MOORES CH.8 HEAD
1/380
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
381 Terms
Ch.8 is used for
Superficial Face & Scalp
know which one is which.
OVERVIEW OF HEAD
The head is the superior part of the body that is attached to the trunk by the neck. It is the control and communications center as well as the “loading dock” for the body. The head houses the brain; therefore, it is the site of our consciousness: ideas, creativity, imagination, responses, decision making, and memory. The head also includes special sensory receivers (eyes, ears, mouth, and nose), broadcast devices for voice and expression, and portals for the intake of fuel (food), water, and oxygen and the exhaust of carbon dioxide.
The head consists of the brain and its protective coverings (cranial vault and meninges), the ears, and the face. The face includes openings and passageways, with lubricating glands and valves (seals) to close some of them, the masticatory (chewing) devices, and the orbits that house the visual apparatus. The face also provides our identity as individuals. Disease, malformation, and trauma of structures in the head form the bases of many specialties, including dentistry, maxillofacial surgery, neurology, neuroradiology, neurosurgery, ophthalmology, oral surgery, otology, rhinology, and psychiatry
CRANIUM
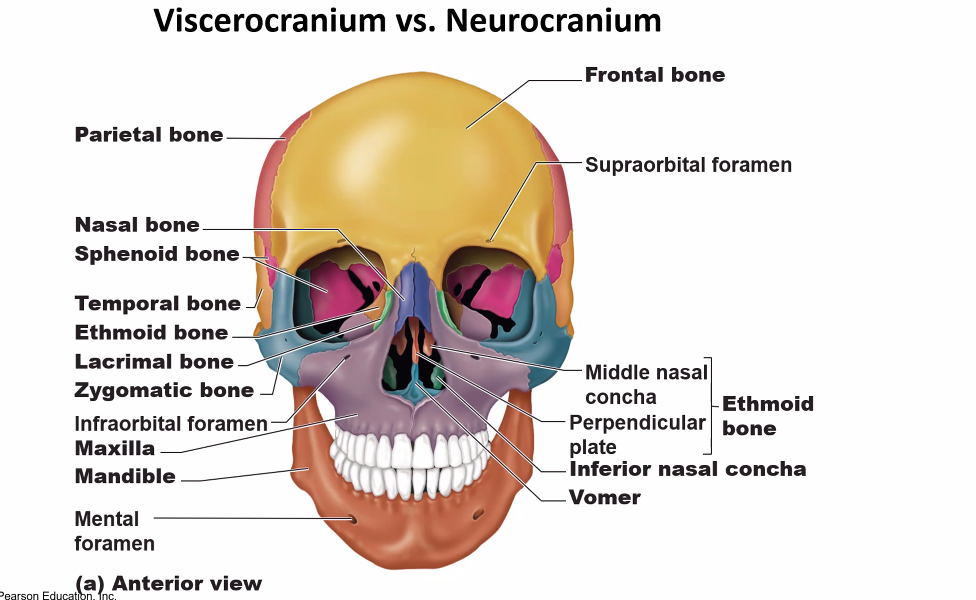
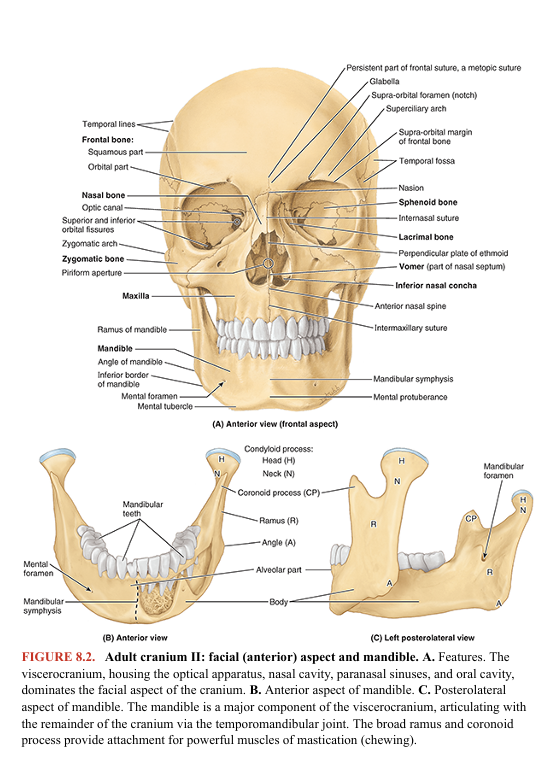
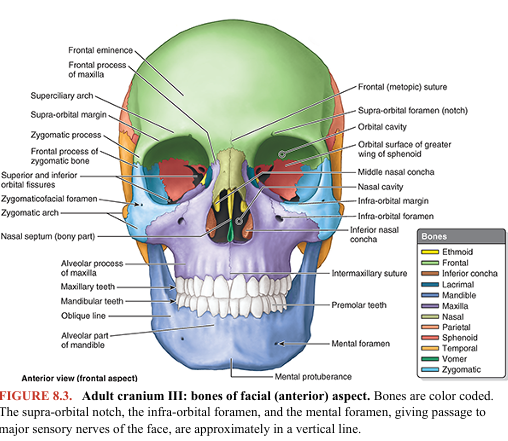
The cranium (skull1) is the skeleton of the head (Fig. 8.1A). It is composed of 22 named bones. A series of bones form its two parts, the neurocranium and viscerocranium (Fig. 8.1B). The neurocranium is the bony case of the brain and its membranous coverings, the cranial meninges. It also contains proximal parts of the cranial nerves and the vasculature of the brain. The neurocranium in adults is formed by a series of eight bones: four singular bones centered on the midline (frontal, ethmoidal, sphenoidal, and occipital), and two sets of bones occurring as bilateral pairs (temporal and parietal) (Figs. 8.1A, 8.2A, and 8.3)

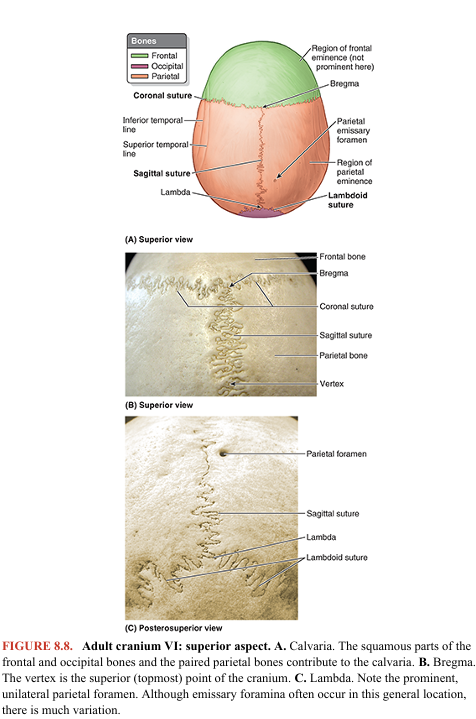
The neurocranium has a dome-like roof, the calvaria (skullcap), and a floor or cranial base (basicranium). The bones forming the calvaria are primarily flat bones (frontal, parietal, and occipital; see Fig. 8.8A) formed by intramembranous ossification of head mesenchyme from the neural crest. These “flat bones” and flat portions of the bones forming the neurocranium are actually curved, with convex external and concave internal surfaces. The bones contributing to the cranial base are primarily irregular bones with substantial flat portions (sphenoidal and temporal) formed by endochondral ossification of cartilage (chondrocranium) or from more than one type of ossification. The ethmoid bone is an irregular bone that makes a relatively minor midline contribution to the neurocranium (see Fig. 8.12A) but is primarily part of the viscerocranium (Figs. 8.2A and 8.3).
Most calvarial bones are united by fibrous interlocking sutures (Fig. 8.1A, B; also see Chapter 1, Overview and Basic Concepts); however, during childhood, some bones (sphenoid and occipital) are united by hyaline cartilage (synchondroses—cartilaginous joints). The spinal cord is continuous with the brain through the foramen magnum, a large opening in the cranial base (Fig. 8.1C).
The viscerocranium (facial skeleton) comprises the facial bones that mainly develop in the mesenchyme of the embryonic pharyngeal arches (Moore et al., 2020). The viscerocranium forms the anterior part of the cranium, and it consists of the bones surrounding the mouth (upper and lower jaws), nose/nasal cavity, and most of the orbits (eye sockets or orbital cavities) (Figs. 8.2 and 8.3).
The viscerocranium consists of 15 irregular bones: 3 singular bones centered on or lying in the midline (mandible, ethmoid, and vomer) and 6 bones occurring as bilateral pairs (maxillae; inferior nasal conchae; and zygomatic, palatine, nasal, and lacrimal bones) (Figs. 8.1A and 8.4A). The maxillae and mandible house the teeth, that is, they provide the sockets and supporting bone for the maxillary and mandibular teeth. The maxillae contribute the greatest part of the upper facial skeleton, forming the skeleton of the upper jaw, which is fixed to the cranial base. The mandible forms the skeleton of the lower jaw, which is movable because it articulates with the cranial base at the temporomandibular joints (Figs. 8.1A and 8.2).
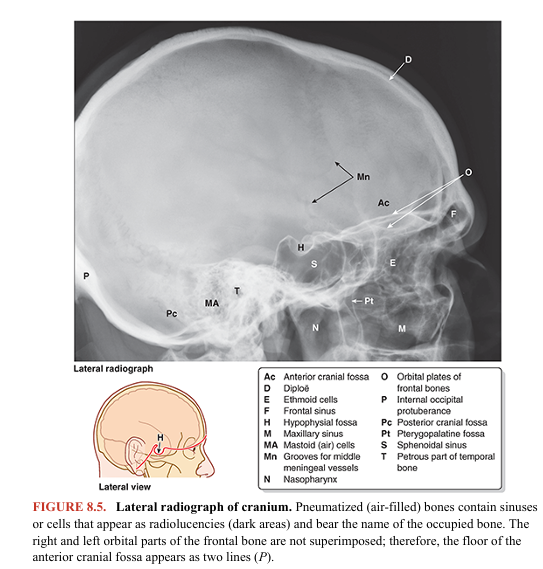
Several bones of the cranium (frontal, temporal, sphenoid, and ethmoid bones) are pneumatized bones, which contain air spaces (air cells or large sinuses), presumably to decrease their weight (Fig. 8.5). The total volume of the air spaces in these bones increases with age.
In the anatomical position, the cranium is oriented so that the inferior margin of the orbit and the superior margin of the external acoustic opening of the external acoustic meatus of both sides lie in the same horizontal plane (Fig. 8.1A). This standard craniometric reference is the orbitomeatal plane (Frankfort horizontal plane).
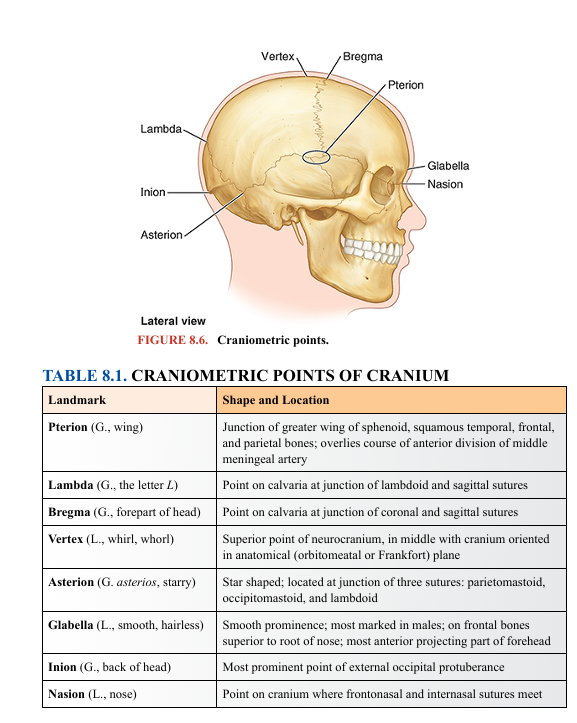
Anterior Aspect of Cranium
Features of the anterior (frontal or facial) aspect of the cranium are the frontal and zygomatic bones, orbits, nasal region, maxillae, and mandible (Figs. 8.2 and 8.3). The frontal bone, specifically its squamous (flat) part, forms the skeleton of the forehead, articulating inferiorly with the nasal and zygomatic bones. In some adults, a frontal suture persists; this remnant is called a metopic suture. It is in the middle glabella, the smooth, slightly depressed area between the superciliary arches. The frontal suture divides the frontal bones of the fetal cranium (see the Clinical Box “Development of Cranium” in this chapter). The intersection of the frontal and nasal bones is the nasion (L. nasus, nose), which in most people is related to a distinctly depressed area (bridge of the nose) (Figs. 8.1A and 8.2A). The nasion is one of many craniometric points that are used radiographically in medicine (or on dry crania in physical anthropology) to make cranial measurements, compare and describe the topography of the cranium, and document abnormal variations (Fig. 8.6; Table 8.1). The frontal bone also articulates with the lacrimal, ethmoid, and sphenoid bones; a horizontal portion of bone (orbital part) forms both the roof of the orbit and part of the floor of the anterior part of the cranial cavity (Fig. 8.3)
The supra-orbital margin of the frontal bone, the angular boundary between the squamous and orbital parts, has a supra-orbital foramen (notch) in some crania for passage of the supra-orbital nerve and vessels. Just superior to the supra-orbital margin is a ridge, the superciliary arch, that extends laterally on each side from the glabella. The prominence of this ridge, deep to the eyebrows, is generally greater in males (Figs. 8.2A and 8.3).
The zygomatic bones (cheek bones, malar bones), forming the prominences of the cheeks, lie on the inferolateral sides of the orbits and rest on the maxillae. The anterolateral rims, walls, floor, and much of the infra orbital margins of the orbits are formed by these quadrilateral bones. A small zygomaticofacial foramen pierces the lateral aspect of each bone (Figs. 8.3 and 8.4A). The zygomatic bones articulate with the frontal, sphenoid, and temporal bones and the maxillae.
Inferior to the nasal bones is the pear-shaped piriform aperture, the anterior nasal opening in the cranium (Figs. 8.1A and 8.2A). The bony nasal septum can be observed through this aperture, dividing the nasal cavity into right and left parts. On the lateral wall of each nasal cavity are curved bony plates, the nasal conchae (Figs. 8.2A and 8.3).
The maxillae form the upper jaw. Their alveolar processes include the tooth sockets (alveoli) and constitute the supporting bone for the maxillary teeth. The two maxillae are united at the intermaxillary suture in the median plane (Fig. 8.2A). The maxillae surround most of the piriform aperture and form the infra-orbital margins medially. They have a broad connection with the zygomatic bones laterally and an infra-orbital foramen inferior to each orbit for passage of the infra-orbital nerve and vessels (Fig. 8.3).
