CHP 11 skeletal muscle physiology
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Universal characteristics of muscle
1) Excitability (responsiveness)
2) conductivity ( signals travel along the muscle fibers)
3) Contractility (contracts)
4) extensibility (can be stretched)
5) elasticity (will go back to original position after being stretched)
Characteristics of skeletal muscle
voluntary
striated
usually attached to bones (w tendons)
cell = muscle fiber
connective tissue wrappings (endomysium, perimysium, epimysium)
Collagen somewhat extensible and elastic
Sarcolemma (apart of muscle fiber)
the cell membrane of a muscle fiber
Sarcoplasm (apart of muscle fiber)
cytoplasm of muscle fiber
contains: myofibrils, glycogen, and myoglobin
Myofibrils (apart of muscle fiber)
in the sarcoplasm
long protein chords
Glycogen (apart of muscle fiber)
in the sarcoplasm
stored blood sugar, stored carb energy for exercise
FOR CELLULAR RESPIRATION
Myoglobin (apart of muscle fiber)
in the sarcoplasm
red pigment
provides oxygen needed for muscle activity
FOR CELLULAR RESPIRATION
Myoblasts (apart of muscle fiber nuclei)
stem cells that fused to form each muscle fiber in EARLY development
Satellite cells (apart of muscle fiber nucleus)
unspecialized myoblasts remaining between muscle fiber and endomysium
play a role in regeneration of damaged skeletal muscle tissue
important parts of a muscle fiber
sarcolemma
sarcoplasm
multiple nuclei
mitochondria
sarcoplasmic reticulum
t tubules
triad
Sarcoplasmic Reticulum (apart of muscle fiber)
wraps around each muscle fiber (the net looking part)
releases calcium to activate contraction
Has terminal cisterns on either side (like a little waste pit)
T tubules (apart of sarcolemma in muscle fiber)
tubular infolding of sarcolemma which penetrate through the cell
Triad (apart of T tubule in muscle fiber)
A T Tubule and two terminal cisterns associated with it
Myofilaments
make up myofibril
1) thick filaments: made of several myosin molecules (shaped like golf club)
2) thin filaments: fibrous actin in 2 intertwined strands + tropomyosin molecules (the strands connecting the actin molecules) + troponin molecule (small calcium binding protein on each tropomyosin molecules)
3) Elastic Filaments: made of Titin (huge springy protein), helps thick filaments stay centered between Z discs and M line= stabilize + shock absorber
Contractile Proteins
myosin + actin
they overlap causes contraction
Regulatory proteins
tropomyosin + troponin
allow muscles to relax or contract (it is like an on off switch)
How? by the release of calcium into sarcoplasm, binds to troponin, changes shape, moves tropomyosin off active sits on actin
Dystrophin
SO IMPORTANT PROTEIN
links actin to outermost myofilaments
allows forces of muscle contraction to transfer to connective tissue to the tendon
GENETIC DEFECT = muscle dystrophy
Striations
alternating A bands (dark) and I bands ( light)
A band: has H band (middle of A band) + M line (middle of H band)
I band: Z disc (anchorage for thin filaments, “zigzags”)
Sarcomere (apart of muscle fiber)
segment from Z disc to Z disc
NO ACTUAL SHORTENING OF LENGTH during contraction only OVERLAP changes
Structural hierarchy of muscle
Muscle- wrapped in epimysium
Fascicles- wrapped in perimysium
Muscle Fibers- wrapped in sarcolemma
Myofibrils- wrapped in endomysium, has striations
myofilaments- causes striations from overlap; causes contraction, Thick (myosin), Think (actin)
sarcomere- z disc to z disc segment
How does a muscle contract?
