Lecture 21: Pain receptors and pain pathways
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
nociception
the unconscious activity induced by a harmful stimulus applied to sensory receptors
allodynia
•sensation of pain in response to an innocuous stimuli
Hyperalgesia
exaggerated response to a noxious stimuli
Nociception
-unspecialized nerve cell endings
-come from cell bodies in dorsal root ganglia or trigeminal ganglion
mechanical, thermal, chemical
what type of stimuli does nociception respond to?
Adelta fibers
type of nociceptor
-thinly myelinated
-FAST
-responds to intense mechanical or cold stimuli
C nociceptive fibers
-unmyelinated, small, slow
-responds to pain, warmth, itch, non-discriminative touch
C nociceptive fiber
what type of nociceptor responds to mechanical, thermal, and chemical stimuli; polymodal
short lived, tingling, sharp
well localized
If stimulus intensity is raised to level that actives Aδ fibers, pain is perceived as
dull, long lasting pain that is poorly localized
if stimulus intensity increases beyond that of Adelta fibers, C fibers are activated, resulting in pain perceived as
first/fast pain
processing of stimulus that activates nociceptors
-acute (sharp)
-well localized
-signals current or impending tissue damage
-is "protective"
-result of AB fiber releasing glutamate
second/slow pain
longer-lasting, dull, diffuse feeling
-C fibers release combo of glutamate and substance P
transient receptor potential
receptors embedded in the membrane of nocireceptors, involved in transduction of thermal, mechanical, and painful stimuli
TRPV1 and TRPA1
-found in Aδ & C fibers
-activated by heat (45°C), acids & chemicals, or indirectly by TRPV3 receptor activation
-similar to voltage gated channels
-open sodium and calcium influx
how do you trigger an AP in a transient receptor potential channel
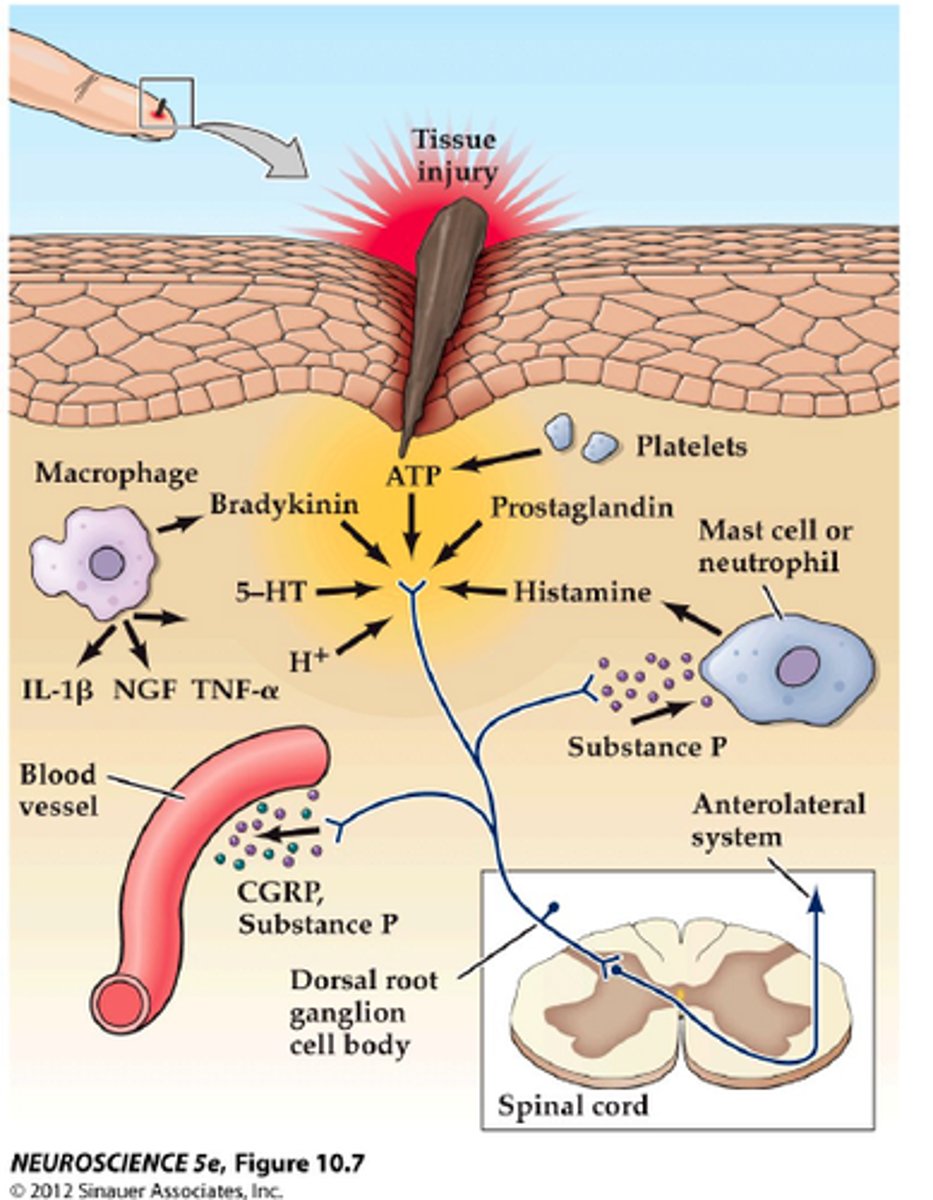