The mandible is a U-shaped bone with an alveolar part that supports the mandibular teeth. It consists of a horizontal part, the body, and a vertical part, the ramus (Fig. 8.2B, C). Inferior to the second premolar teeth are the mental foramina for the mental nerves and vessels (Figs. 8.1A; 8.2A, B; and 8.3). The mental protuberance, forming the prominence of the chin, is a triangular bony elevation inferior to the mandibular symphysis (L. symphysis menti), the osseous union where the halves of the infantile mandible fuse (Fig. 8.2A, B; see Fig. B8.6A)
Lateral Aspect of Cranium
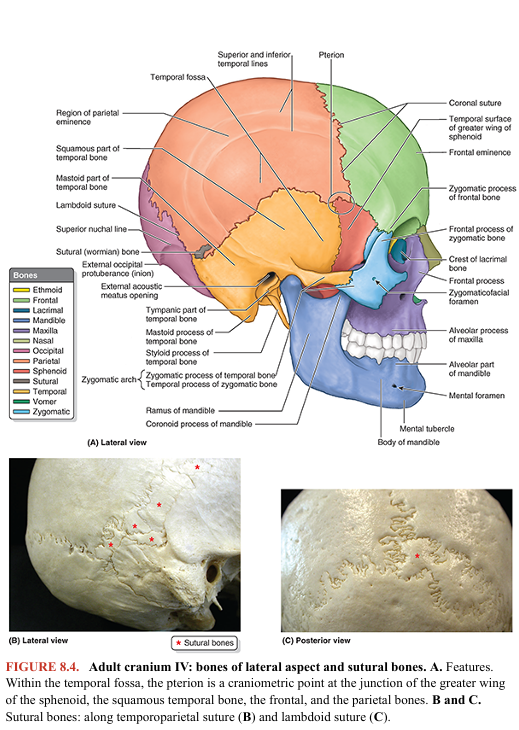
The lateral aspect of the cranium is formed by both neurocranium and viscerocranium (Figs. 8.1A, B and 8.4A). The main features of the neurocranial part are the temporal fossa, the external acoustic meatus opening, and the mastoid process of the temporal bone. The main features of the viscerocranial part are the infratemporal fossa, zygomatic arch, and lateral aspects of the maxilla and mandible.
The temporal fossa is bounded superiorly and posteriorly by the superior and inferior temporal lines, anteriorly by the frontal and zygomatic bones, and inferiorly by the zygomatic arch (Figs. 8.1A and 8.4A). The superior border of this arch corresponds to the inferior limit of the cerebral hemisphere of the brain. The zygomatic arch is formed by the union of the temporal process of the zygomatic bone and the zygomatic process of the temporal bone.
In the anterior part of the temporal fossa, 3–4 cm superior to the midpoint of the zygomatic arch, there is a clinically important area of bone junctions: the pterion (G. pteron, wing) (Figs. 8.4A and 8.6; Table 8.1). It is usually indicated by an H-shaped formation of sutures that unite the frontal, parietal, sphenoid (greater wing), and temporal bones. Less commonly, the frontal and temporal bones articulate. Sometimes all four bones meet at a point.
The external acoustic meatus opening (pore) is the entrance to the external acoustic meatus (canal), which leads to the tympanic membrane (eardrum) (Fig. 8.4A). The mastoid process of the temporal bone is postero inferior to the external acoustic meatus opening. Anteromedial to the mastoid process is the styloid process of the temporal bone, a slender needle-like, pointed projection. The infratemporal fossa is an irregular space inferior and deep to the zygomatic arch and mandible and posterior to the maxilla (see Fig. 8.69B).
Occipital Aspect of Cranium
The posterior or occipital aspect of the cranium is composed of the occiput (L., back of head, the convex posterior protuberance of the squamous part of the occipital bone), parts of the parietal bones, and mastoid parts of the temporal bones (Fig. 8.7A).
The external occipital protuberance is usually easily palpable in the median plane. However, occasionally (especially in females), it may be inconspicuous. A craniometric point defined by the tip of the external protuberance is the inion (G., nape of neck) (Figs. 8.1A, 8.4A, and 8.6; Table 8.1). The external occipital crest descends from the external protuberance toward the foramen magnum, the large opening in the basal part of the occipital bone (Figs. 8.1C and 8.7A; see Fig. 8.9).
The superior nuchal line, marking the superior limit of the neck, extends laterally from each side of the external protuberance. The inferior nuchal line is less distinct. In the center of the occiput, lambda indicates the junction of the sagittal and the lambdoid sutures (Figs. 8.1A, 8.6, and 8.7A; Table 8.1). Lambda can sometimes be felt as a depression. One or more sutural bones (accessory or wormian bones) may be located at lambda or near the mastoid process (Fig. 8.4B, C).
Superior Aspect of Cranium
The superior (vertical) aspect of the cranium, usually somewhat oval in form, broadens posterolaterally at the parietal eminences (Fig. 8.8A). In some people, frontal eminences are also visible, giving the calvaria a somewhat square appearance.
The coronal suture separates the frontal and parietal bones (Fig. 8.8A, B), the sagittal suture separates the parietal bones, and the lambdoid suture separates the parietal and temporal bones from the occipital bone (Fig. 8.8A, C). Bregma is the craniometric landmark formed by the intersection of the sagittal and coronal sutures (Figs. 8.6 and 8.8A; Table 8.1). Vertex, the most superior point of the calvaria, is near the midpoint of the sagittal suture (Figs. 8.6 and 8.7A).
The parietal foramen is a small, inconstant aperture located posteriorly in the parietal bone near the sagittal suture (Fig. 8.8A, C). Sometimes, paired parietal foramina are present. Most irregular, highly variable foramina that occur in the neurocranium are emissary foramina that transmit emissary veins connecting scalp veins to the venous sinuses of the dura mater (see “Scalp” in this chapter).
External Surface of Cranial Base
The cranial base (basicranium) is the inferior portion of the neurocranium (floor of the cranial cavity) and viscerocranium minus the mandible (Fig. 8.9). The external surface of the cranial base features the alveolar arch of the maxillae (the free border of the alveolar processes surrounding and supporting the maxillary teeth); the palatine processes of the maxillae; and the palatine, sphenoid, vomer, temporal, and occipital bones.
The hard palate (bony palate) is formed by the palatal processes of the maxillae anteriorly and the horizontal plates of the palatine bones posteriorly. The free posterior border of the hard palate projects posteriorly in the median plane as the posterior nasal spine. Posterior to the central incisor teeth is the incisive fossa, a depression in the midline of the bony palate into which the incisive canals open.
The right and left nasopalatine nerves pass from the nose through a variable number of incisive canals and foramina (they may be bilateral or merged into a single formation). Posterolaterally are the greater and lesser palatine foramina. Superior to the posterior edge of the palate are two large openings: the choanae (posterior nasal apertures), which are separated from each other by the vomer (L., plowshare), a flat unpaired bone of trapezoidal shape that forms a major part of the bony nasal septum (Fig. 8.9B).
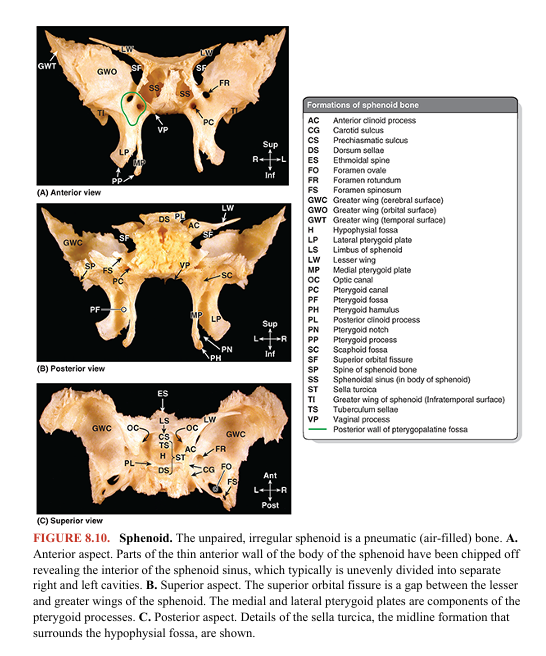
Wedged between the frontal, temporal, and occipital bones is the sphenoid (L., winged; pterygoid is an often-used synonym for sphenoid), an irregular unpaired bone that consists of a body and three pairs of processes: greater wings, lesser wings, and pterygoid processes (Fig. 8.10). The greater and lesser wings of the sphenoid spread laterally from the lateral aspects of the body of the sphenoid. The greater wings have orbital, temporal, and infratemporal surfaces apparent in facial, lateral, and inferior views of the exterior of the cranium (Figs. 8.3, 8.4A, and 8.9A). Their cerebral surfaces are seen in internal views of the cranial base (Fig. 8.11). The pterygoid processes, consisting of lateral and medial pterygoid plates, extend inferiorly on each side of the sphenoid from the junction of the body and greater wings (Figs. 8.9A and 8.10A, B).
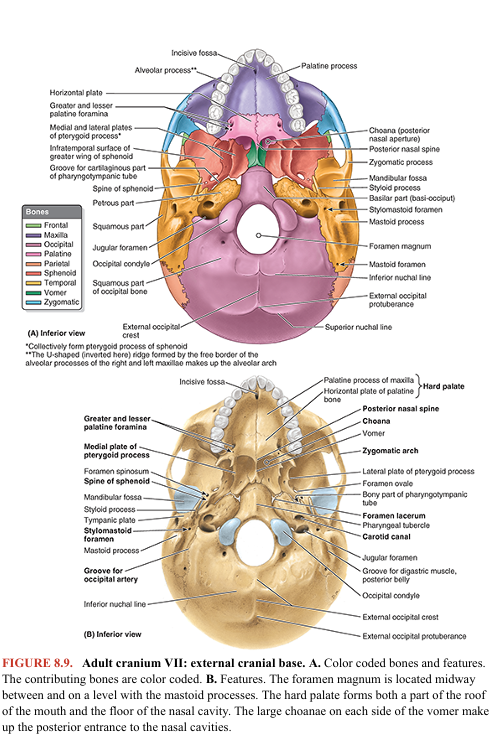

The groove for the cartilaginous part of the pharyngotympanic (auditory) tube lies medial to the spine of the sphenoid, inferior to the junction of the greater wing of the sphenoid and the petrous (L., rock-like) part of the temporal bone (Fig. 8.9B). Depressions in the squamous (L., flat) part of the temporal bone, called the mandibular fossae, accommodate the mandibular condyles when the mouth is closed. The occipital bone articulates with the sphenoid anteriorly, forming the posterior part of the cranial base. The four parts of the occipital bone are arranged around the foramen magnum, the most conspicuous feature of the cranial base. The major structures passing through this large foramen are the spinal cord (where it becomes continuous with the medulla oblongata of the brain), the meninges (coverings) of the brain and spinal cord, the vertebral arteries, the anterior and posterior spinal arteries, and the spinal accessory nerve (CN XI). On the lateral parts of the occipital bone are two large protuberances, the occipital condyles, by which the cranium articulates with the vertebral column. The large opening between the occipital bone and the petrous part of the temporal bone is the jugular foramen, from which the internal jugular vein (IJV) and several cranial nerves (CN IX–CN XI) emerge from the cranium (Figs. 8.9A and 8.11; Table 8.2). The entrance to the carotid canal for the internal carotid artery is just anterior to the jugular foramen (Fig. 8.9B). The mastoid processes provide for muscle attachments. The stylomastoid foramen, transmitting the facial nerve (CN VII) and stylomastoid artery, lies posterior to the base of the styloid process.
Internal Surface of Cranial Base
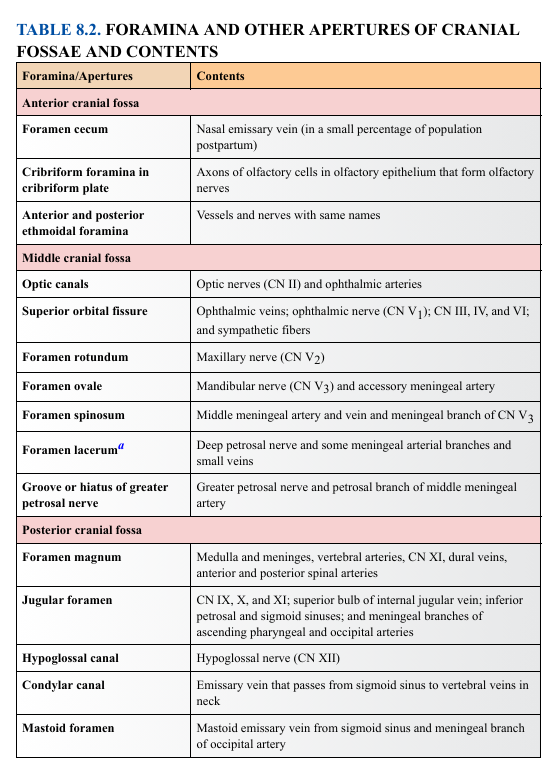
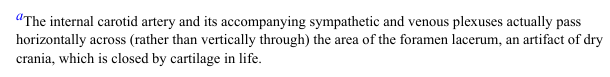
The internal surface of the cranial base (L. basis cranii interna) has three large depressions that lie at different levels: the anterior, middle, and posterior cranial fossae, which form the bowl-shaped floor of the cranial cavity, the space enclosed within the neurocranium occupied by the brain (Fig. 8.12). The anterior cranial fossa is at the highest level, and the posterior cranial fossa is at the lowest level.
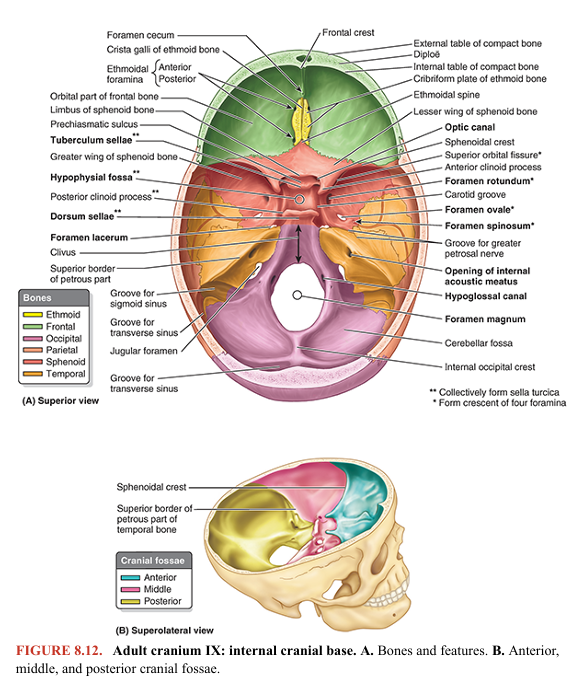
ANTERIOR CRANIAL FOSSA
The inferior and anterior parts of the frontal lobes of the brain occupy the anterior cranial fossa, the shallowest of the three cranial fossae (Fig. 8.12B). The fossa is formed by the frontal bone anteriorly, the ethmoid bone in the middle, and the body and lesser wings of the sphenoid posteriorly. The greater part of the fossa is formed by the orbital parts of the frontal bone, which support the frontal lobes of the brain and form the roofs of the orbits. This surface shows sinuous impressions (brain markings) of the orbital gyri (ridges) of the frontal lobes (Fig. 8.11).
The frontal crest is a median bony extension of the frontal bone (Fig. 8.12A). At its base is the foramen cecum of the frontal bone, which accommodates a diverticulum of dura mater during fetal development, and conducts a small vein in some people, but is generally insignificant postnatally. The crista galli (L., cock’s comb) is a thick, median ridge of bone posterior to the foramen cecum, which projects superiorly from the ethmoid. On each side of this ridge is the sieve-like cribriform plate of ethmoid bone. Its numerous tiny foramina transmit the olfactory nerves (CN I) from the olfactory areas of the nasal cavities to the olfactory bulbs of the brain, which lie on this plate (Fig. 8.12A; Table 8.2).