It should NEVER contract unless stimulated by a nerve
Denervation atrophy
shrinkage of paralyzed muscle when nerve remains disconnected
Somatic Motor neuron
nerve cells whose bodies are in the brainstem and spinal cord that serve skeletal muscles
includes somatic motor fibers (their axons lead to the skeletal muscle that then branches out to a number of muscle fibers
ONLY ONE MUSCLE FIBER TO ONE MOTOR NEURON
Motor Unit
one nerve fiber and all the muscle fibers activated by it
-contract in unison but motor units take turns contracting
-small or large
Small motor unit
-for fine degree of control
-eye and hand muscles
Large motor unit
-for more strength than control
-powerful contractions because they have HUNDRED of fibers
Neuromuscular junction
-one electrically active cell to another
-when target cell is a muscle fiber
-nerve fiber connected to muscle fiber by a synapse
synapse
point where a nerve fiber meets its target cell
Axon terminal
-apart of a neuromuscular junction
-swollen end of a nerve fiber
-contains synaptic vesicles with acetylcholine
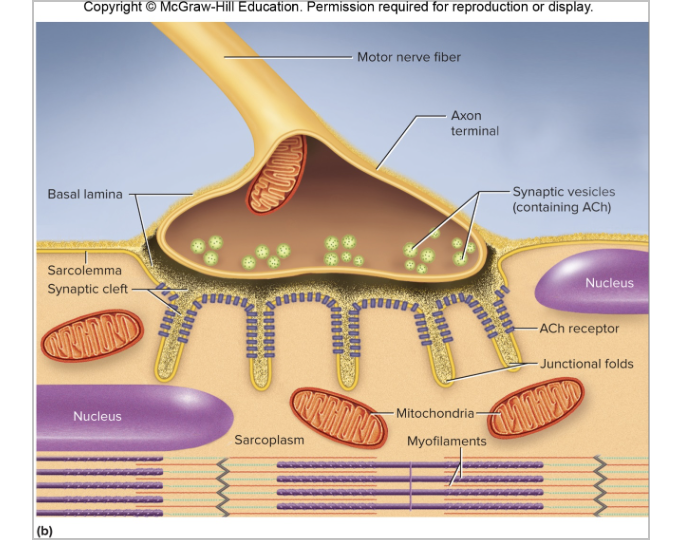
Synaptic Cleft
-apart of a neuromuscular junction
-gap between axon terminal and sarcolemma
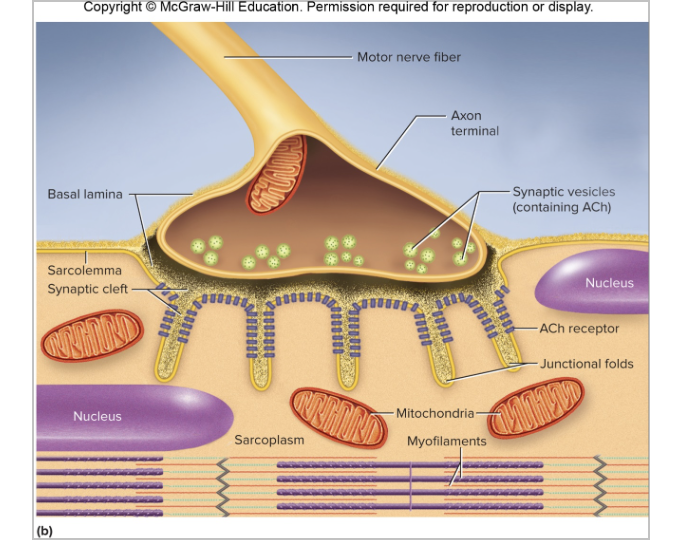
Schwann cell
-apart of a neuromuscular junction
-envelops and isolates NMJ
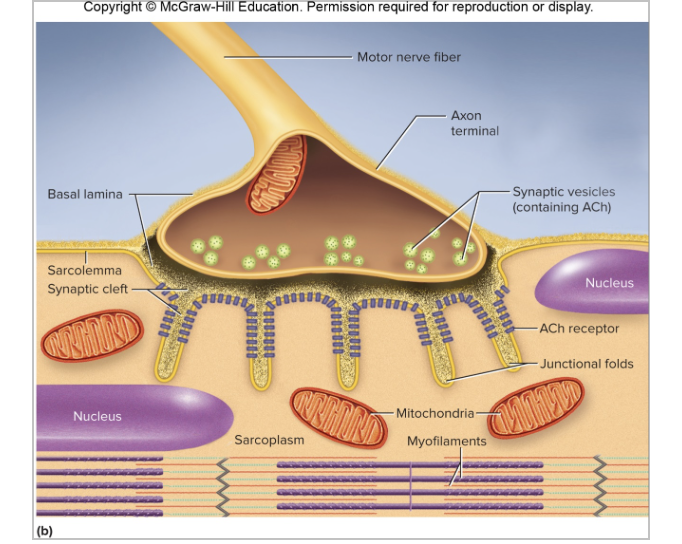
The process of the neuromuscular junction
-nerve impulses cause synaptic vesicles to do exocytosis and release ACh into synaptic cleft
-ACh carries signals (neurotransmitters)
-Muscle cell has millions of ACh receptors (proteins incorporated into its membrane)
-lack of these receptors = weakness in skeletal muscles; myasthenia gravis
How muscle cells respond to stimulation (voltage)
-their membranes exhibit voltage changes
-voltage (electrical potential) = a difference in electrical charge from one point to another
-resting membrane potential = about -90 mV which is maintained by the sodium potassium pump
The process of electrically excitable cells
1) REST (-70mv) = more negative ions inside the cell which causes the inside to be negatively charged; potassium ions in the cell, sodium ions outside the cell
-maintained by the sodium potassium pump
2) LOCAL POTENTIAL= chemical stimulant binds to a receptor on a neuron, opens Na+ gates to slowly let Na+ into the cell, but it isn’t anything drastic
3/4) is ABSOLUTE REFRACTORY PERIOD
3)WHEN REACHES CRITICAL VOLTAGE THRESHOLD (-55mv) : SWITCH TO ACTION POTENTIAL: protein channels are now being used to allow the transfer of ions; Sodium gates open up and sodium flows into the cell RAPIDLY NOW = DEPOLARIZATION (inside cell is now positive)
4) ACTION POTENTIAL CONT (+35mv)= sodium gates immediately close and potassium ones open, potassium ions leave the cell =REPOLARIZATION (inside cell is back to negative)
5) RELATIVE REFRACTORY PERIOD: continues until the cell reaches a hyper polarized state (below resting membrane potential) , then potassium gates close
6) Sodium potassium pump plays catch up to get back to resting membrane potential (3 sodiums in, 2 potassiums out)
Resting Membrane Potential vs Action Potential
Resting Membrane Potential= negative intracellular in a waiting cell to be stimulated
Action Potential= causes voltage changes, quick event in a. stimulated cell
a positive feedback loop that ripples one cell to another is called IMPULSE
Spastic Paralysis
continuous contraction, possible suffocation
Tetanus
(lockjaw)
form of spastic paralysis caused by the toxin Clostridium tetani
