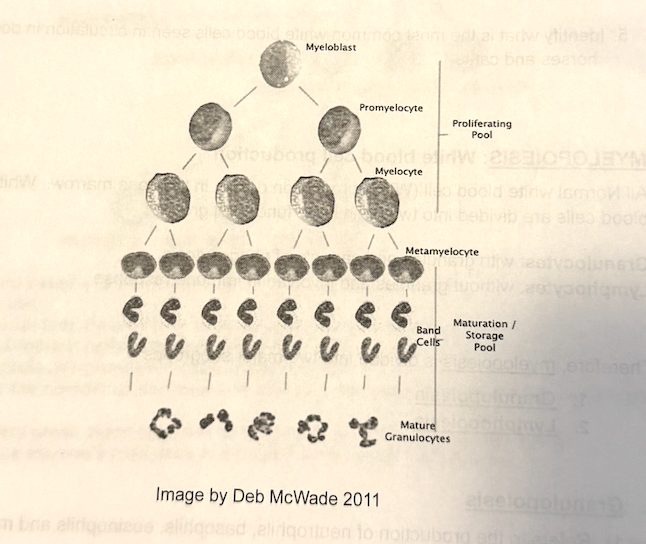
What are the two main bone marrow pools involved in WBC production?
Proliferating pool – contains dividing granulocytic cells.
Maturation (storage) pool – contains non-dividing cells that continue to mature and wait for release into circulation.
Marginated pool
granulocytes rolling along vessel walls, ready to move into tissues when needed.
Circulating pool
granulocytes freely moving in the bloodstream.
What are the five main types of white blood cells (WBCs)?
Neutrophils
Eosinophils
Basophils
Monocytes
Lymphocytes
What is the main function of neutrophils?
First line of phagocytic defense — they engulf and destroy pathogens in the tissues (not in circulation).
What is emigration
movement of neutrophils between endothelial cells of blood vessels into tissues, guided by chemical signals from infection or inflammation.
What is chemotaxis?
Chemical attraction of neutrophils to the site of inflammation or infection, where they aggregate in response to signals from damaged tissue, pathogens, and other immune cells.
Where does neutrophil phagocytosis occur — in blood or tissues?
In the tissues, not in the blood
What is the main function of eosinophils?
first line of defense in the gastrointestinal tract against parasite invasion.They also play a role in allergic reactions and asthma.
Where are basophils found, and what is their possible function?
Basophils are found near the respiratory system and may play a role in respiratory inflammation, though their exact function is not well understood.
How common are basophils in the blood?
Very rare, normally seen in very small numbers in peripheral blood.
Where do monocytes originate, and are they mature when released?
Monocytes come from the same stem cell line as granulocytes.
They are not fully mature when they leave the bone marrow and mature after entering tissues.
What do monocytes become once in tissues, and what is their role?
Monocytes transform into macrophages, which are highly efficient phagocytes that ingest bacteria, dead cells, and debris to protect the body.
What are the three main functions of macrophages?
Phagocytize dead cells, debris, and pathogens.
Process and present antigens to lymphocytes to start a specific immune response.
Release inflammatory mediators that stimulate production of new leukocytes (part of leukopoietin activity).
What is lymphopoiesis?
The production and maturation of lymphocytes, which occurs in the bone marrow.
What is the main role of lymphocytes?
Essential for acquired (adaptive) immunity and the body’s immune response to antigens.
What triggers lymphocyte production in the bone marrow?
A signal from leukopoietin stimulates the bone marrow to begin lymphocyte production.
What cellular changes occur during lymphocyte maturation?
Increased cellular proliferation (more cells divide)
Increased cellular differentiation (cells specialize)
Enhanced cell function (improved immune capability)
Which white blood cell is most common in circulation?
In most animals, the neutrophil is most common; however, in cattle, the lymphocyte is the most common WBC in circulation.
What can increased lymphocyte numbers indicate?
