8.3 The Adaptive Immune System
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
Humoral Immunity
Involves the production of antibodies and may take as long as a week to become fully effective.
Antibodies
Produced by B-cells, they are specific to the antigens of the invading microbe.
Immunoglobulins
Another name for antibodies, they can attract leukocytes to phagocytize invaders, they can agglutinate which is when the pathogens clump together, or they can render invaders inactive by blocking their entry to the tissues.
Agglutination
Antibodies may cause pathogens to clump together to form large insoluble complexes that can be phagocytized.
Cell-Surface Antibodies
The binding of an antigen to a B-cell causes activation of that cell, resulting in its proliferation and formation of plasma and memory cells.
Degranulation
When an antigen binds to antibodies on the surface of a mast cell, it causes the cell to exocytose its granule contents, allowing the release of histamine and causing an inflammatory allergic reaction.
Structure of an Antibody Molecule
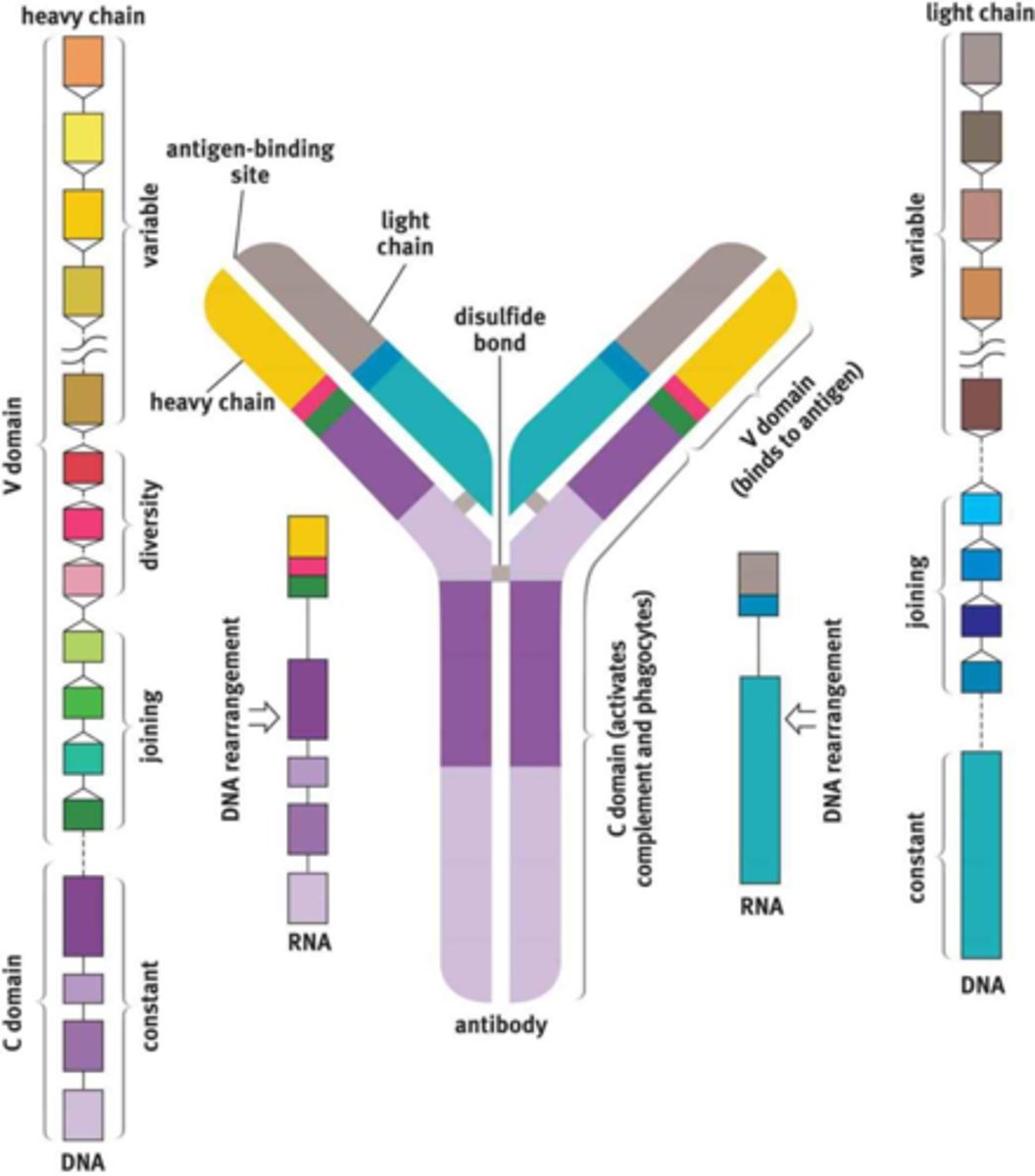
Variable Region Domain
The region at the tip of the Y that holds specific polypeptide sequences that will bind to only one antigen sequence.
