EKG
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
Vessels
carry blood to and from the heart, including arteries, veins, and capillaries.
Right coronary artery
supplies oxygenated blood to the ra, rv, part of the la, and the inferior wall of the left ventricle. it also perfused the sinoatrial node in most people. in some patients, the posterior descending artery also arises from the distal region of the rca
left main coronary artery
the second of two main arteries that carry oxygenated blood to the myocardium. the lmca is short and branches into the left circumflex artery (LCx) and left anterior descending artery (LAD)
left circumflex artery
supplies oxygenated blood to the posterolateral aspect of the la
left anterior descending artery
supplies the anterior wall of the lv. lad occulsion can lead to ventricular dysrhythmias and death
sinoatrial node artery
the artery that supplies blood to the sinoatrial node, the heart's natural pacemaker, which regulates heart rhythm. branches from the RCA. occlusion of this artery can lead to bradycardia.
atrioventricular node artery
the artery that supplies blood to the atrioventricular node, which is crucial for the conduction of electrical impulses between the atria and ventricles. It typically branches from the RCA or the LCX. occlusion can result in high-degree heart block
collateral circulation
the network of tiny blood vessels that can develop to supply blood to the heart muscle when main coronary arteries are narrowed or blocked, helping to maintain blood flow and protect the heart.
occlusion
the blockage or closing of a blood vessel, which can lead to a reduction in blood flow to tissues, potentially causing ischemia or infarction.
ischemia
a condition characterized by reduced blood flow to tissues, leading to a shortage of oxygen and nutrients needed for cellular metabolism. It can cause pain and damage to organs.
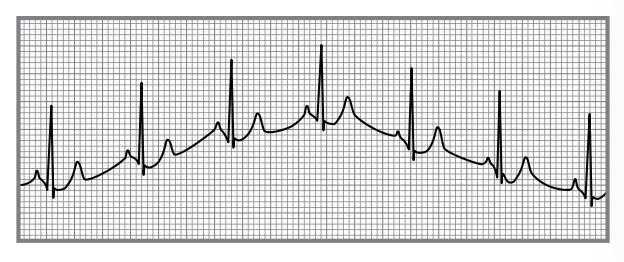
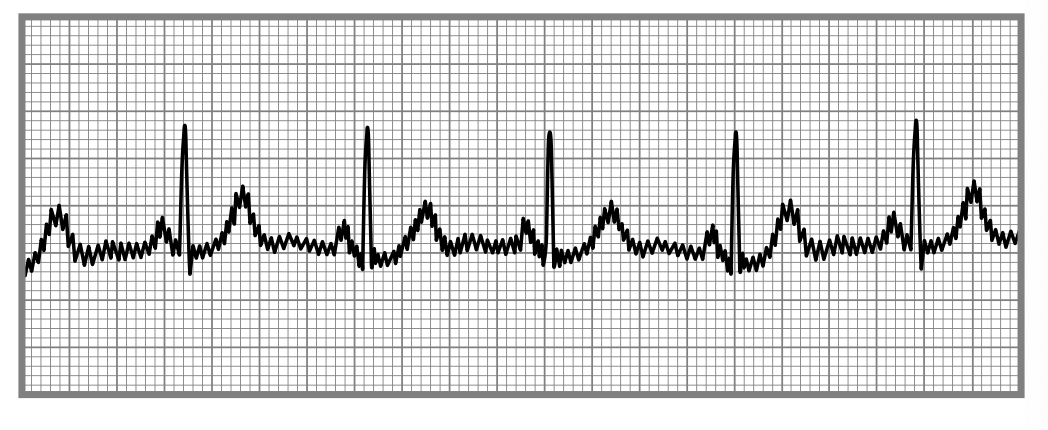
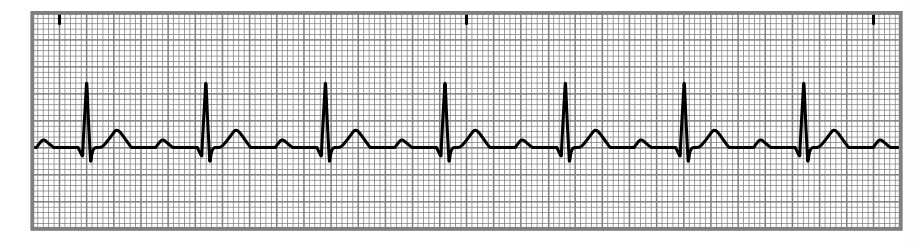
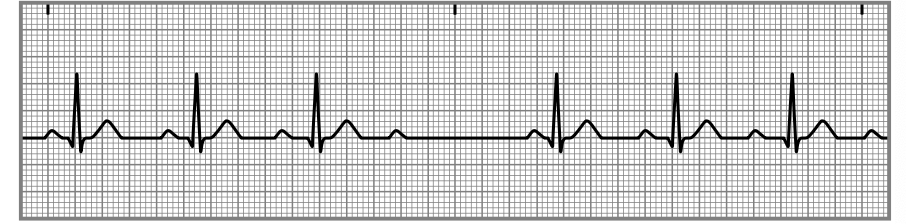
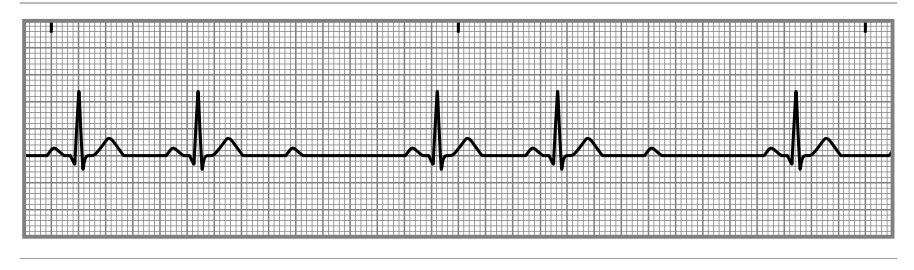
artifact
any unwanted interference or distortion on an EKG trace caused by movement, electrical interference, or other factors, often obscuring the true cardiac signals.
causes for wandering baseline
movement of cables or leads, dry electrodes, labored breathing, improper skin prep (lotion, oils or gels on skin), patient movement and loose electrodes
elimination of wandering baseline
