cardiac rhythm disturbances + acid/base balance and buffers
1/56
Earn XP
Description and Tags
patho/pharm exam 3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
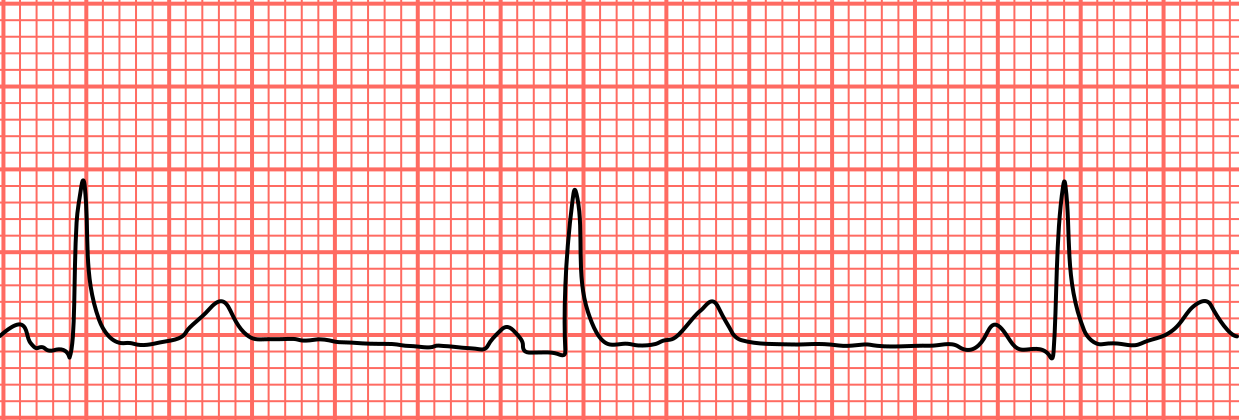
P wave
when the atria contract to fill the ventricles (atrial depolarization)
QRS complex
when ventricles contract (ventricle depolarization)
T wave
when ventricles are at rest (ventricular repolarization)
dysrhythmias
problem with impulse formation and impulse conduction causing abnormal heart rhythms. Affects cardiac output and perfusion.
sinus rhythm disorders
problems that start in the SA node. SA node happens at the P WAVE. (P wave issues)
sinus bradycardia
SA node fires too slowly (< 60 bpm), decreases O2 demand, normal in athletes
vagal stimulation (causes SNS to decrease)
what can cause a sinus bradycardia reaction?

sinus tachycardia
SA node fires too fast (>100 bpm), increase in O2 depmand, the faster the heart is beating, the harder it is to fill chambers.
beta blockers (atenolol), DILTIAZAM (calicum channel blocker)
what drugs are used to treat sinus tachycardia?
caffeine, nicotine, alcohol, cocaine
what can cause HR to increase?
heart block