Sensitization
in the instance of exceptionally intense, repeated, or prolonged stimuli, the threshold for activating primary afferent nociceptors is lowered and the frequency of firing is higher for all stimulus intensities
sensitization
keeps person apprised of tissue damaging stimulus as long as it persists
the level of the peripheral nerve terminal as well as at the dorsal horn of the spinal cord
at what levels does sensitization occur?
peripheral sensitization
consequence: sub-threshold stimuli now become sufficient to generate AP, increasing pain sensitivity
-harmless stimuli now perceived as pain (allodynia)
central sensitization
•Immediate onset, activity-dependent increase in excitability of neurons in dorsal horn of spinal cord, following high levels of activity in peripheral nociceptive afferents
transcription independent central sensitization
"wind up"
-persistent injury results in prolonged release of glutamate on nociceptive dorsal horn cells
-this results in opening of postsynaptic ion channels gated by NMDA receptors--> hyperexcitability
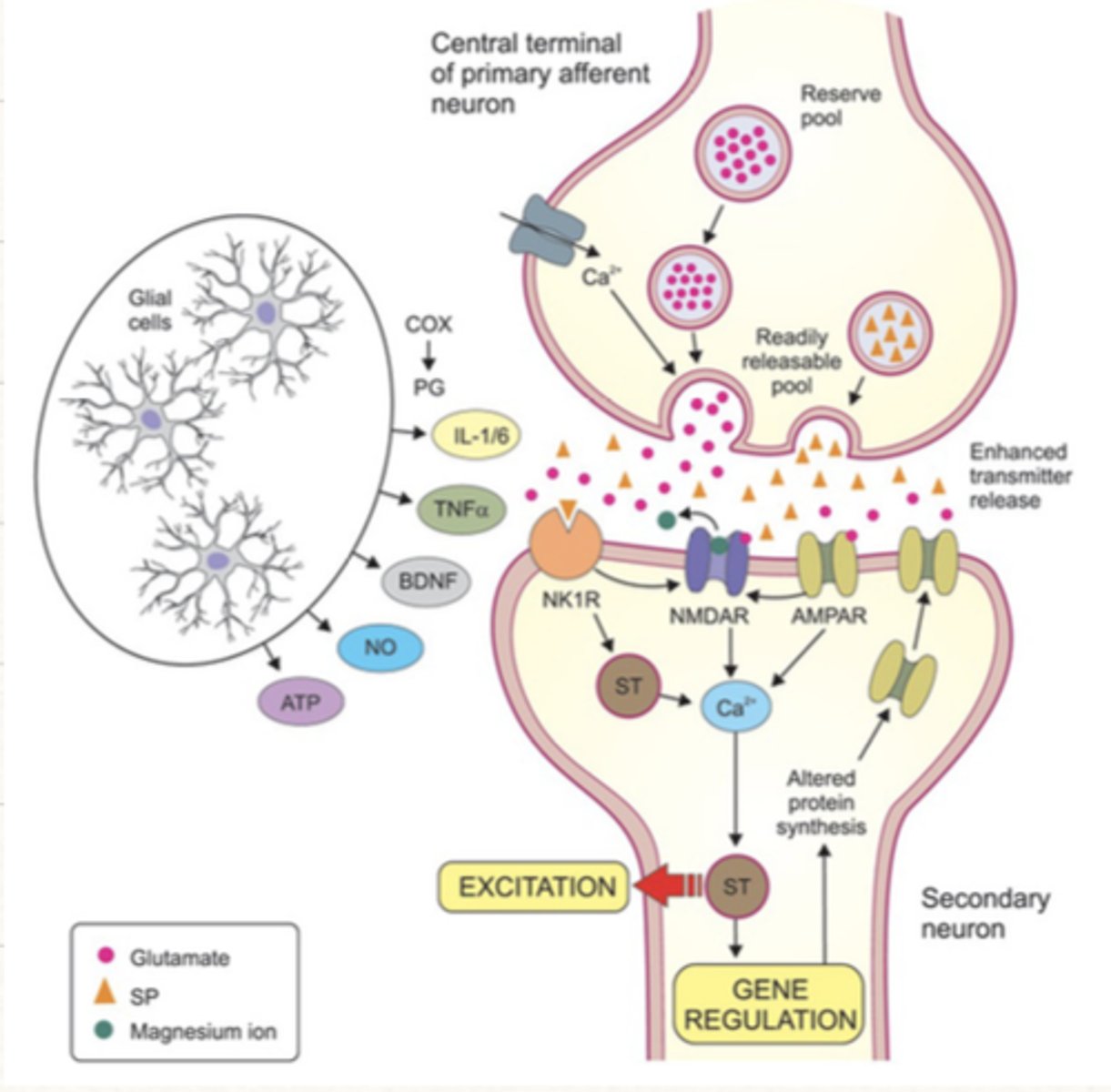
transcription dependent central sensitization
Prolonged changes in the transcription of proteins necessary to the transmission of pain
-NMDA receptor mediated elevations in calcium in postsynaptic spinal cord neurons
-reduction in level of GABAergic or glycinergic inhibition in spinal cord circuits
transcription dependent central sensitization is dependent on
Laminae III-V
on what laminae do AB afferent fibers (nonpain) terminate in

laminae I and III-V
on what laminae do Adelta afferent fibers (fast pain) terminate in?
laminae I and II
on what laminae do C-fiber afferents (slow pain) terminate?
-begin at laminae
-decussate at midline to contralateral, anterolateral spinothalamic tract
-synapses onto 3rd order neuron in ventral posterolateral nuclei
