Ch. 10 Heart Electrical Conduction System + Ch. 11 Electrocardiogram
1/33
Earn XP
Description and Tags
Flashcards about the heart's electrical conduction system
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
What is the significance of the heart's specialized system?
Generating rhythmical electrical impulses and rapid conduction of these impulses.
Atria contract 1/6 of a second before ventricles
All portions of the ventricles contract simultaneously for effective pressure generation
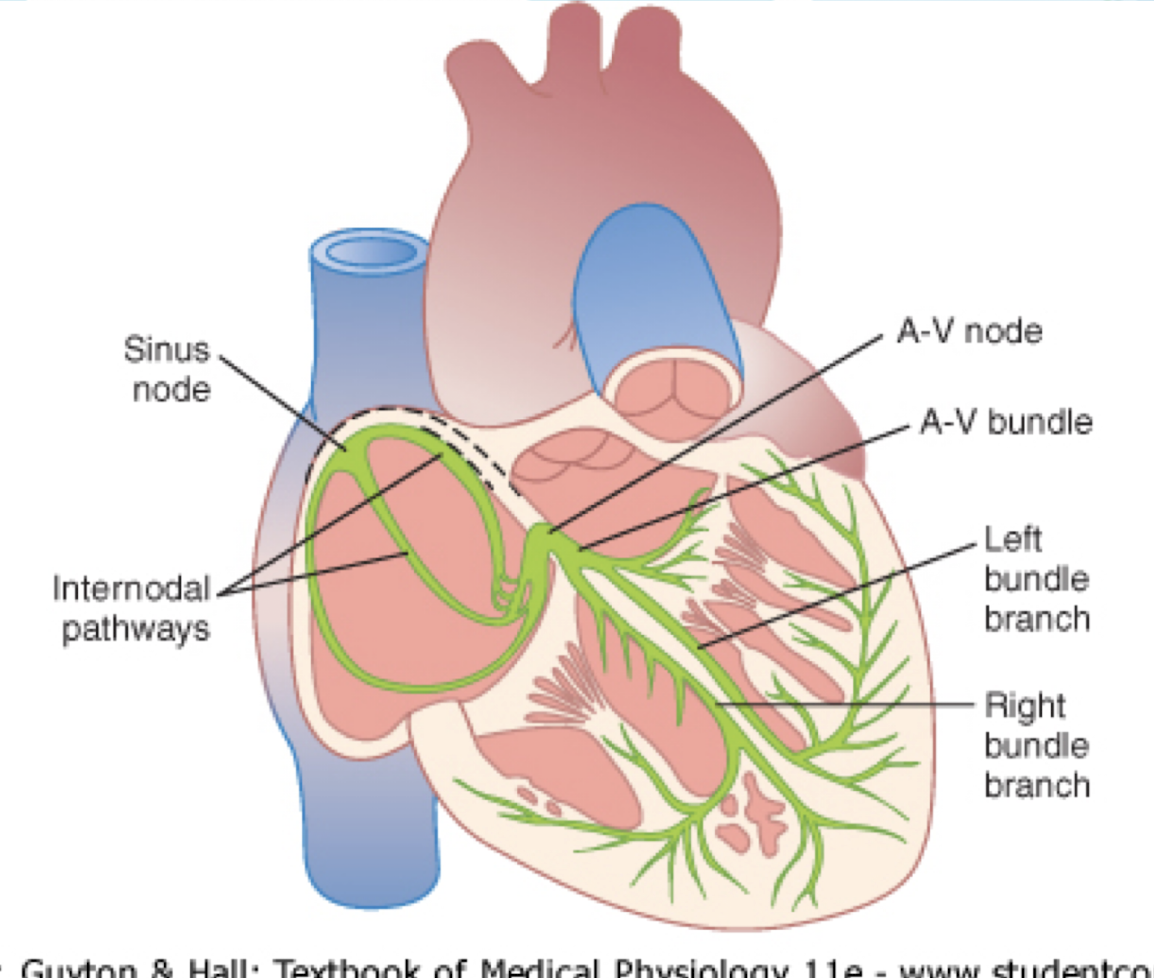
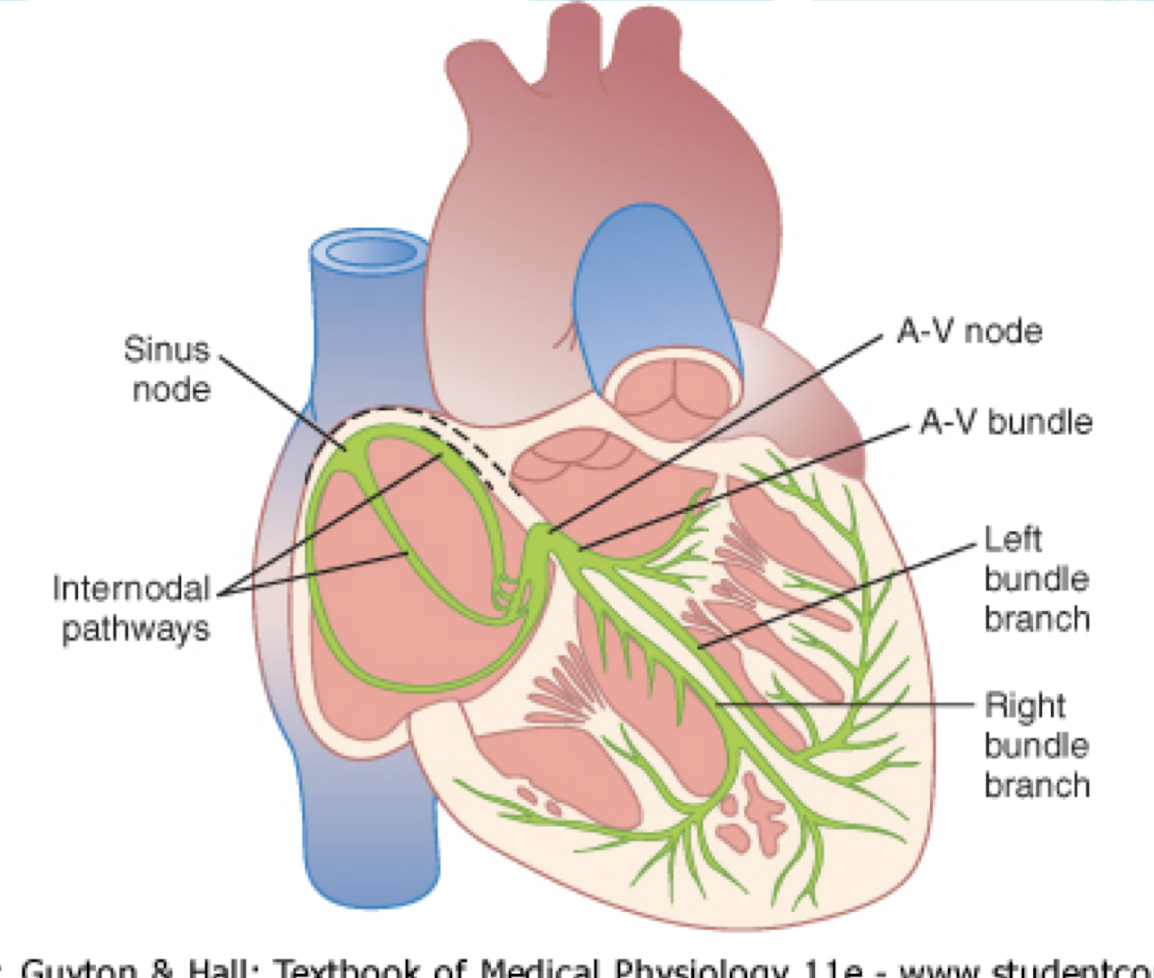
Name the parts of the heart related to the electrical conduction system.
S-A node
internodal pathway,
A-V node,
A-V bundle
left & right bundle branches of Perkinje fibers.