Hypermutation
B-cells undergo this on its antigen-binding region, trying to find the best match for the antigen.
Clonal Selection
Mechanism of generating antibody specificity by allowing only B-cells with high affinity to their antigen to survive.
Constant Region
The part of the antibody molecule that cells like natural killers, macrophages, monocytes, eosinophils, and many others bind to.
Isotype Switching
The process by which cells can change which isotype of antibody they produce when stimulated by specific cytokines.
Naive B-Cells
When B-cells are released into the bloodstream when they have not yet been exposed to an antigen.
Plasma Cells
Produce large amounts of antibodies.
Memory B-Cells
When a B-cell remains in the lymph node, awaiting reexposure to the same antigen.
Primary Response
Initial activation of B-cells which takes approximately 7 to 10 days and results in forming memory B-cells to speed up future exposures.
Secondary Response
When an organism encounters a familiar antigen, the memory B-cells for that pathogen begin producing antibodies specific to that pathogen.
Vaccinations
Rely on the memory B-cells.
T-Cells
Mature in the thymus, where they undergo both positive and negative selection.
Positive Selection
Refers to maturing only the cells that can respond to the presentation of antigen on MHC. Cells that cannot respond to MHC undergo apoptosis because they will not be able to respond in the periphery.
Negative Selection
Refers to causing apoptosis in cells that are self-reactive, meaning they are activated by proteins produced by the organism itself.
Thymosin
A peptide hormone secreted by the thymic cells that drives T-cell maturation.
Naive T-Cell
A T-cell that has already matured in the thymus but has not yet encountered an antigen.
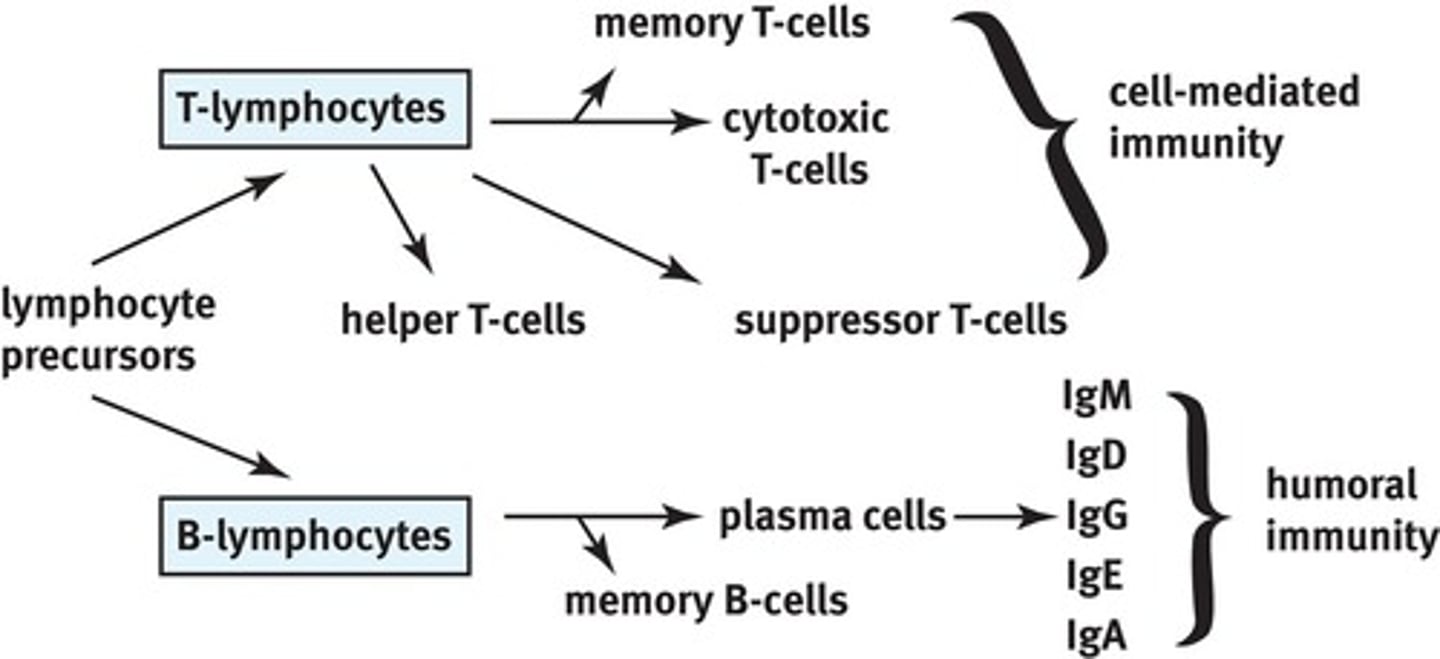
Helper T-Cells, Cytotoxic T-Cells, Suppressor T-Cells
The three major types of T-cells.