2nd order neurons of the ascending spinal pathway:
A delta fiber pain (fast, somatic)
neospinothalamic tract transmits...?
C fiber pain (slow, visceral)
Archiospinothalamic & Paleospinothalamic tracts transmits
-first order neuron in CN ganglion
-1st order afferent axons enter pons and descend ipsilateral to medulla
-synapse at spinal trigeminal nucleus onto second order neuron
-2nd order neuron decussates and ascends contralaterally as the trigeminothalamic tract
-3rd order neuron in the ventral posteromedial nuclei, ascends too the somatosensory cortex
describe the ascending pathway from the head and neck
lateral pathway
sensory discriminative ascending pathway=
lateral ascending pathway
-mediates location, intensity, and quality of noxious stimuli
-depends on info relayed through VPL (body) or VPM (face)
medial ascending pathway
affective motivational ascending pathway=
medial ascending pathway
•Mediates unpleasant feeling, fear & anxiety, and autonomic activation accompanying exposure to noxious stimuli
-Targets of 3rd-order projections from VPL & VML
-sends info to the anterior cingulate cortex and insula
DCML and ALS
list the central pain pathways
•symptoms (loss of touch/pressure/vibration/proprioception) on side of body ipsilateral to lesion
lesion to the DCML pathway results in
•symptoms (deficits of pain & temperature discrimination) on side of body contralateral to lesion
lesion to the Anterolateral system results in
dissociated sensory loss
-sinngle tract lesions involving selective loss of sensation
•Periaqueductal grey (mesencephalon) & periventricular areas (hypothalamus)
•Raphe nucleus (lower pons/upper medulla) & reticular nuclei (lateral medulla)
•Dorsal horn of spinal cord
what are the 3 major components of the brain that suppress pain signal?
descending pathways
from what pathways do we modulate/suppress pain?