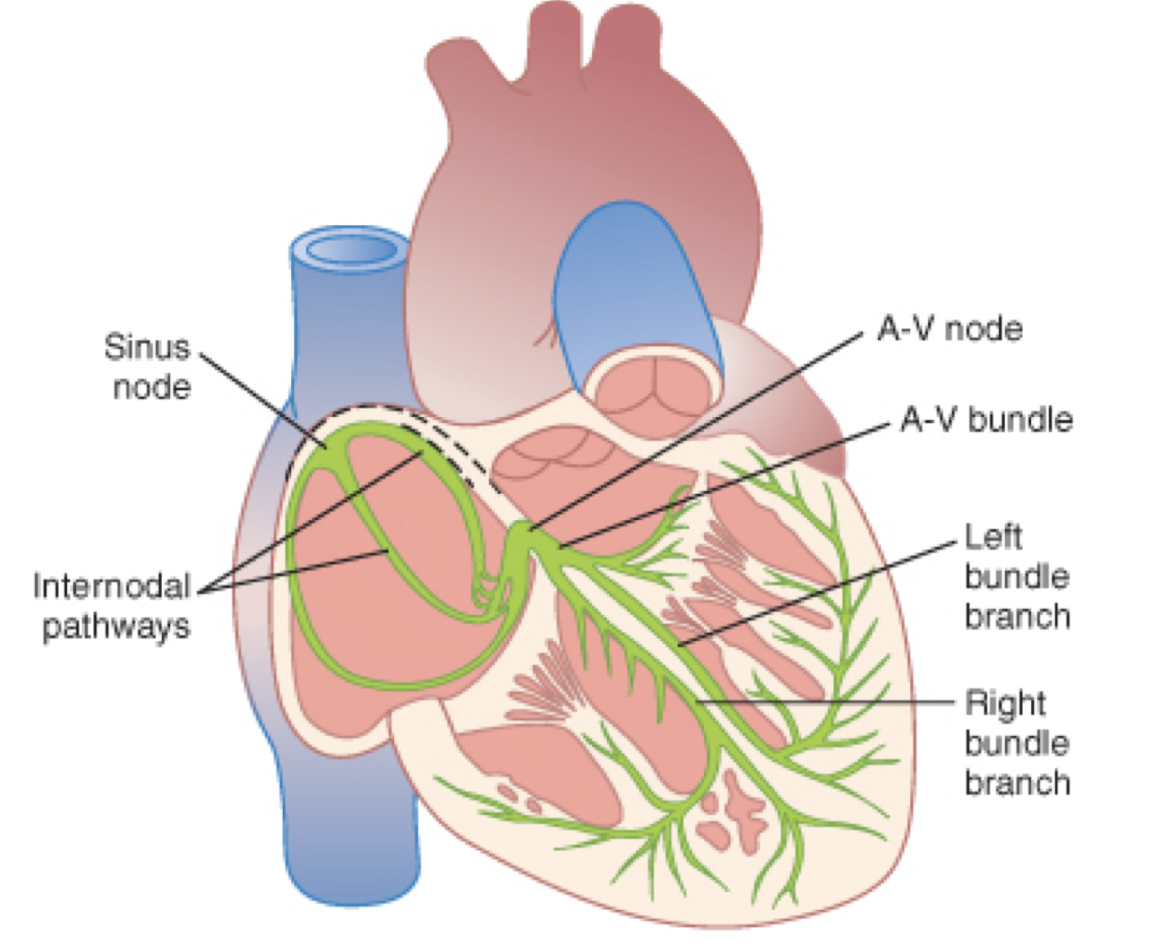
Where is the sinus node located?
In the superior posterolateral wall of the right atrium, immediately below and slightly lateral to the opening of the superior vena cava.
What unique characteristic allows the sinus node to self-excite?
It connects directly with atrial muscle fibers and has no contractile filaments.