MIDDLE CRANIAL FOSSA
The butterfly-shaped middle cranial fossa has a central part composed of the sella turcica on the body of the sphenoid and large, depressed lateral parts on each side (Fig. 8.12). The middle cranial fossa is postero-inferior to the anterior cranial fossa, separated from it by the sharp sphenoidal crests laterally and the limbus of the sphenoid centrally. A variably prominent ridge, the limbus of the sphenoid forms the anterior boundary of the transversely oriented prechiasmatic sulcus extending between the right and the left optic canals. The sphenoidal crests are formed mostly by the sharp posterior borders of the lesser wings of the sphenoid bones, which overhang the lateral parts of the fossae anteriorly. The sphenoidal crests end medially in two sharp bony projections, the anterior clinoid processes. The bones forming the lateral parts of the fossa are the greater wings of the sphenoid, the squamous parts of the temporal bones laterally, and the petrous parts of the temporal bones posteriorly. The lateral parts of the middle cranial fossa support the temporal lobes of the brain. The boundary between the middle and the posterior cranial fossae is the superior border (crest) of the petrous part of the temporal bone laterally and a flat plate of bone, the dorsum sellae of the sphenoid, medially. The sella turcica (L., Turkish saddle) is the saddle-like bony formation on the upper surface of the body of the sphenoid, which is surrounded by the anterior and posterior clinoid processes (Figs. 8.10C and 8.12A). Clinoid means “bedpost,” and the four processes (two anterior and two posterior) surround the hypophysial fossa, the “bed” of the pituitary gland, like the posts of a four-poster bed. The sella turcica is composed of three parts: 1. The tuberculum sellae (horn of saddle): a variable slight to prominent median elevation forming the posterior boundary of the prechiasmatic sulcus and the anterior boundary of the hypophysial fossa 2. The hypophysial fossa (pituitary fossa): a median depression (seat of saddle) in the body of the sphenoid that accommodates the pituitary gland (L. hypophysis) 3. The dorsum sellae (back of saddle): a square plate of bone projecting superiorly from the body of the sphenoid. It forms the posterior boundary of the sella turcica, and its prominent superolateral angles make up the posterior clinoid processes.
On each side of the body of the sphenoid, a crescent of four foramina perforates the roots of the cerebral surfaces of the greater wings of the sphenoid (Figs. 8.10C, 8.11, and 8.12A); structures transmitted by the foramina are listed in Table 8.2: 1. Superior orbital fissure: Located between the greater and the lesser wings, it opens anteriorly into the orbit (Fig. 8.2A). 2. Foramen rotundum (round foramen): Located posterior to the medial end of the superior orbital fissure, it runs a horizontal course to an opening on the anterior aspect of the root of the greater wing of the sphenoid (Figs. 8.10A and 8.12A) into a bony formation between the sphenoid, the maxilla, and the palatine bones, the pterygopalatine fossa. 3. Foramen ovale (oval foramen): a large foramen posterolateral to the foramen rotundum; it opens inferiorly into the infratemporal fossa (Fig. 8.9B). 4. Foramen spinosum (spinous foramen): located posterolateral to the foramen ovale and opens into the infratemporal fossa in relationship to the spine of the sphenoid (Fig. 8.11)
The foramen lacerum (lacerated or torn foramen) is not part of the crescent of foramina. This ragged foramen lies posterolateral to the hypophysial fossa and is an artifact of a dried cranium (Fig. 8.12A). In life, it is closed by a cartilage plate. Only some meningeal arterial branches and small veins are transmitted vertically through the cartilage, completely traversing this foramen. The internal carotid artery and its accompanying sympathetic and venous plexuses pass across the superior aspect of the cartilage (i.e., pass over the foramen), and some nerves traverse it horizontally, passing to a foramen in its anterior boundary. Extending posteriorly and laterally from the foramen lacerum is a narrow groove for the greater petrosal nerve on the anterosuperior surface of the petrous part of the temporal bone. There is also a small groove for the lesser petrosal nerve.
POSTERIOR CRANIAL FOSSA
The posterior cranial fossa, the largest and deepest of the three cranial fossae, lodges the cerebellum, pons, and medulla oblongata (Fig. 8.12B). The posterior cranial fossa is formed mostly by the occipital bone, but the dorsum sellae of the sphenoid marks its anterior boundary centrally (Fig. 8.12A), and the petrous and mastoid parts of the temporal bones contribute its anterolateral “walls.” From the dorsum sellae, there is a marked incline, the clivus, in the center of the anterior part of the fossa leading to the foramen magnum. Posterior to this large opening, the posterior cranial fossa is partly divided by the internal occipital crest into bilateral large concave impressions, the cerebellar fossae. The internal occipital crest ends in the internal occipital protuberance formed in relationship to the confluence of the sinuses, a merging of dural venous sinuses. Broad grooves show the horizontal course of the transverse sinus and the S-shaped sigmoid sinus. At the base of the petrous ridge of the temporal bone is the jugular foramen, which transmits several cranial nerves in addition to the sigmoid sinus that exits the cranium as the internal jugular vein (IJV) (Fig. 8.11; Table 8.2). Anterosuperior to the jugular foramen is the internal acoustic meatus for the facial (CN VII) and vestibulocochlear nerves (CN VIII) and the labyrinthine artery. The hypoglossal canal for the hypoglossal nerve (CN XII) is superior to the anterolateral margin of the foramen magnum.
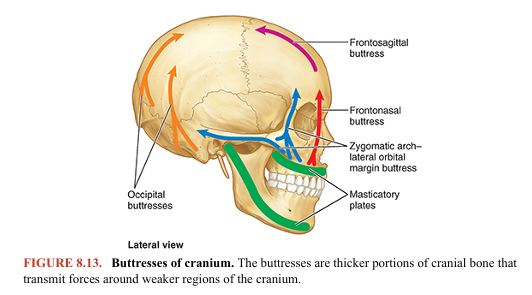
Walls of Cranial Cavity
The walls of the cranial cavity vary in thickness in different regions. They are usually thinner in females than in males and are thinner in children and elderly people. The bones tend to be thinnest in areas that are well covered with muscles, such as the squamous part of the temporal bone (Fig. 8.11). Thin areas of bone can be seen radiographically (Fig. 8.5) or by holding a dried cranium up to a bright light. Most bones of the calvaria consist of internal and external tables of compact bone, separated by diploë (Figs. 8.5 and 8.11). The diploë is cancellous bone containing red bone marrow during life, through which run canals formed by diploic veins. The diploë in a dried calvaria is not red because the protein was removed during preparation of the cranium. The internal table of bone is thinner than the external table, and in some areas, there is only a thin plate of compact bone with no diploë. The bony substance of the cranium is unequally distributed. Relatively thin (but mostly curved) flat bones provide the necessary strength to maintain cavities and protect their contents. However, in addition to housing the brain, the bones of the neurocranium (and processes from them) provide proximal attachment for the strong muscles of mastication that attach distally to the mandible. Consequently, high compressive forces occur across the nasal cavity and orbits that are sandwiched between. Therefore, thickened portions of the cranial bones form stronger pillars or buttresses that transmit forces, bypassing the orbits and nasal cavity (Fig. 8.13). The main buttresses are the frontonasal buttress, extending from the region of the canine teeth between the nasal and the orbital cavities to the central frontal bone, and the zygomatic arch–lateral orbital margin buttress from the region of the molars to the lateral frontal and temporal bones. Similarly, occipital buttresses transmit forces received lateral to the foramen magnum from the vertebral column. Perhaps to compensate for the denser bone required for these buttresses, some areas of the cranium not as mechanically stressed become pneumatized (air filled).
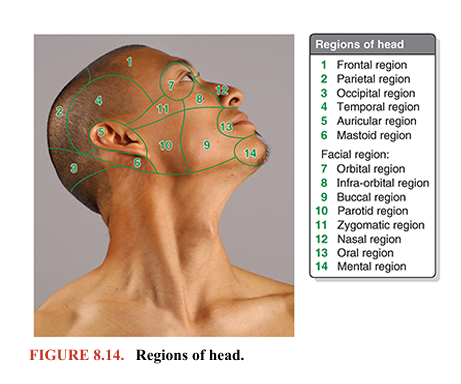
Regions of Head
To allow clear communications regarding the location of structures, injuries, or pathologies, the head is divided into regions (Fig. 8.14). The large number of regions into which the relatively small area of the face is divided (eight) reflects its functional complexity and personal importance, as do annual expenditures for elective aesthetic surgery. Except for the auricular region, which includes the external ear, the names of the regions of the neurocranial portion of the head correspond to the underlying bones or bony features: frontal, parietal, occipital, temporal, and mastoid regions.
The viscerocranial portion of the head includes the facial region, which is divided into five bilateral and three median regions related to superficial features (oral and buccal regions), to deeper soft tissue formations (parotid region), and to skeletal features (orbital, infra-orbital, nasal, zygomatic, and mental regions). The remainder of this chapter discusses several of these regions in detail as well as some deep regions not represented on the surface (e.g., the infratemporal region and pterygopalatine fossa). The surface anatomy of these regions is discussed with the description of each region.
CRANIUM Head Injuries
Head injuries are a major cause of death and disability. The complications of head injuries include hemorrhage, infection, and injury to the brain (e.g., concussion) and cranial nerves. Disturbance in the level of consciousness is the most common symptom of head injury. Almost 10% of all deaths in the United States are caused by injury, and approximately half of traumatic deaths involve the brain (Louis et al., 2022). Head injuries occur mostly in young persons between the ages of 15 and 24 years. The major cause of brain injury varies; however, motor vehicle and motorcycle accidents are prominent. The high energy transmitted during these accidents can cause fiber tracts and axons within the brain to shear, causing a pattern called “diffuse axonal injury” for which there is no good treatment.
Headaches and Facial Pain
Few complaints are more common than headaches and facial pain. Although usually benign and frequently associated with tension, fatigue, or mild fever, headaches may indicate a serious intracranial problem such as a brain tumor, subarachnoid hemorrhage, or meningitis. Neuralgias (G. algos, pain) are characterized by severe throbbing or stabbing pain along the course of a nerve caused by a demyelinating lesion. They are a common cause of facial pain. Terms such as facial neuralgia describe diffuse painful sensations. Localized aches have specific names, such as earache (otalgia) and toothache (odontalgia). A sound knowledge of the clinical anatomy of the head helps in understanding the causes of headaches and facial pain.
Injury to Superciliary Arches
The superciliary arches are relatively sharp bony ridges (see Fig. 8.3). Consequently, a blow to them (e.g., during boxing) may lacerate the skin and cause bleeding. Bruising of the skin surrounding the orbit causes tissue fluid and blood to accumulate in the surrounding connective tissue, which gravitates, usually unilaterally, into the superior (upper) eyelid and around the eye (“black eye”; see Fig. B8.12)
Malar Flush
The zygomatic bone was once called the malar bone; consequently, you are likely to hear the clinical term malar flush. This redness of the skin covering the zygomatic process (malar eminence) is associated with a rise in temperature in various fevers occurring with certain diseases, such as tuberculosis. A characteristic “butterfly rash” is seen over the zygomatic eminence in some cases of systemic lupus erythematosus disease, an autoimmune disease.
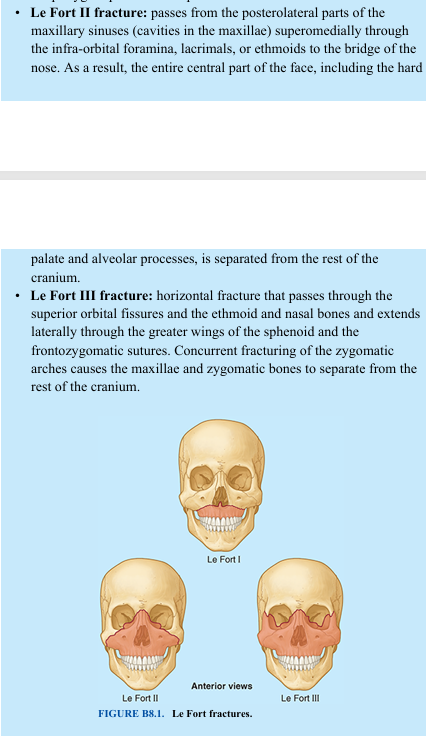
Fractures of Maxillae and Associated Bones
Dr. Léon-Clement Le Fort (a Paris surgeon and gynecologist, 1829–1893) classified three common variants of fractures of the maxillae (Fig. B8.1): • Le Fort I fracture: wide variety of horizontal fractures of the maxillae, passing superior to the maxillary alveolar process (i.e., to the roots of the teeth), crossing the bony nasal septum and possibly the pterygoid plates of the sphenoid • Le Fort II fracture: passes from the posterolateral parts of the maxillary sinuses (cavities in the maxillae) superomedially through the infra-orbital foramina, lacrimals, or ethmoids to the bridge of the nose. As a result, the entire central part of the face, including the hard palate and alveolar processes, is separated from the rest of the cranium. • Le Fort III fracture: horizontal fracture that passes through the superior orbital fissures and the ethmoid and nasal bones and extends laterally through the greater wings of the sphenoid and the frontozygomatic sutures. Concurrent fracturing of the zygomatic arches causes the maxillae and zygomatic bones to separate from the rest of the cranium.
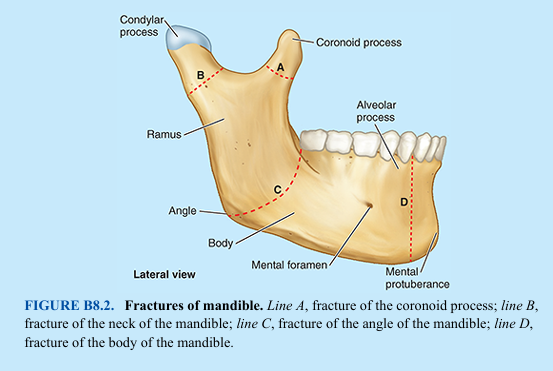
Fractures of Mandible
A broken mandible usually involves two fractures, which frequently occur on opposite sides of the mandible. Therefore, if one fracture is observed, a search should be made for another (e.g., a hard blow to the jaw often fractures the neck and body of the mandible in the region of the opposite canine tooth). Fractures of the coronoid process of the mandible are uncommon and usually single (Fig. B8.2). Fractures of the neck of the mandible are often transverse and may be associated with dislocation of the temporomandibular joint (TMJ) on the same side. Fractures of the angle of the mandible are usually oblique and may involve the bony socket or alveolus of the 3rd molar tooth (Fig. B8.2, line C). Fractures of the body of the mandible frequently pass through the socket of a canine tooth (Fig. B8.2, line D).
Resorption of Alveolar Bone
Extraction of teeth causes the alveolar bone to resorb in the affected region(s) (Fig. B8.3). Following complete loss or extraction of maxillary teeth, the tooth sockets begin to fill in with bone, and the alveolar process begins to resorb. Similarly, extraction of mandibular teeth causes the bone of the alveolar part to resorb. Gradually, the mental foramen comes to lie near the superior border of the body of the mandible (Fig. B8.3A–C). In some cases, the mental foramina disappear, exposing the mental nerves to injury. Pressure from a dental prosthesis (e.g., a denture resting on an exposed mental nerve) may produce pain during eating. Loss of all the teeth results in a decrease in the vertical facial dimension and mandibular prognathism (overclosure). Deep creases in the facial skin also appear that pass posteriorly from the corners of the mouth.