1. nerve fibers from periventricular nuclei and PAG secrete enkephalin at nerve endings in raphe magnus nucleus
2.fibers in raphe magnus nucleus secrete serotonin at the dorsal horn of spinal cord
3. Local spinal cord neurons secrete enkephalin to cause presynaptic & postsynaptic inhibition of incoming Aδ & C pain fibers synapsing in dorsal horns
descending pathway steps
-blocking NT release by inhibiting presynaptic calcium influx
-opening potassium channels to hyperpolarize the cell and prevent AP
endogenous opiates modulate nociceptive input by
-enkephalin and dynorphin containing neurons (in PAG, RVM, and spinal cord dorsal horn)
-endorphin containing neurons in the hypothalamus
where is the highest density of opiate receptors found?
gate control theory of pain
the theory that non-painful input "closes the gates" to painful input, preventing pain sensation from traveling to CNS
-reduce the sensation of pain by activating low-threshold mechanoreceptors
•Sensitization typically declines
•Pain threshold returns to baseline, pre-injury levels
as an injured tissue heals, what happens to sensitization?
neuropathic pain
•If afferent fibers or central pathways are damaged, sensitization processes can persist in the absence of physical stimuli
•Cortical structures can reorganize after loss of a body part
•Axons from neighboring cortical areas spread to area occupied by amputated tissue
how does phantom limb syndrome arise?
sympathetic nerves--> VPL pathway---> DCML
visceral afferents are conducted almost exclusively via what pathways
•Far fewer per unit area vs. mechanosensory neurons supplying skin and somatic structures)
•Visceral sensations are diffuse & difficult to localize precisely
distribution of visceral sensory neurons:
severe pain
diffuse stimulation (ischemia) of visceral pain receptors results in
mild pain
highly localized (like laceration) stimulation of visceral sensory neurons results in
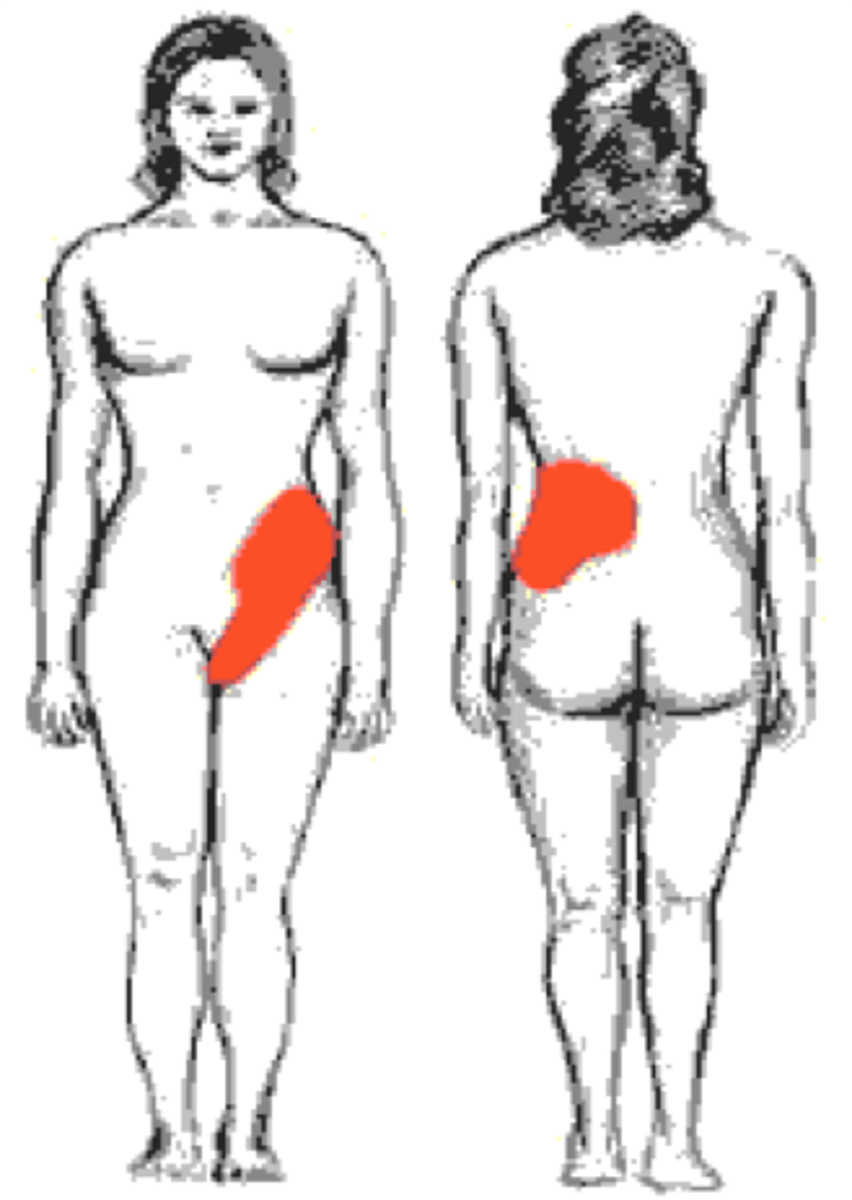
referred pain
•Phenomenon whereby noxious stimuli originating at visceral structure is perceived by patient as pain arising from a remote, somatic portion of body wall
-occurs between somatic structures whose afferents enter the cord at the same level
•"Cross talk" or "bleed over" of somatic and visceral afferent information onto pools of dorsal horn neurons
what causes referred pain?