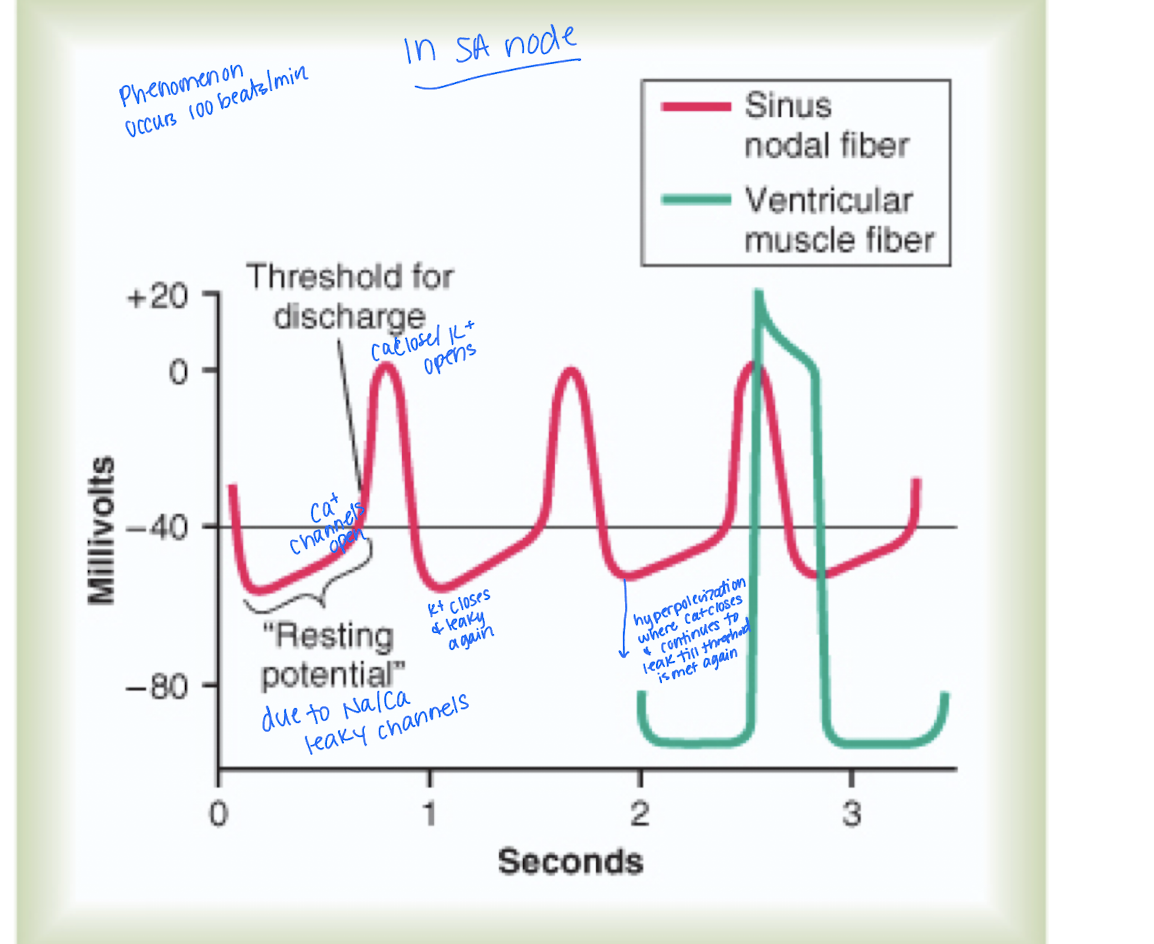
What is the inherent heart rate set by the sinus node?
Approximately 100 beats/min, but parasympathetic system usually overrides to keep it within a safer range.
What causes the lesser Resting Membrane Potential (RMP) in the sinus node?
The cell membrane is naturally leaky to sodium and calcium.
Why doesn't the S-A node remain depolarized?
Sodium-calcium channels close quickly, and potassium channels open, leading to hyperpolarization and reduced cell permeability.
What brings RMP to threshold regularly between heart beats?
Sodium-calcium channel leakiness into the cell
Why doesn’t the SA node remain depolarized?
Sodium-calcum channel closes quickly = permeability reduced
potassium channels open
hyperpolarization due to channel staying open a little longer
What mechanisms are in place to terminate AP in the cardiac muscle?
Potassium channels open
sodium-calcium channel closes quickly
Where does the action potential from the S-A node travel?