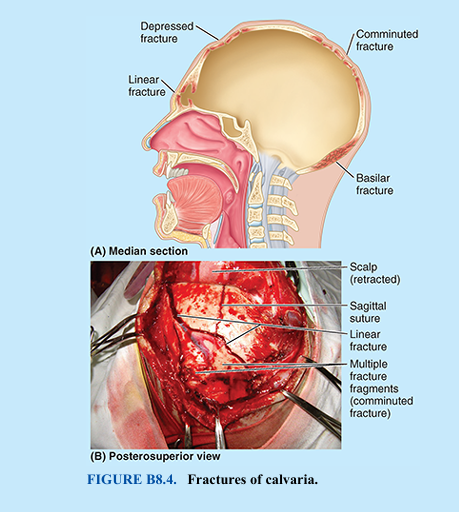
Fractures of Calvaria
The convexity of the calvaria distributes and thereby usually minimizes the effects of a blow to the head. However, hard blows in thin areas of the calvaria are likely to produce depressed fractures, in which a bone fragment is depressed inward, compressing and/or injuring the brain (Fig. B8.4). Linear calvarial fractures, the most frequent type, usually occur at the point of impact, but fracture lines often radiate away from it in two or more directions. In comminuted fractures, the bone is broken into several pieces. If the area of the calvaria is thick at the site of impact, the bone may bend inward without fracturing. However, a fracture may occur some distance from the site of direct trauma where the calvaria is thinner. In a contrecoup (counterblow) fracture, no fracture occurs at the point of impact, but one occurs on the opposite side of the cranium.
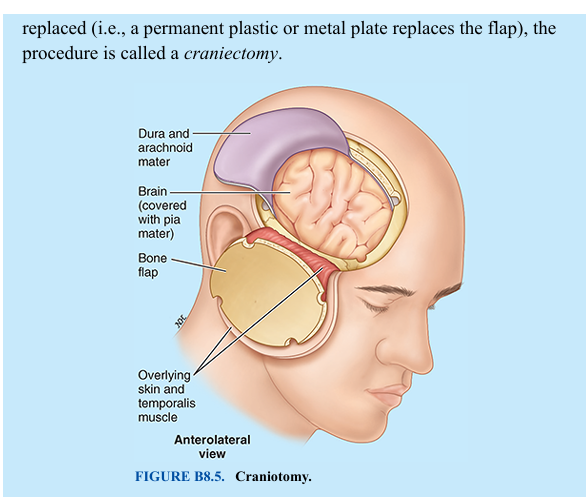
Surgical Access to Cranial Cavity: Bone Flaps
Surgeons access the cranial cavity and brain by performing a craniotomy, in which a section of the neurocranium, called a bone flap, is elevated or removed (Fig. B8.5). Because the adult pericranium (periosteum of cranium) has poor osteogenic (bone forming) properties, little regeneration occurs after bone loss (e.g., when pieces of bone are removed during repair of a comminuted cranial fracture). Surgically produced bone flaps are put back into place and wired to other parts of the calvaria or held in place temporarily with metal plates. Reintegration is most successful when the bone is reflected with its overlying muscle and skin so that it retains its own blood supply during the procedure and after repositioning. If the bone flap is not replaced (i.e., a permanent plastic or metal plate replaces the flap), the procedure is called a craniectomy.
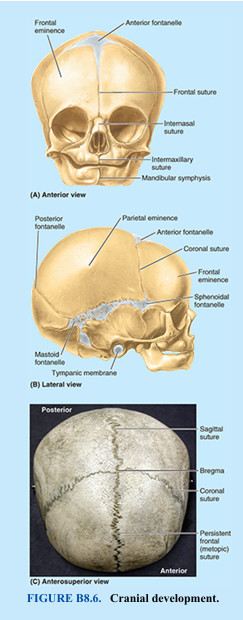
Development of Cranium
The bones of the calvaria and some parts of the cranial base develop by intramembranous ossification. Most parts of the cranial base develop by endochondral ossification. At birth, the bones of the calvaria are smooth and unilaminar; no diploë is present. The frontal and parietal eminences are especially prominent (Fig. B8.6). The cranium of a neonate is disproportionately large compared to other parts of the skeleton; however, the facial aspect is small compared to the calvaria, which forms approximately one eighth of the cranium. In the adult, the facial skeleton forms one third of the cranium. The large size of the calvaria in infants results from precocious growth and development of the brain and eyes.
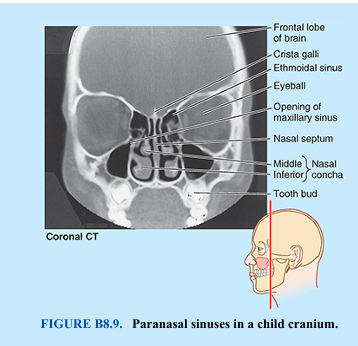
The rudimentary development of the face makes the orbits appear relatively large (Fig. B8.6A). The smallness of the face results from the rudimentary development of the maxillae, mandible, and paranasal sinuses (air-filled bone cavities), the absence of erupted teeth, and the small size of the nasal cavities.
The halves of the frontal bone in the neonate are separated by the frontal suture, the frontal and parietal bones are separated by the coronal suture, and the maxillae and mandibles are separated by the intermaxillary suture and mandibular symphysis (secondary cartilaginous joint), respectively. There are no mastoid and styloid processes (Fig. B8.6A, B). Because there are no mastoid processes at birth, the facial nerves are close to the surface when they emerge from the stylomastoid foramina. Thus, the facial nerves may be injured by forceps during a difficult delivery or later by an incision posterior or inferior to the auricle of the external ear (e.g., for the surgical treatment of mastoiditis or middle ear problems). The mastoid processes form gradually during the 1st year as the sternocleidomastoid muscles complete their development and pull on the petromastoid parts of the temporal bones.
The bones of the calvaria of neonates are separated by fontanelles (fibrous membranes; palpable deep to the scalp, these are perceived as “soft spots”). The largest occur between the angles (corners) of the flat bones (Fig. B8.6A, B). They include the anterior and posterior fontanelles and the paired sphenoidal and mastoid fontanelles. Palpation of the fontanelles during infancy, especially the anterior and posterior ones, enables physicians to determine the following: • Progress of growth of the frontal and parietal bones • Degree of hydration of an infant (a depressed fontanelle indicates dehydration) • Level of intracranial pressure (a bulging fontanelle indicates increased pressure on the brain)
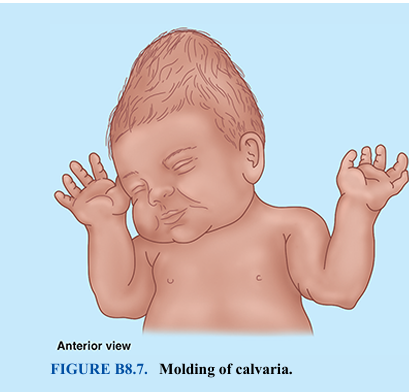
The anterior fontanelle, the largest one, is diamond or star shaped. It is bounded by the halves of the frontal bone anteriorly and the parietal bones posteriorly (Fig. B8.6). Therefore, it is located at the junction of the sagittal, coronal, and frontal sutures, the future site of the bregma (see Fig. 8.6; Table 8.1). By 18 months of age, the surrounding bones have fused, and the anterior fontanelle is no longer clinically palpable. At birth, the frontal bone consists of two halves. Union of the halves begins in the 2nd year. In most cases, the frontal suture is obliterated by the 8th year. However, in approximately 8% of people, a remnant of the frontal suture, the metopic suture, persists (see Figs. 8.2A and 8.3). Much less frequently, the entire suture remains (Fig. B8.6C). A persistent suture must not be interpreted as a fracture in a radiograph or another medical image (e.g., a CT scan). The posterior fontanelle is triangular and bounded by the parietal bones anteriorly and the occipital bone posteriorly. It is located at the junction of the lambdoid and sagittal sutures, the future site of lambda (see Figs. 8.7A and 8.8C). The posterior fontanelle begins to close during the first few months after birth, and by the end of the 1st year, it is small and no longer clinically palpable. The sphenoidal and mastoid fontanelles, overlain by the temporalis muscle (see Fig. 8.16A), fuse during infancy and are less important clinically than the midline fontanelles. The halves of the mandible fuse early in the 2nd year (Fig. B8.6). The two maxillae and nasal bones usually do not fuse. The softness of the cranial bones in fetuses and their loose connections at the sutures and fontanelles enable the shape of the cranium to be molded during birth (Fig. B8.7). During passage of the fetus through the birth canal, the halves of the frontal bone become flat, the occipital bone is drawn out, and one parietal bone slightly overrides the other. Within a few days after birth, the shape of the neonatal cranium returns to normal. The resilience of the cranial bones of infants allows them to resist forces that would produce fractures in adults. The fibrous sutures of the calvaria also permit the cranium to enlarge during infancy and childhood. The increase in the size of the calvaria is greatest during the first 2 years, the period of most rapid brain development. The calvaria normally increases in capacity for 15–16 years. After this, the calvaria usually increases slightly in size for 3–4 years due to bone thickening
Age Changes in Face
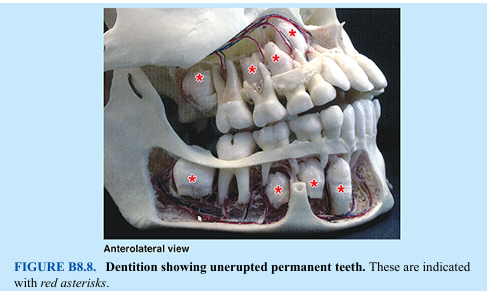
The mandible is the most dynamic of our bones; its size and shape and the number of teeth it normally bears undergo considerable change with age. In the neonate, the mandible consists of two halves united in the median plane by a cartilaginous joint, the mandibular symphysis. Union between the halves of the mandible is affected by means of fibrocartilage. This union begins during the 1st year, and the halves are fused by the end of the 2nd year. The body of the mandible in neonates is a mere shell lacking an alveolar part with each half enclosing five deciduous teeth. These teeth usually begin to erupt in infants at approximately 6 months of age. The body of the mandible elongates, particularly posterior to the mental foramen (Fig. B8.2), to accommodate this development. Later, eight permanent teeth begin to erupt during the 6th year of life (Fig. B8.8). Eruption of the permanent teeth is not complete until early adulthood.
Rapid growth of the face during infancy and early childhood coincides with the eruption of deciduous teeth. Vertical growth of the upper face results mainly from dento-alveolar development of alveolar bone. These changes are more marked after the permanent teeth erupt. Concurrent enlargement of the frontal and facial regions is associated with the increase in the size of the paranasal sinuses, the air-filled extensions of the nasal cavities in certain cranial bones (Fig. B8.9). Most paranasal sinuses are rudimentary or absent at birth. Growth of the paranasal sinuses is important in altering the shape of the face and in adding resonance to the voice
Obliteration of Cranial Sutures
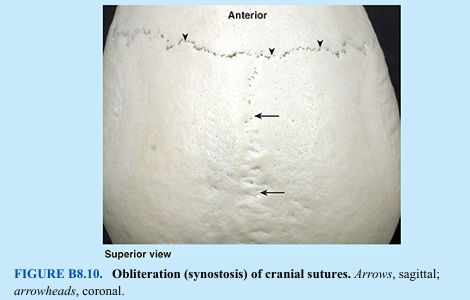
The obliteration of sutures between the bones of the calvaria usually begins between the ages of 30 and 40 years on the internal surface. Approximately 10 years later, the sutures on the external surface obliterate (Fig. B8.10; cf. Fig. 8.8B). Obliteration of sutures usually begins at the bregma and continues sequentially in the sagittal, coronal, and lambdoid sutures. Closure times vary considerably.
Age Changes in Cranium
As people age, the cranial bones normally become progressively thinner and lighter, and the diploë gradually becomes filled with a gray gelatinous material. In these individuals, the bone marrow has lost its blood cells and fat, giving it a gelatinous appearance.
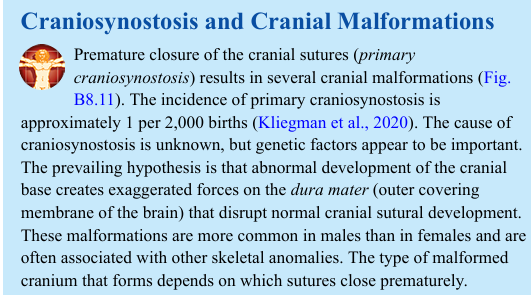
Craniosynostosis and Cranial Malformations
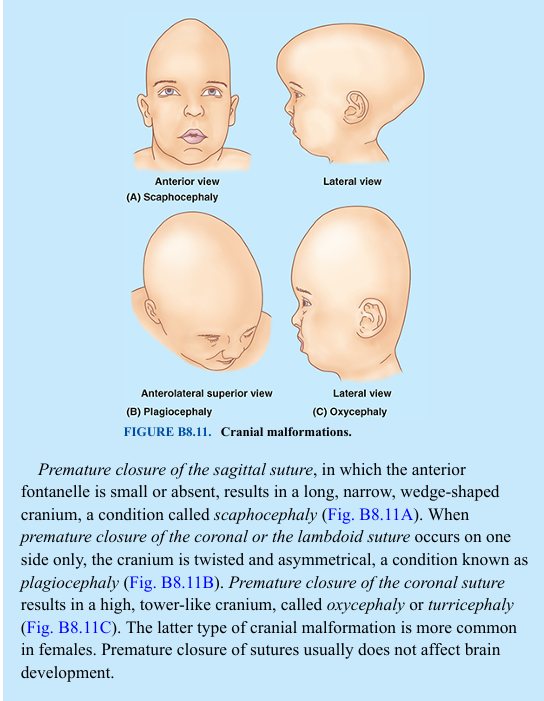
Premature closure of the cranial sutures (primary craniosynostosis) results in several cranial malformations (Fig. B8.11). The incidence of primary craniosynostosis is approximately 1 per 2,000 births (Kliegman et al., 2020). The cause of craniosynostosis is unknown, but genetic factors appear to be important. The prevailing hypothesis is that abnormal development of the cranial base creates exaggerated forces on the dura mater (outer covering membrane of the brain) that disrupt normal cranial sutural development. These malformations are more common in males than in females and are often associated with other skeletal anomalies. The type of malformed cranium that forms depends on which sutures close prematurely.
Premature closure of the sagittal suture, in which the anterior fontanelle is small or absent, results in a long, narrow, wedge-shaped cranium, a condition called scaphocephaly (Fig. B8.11A). When premature closure of the coronal or the lambdoid suture occurs on one side only, the cranium is twisted and asymmetrical, a condition known as plagiocephaly (Fig. B8.11B). Premature closure of the coronal suture results in a high, tower-like cranium, called oxycephaly or turricephaly (Fig. B8.11C). The latter type of cranial malformation is more common in females. Premature closure of sutures usually does not affect brain development.
The Bottom Line: Cranium
The cranium is the skeleton of the head, an amalgamation of functional components united to form a single skeletal formation. ■ The basic functional components include the neurocranium, the container of the brain and internal ears, and viscerocranium, providing paired orbits, nasal cavities, and teeth-bearing plates (alveolar processes) of the oral cavity. ■ Although some mobility between cranial bones is advantageous during birth, they become fixed together by essentially immovable joints (sutures), allowing independent movement of only the mandible. ■ Abundant fissures and foramina facilitate communication and passage of neurovascular structures between functional components. ■ The bony substance of the cranium is unequally distributed. Relatively thin (but mostly curved) flat bones provide the necessary strength to maintain cavities and protect contents. ■ However, the bones and processes of the neurocranium also provide proximal attachment for the strong muscles of mastication (chewing) that attach distally to the mandible. ■ The high compressive forces generated across the nasal cavity and orbits, sandwiched between the muscle attachments, are resisted by thickened portions of the bones forming stronger pillars or buttresses. ■ The mostly superficial surface of the cranium provides both visible and palpable landmarks. Internal features of the cranial base reflect the major formations of the brain that rest on it. ■ Bony ridges radiating from the centrally located sella turcica divide it into three cranial fossae. ■ The frontal lobes of the brain lie in the anterior cranial fossa. ■ The temporal lobes lie in the middle cranial fossa. ■ The hindbrain, consisting of the pons, cerebellum, and medulla, occupies the posterior cranial fossa, with the medulla continuing through the foramen magnum where it is continuous with the spinal cord.