referred pain of esophagus
referred pain of what structure?

referred pain of heart:
referred pain of what structure?

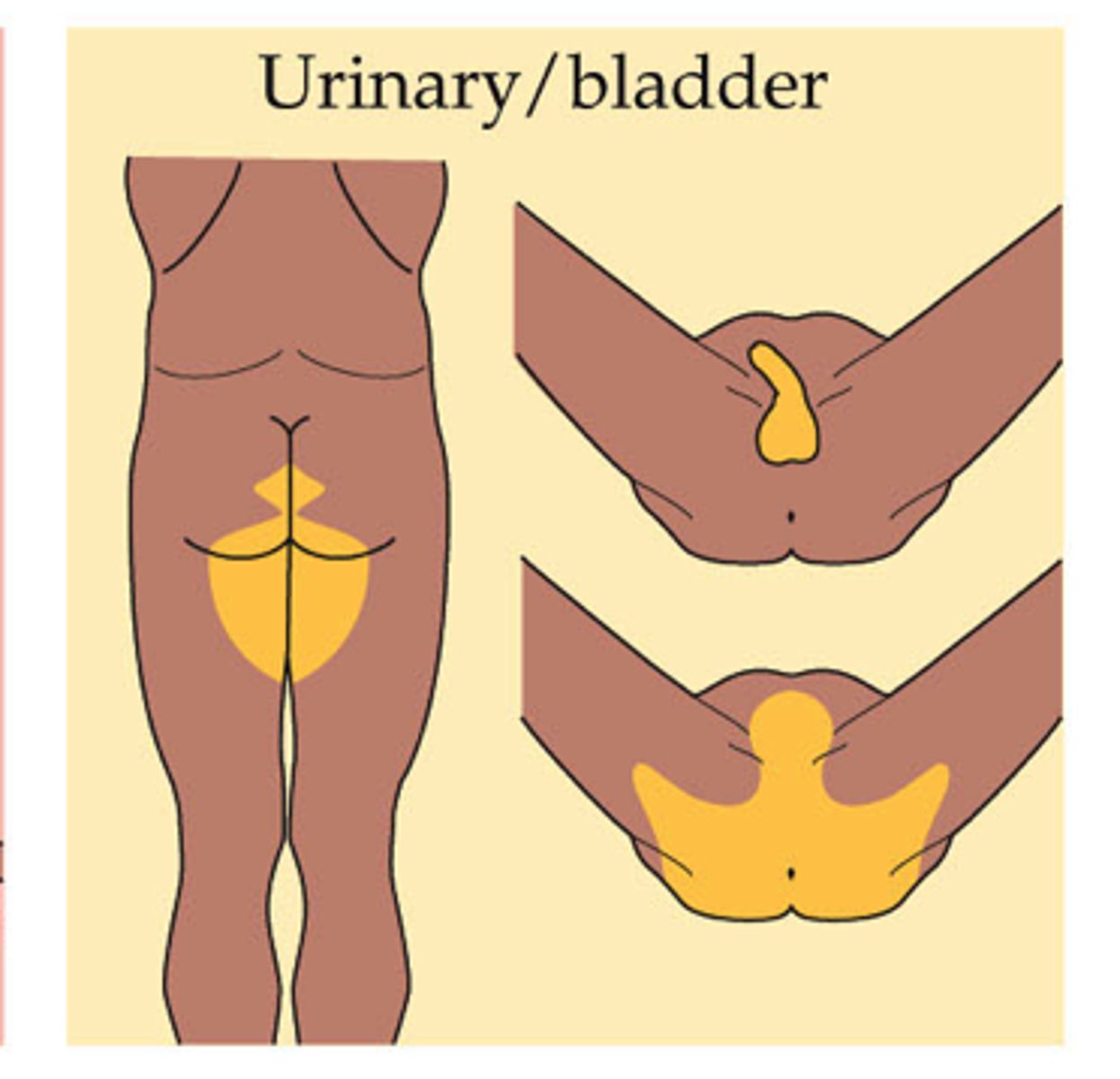
referred pain of bladder
referred pain of what structure?