Helper T-Cells
Also known as CD4+ T-cells, they coordinate the immune response by secreting lymphokines.
Lymphokines
Released from helper T-cells, these molecules are capable of recruiting other immune cells such as plasma cells, cytotoxic T-cells, or macrophages and increasing their activity.
Lymphocyte Chemotaxis
Circulating lymphocytes can detect a very small concentration of lymphokine and then move up the concentration gradient towards where the immune response is required.
Interleukins
The most common family of lymphokines secreted by helper T-cells.
Human Immunodeficiency Virus
Infection by this virus causes the loss of helper T-cells, thus preventing the immune system from mounting a response to an infection.
CD4+ T-Cells
Another name for helper T-cells, they respond to antigens presented on MHC-II molecules. Since MHC-II molecules present exogenous antigens, these cells are most effective against bacterial, fungal, and parasitic infections.
Cytotoxic T-Cells or Cytotoxic T-Lymphocytes or CD8+ T-Cells
Cells that are capable of directly killing virally infected cells by injecting toxic chemicals that promote apoptosis in the infected cell. These cells respond to antigens on MHC-I molecules, meaning that they respond to endogenous antigens. They are most effective against viral infections.
Suppressor or Regulatory T-Cells
These cells also express CD4 but are different from helper T-cells in that they also express a protein called Foxp3. These cells help to tone down the immune response once infection has been adequately contained.
Memory T-Cells
Lie in wait until the next exposure to the same antigen. When activated, the response is much quicker and more robust the second time around.
CD4/8 Mnemonic
CD4+ T-cells are better at fighting extracellular infections. CD8+ T-cells are better at fighting intracellular infections.
(CD x MHC = 8); (4 x 2 = 8) and (8 x 1 = 8).
Lymphocytes of Specific Immunity
Ig types in humoral immunity: GAMED.
Th1 and Th2 Cells
The two types of CD4+ T-cells, which are activated when dendritic cells present the antigen to T-cells.
Th1 Cells
Release interferon gamma, which activates macrophages and increases their ability to kill bacteria.
Th2 Cells
Help activate B-cells and are more common in parasitic infections.
After Pathogen Elimination
The plasma cells die off but memory B-cells and memory T-cells remain and allow for a much faster secondary response upon exposure to the pathogen at a later time.
Interferons
Produced and secreted in response to viral infection. They reduce the permeability of nearby cells which makes it hard for viruses to invade them, and they also reduce the rate of transcription and translation in these cells.
Malaise, Muscle Ache, and Fever
Symptoms caused by interferons.
Virally Infected Cells
Present intracellular proteins on their surface in conjunction with MHC-I, almost always including viral proteins.
CD8+ T-Cell Response to Virally Infected Cells
Recognize the MHC-I and antigen complex as foreign and will inject toxins into the cell to promote apoptosis.
Self-Antigens
The proteins and carbohydrates present on the surface of every cell of the body. Under normal circumstances, they signal to immune cells that the cell is not threatening and should not be attacked.
Autoimmunity
A condition in which the immune system attacks cells presenting certain self-antigens.
Hypersensitivity Reactions
Include allergies and autoimmunity. Occurs when the immune system attacks certain antigens that are not inherently threatening. Examples include pet dander, pollen, and peanuts.
Negative Selection
Mechanism of Preventing B-Cell Autoimmunity
Negative selection process by which B-cells in the bone marrow which are responsive to self-antigens are killed while still in the bone marrow.
Glucocorticoids
Drugs for treating autoimmune diseases. They work through their potent immunosuppressive qualities.
Active Immunity
Immunization through which the immune system is stimulated to produce antibodies against a specific pathogen. The means of exposure may be natural or artificial.
Natural Exposure
Antibodies are generated by B-cells once an individual becomes infected.
Artificial Exposure
Usually done through vaccines, in which an antigen is injected and antibodies are produced. The antigen may be a weakened or killed form of a microbe, or it may be a part of a microbe's protein structure.
Passive Immunity
Results from the transfer of antibodies to an individual. The immunity is transient because only the antibodies, and not the plasma cells that produce them, are given to the individual. A natural example is the transfer of antibodies from a mother to the fetus through the placenta and in the breast milk.
Intravenous Immunoglobulin
Given to patients in cases of exposure to tetanus or rabies to prevent the pathogen from spreading.
Mechanism of Preventing T-Cell Autoimmunity
Negative selection process by which T-cells in the thymus that respond to and attack self-antigens are killed off and not allowed to mature.