a delay or interruption in the electrical signal. Pathway is partially or completely blocked, slowing, or stopping heart beat.
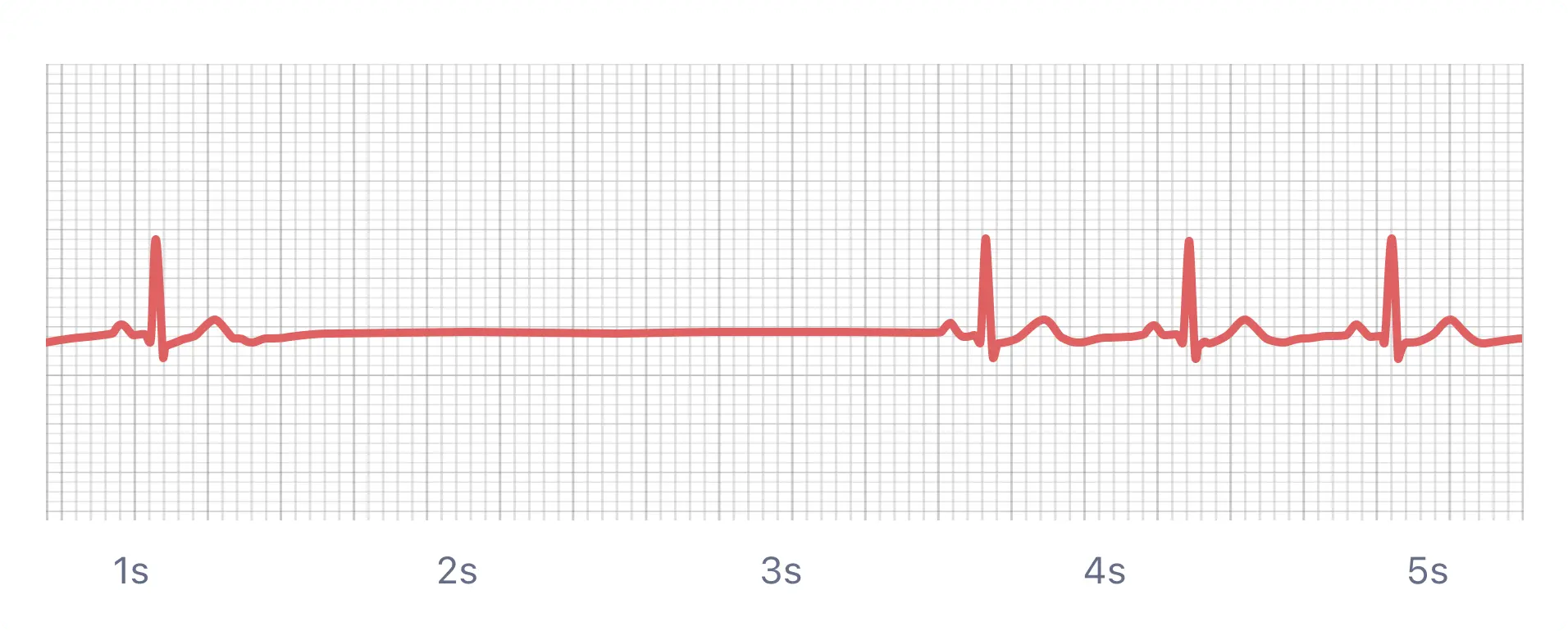
sinus arrest/pause
SA node fails to fire temporarely causing disruption in P wave.
Missing P wave and QRS for a period of time.
CPR, amiodarone, epinephrine
how do you treat sinus arrest/pause?

atrial fibrilation
an irregular, rapid heart rhythm where the atria quiver instead of contracting effectively and cause decrease in filling time. No P WAVE.
Radial pulse may be slower than apical pulse!
clots in the atria → stroke risk
what is the biggest risk for atrial fibrillation?
control rate with diltiazam + control rhythm with cardioversion
treatment for atrial fibrillation?
cardioversion
to correct abnormal rhythm, used when pt is STILL ALIVE (HAS A PULSE) and needs to have rhythm interrupted or reset
MUST PRE-MEDICATE + set monitor to SYNCHRONIZE (will send electricity with QRS complex)
defibrillation
to restart the heart in cardiac arrest, used when pt is DEAD (NO PULSE)
unsynchronized shock given at any time (MUST TURN OFF SYNCHRONIZE)
premature ventricular contraction (PVC)
an extra early heartbeat that starts in the ventricle instead of the SA node, decrease CO. Ventricles will contract before they have time to fill.