how? the toxin blocks glycine release (in spinal chord that normally stops motor neurons from producing unwanted muscle contractions)
Flaccid Paralysis
a state where muscles are limp and cannot contract
How? Curare competes w ACh for receptor sites but does not stimulate the muscles so it being there is a blockage
Botulism
type of food poisoning caused by a neuromuscular toxin in the bacterium clostridium botulinum
how? blocks the release of ACh causing flaccid paralysis
other ways? botox cosmetic injections used for wrinkle removal
How do toxins paralyze muscles?
some things have cholinesterase inhibitors (they bind to acetylcholinesterase and prevent it from degrading ACh; initiating muscle contraction at the neuromuscular junction)
Behaviors of skeletal muscle fibers
1) Excitation= nerve action potentials lead to muscle action potentials
2) excitation-contraction coupling= events that link action potentials on the sarcolemma to activation of the myofilaments, preparing them for contraction
3) contraction= muscle fiber develops tension and may shorten
4) relaxation= stimulation ends and a muscle fiber relaxes and returns to OG length
STEPS FOR MUSCLE CONTRACTION HERE
1) Excitation (review those steps)
2) voltage gradient travels down t-tubule
3) calcium released into the sarcoplasm and binds to troponin
4) tropomyosin pulls away (allowing myosin + actin to interact) = overlapping
5) they STAY stuck together until an ATP molecule attaches
STEPS FOR RELAXATION HERE
1) remove calcium, separate acetylcholine= causes a stop
diffusion
acetylcholinesterase breaks it up
2) pulls calcium ions back into the cisterna = pulls away from troponin
3) causes tropomyosin to block the active sites again
Length-Tension Relationship
about of tennis generated by a muscle depends on how much its stretched/shortened before it was stimulated
-optimal resting length = a small overlap to allow for maximum force produced during contraction
Rigor Mortis
= hardening of the muscles + stiffening of the body 3-4 hours after death
muscles contract (sarcoplasmic reticulum decays releasing calcium into the cytosol and activates the myosin-actin overlapping) but no relax because there is no ATP generated to cause relaxation
fibers remain contracted until myofilaments decay
peaks about 12 hours after death then tapers over the next 48-60 hours
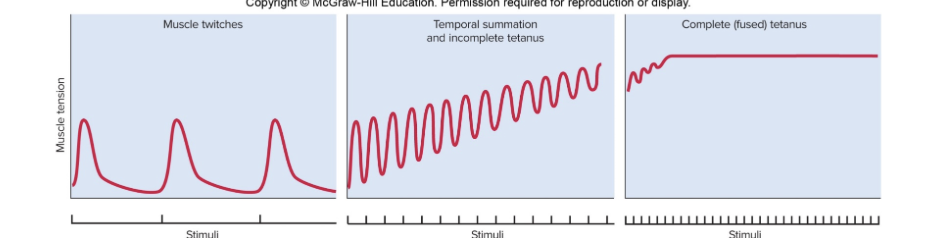
Myogram
a chart of the timing and strength of a muscles contraction
Threshold
minimum voltage necessary to generate an action potential in the muscle fiber and produce a contraction
if below threshold = no contraction
Twitch
a quick cycle of contraction/relaxation when stimulus is at a threshold or higher
Latent Period
the delay between stimulus and contraction (the time required for excitation + internall tension)
contraction phase
time when the muscle generates external tension (force can overcome the load = movement)
relaxation phase
time when tension declines to baseline
longer than contraction
SR reabsorbs calcium, myosin and actin detach from each other
the phases of contraction
1) latent period
2) contraction phase
Isometric phase- tension rises but length no change
tension overcomes resistance of the load = stops increasing
isotonic phase - muscle shortens and moves load
3) relaxation phase
What can change contraction strength
muscles starting length
fatigue after continual use
warmer muscles enzymes can speed up process
hydration levels
higher voltages = stronger contractions
if a muscle is stimulated by a higher voltage…