FACE AND SCALP
Face
The face is the anterior aspect of the head from the forehead to the chin and from one ear to the other. The face provides our identity as an individual human. Thus, birth defects, scarring, or other alterations resulting from pathology or trauma have marked consequences beyond their physical effects. The basic shape of the face is determined by the underlying bones. The individuality of the face results primarily from anatomical variations in the shape and relative prominence of the features of the underlying cranium; in the deposition of fatty tissue; in the color and effects of aging on the overlying skin; and in the abundance, nature, and placement of hair on the face and scalp. The relatively large size of the buccal fat-pads in infants prevents collapse of the cheeks during sucking and produces their chubby cheeked appearance. Growth of the facial bones takes longer than those of the calvaria. The ethmoid bone, orbital cavities, and superior parts of the nasal cavities have nearly completed their growth by the 7th year. Expansion of the orbits and growth of the nasal septum carry the maxillae infero-anteriorly. Considerable facial growth occurs during childhood as the paranasal sinuses develop and permanent teeth erupt. The face plays an important role in communication. Our interactions with others take place largely via the face (including the ears) and thus the term interface for a site of interactions. Whereas the shape and features of the face provide our identity, much of our effect on others and their perceptions about us result from the way we use facial muscles to make the slight alterations in the features that constitute facial expression.
Scalp
The scalp consists of skin (normally hair bearing) and subcutaneous tissue that cover the neurocranium from the superior nuchal lines on the occipital bone to the supra-orbital margins of the frontal bone (see Figs. 8.3 and 8.4A). Laterally, the scalp extends over the temporal fascia to the zygomatic arches. The scalp is composed of five layers, the first three of which are connected intimately and move as a unit (e.g., when wrinkling the forehead and moving the scalp). Each letter in the word scalp serves as a memory key for one of its five layers (Fig. 8.15A):
1. Skin: thin, except in the occipital region, contains many sweat and sebaceous glands and hair follicles. It has an abundant arterial supply and good venous and lymphatic drainage. 2. Connective tissue: forms the thick, dense, richly vascularized subcutaneous layer that is well supplied with cutaneous nerves 3. Aponeurosis (epicranial aponeurosis): the broad, strong, tendinous sheet that covers the calvaria and serves as the attachment for muscle bellies converging from the forehead and occiput (occipitofrontalis muscle) (Fig. 8.15B) and from the temporal bones on each side (temporoparietalis and anterior and superior auricular muscles). Collectively, these structures constitute the musculo-aponeurotic epicranius. The frontal belly of the occipitofrontalis pulls the scalp anteriorly, wrinkles the forehead, and elevates the eyebrows. The occipital belly of the occipitofrontalis pulls the scalp posteriorly, smoothing the skin of the forehead. The superior auricular muscle (a specialized posterior part of the temporoparietalis) elevates the auricle of the external ear. All parts of the epicranius (muscle and aponeurosis) are innervated by the facial nerve. 4. Loose areolar tissue: a sponge-like layer including potential spaces that may distend with fluid as a result of injury or infection. This layer allows free movement of the scalp proper (the first three layers—skin, connective tissue, and epicranial aponeurosis) over the underlying calvaria. 5. Pericranium: a dense layer of connective tissue that forms the external periosteum of the neurocranium. It is firmly attached but can be stripped from the crania of living persons, except where the pericranium is continuous with the fibrous tissue in the cranial sutures.

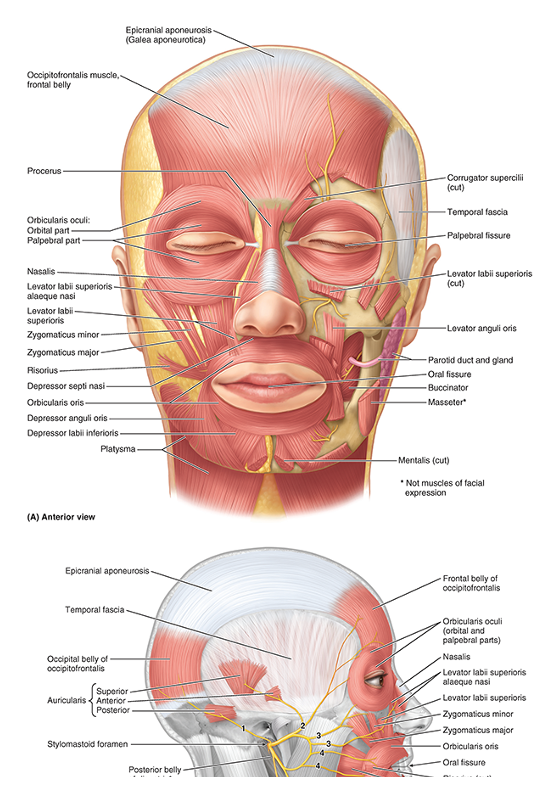
Muscles of Face and Scalp
The facial muscles (muscles of facial expression) are in the subcutaneous tissue of the anterior and posterior scalp, face, and neck. They move the skin and change facial expressions to convey mood. Most muscles attach to bone or fascia and produce their effects by pulling the skin. The muscles of the scalp and face are illustrated in Figure 8.16, and their attachments and actions are provided in Table 8.3. Certain muscles and/or muscle groups are discussed in further detail.
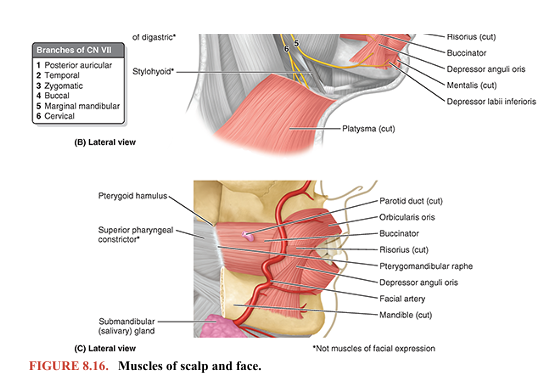
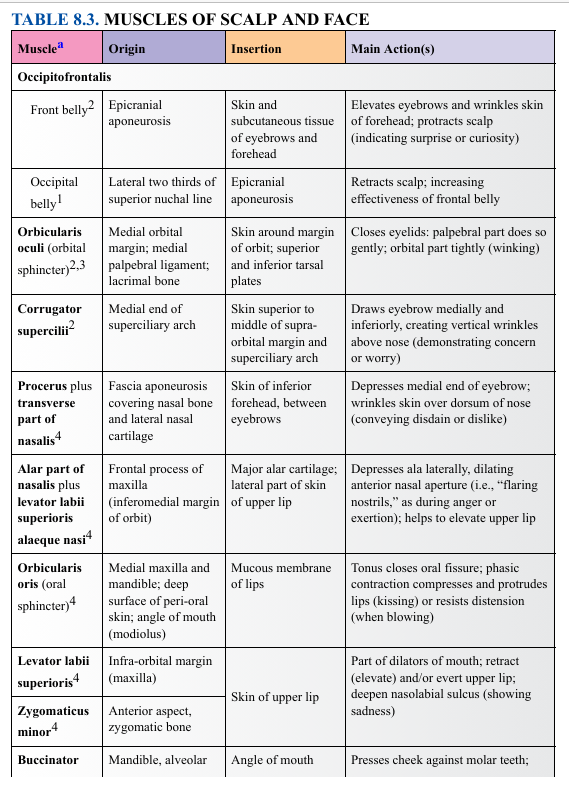
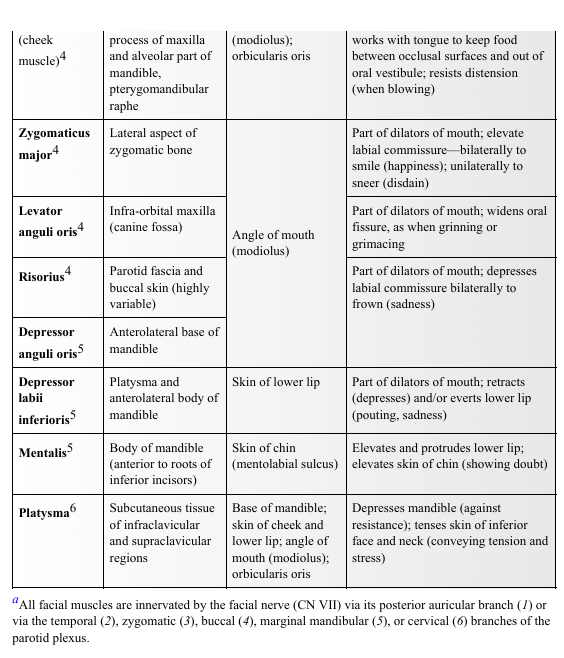
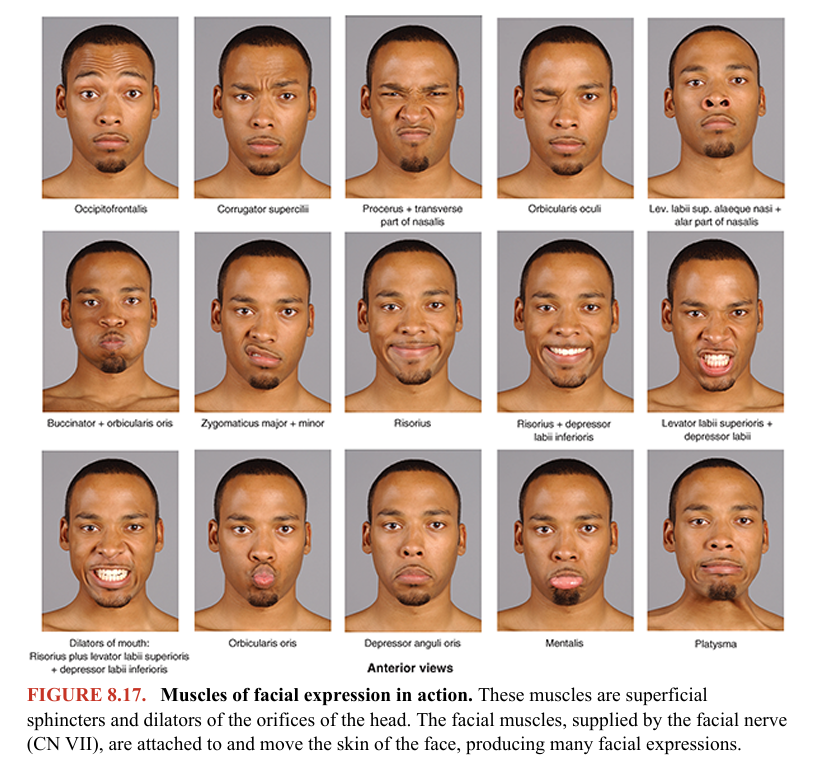
All muscles of facial expression develop from mesoderm in the second pharyngeal arches. A subcutaneous muscular sheet forms during embryonic development that spreads over the neck and face, carrying branches of the nerve of the arch (the facial nerve, CN VII) with it to supply all the muscles formed from the arch (Moore et al., 2020). The muscular sheet differentiates into muscles that surround the facial orifices (mouth, eyes, and nose), serving as sphincter and dilator mechanisms that also produce many facial expressions (Fig. 8.17). Because of their common embryological origin, the platysma and facial muscles are often fused, and their fibers are frequently intermingled
MUSCLES OF SCALP, FOREHEAD, AND EYEBROWS
The occipitofrontalis is a flat digastric muscle, with occipital and frontal bellies that share a common tendon, the epicranial aponeurosis (Figs. 8.15 and 8.16A, B; Table 8.3). Because the aponeurosis is a layer of the scalp, independent contraction of the occipital belly retracts the scalp and contraction of the frontal belly protracts it. Acting simultaneously, the occipital belly, with bony attachments, works as a synergist with the frontal belly, which has no bony attachments, to elevate the eyebrows and produce transverse wrinkles across the forehead. This gives the face a surprised look.
MUSCLES OF MOUTH, LIPS, AND CHEEKS
The lips, shape, and degree of opening of the mouth are important for clear speech. In addition, we add emphasis to our vocal communication with our facial expressions. Several muscles alter the shape of the mouth and lips during speaking as well as during such activities as singing, whistling, and mimicry. The shape of the mouth and lips is controlled by a complex three dimensional group of muscular slips, which include the following (Fig. 8.16B, C; Table 8.3):
• Elevators, retractors, and evertors of the upper lip • Depressors, retractors, and evertors of the lower lip • The orbicularis oris, the sphincter around the mouth • The buccinator in the cheek
At rest, the lips are in gentle contact and the teeth are close together. The orbicularis oris, the first of the series of sphincters associated with the alimentary system (digestive tract), encircles the mouth within the lips, controlling entry and exit through the oral fissure (L. rima oris, the opening between the lips). The orbicularis oris is important during articulation (speech).
The buccinator (L., trumpeter) is a thin, flat, rectangular muscle that attaches laterally to the alveolar process of the maxillae and alveolar part of the mandible, opposite the molar teeth. It also attaches to the pterygomandibular raphe, a tendinous thickening of the buccopharyngeal fascia separating and giving origin to the superior pharyngeal constrictor posteriorly. The buccinator occupies a deeper, more medially placed plane than the other facial muscles, passing deep to the mandible so that it is more closely related to the buccal mucosa than to the skin of the face. The buccinator, active in smiling, also keeps the cheek taut, thereby preventing it from folding and being injured during chewing.
Anteriorly, the fibers of the buccinator mingle medially with those of the orbicularis oris, and the tonus of the two muscles compresses the cheeks and lips against the teeth and gums. The tonic contraction of the buccinator, and especially of the orbicularis oris, provides a gentle but continual resistance to the tendency of the teeth to tilt in an outward direction. In the presence of a short upper lip, or retractors that remove this force, crooked or protrusive (“buck”) teeth develop.
The orbicularis oris (from the labial aspect) and buccinator (from the buccal aspect) work with the tongue (from the lingual aspect) to keep food between the occlusal surfaces of the teeth during mastication (chewing) and to prevent food from accumulating in the oral vestibule. The buccinator also helps the cheeks resist the forces generated by whistling and sucking. The buccinator was given its name because it compresses the cheeks (L. buccae) during blowing (e.g., when a musician plays a wind instrument). Some trumpeters (notably the late Dizzy Gillespie) stretch their buccinators and other cheek muscles so much that their cheeks balloon out when they blow forcibly on their instruments.
Several dilator muscles radiate from the lips and angles of the mouth, somewhat like the spokes of a wheel, retracting the various borders of the oral fissure collectively, in groups, or individually. Lateral to the angles of the mouth or commissures of the lips (the junctions of the upper and lower lips), fibers of as many as nine facial muscles interlace or merge in a highly variable and multiplanar formation called the modiolus, which is largely responsible for the occurrence of dimples in many people.