Directly to atrial muscle fibers and eventually to the A-V node.
Describe the Internodal pathway
AP from the SA node travels directly to atrial muscle fibers and to AV node
Consists of the Anterior interatrial band - excitatory tissues sending signals from SA node to Left Atria
3 bands: Anterior, Middle, and Posterior
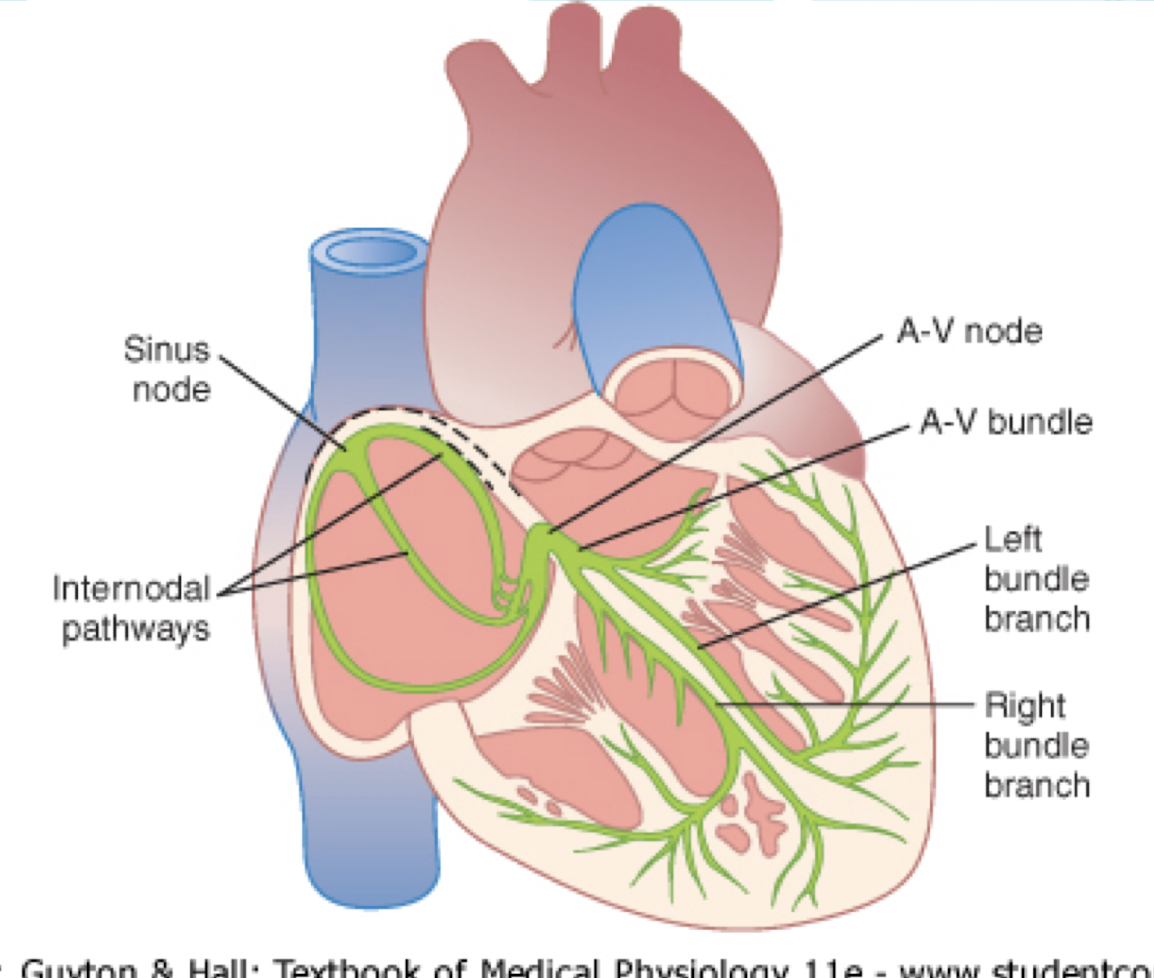
What are two keys to knowing about the Internodal pathway?