there is a stronger contraction due to more nerve fibers being excited = more motor units contracted
Difference between frequencies in contraction strength
low frequency stimuli = identical twitches
higher frequency stimuli = temporal (wave) summation creating higher tension as it goes (fluttering)
unnaturally high frequency stimuli = steady contraction called complete (fused) tetanus
Isometric contraction
apart of contraction phase
= “same length”
trying to push something you can’t move
the external resistance causes the muscle to stay the same length
POSTURE MUSCLES
Isotonic contraction
apart of contraction phase
= “same tension”
muscles change in length but not in tension
Concentric contraction = muscle shortens as it maintains tensions (ex: lifting weight)
Eccentric contraction = muscle lengths as it maintains tension (ex: slowly lowering weight)
ATP sources
-ALL muscle contraction depends on ATP
1) Anaerobic fermentation
2) Aerobic respiration
Anaerobic fermentation
atp source for muscle contraction
making ATP and lactate with NO OXYGEN
Aerobic respiration
atp source for muscle contraction
makes WAY MORE ATP
NO lactate made
REQURES OXYGEN
How is energy used in short exercises/sprints? (about 6 seconds worth)
-oxygen briefly supplied by myoglobin but gone FAST
-muscle meets ATP demand by borrowing phosphate groups from other molecules and sending them to ADP, controlled by:
myokinase = transfers phosphate from one ADP to another, converting latter to ATP
Creatine Kinase = gets phosphate from phosphate storage molecule creatine phosphate and gives it to the ADP to make ATP
-Phosphagen system= combining ATP and CP
myokinase
transfers phosphate from one ADP to another to it can be changed to ATP
used for short term sprint energy
creatine kinase
takes phosphate from phosphate storage molecule, creatine phosphate (CP), and gives it to the ADP to turn into ATP
used for short term sprint energy
Phosphagen system
the combination of ATP and creatine phosphate (CP) that provided nearly all the energy needed for short term sprint activities
How is energy used in short term exercise (after phosphagen system is exhausted)? (30-40 seconds of activity)
-shifts to anaerobic fermentation
-muscles take in glucose from blood + stored glycogen to then do glycolysis and get TWO ATP for ONE glucose molecule + turning glucose into lactate (glycogen-lactate system)
-up until anaerobic threshold
Anaerobic threshold
lactate threshold
point when lactate becomes detectable in the blood
glycogen-lactate system
turning glycogen into lactate until it reaches the anaerobic threshold
how is energy used in long term exercise? (after 40 seconds)
-rely on respiratory and cardiovascular systems to deliver oxygen fast enough for aerobic respiration to meet demands
-aerobic respiration = THIRTY ATP for ONE glucose
after 3-4 minutes: oxygen consumption levels off and aerobic ATP meets demands
30 minutes: energy from glucose AND FATTY ACIDS
after 30 minutes: primarily fatty acids because glucose is gone
Muscle Fatigue
weakness from prolonged use of muscles
cause in high intensity:
potassium build up in T tubes reducing excitability
Excess ADP and Potassium inhibits calcium release and decrease force production from myofibrils
cause in low intensity:
fuel loss
electrolyte loss (in sweat)
central fatigue (less motor signals from brain)
both? psychological will to persevere
Central Fatigue
less motor signals coming from the brain
Brian cells inhibited by exercising muscles releasing ammonia
VO2 Max