The platysma (G., flat plate) is a broad, thin sheet of muscle in the subcutaneous tissue of the neck (Fig. 8.16A, B; Table 8.3). The anterior borders of the two muscles decussate over the chin and blend with the facial muscles. Acting from its superior attachment, the platysma tenses the skin, producing vertical skin ridges, conveying great stress, and releasing pressure on the superficial veins. Acting from its inferior attachment, the platysma helps depress the mandible and draw the corners of the mouth inferiorly, as in a grimace.
MUSCLES OF ORBITAL OPENING
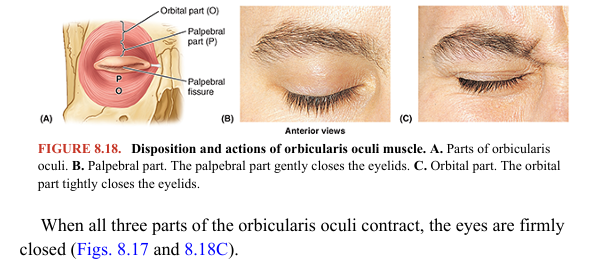
The function of the eyelids (L. palpebrae) is to protect the eyeballs from injury and excessive light. The eyelids also keep the cornea moist by spreading the tears. The orbicularis oculi closes the eyelids and wrinkles the forehead vertically (Figs. 8.16A, B and 8.18; Table 8.3). Its fibers sweep in concentric circles around the orbital margin and eyelids. Contraction of these fibers narrows the palpebral fissure (aperture between the eyelids) and assists the flow of lacrimal fluid (tears) by bringing the lids together laterally first, closing the palpebral fissure in a lateral to medial direction. The orbicularis oculi muscle consists of three parts: 1. Palpebral part: arising from the medial palpebral ligament (see Fig. 8.21) and mostly located within the eyelids, gently closes the eyelids (as in blinking or sleep) to keep the cornea from drying 2. Lacrimal part: passing posterior to the lacrimal sac, draws the eyelids medially, aiding drainage of tears 3. Orbital part: overlying the orbital rim and attached to the frontal bone and maxilla medially, tightly closes the eyelids (as in winking or squinting) to protect the eyeballs against glare and dust
MUSCLES OF NOSE AND EARS
As demonstrated in the Clinical Box “Flaring of Nostrils” in this chapter, the muscles of the nose may provide evidence of breathing behaviors. Otherwise, although these muscles are functionally important in certain mammals (elephants, tapirs, rabbits, and some diving mammals), they are relatively unimportant in humans, except in terms of facial expression and in the specialized field of aesthetic plastic surgery. The muscles of the ears, important in animals capable of cocking or directing the ears toward the sources of sounds, are even less critical in humans
Nerves of Face and Scalp
Cutaneous (sensory) innervation of the face and anterosuperior part of the scalp is provided primarily by the trigeminal nerve (CN V), whereas motor innervation to the facial muscles is provided by the facial nerve (CN VII).
CUTANEOUS NERVES OF FACE AND SCALP
The trigeminal nerve (CN V) originates from the lateral surface of the pons of the midbrain by two roots: motor and sensory. These roots are comparable to the motor (anterior) and sensory (posterior) roots of spinal nerves. The sensory root of CN V consists of the central processes of pseudounipolar neurons located in a sensory ganglion (trigeminal ganglion) at the distal end of the root, which is bypassed by the multipolar neuronal axons making up the motor root. CN V is the sensory nerve for the face and the motor nerve for the muscles of mastication and several small muscles (Fig. 8.19).
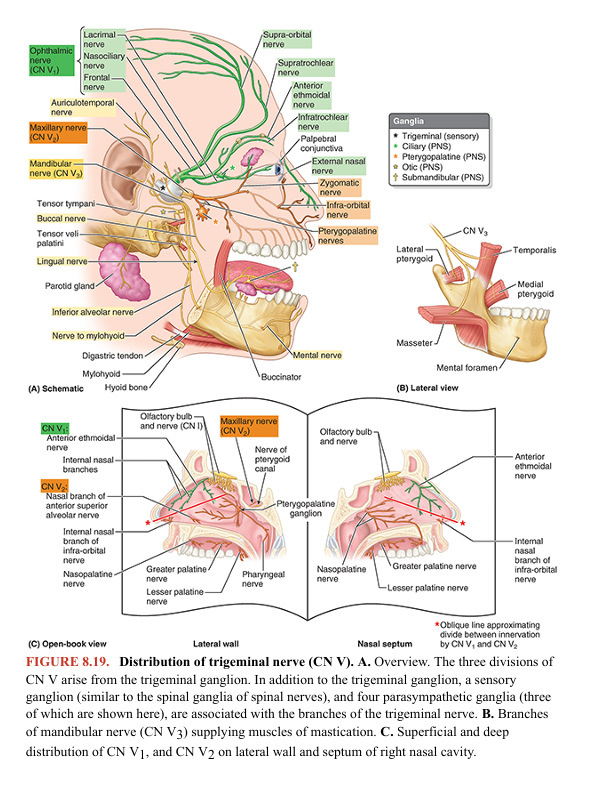
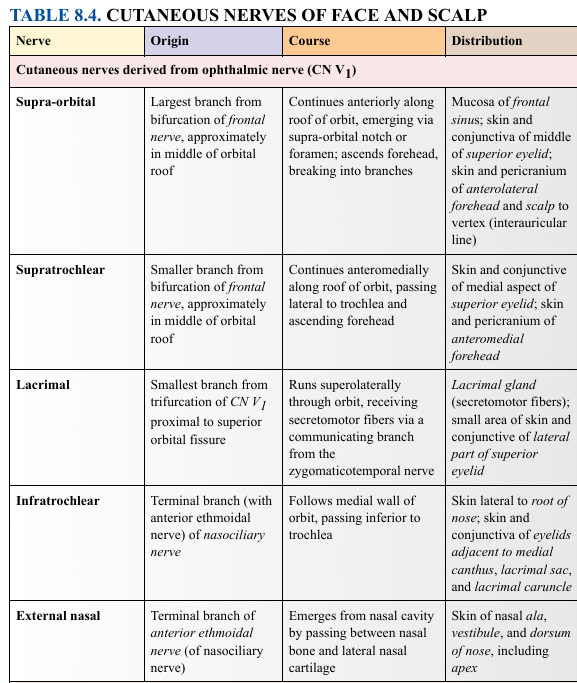
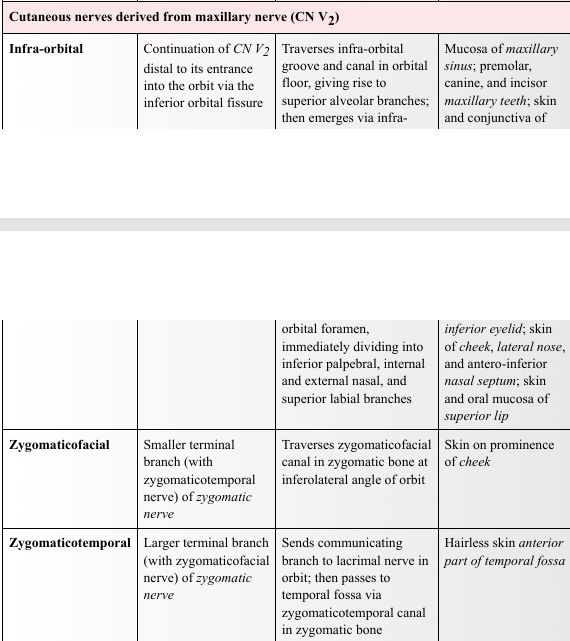
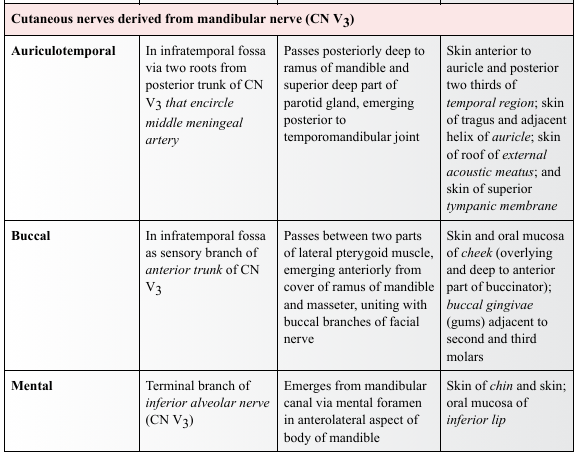
The peripheral processes of the neurons of the trigeminal ganglion constitute three divisions of the nerve: the ophthalmic nerve (CN V1), the maxillary nerve (CN V2), and the sensory component of the mandibular nerve (CN V3). These nerves are named according to their main areas of termination: the eye, maxilla, and mandible, respectively. The first two divisions (ophthalmic and maxillary nerves) are wholly sensory. The mandibular nerve is largely sensory, but it also receives the motor fibers (axons) from the motor root of CN V that mainly supply the muscles of mastication. The cutaneous nerves derived from each division of CN V are illustrated in Figure 8.20, and the origin, course, and distribution of each nerve are listed and described in Table 8.4

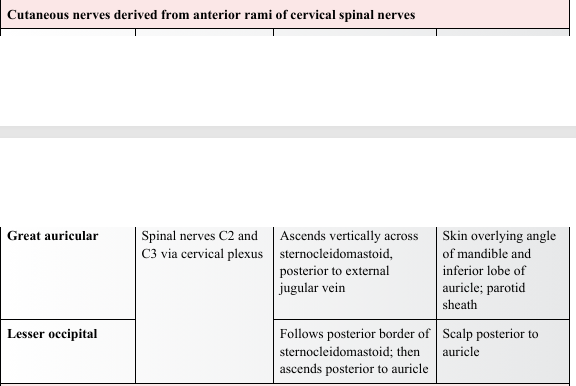
The cutaneous nerves of the neck overlap those of the face. Cutaneous branches of cervical nerves from the cervical plexus extend over the posterior aspect of the neck and scalp. The great auricular nerve innervates the inferior aspect of the auricle (external ear) and much of the parotid region of the face (the area overlying the angle of the jaw).
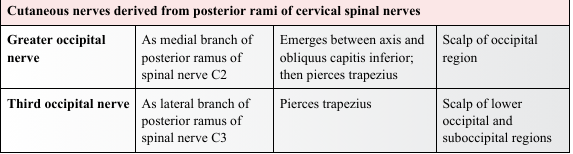
OPHTHALMIC NERVE
The ophthalmic nerve (CN V1), the superior division of the trigeminal nerve, is the smallest of the three divisions of CN V. It arises from the trigeminal ganglion as a wholly sensory nerve and supplies the area of skin derived from the embryonic frontonasal prominence (Moore et al., 2020). As CN V1 enters the orbit through the superior orbital fissure, it trifurcates into the frontal, nasociliary, and lacrimal nerves (Fig. 8.19). Except for the external nasal nerve, the cutaneous branches of CN V1 reach the skin of the face via the orbital opening (Fig. 8.21).
The frontal nerve, the largest branch produced by the trifurcation of CN V1, runs along the roof of the orbit toward the orbital opening, bifurcating approximately midway into the cutaneous supra-orbital and supratrochlear nerves, distributed to the forehead and scalp (Figs. 8.21 and 8.22).The frontal nerve, the largest branch produced by the trifurcation of CN V1, runs along the roof of the orbit toward the orbital opening, bifurcating approximately midway into the cutaneous supra-orbital and supratrochlear nerves, distributed to the forehead and scalp (Figs. 8.21 and 8.22).
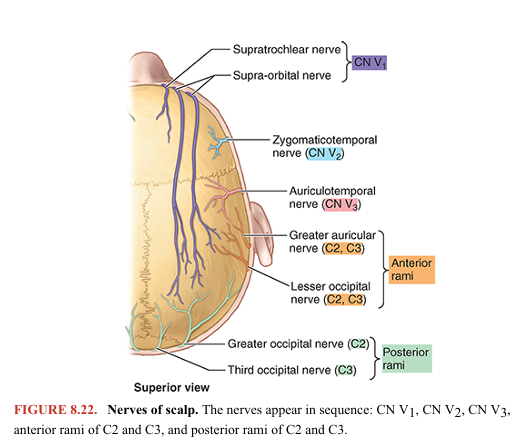
The nasociliary nerve, the intermediate branch of the CN V1 trifurcation, supplies branches to the eyeball and divides within the orbit into the posterior ethmoidal, anterior ethmoidal, and infratrochlear nerves (Fig. 8.19). The posterior and anterior ethmoidal nerves leave the orbit, the latter running a circuitous course passing through the cranial and nasal cavities. Its terminal branch, the external nasal nerve, is a cutaneous nerve supplying the external nose. The infratrochlear nerve is a terminal branch of the nasociliary nerve and its main cutaneous branch.
The lacrimal nerve, the smallest branch from the trifurcation of CN V1, is primarily a cutaneous branch, but it also conveys some secretomotor fibers, sent via a communicating branch, from a ganglion associated with the maxillary nerve for innervation of the lacrimal gland (Figs. 8.19, 8.20, and 8.21).
MAXILLARY NERVE
The maxillary nerve (CN V2), the intermediate division of the trigeminal nerve, also arises as a wholly sensory nerve (Fig. 8.19A). CN V2 passes anteriorly from the trigeminal ganglion and leaves the cranium through the foramen rotundum in the base of the greater wing of the sphenoid. The maxillary nerve enters the pterygopalatine fossa, where it gives off branches to the pterygopalatine ganglion and continues anteriorly, entering the orbit through the inferior orbital fissure (Fig. 8.21). It gives off the zygomatic nerve and passes anteriorly into the infra-orbital groove and foramen as the infra-orbital nerve. The zygomatic nerve runs to the lateral wall of the orbit, giving rise to two of the three cutaneous branches of CN V2, the zygomaticofacial and zygomaticotemporal nerves. The zygomatic nerve then continues as a communicating branch conveying secretomotor fibers to the lacrimal nerve. En route to the face, the infra-orbital nerve gives off palatine branches, branches to the mucosa of the maxillary sinus, and branches to the middle and anterior upper teeth. It reaches the skin of the face by traversing the infra orbital foramen on the infra-orbital surface of the maxilla. The three cutaneous branches of the maxillary nerve supply the area of skin derived from the embryonic maxillary prominences (Fig. 8.20) (Moore et al., 2020).
MANDIBULAR NERVE
The mandibular nerve (CN V3) is the inferior and largest division of the trigeminal nerve (Fig. 8.19A). It is formed by the union of sensory fibers from the sensory ganglion and the motor root of CN V in the foramen ovale in the greater wing of the sphenoid, through which CN V3 emerges from the cranium. CN V3 has three sensory branches that supply the area of skin derived from the embryonic mandibular prominence. It also supplies motor fibers to the muscles of mastication (Fig. 8.19B). CN V3 is the only division of CN V that carries motor fibers. The major cutaneous branches of CN V3 are the auriculotemporal, buccal, and mental nerves. En route to the skin, the auriculotemporal nerve passes deep to the parotid gland, conveying secretomotor fibers to it from the otic ganglion (Fig. 8.19A).
NERVES OF SCALP
Innervation of the scalp anterior to the auricles of the external ears is through branches of all three divisions of CN V, the trigeminal nerve (Figs. 8.20B and 8.22; Table 8.4). Posterior to the auricles, the nerve supply is from spinal cutaneous nerves (C2 and C3).