Chronic antigen stimulation from long-term infection (virus, bacteria, etc.)
Response to vaccination or antigen exposure in young animals
How are lymphocytes identified on a blood smear?
They are round cells with a large, round nucleus and vary in size (small, medium, or large).
What happens to neutrophils during acute inflammation?
Bone marrow releases large numbers from the storage pool.
Causes neutrophilia with a left shift (bands ± metamyelocytes).
Represents an appropriate, early response to tissue injury or infection.
How does the neutrophil response differ in chronic inflammation?
Marrow maintains sustained production.
Monocytosis develops as macrophages join.
If demand exceeds supply → degenerative left shift (immature cells > mature).
How do dogs and cats differ from horses and cattle in their neutrophil response?
Large marrow storage pool → easily mount marked neutrophilia and moderate left shift.
Small pool → often show leukopenia with mild left shift (normal early response).
What does a “left shift” mean?
An increase in immature neutrophils (bands ± metamyelocytes) in circulation due to increased demand for neutrophils.
What is a regenerative left shift?
Leukocytosis with immature neutrophils present.
Mature cells still outnumber immature cells.
Indicates effective bone marrow response to inflammation.
What is a degenerative left shift?
Normal or low WBC count, with immature cells outnumbering mature cells.
Indicates bone marrow cannot keep up with demand.
Often associated with toxic changes → poor prognosis.
What are toxic changes in neutrophils, and why do they occur?
Morphologic signs of accelerated production or immature release from marrow.
Occur with infection, inflammation, or toxin exposure when marrow releases cells early.
List the five types of toxic change seen in neutrophils.
Toxic granulation – large blue granules (dog).
Toxic vacuolation – “moth-eaten” cytoplasm.
Döhle bodies – light blue inclusions (common in cats).
Cytoplasmic basophilia – blue streaking appearance.
Nuclear immaturity – less condensed chromatin.
What is a stress leukogram, and what causes it?
Caused by corticosteroid release (pain, trauma, stress, Cushing’s).
neutrophilia, monocytosis, lymphopenia, will be present
What is Physiologic neutrophilia:
short-term response to excitement or fear
caused by epinephrine release.
It results from neutrophils shifting from the marginated pool into the circulating pool, and it lasts only 30–60 minutes.
No left shift or toxic change, and other white cell types remain normal.
What is Stress neutrophilia?
corticosteroid release (from pain, trauma, long-term illness, or chronic stress).
neutrophils are retained in circulation instead of moving into tissues,
bone marrow storage pool is stimulated to release more cells.
It is typically accompanied by lymphopenia and eosinopenia, and sometimes mild monocytosis — forming a stress leukogram.
What is inflammatory neutrophilia?
Occurs when true tissue damage or infection
creating a demand for phagocytic cells.
bone marrow increases production and release, often showing a left shift and possibly toxic changes if the demand is high.
If the bone marrow keeps up, this is an appropriate response; if not, a degenerative left shift may appear.
What causes neutropenia?
Excess usage/consumption – acute infection overwhelms supply.
Reduced production – marrow suppression (e.g. FeLV, parvo, chemo).
Ineffective production – abnormal maturation (“maturation arrest”).
Sequestration – sudden margination (shock, endotoxemia).
Why is neutropenia with toxic change a poor prognostic sign?
It indicates severe, overwhelming inflammation where demand exceeds marrow capacity — the body cannot produce neutrophils fast enough.
What causes lymphopenia, and what are its effects?
Cause: Endogenous corticosteroids (stress, pain, chronic illness).
Effect: Depresses immune response and forms part of the stress leukogram pattern.
What does monocytosis indicate?
Occurs in chronic or late-stage inflammation.
Reflects macrophage cleanup of debris.
Return of monocytes after a degenerative left shift = good prognosis.
What are common causes of eosinophilia?
Chronic respiratory disease
Chronic skin disease
Parasitism
Immune-mediated disorders
(Not diagnostic, but supports these conditions.)