maximum oxygen uptake
ones ability to maintain high intensity exercise for more than 4-5 minutes
the point at which the rate of oxygen flat lines and doesn’t increase anymore
Excess PostExercise Oxygen Consumption (EPOC)
oxygen debt
difference between elevated rate of oxygen consumption after exercising and the usual resting rate
WHY? needed to replenish ATP, replenish oxygen reserves, get rid of lactate, provide oxygen to the cells
Physiological Classes of Muscle Fibers
1) Slow twitch, slow oxidative (SO), red or type I fibers
2) Fast twitch, fast glycolytic (FG), white or type II fibers
3) Fast twitch, intermediate, type IIA fibers
Slow twitch, slow oxidative (SO), red or type I fibers
-resist fatigue, good for endurance
-use aerobic production
-POSTURE MUSCLES (always contracting muscles)
-lots of mitochondria
-lots of myoglobin = red color
-contain myosin type w slow ATPase + SR that relate calcium SLOW
-for PRECISE movement
-THIN fibers
Fast twitch, fast glycolytic (FG), white or type II fibers
-for quick responses and POWERFUL muscles/movement
-lack of myoglobin = white color
-contain myosin type w fast ATPase and a large SR that releases calcium FAST
-uses glycolysis and anaerobic fermentation for energy
-THICK fibers
Fast twitch, intermediate, type IIA fibers
-fast twitch but fatigue resistant
-RARE in humans
Muscular strength depends on:
muscle size = bigger muscle = more cross bridges + area
fascicle arrangement = pennate stronger than parallel, stronger than circular
size of active motor units = larger motor unit= larger contraction
multiple motor unit summation = more units together = more tension
Temporal summation = greater frequency of stimulation = stronger contraction
length-tension relationship = optimal length is better than over contracted/stretched
fatigue = more fatigued = weaker contraction
Resistance Training
ex: weightlifting
-contraction of a muscle against a load that resists movement
-stimulates muscle growth + cellular enlargement
Endurance training
ex: aerobic exercises
-improve fatigue resistant muscles
-improves skeletal strength
-enhancing the function of the cardiovascular, respiratory, and nervous systems
Peristalsis
waves of contraction brought by food movement in digestive system
stress-relaxation response
helps hollow organs gradually refill (ex: urinary bladder)
no sloshing around
What muscle contracts forcefully even when greatly stretched?
smooth muscle
why? allows hollow organs like the stomach and bladder to fill and then expel their contents correctly
plasticity
the ability to adjust the tension based on how stretched it is
ex: bladder gets greatly stretched but does not become flabby when empty
Muscular Dystrophy
hereditary diseases where skeletal muscles degenerate and weaken then replaced with fat and scar tissue
Duchenne Muscular Dystrophy
cause: sex linked recessive trait (MALES)
mutation in gene for the muscle protein dystrophin = sarcomere (inside) contracts but not the sarcolemma (outside) = cell death
rarely live past 20 years
Fascioscapulohumeral MD
autosomal dominant trait in both sexes
facial and shoulder muscles dystrophy (upper body)
Limb-girdle dystrophy
combo of several diseases
shoulder, arm, pelvic muscles dystrophy
Senescence of muscular system
-replacement of muscle with fat
-fast-twitch fibers earliest on and most severe atrophy
cause? fibers have less stuff to support them, fewer motor neurons in spinal chord, sympathetic nervous system is less efficient so less efficient blood flow (fatigue and more scar tissue)