MOTOR NERVES OF FACEMOTOR NERVES OF FACE
The motor nerves of the face are the facial nerve to the muscles of facial expression and the motor root of the trigeminal nerve/mandibular nerve to the muscles of mastication (masseter, temporal, medial, and lateral pterygoids). These nerves also supply some more deeply placed muscles (described later in this chapter in relation to the mouth, middle ear, and neck) (Fig. 8.19A).
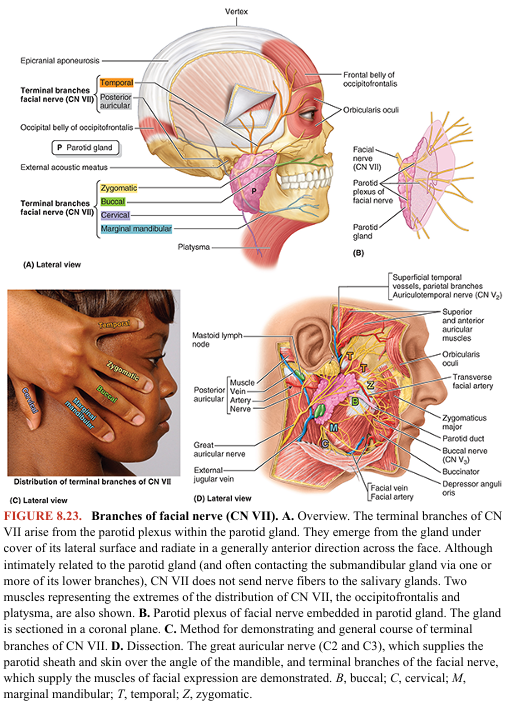
FACIAL NERVE
CN VII, the facial nerve, has a motor root and a sensory/parasympathetic root (the latter being the intermediate nerve). The motor root of CN VII supplies the muscles of facial expression, including the superficial muscle of the neck (platysma), auricular muscles, scalp muscles, and certain other muscles derived from mesoderm in the embryonic second pharyngeal arch (Fig. 8.23). Following a circuitous route through the temporal bone, CN VII emerges from the cranium through the stylomastoid foramen located between the mastoid and styloid processes (see Figs. 8.9B and 8.11). It immediately gives off the posterior auricular nerve, which passes posterosuperior to the auricle of the ear to supply the auricularis posterior and occipital belly of the occipitofrontalis muscle (Fig. 8.23A, C).
The main trunk of CN VII runs anteriorly and is engulfed by the parotid gland, in which it forms the parotid plexus. This plexus gives rise to the five terminal branches of the facial nerve: temporal, zygomatic, buccal, marginal mandibular, and cervical. The names of the branches refer to the regions they supply. Specific muscles supplied by each branch are identified in Table 8.3.
The temporal branch of CN VII emerges from the superior border of the parotid gland and crosses the zygomatic arch to supply the auricularis superior and auricularis anterior; the frontal belly of the occipitofrontalis; and, most important, the superior part of the orbicularis oculi.
The zygomatic branch of CN VII passes via two or three branches superior and mainly inferior to the eye to supply the inferior part of the orbicularis oculi and other facial muscles inferior to the orbit.
The buccal branch of CN VII passes external to the buccinator to supply this muscle and the muscles of the upper lip (upper parts of orbicularis oris and inferior fibers of levator labii superioris).
The marginal mandibular branch of CN VII supplies the risorius and muscles of the lower lip and chin. It emerges from the inferior border of the parotid gland and crosses the inferior border of the mandible deep to the platysma to reach the face. In approximately 20% of people, this branch passes inferior to the angle of the mandible.
The cervical branch of CN VII passes inferiorly from the inferior border of the parotid gland and runs posterior to the mandible to supply the platysma (Fig. 8.23). Cutaneous branches from the geniculate ganglion accompany the auricular branch of the vagus nerve to skin on both sides of the auricle, in the region of the concha. Although not evident anatomically, their existence is most evident through clinical manifestations.
Superficial Vasculature of Face and Scalp
The face is richly supplied by with superficial arteries and external veins, as is evident in blushing and blanching (e.g., becoming pale due to cold). The terminal branches of both arteries and veins anastomose freely, including anastomoses across the midline with contralateral partners.
SUPERFICIAL ARTERIES OF FACE
Most superficial arteries of the face are branches or derivatives of branches of the external carotid artery, as illustrated in Figure 8.24. The origin, course, and distribution of these arteries are presented in Table 8.5. The facial artery provides the major arterial supply to the face. It arises from the external carotid artery and winds its way to the inferior border of the mandible, just anterior to the masseter (Figs. 8.23C and 8.24B). The artery lies superficially here, immediately deep to the platysma. The facial artery crosses the mandible, buccinator, and maxilla as it courses over the face to the medial angle (canthus) of the eye, where the superior and inferior eyelids meet (Fig. 8.24B). The facial artery lies deep to the zygomaticus major and levator labii superioris muscles. Near the termination of its sinuous course through the face, the facial artery passes approximately a finger’s breadth lateral to the angle of the mouth. The facial artery sends branches to the upper and lower lips (superior and inferior labial arteries), ascends along the side of the nose, and anastomoses with the dorsal nasal branch of the ophthalmic artery. Distal to the lateral nasal artery at the side of the nose, the terminal part of the facial artery is called the angular artery.
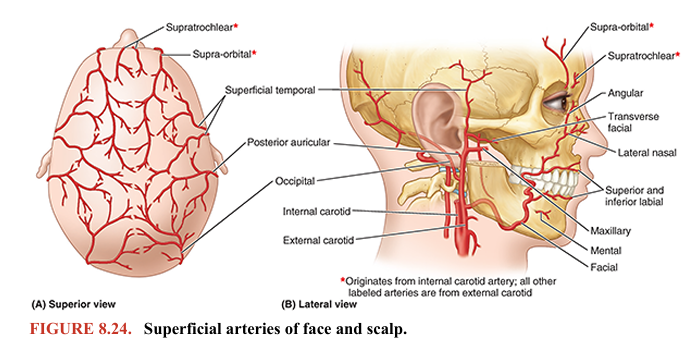
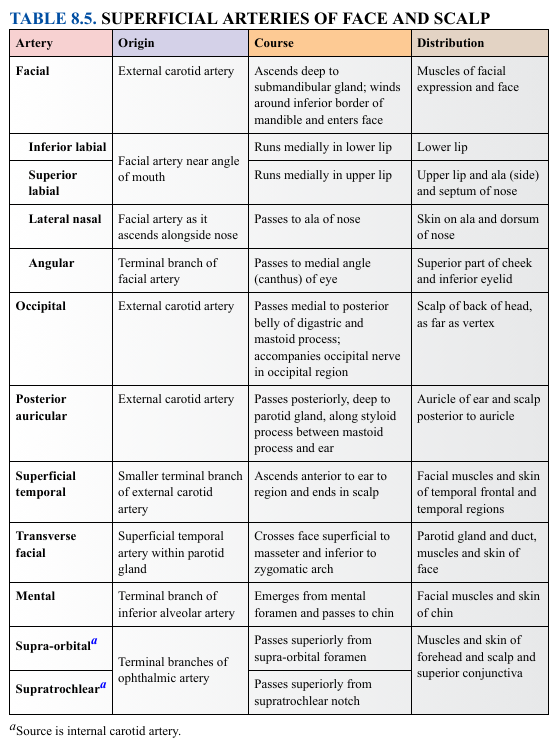
TABLE 8.5. SUPERFICIAL ARTERIES OF FACE AND SCALP
The superficial temporal artery is the smaller terminal branch of the external carotid artery; the other branch is the maxillary artery. The superficial temporal artery emerges on the face between the temporomandibular joint (TMJ) and the auricle, enters the temporal fossa, and ends in the scalp by dividing into frontal and parietal branches. These arterial branches accompany or run in close proximity to the corresponding branches of the auriculotemporal nerve. The transverse facial artery arises from the superficial temporal artery within the parotid gland and crosses the face superficial to the masseter (Figs. 8.23C and 8.24B), approximately a finger’s breadth inferior to the zygomatic arch. It divides into numerous branches that supply the parotid gland and duct, the masseter, and the skin of the face. It anastomoses with branches of the facial artery. In addition to the superficial temporal arteries, several other arteries accompany cutaneous nerves in the face. Supra-orbital and supratrochlear arteries, branches of the ophthalmic artery, accompany nerves of the same name across the eyebrows and forehead (Fig. 8.24; Table 8.5). The supra orbital artery continues and supplies the anterior scalp to the vertex. The mental artery, the only superficial branch derived from the maxillary artery, accompanies the nerve of the same name in the chin
ARTERIES OF SCALPARTERIES OF SCALP
The scalp has a rich blood supply (Fig. 8.24A; Table 8.5). The arteries course within layer two of the scalp, the subcutaneous connective tissue layer between the skin and the epicranial aponeurosis. The arteries anastomose freely with adjacent arteries and across the midline with the contralateral artery. The arterial walls are firmly attached to the dense connective tissue in which the arteries are embedded, limiting their ability to constrict when cut. Consequently, bleeding from scalp wounds is profuse. The arterial supply is from the external carotid arteries through the occipital, posterior auricular, and superficial temporal arteries and from the internal carotid arteries through the supratrochlear and supra-orbital arteries. The arteries of the scalp supply little blood to the neurocranium, which is supplied primarily by the middle meningeal artery.
EXTERNAL VEINS OF FACE
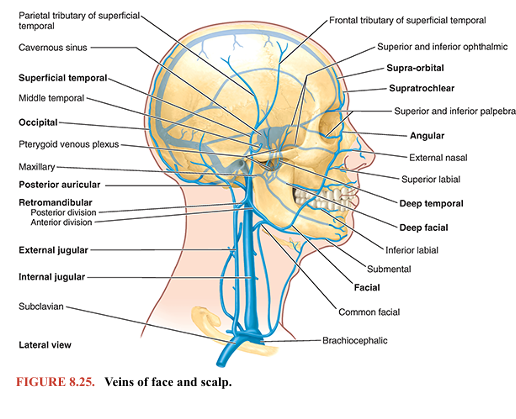
Most external facial veins are drained by veins that accompany the arteries of the face. As with most superficial veins, they are subject to many variations; a common pattern is shown in Figure 8.25, and Table 8.6 provides details
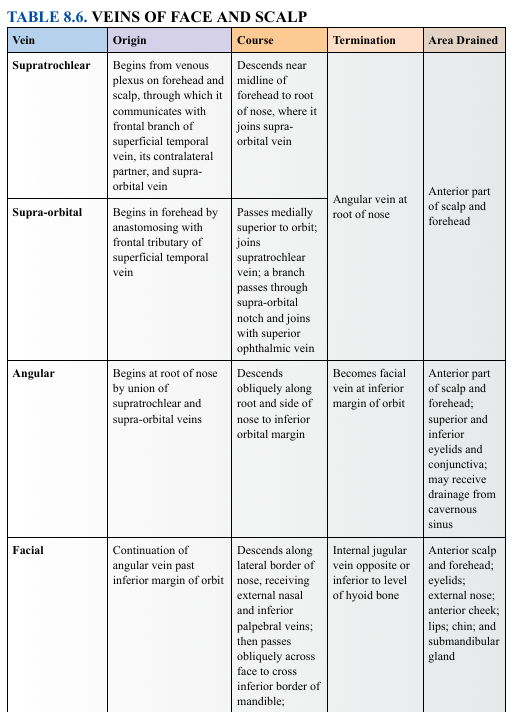
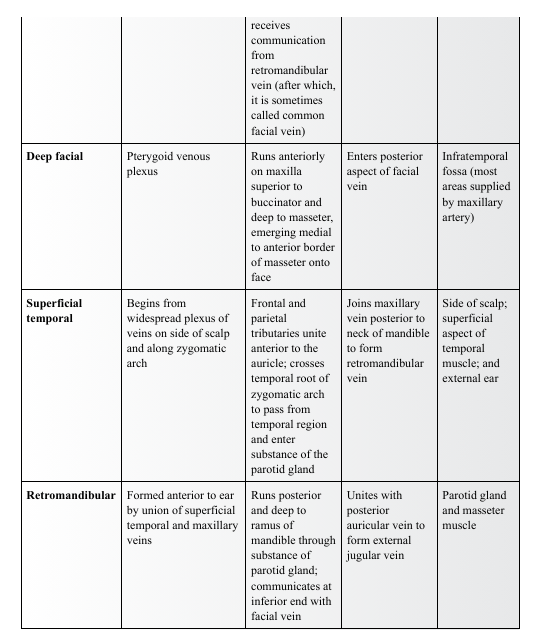
Like veins elsewhere, they have abundant anastomoses that allow drainage to occur by alternate routes during periods of temporary compression. The alternate routes include both superficial pathways (via the facial and retromandibular/external jugular veins) and deep drainage (via the anastomoses with the cavernous sinus, pterygoid venous plexus, and the internal jugular vein). The facial veins, coursing with or parallel to the facial arteries, are valveless veins that provide the primary superficial drainage of the face. Tributaries of the facial vein include the deep facial vein, which drains the pterygoid venous plexus of the infratemporal fossa. Inferior to the margin of the mandible, the facial vein is joined by the anterior (communicating) branch of the retromandibular vein. The facial vein drains directly or indirectly into the internal jugular vein (IJV). At the medial angle of the eye, the facial vein communicates with the superior ophthalmic vein, which drains into the cavernous sinus. The retromandibular vein is a deep vessel of the face formed by the union of the superficial temporal vein and the maxillary vein, the latter draining the pterygoid venous plexus. The retromandibular vein runs posterior to the ramus of the mandible within the substance of the parotid gland, superficial to the external carotid artery and deep to the facial nerve. As it emerges from the inferior pole of the parotid gland, the retromandibular vein divides into an anterior branch that unites with the facial vein and a posterior branch that joins the posterior auricular vein inferior to the parotid gland to form the external jugular vein. This vein passes inferiorly and superficially in the neck to empty into the subclavian vein
VEINS OF SCALP
The venous drainage of the superficial parts of the scalp is through the accompanying veins of the scalp arteries, the supra-orbital and supratrochlear veins. The superficial temporal veins and posterior auricular veins drain the scalp anterior and posterior to the auricles, respectively. The posterior auricular vein often receives a mastoid emissary vein from the sigmoid sinus, a dural venous sinus (see Fig. 8.33). The occipital veins drain the occipital region of the scalp. Venous drainage of deep parts of the scalp in the temporal region is through deep temporal veins, which are tributaries of the pterygoid venous plexus
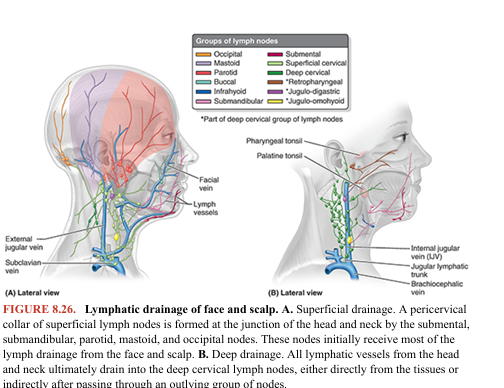
LYMPHATIC DRAINAGE OF FACE AND SCALPLYMPHATIC DRAINAGE OF FACE AND SCALP
There are no lymph nodes in the scalp, and except for the parotid/buccal region, there are no lymph nodes in the face. Lymph from the scalp, face, and neck drains into the superficial ring (pericervical collar) of lymph nodes— submental, submandibular, parotid, mastoid, and occipital—located at the junction of the head and neck (Fig. 8.26A). The lymphatic vessels of the face accompany other facial vessels. Superficial lymphatic vessels accompany veins, and deep lymphatics accompany arteries. All lymphatic vessels from the head and neck drain directly or indirectly into the deep cervical lymph nodes (Fig. 8.26B), a chain of nodes mainly located along the IJV in the neck. Lymph from these deep nodes passes to the jugular lymphatic trunk, which joins the thoracic duct on the left side and the IJV or brachiocephalic vein on the right side. A summary of the lymphatic drainage of the face follows: • Lymph from the lateral part of the face and scalp, including the eyelids, drains to the superficial parotid lymph nodes. • Lymph from the deep parotid nodes drains to the deep cervical lymph nodes. • Lymph from the upper lip and lateral parts of the lower lip drains to the submandibular lymph nodes. • Lymph from the chin and central part of the lower lip drains to the submental lymph nodes.