Signal is initiated from SA node to L. Atria because SA node sits in the right atria
Atria contract before the ventricles
What would happen if the Atrioventricular fibrous tissue did not perform correctly?
Action potential would travel into branches & atria simultaneously, ventricles would contract.
Where is the A-V node located?
What is the AV node function?
In the posterior wall of the right atrium behind the tricuspid valve.
Delay AP to ventricles due to diminished number of gap junctions - reason why AP will slow/stop at the AV node to allow atria to contract before the ventricles
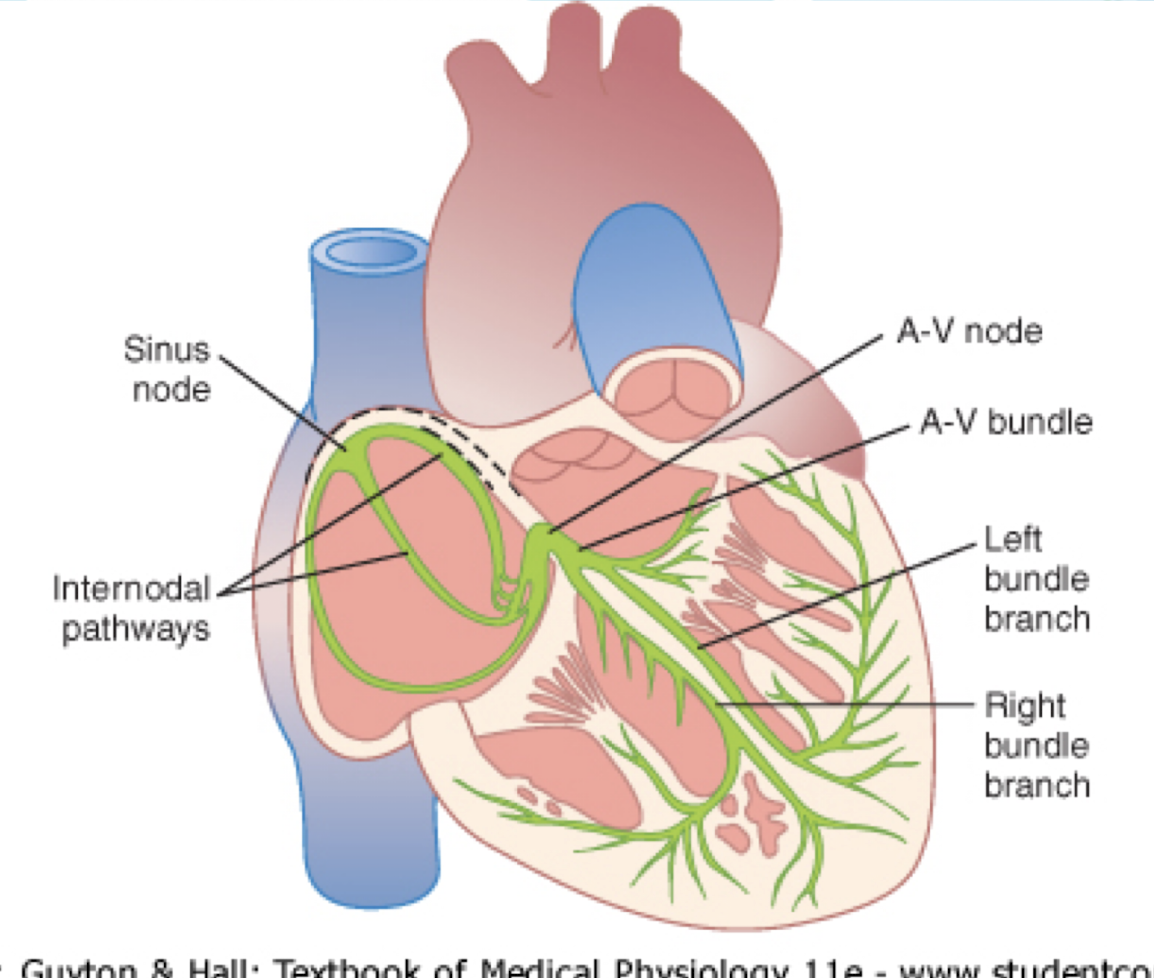
What is a unique feature of the Perkinje system's conduction?