unifocal PVC
all PVCs look the same shape and come from one spot in the ventricle. Less serious.
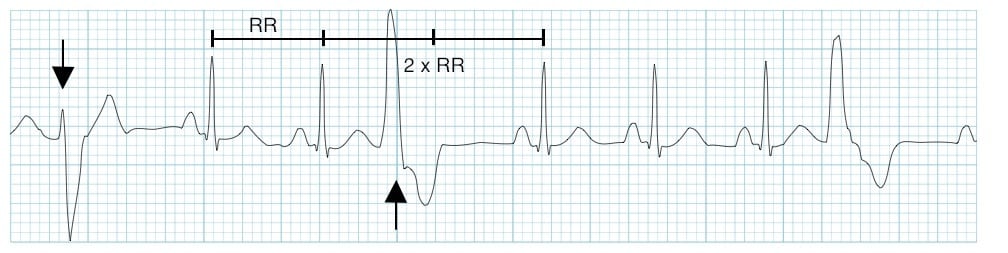
multifocal PVC
electricity shooting off from multiple places in the ventricle, PVCs look all different shapes and sizes
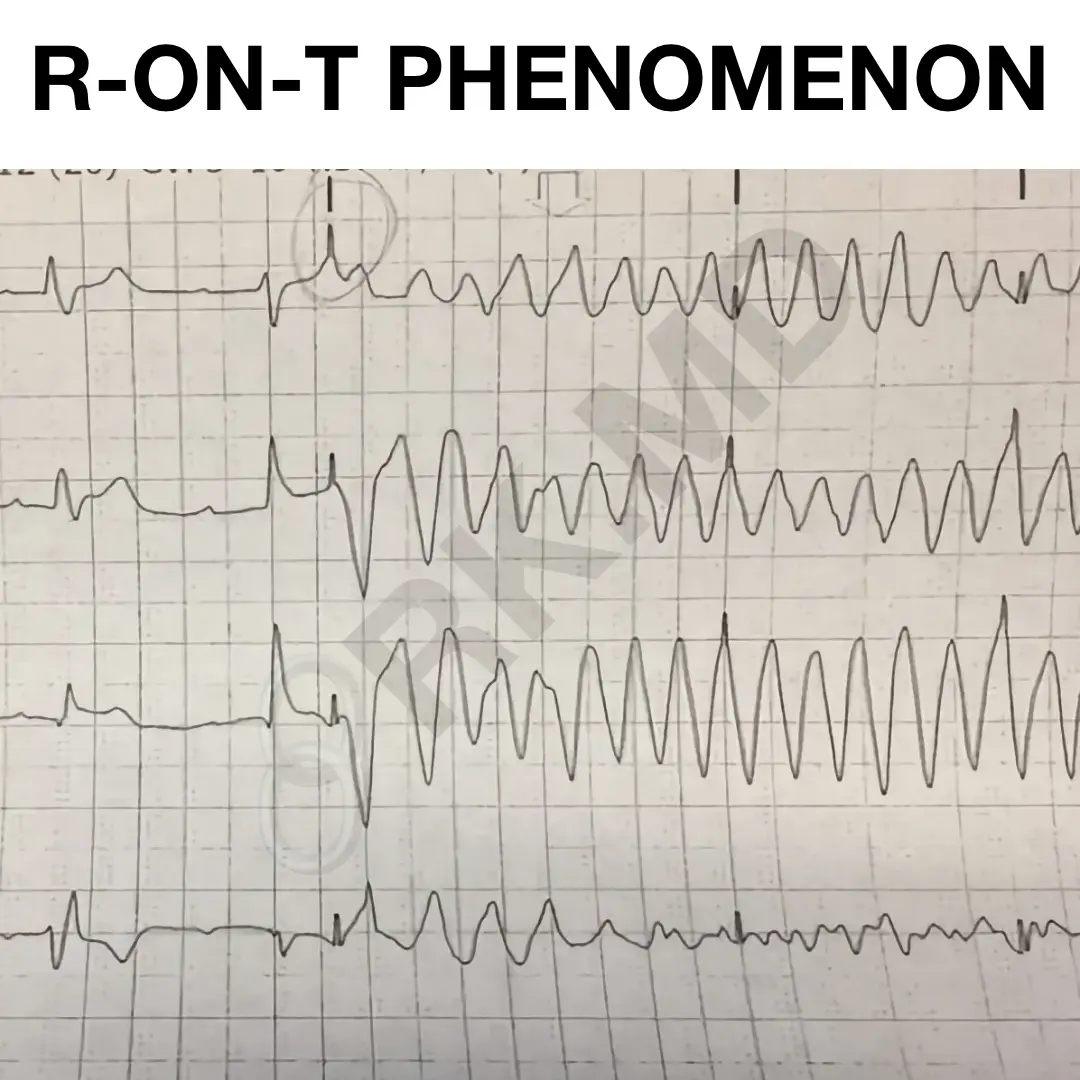
R-on-T phenomenon
a PVC lands right on the T-wave of the previous beat, so PVC hits while heart is recharging. Comes very quickly after QRS complex.
VERY DANGEROUS can cause ventricular fibrillation!
treatment of PVCs?
O2 + correct electrolytes, drugs (lidocane, amidodarone)
ventricular tachycardia
a fast, unstable rhythm that starts in the ventricles instead of the SA node, ventricles fire rapidly + independently. Reduces ventricular filling time and decreases CO.
how to treat ventricular tachycardia with stable pulse?
amiodarone, liodcane, cardiovert (if unstable)
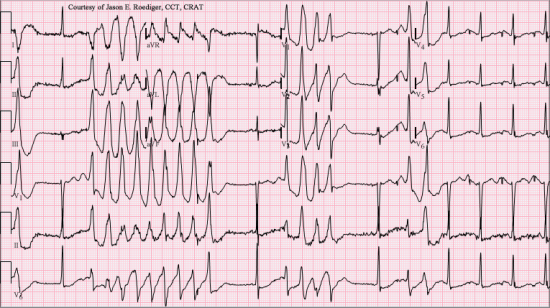
toursades de pointes
polymorphic ventricular tachycardia where QRS rotates around baseline, deflecting downward and upward several beats
Usually caused my Mg deficiency or antibiotics (macrolides)
Mg sulfate or cardioversion
how to treat toursades de pointes?