referred pain of ureter
referred pain of what area
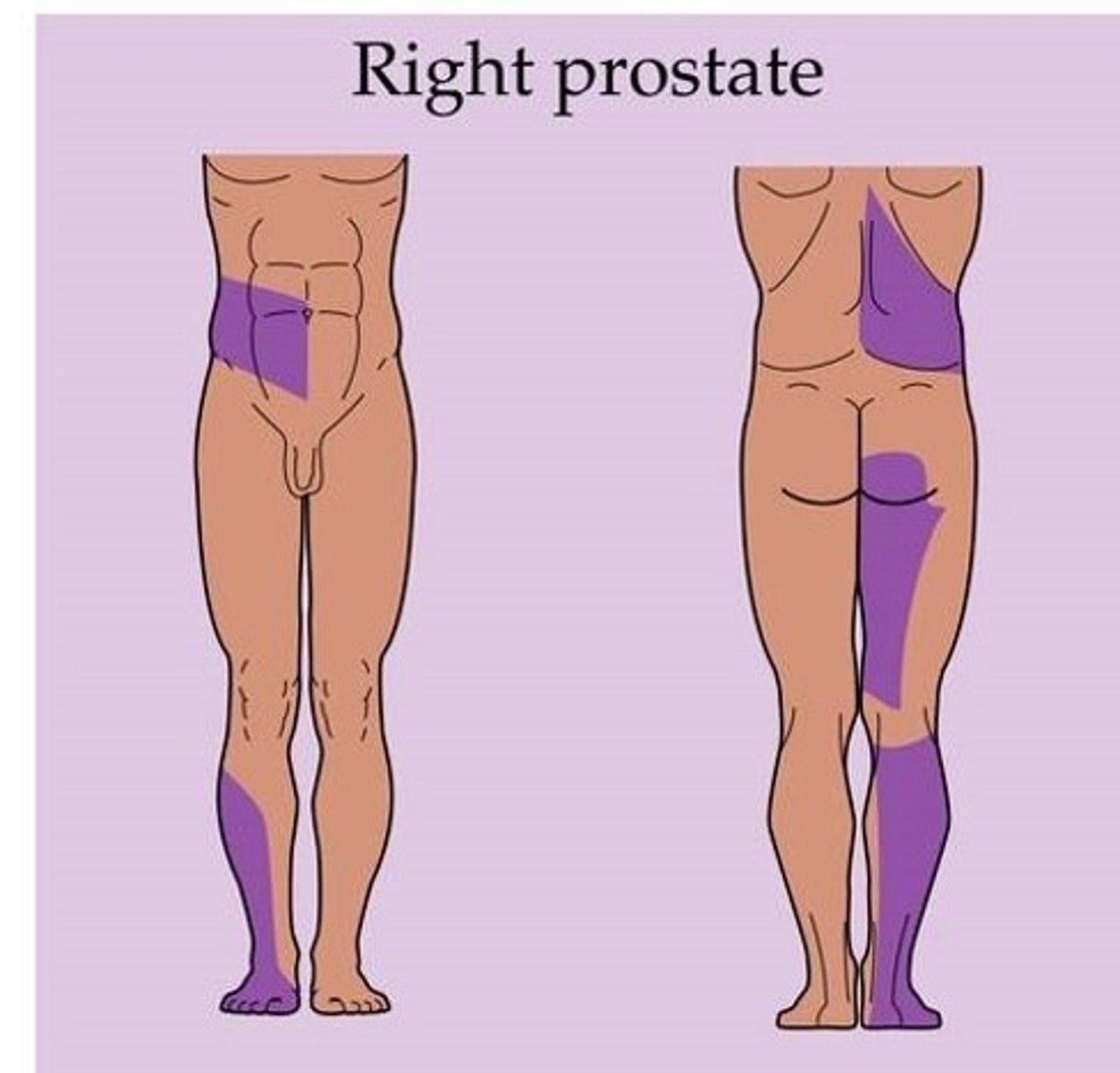
referred pain of prostate
referred pain of what structure?