It is a one-way conduction system not allowing re-entry to atria.
Almost instantaneous transmission throughout the ventricular muscle.
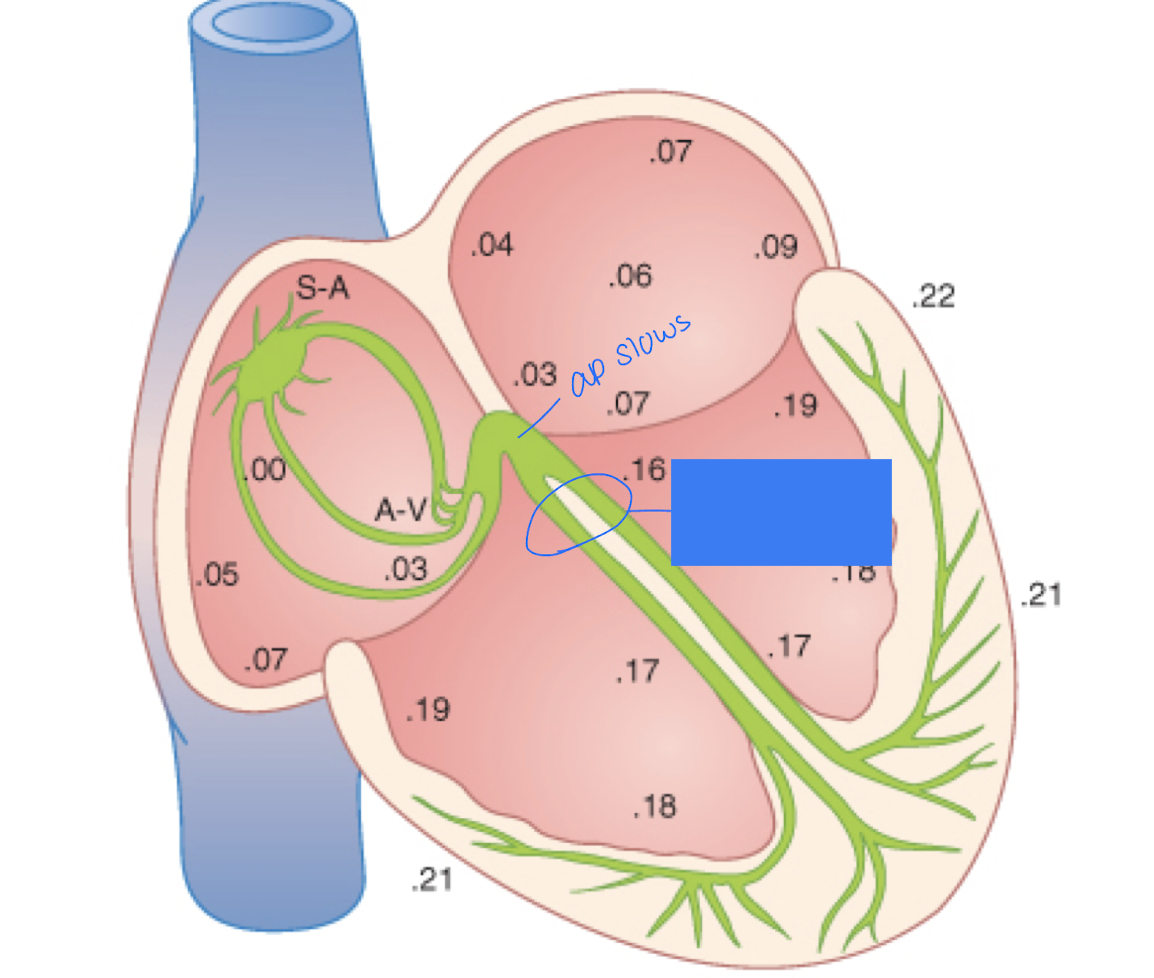
What can be noted about the area circled in the image?
Once action potential reaches here, the atria are done contracting.