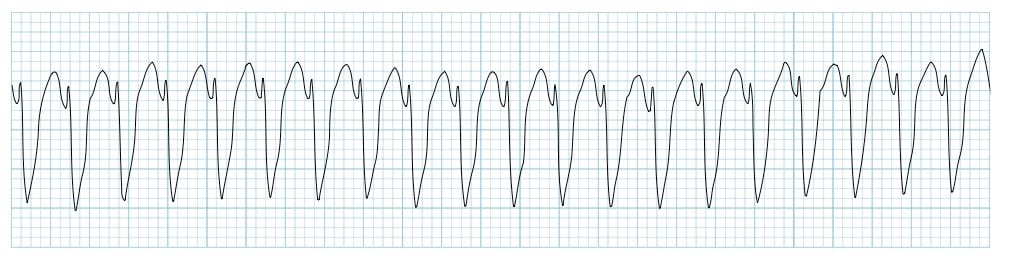
ventricular fibrillation
life threatening cardiac arrest rhythm where the ventricles quiver chaotically instead of contracting. Chaotic pattern of electrical activity in the ventricles.
quivering ventricles → no CO → no pulse → dead
no P waves, QRS, or T-wave. Looks like a bag of worms
metabolic acidosis, MI, electrocution
what causes ventricular fibrillation?
treatment for ventricular fibrilation?
start CPR immediately, defibrillate, epinephrine or vasopressin, AMIODARONE
what does it mean is defibrillator reads “no shock advised”
means there is no electricity in pts body so electricity wont help
electrolytes important for heart?
K+, Mg, Ca+
amiodarone
most common antiarrhythmics for ventricular issues?
dysrhythmia symptoms
SOB, diaphoresis, chest pain, hypotension, heart failure, palpations
bicarbonate (HCO3-)
a base (alkaline substance) that helps the body neutralize acid and maintain normal pH balance. Major Buffer System!
regulated by the KIDNEYS
long process where kidneys do bulk of work and takes about 1.5 days to fix metabolic issues
how long does bicarbonate take to fix issues?
PaCO2
an acidic gas measures how well the lungs are ventilating. Measure CO2 level which reflects respiratory function.
sleepy, hypoventilation, shallow slow breathing
signs of being acidotic
normal pH value
7.35-7.45
low (< 7.35) → acidic
high (> 7.45) → alkaline
normal PaCO2 value (LUNGS + RESPIRATORY)
35-45 mmHg
low (< 35) → alkaline
high (> 45) → acidic
normal HCO3- value (KIDNEYS + METABOLIC)
22-26 mEq/L
low (< 22) → acidic
high (> 26) → alkaline
primary event
what started the issue, either respiratory or metabolic
compensation
body’s effort to adapt to primary event with either lungs or kidneys helping the issue
partial compensation
pH level of opposite organ than one with issue are moving in nopposite direction to help the problem
(ex. during metabolic acidosis the lungs will hyperventilate to help so pH levels begin increasing)
respiratory acidosis
decrease in pH + increase in PaCO2
barely breathing, HYPOVENTILATION (not enough O2)
NO HCO3- TO TREAT
narcotics, sleep apnea, neuro injury, pain when breathing
what causes respiratory acidosis?
sleep apnea
upper airway obstruction, waking up many times during the night bc cannot breath
S+S → snoring, being exhaused, secretions
CPAP (continuous posive airway pressure)
one continues steady pressure of O2. Keeps airways open.
Used for sleep apnea
BiPAP (bilevel positive airway pressure)
two pressure levels higher O2 upon inhalation and low CO2 when exhaling. Aids in ventilation/breathes for pt.
Used for COPD or respiratory failure
Respiratory alkalosis
decrease in pH + decrease PCO2
body trying to cool down, HYPERVENTILATION
sepsis, fever, pain, anxiety
what is respiratoy alkalosis caused by?
metabolic acidosis
decrease in pH + decrease in HCO3-
excessive loss of bicarbonate, causes DIARRHEA
shock, kidney disease (pts norm will be more acidic), hypoxemia
what causes metabolic acidosis?
chronic lung or kidney disease
when is the only time bicarbonate (HCO3-) is used to treat?
metabolic alkalosis
increase in pH + increase in HCO3-
excessive increase of bicarbonate, causes VOMITING
hydrate (hypotonic fluids)
how to treat metabolic alkalosis?
normal PaO2 value
80-100 mmHg