Surface Anatomy of Face
Despite the apparently infinite variations that enable people to be identified as individuals, the features of the human face are constant (Fig. 8.27). The eyebrows (L. supercilia) are linear growths of hair overlying the supra orbital margin. The hairless region between the eyebrows overlies the glabella, and the prominent ridges that extend laterally on each side above the eyebrows are the superciliary arches.
The eyelids (L. palpebrae) are mobile, musculofibrous folds that overlie the eyeball. They are joined at each end of the palpebral fissure between the eyelids at the medial and lateral angles (canthi) of the eye. The epicanthal fold (epicanthus) is a fold of skin that covers the medial angle of the eye in some people, chiefly Asians. The depressions superior and inferior to the eyelids are the suprapalpebral and infrapalpebral sulci. The shape of the nose varies remarkably. The external nose presents a prominent apex and is continuous with the forehead at the root of the nose (bridge). The rounded anterior border between the root and apex is the dorsum of the nose. Inferior to the apex, the nasal cavity of each side opens anteriorly by a naris (plural = nares), bounded medially by the nasal septum and laterally by an ala (wing) of the nose. The lips surround the opening of the mouth, the oral fissure. The vermillion border of the lip marks the beginning of the transitional zone (commonly referred to as the lip) between the skin and mucous membrane of the lip. The skin of the transitional zone is hairless and thin, increasing its sensitivity and causing its color to be different (because of underlying capillary beds) from that of the adjacent skin of the face. The lateral junction of the lips is the labial commissure; the angle between the lips, medial to the commissure, that increases as the mouth opens and decreases as it closes is the angle of the mouth. The median part of the upper lip features a tubercle, superior to which is a shallow groove, the philtrum (G., love charm), extending to the nasal septum. The musculofibrous folds of the lips continue laterally as the cheek, which also contains the buccinator muscle and buccal fat-pad. The cheek is separated from the lips by the nasolabial sulcus, which runs obliquely between the ala of the nose and the angle of the mouth. These grooves are easiest to observe during smiling. The lower lip is separated from the mental protuberance (chin) by the mentolabial sulcus. The lips, cheeks, and chin of the mature male grow hair as part of the secondary sex characteristics, the beard.

Scalp Wounds
The epicranial aponeurosis is clinically important. Because of the strength of this aponeurosis, superficial scalp wounds do not gape, and the margins of the wound are held together. Furthermore, deep sutures are not necessary when suturing superficial wounds because the epicranial aponeurosis does not allow wide separation of the skin. Deep scalp wounds gape widely when the epicranial aponeurosis is lacerated in the coronal plane because of the pull of the frontal and occipital bellies of the occipitofrontalis muscle in opposite directions (anteriorly and posteriorly)
Scalp Infections
The loose connective tissue layer (layer four) of the scalp is the danger area of the scalp because pus or blood spreads easily in it. Infection in this layer can also pass into the cranial cavity through small emissary veins, which pass through parietal foramina in the calvaria, and reach intracranial structures such as the meninges (see Fig. 8.8A, C). An infection cannot pass into the neck because the occipital bellies of the occipitofrontalis muscle attach to the occipital bone and mastoid parts of the temporal bones (see Fig. 8.16A). Neither can a scalp infection spread laterally beyond the zygomatic arches because the epicranial aponeurosis is continuous with the temporal fascia that attaches to these arches. An infection or fluid (e.g., pus or blood) from an injury to the scalp and/or the forehead can enter the eyelids and the root of the nose because the occipitofrontalis inserts into the skin and subcutaneous tissue and does not attach to the bone (see Fig. 8.16B). Consequently, “black eyes” (periorbital ecchymosis) can result (Fig. B8.12). The skin of the eyelid is the thinnest of the body and is delicate and sensitive. Because of the loose nature of the subcutaneous tissue within the eyelids, even a relatively slight injury or inflammation may result in an accumulation of fluid, causing the eyelids to swell. Blows to the periorbital region usually produce soft tissue damage because the tissues are crushed against the strong and relatively sharp margin. Ecchymoses (purple patches) develop as a result of extravasation of blood into the subcutaneous tissue and skin of the eyelids and surrounding regions.
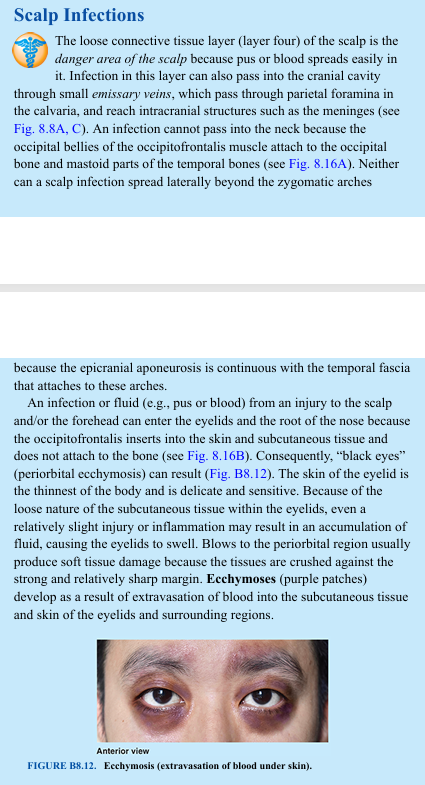
Sebaceous Cysts
The ducts of sebaceous glands associated with hair follicles in the scalp may become obstructed, resulting in the retention of secretions and the formation of sebaceous cysts (pilar cysts). Because they are in the skin, sebaceous cysts move with the scalp. Cephalohematoma Sometimes after a difficult birth, bleeding occurs between the baby’s pericranium (layer 5 of scalp) (see Fig. 8.15A) and calvaria, usually over one parietal bone. Blood becomes trapped in this area, forming a cephalohematoma. This benign condition frequently seen in neonates results from birth trauma that ruptures multiple, minute periosteal arteries that nourish the bones of the calvaria.
Cephalohematoma
Sometimes after a difficult birth, bleeding occurs between the baby’s pericranium (layer 5 of scalp) (see Fig. 8.15A) and calvaria, usually over one parietal bone. Blood becomes trapped in this area, forming a cephalohematoma. This benign condition frequently seen in neonates results from birth trauma that ruptures multiple, minute periosteal arteries that nourish the bones of the calvaria.
Flaring of Nostrils
The actions of the nasalis muscles (see Fig. 8.17, center top row) have generally been held as insignificant. However, observant clinicians study their action because of their diagnostic value (e.g., true nasal breathers can flare their nostrils distinctly). Habitual mouth breathing, caused by chronic nasal obstruction, for example, diminishes and sometimes eliminates the ability to flare the nostrils. Children who are chronic mouth breathers often develop dental malocclusion (improper bite) because the alignment of the teeth is maintained to a large degree by normal periods of occlusion and labial closure. Antisnoring devices have been developed that attach to the nose to flare the nostrils and maintain a more patent air passageway.
Paralysis of Facial Muscles
Injury to the facial nerve (CN VII) or its branches produces paralysis of some or all facial muscles on the affected side (Bell palsy). The affected area sags, and facial expression is distorted, making it appear passive or sad (Fig. B8.13). The loss of tonus of the orbicularis oculi causes the inferior eyelid to evert (fall away from the surface of the eyeball). Thus, lacrimal fluid is not spread over the cornea, preventing adequate lubrication, hydration, and flushing of the surface of the cornea.
This makes the cornea vulnerable to ulceration. A resulting corneal scar can impair vision. If the injury weakens or paralyzes the buccinator and orbicularis oris, food will accumulate in the oral vestibule during chewing, usually requiring continual removal with a finger. When the sphincters or dilators of the mouth are affected, displacement of the mouth (drooping of its corner) is produced by contraction of unopposed contralateral facial muscles and gravity, resulting in food and saliva dribbling out of the side of the mouth. Weakened lip muscles affect speech as a result of an impaired ability to produce labial (B, M, P, or W) sounds. Affected persons cannot whistle or blow a wind instrument. They frequently dab their eyes and mouth with a handkerchief to wipe the fluid (tears and saliva), which runs from the drooping lid and mouth. The fluid and constant wiping may result in localized skin irritation.
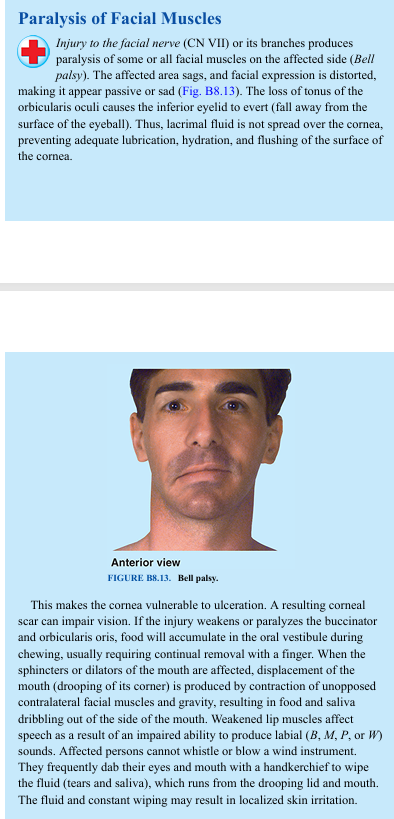
Infra-Orbital Nerve Block For treating wounds of the upper lip and cheek or, more commonly, for repairing the maxillary incisor teeth, local anesthesia of the inferior part of the face is achieved by infiltration of the infra-orbital nerve with an anesthetic agent. The injection is made in the region of the infra-orbital foramen, by elevating the upper lip and passing the needle through the junction of the oral mucosa and gingiva at the superior aspect of the oral vestibule. To determine where the infra-orbital nerve emerges, pressure is exerted on the maxilla in the region of the infra-orbital foramen. Too much pressure on the nerve causes considerable pain. Because companion infra-orbital vessels leave the infra-orbital foramen with the nerve, aspiration of the syringe during injection prevents inadvertent injection of anesthetic fluid into a blood vessel. Because the orbit is located just superior to the injection site, a careless injection could result in passage of anesthetic fluid into the orbit, causing temporary paralysis of the extra-ocular muscles.
Mental Nerve Blocks Occasionally, it is desirable to anesthetize one side of the skin and mucous membrane of the lower lip and the skin of the chin (e.g., to suture a severe laceration of the lip or chin). Injection of an anesthetic agent into the mental foramen blocks the mental nerve that supplies the skin and mucous membrane of the lower lip from the mental foramen to the midline, including the skin of the chin.

Buccal Nerve Block To anesthetize the skin and mucous membrane of the cheek (e.g., to suture a knife wound), an anesthetic injection can be made into the mucosa covering the retromolar fossa, a triangular depression posterior to the 3rd mandibular molar tooth between the anterior border of the ramus and the temporal crest (on the medial side of the coronoid process of the mandible).
Trigeminal Neuralgia Trigeminal neuralgia or tic douloureux is a sensory disorder of the sensory root of CN V that occurs most often in middle-aged and elderly persons. It is characterized by sudden attacks of excruciating, lightning-like jabs of facial pain. A paroxysm (sudden sharp pain) can last for 15 minutes or more. The pain may be so intense that the person winces, thus the common term tic (twitch). In some cases, the pain may be so severe that psychological changes occur, leading to depression and even suicide attempts. CN V2 is most frequently involved, then CN V3, and, least frequently, CN V1. The paroxysms are often set off by touching the face, brushing the teeth, shaving, drinking, or chewing. The pain is often initiated by touching an especially sensitive trigger zone, frequently located around the tip of the nose or the cheek (Haines & Mihailoff, 2018). In trigeminal neuralgia, demyelination of axons in the sensory root occurs. In most cases, this is caused by pressure of a small aberrant artery (Kiernan, 2014). Often, when the aberrant artery is moved away from the sensory root of CN V, the symptoms disappear. Other scientists believe the condition is caused by a pathological process affecting neurons in the trigeminal ganglion. Medical or surgical treatment or both are used to alleviate the pain. In cases involving the CN V2, attempts have been made to block the infra orbital nerve at the infra-orbital foramen using alcohol. This treatment usually relieves pain temporarily. The simplest surgical procedure is avulsion or cutting of the branches of the nerve at the infra-orbital foramen. Other treatments have used radiofrequency selective ablation of parts of the trigeminal ganglion by a needle electrode passing through the cheek and foramen ovale. In some cases, it is necessary to section the sensory root for relief of the pain. To prevent regeneration of nerve fibers, the sensory root of the trigeminal nerve may be partially cut between the ganglion and the brainstem (rhizotomy). Although the axons may regenerate, they do not do so within the brainstem. Surgeons attempt to differentiate and cut only the sensory fibers to the division of CN V involved. The same result may be achieved by sectioning the spinal tract of CN V (tractotomy). After this operation, the sensation of pain, temperature, and simple (light) touch is lost over the area of skin and mucous membrane supplied by the affected component of the CN V. This loss of sensation may annoy the patient, who may not recognize the presence of food on the lip and cheek or feel it within the mouth on the side of the nerve section. However, these disabilities are usually preferable to excruciating pain
Lesions of Trigeminal Nerve Lesions of the entire trigeminal nerve cause widespread anesthesia involving the: • Corresponding anterior half of the scalp • Face (except for skin over the angle of the mandible) and the cornea and conjunctiva • Mucous membranes of the nose, mouth, and anterior part of the tongue Paralysis of the muscles of mastication also occurs.
Herpes Zoster Infection of Trigeminal Ganglion A herpes zoster virus infection may produce a lesion in the cranial ganglia. Involvement of the trigeminal ganglion occurs in approximately 20% of cases (Mukerji et al., 2022). The infection is characterized by an eruption of groups of vesicles following the course of the affected nerve (e.g., ophthalmic herpes zoster). Any division of CN V may be involved, but the ophthalmic division is most commonly affected. Usually, the cornea is involved, often resulting in painful corneal ulceration and subsequent scarring of the cornea. Testing Sensory Function of CN V The sensory function of the trigeminal nerve is tested by asking the person to close his or her eyes and respond when types of touch are felt (e.g., a piece of dry gauze is gently stroked across the skin of one side of the face and then to the corresponding position on the other side). The test is then repeated until the skin of the forehead (CN V1), cheek (CN V2), and lower jaw (CN V3) has been tested. The person is asked if one side feels the same as or different from the other side. The testing may then be repeated using warm or cold instruments and the gentle touch of a sharp pin, again alternating sides (Fig. B8.14A). Specific testing for CN V1 is performed by touching the cornea with a strand of cotton to elicit a reflexive blink (Fig. B8.14B)