Prior to, the action potential will slow at the AV node
In the case the SA node has trouble firing, what mechanism can be be initiated?
The AV node and Perkinje fibers can discharge an intrinsic rhythm and operate an action potential
AV node is first line of defense firing at a rate of 40-60 times/min and Perkinje is next but slower at 15-40 times/min
The AV node sits PAST the atria and in the case SA node is out, the AV won’t be able to contract the atria but it’s okay because the atria passively fill majority (80%) of blood
Since the AV node and Perkinje fibers can step in for the SA node and generate an action potential, why do we need to use the SA node as the pacemaker?
SA node fires faster per minute (100 beats/min) than the AV node and Perkinje fibers, ensuring efficient heart rhythm and optimal blood flow.
What is an ectopic pacemaker?
A signal initiated somewhere other than the S-A node in the atria or ventricle, causing an abnormal sequence of contraction, severely limit pumping of the heart
Can cause an AV block and Stokes-Adams syndrome
What happens during an A-V block?
Occurs due to an ectopic pacemaker
The impulse fails to pass from atria into ventricles through the A-V node and bundle system.
Next line of defense: Purkinje do not begin to emit intrinsic rhythmical impulses for 5-20 seconds due to suppressed state of rapid sinus rhythm
Ventricles will fail to pump and person will faint due to hypoxia (reduced blood flow to the brain) known as Stokes-Adams syndrome and occurs spontaneously
Why is synchronous contraction of the heart critical?
Critical to the overall effectiveness of pumping by ventricles.
What is the Vagal Effect on Heart Rate?
(parasympathetic view)
ACH will be released from nerve endings
causes decrease in HR from SA node and decrease in excitability of the AV junctional fibers (between atrial muscles and AV node) slowing conduction into the ventricles
Overall - weak to moderate vagal stimulation (Parasympathetic system) slows heart rate by ½
Vagal effects will decrease the heart rate by decreasing firing of the SA node and excitability of the AV junctional fibers. How is this process occurring mechanistically and how does it relate to membrane potential?
ACH increases permeability K+ to the cell membrane causing a leak = hyperpolarization (less excitable and reducing heart rate)
The decrease in resting membrane potential causes a longer time for sodium and calcium to LEAK and reach threshold for excitation
A normal vagal effect will slow heart rate. What will a strong vagal stimulation produce?
Strong stimulation will cause a significant drop in HR through the AV node and potentially lead to fainting.
Heart can temporarily stop and spontaneously restart with next line of defense: Purkinje develop rhythm of its own (15-40 beats/min)
known as ventricular escape
What is Ventricular Escape?
When strong vagal stimulation stops impulses through A-V node, Purkinje develop rhythm of own (15-40 bpm).
describe the effects of sympathetic stimulation on the heart
Increases rate of sinus node discharge
Increases rate of conduction of AP and excitability
Greatly increases force of contraction.
What effects does NE (norepinephrine) have on the heart?
Increases permeability to sodium and calcium, causing a more positive RMP.
Describe the mechanistic relation of sympathetic stimulation on the heart
NE will be released from nerve endings causing an increase in permeability to sodium and calcium
RMP will become positive moving the RMP closer to threshold for self-excitation and accelerating heart rate
also decreases conduction time from atria to ventricles
What are the characteristics of a normal EKG?
P wave
QRS complex
T wave
P wave - atrial depolarization
QRS complex - ventricular depolarization
T wave - ventricular repolarization
T/F: P wave occurs beginning of contraction of atria
true
same for QRS - occurs beginning of ventricular contraction
The QRS complex signifies ventricular contraction. How long do the ventricles remain contracted?
A. Till repolarization begins
B. Till after repolarization occurs
C. Till the end of the T wave
D. none of the above
B. Till after repolarization occurs
C. Till the end of the T wave
T/F: Atrial T wave is obscured by P wave
False - by QRS complex
A person’s EKG shows prolonged PR interval. What part of the conduction system is likely involved, and what does this signify?
a delay in the impulse traveling through the AV node, which is responsible for:
Slowing conduction to allow the ventricles time to fill after atrial contraction