clean the skin, provide clear instructions on how to breathe and when to talk,and ensure proper electrode placement.
somatic tremor
an artifact on an EKG caused by involuntary muscle contractions, often resulting in erratic spikes or waves in the trace.

wandering baseline
an uneven or fluctuating EKG baseline that can obscure cardiac signals.
causes for somatic tremor
shivering or seizures
elimination of somatic tremors
offering a blanket, maintaining warm temp, explain the procedure to calm nerves, slow breathing and placing palms in a prone position with hands under butt or crossed over abdomen.
alternation current interference
an artifact caused by any electronic device near or on the patient shown by small uniform spikes
causes of ac interference
cellphones, wires or nearby medical equipment
elimination of ac interference
ensure cellphones are off and away from patients, move the exam table away from the wall, check the ground prong of the three prong plug to ensure it is tight
interrupted baseline
an EKG artifact where the baseline is disrupted due to a loss of contact between the electrodes and the skin, often caused by movement or poor electrode placement.

causes of interrupted baseline
movement, poor placement or faulty electrodes
elimination of interrupted baseline
regular observation and maintenance of lead wires and double checking connections
ventricular fibrillation (VF)
causes dizziness, a feeling of impending doom, chest discomfort, shortness of breath, seizures, and death. take action immediately. call a code, initiate cpr and have someone bring an aed.
ventricular tachycardia (vt)
drop in blood pressure and level of consciousness due to a decrease in cardiac output. vt can continue to produce a pulse but often deteriorates to a pulseless rhythm or into vf. patients can have dizziness, a feeling of impending doom, chest discomfort and shortness of breath. the same response is the same as that for vf.
asystole
a complete cessation of electrical activity in the heart. common causes include large pulmonary embolism, a large myocardial infarction, respiratory arrest, hypoxia and overdose. other causes include hypothermia, acidosis, electrolyte abnormalities, tension pneumothorax, and trauma. Ii you see asystole on the EKG, observe the patient. if you see breathing and there is a pulse, switch to another lead and see if you have a rhythm. sometimes, patients going into cardiac arrest do not have any warning signs. when a patient’s rhythm deteriorates to asystole, call for help, and begin CPR. using the aed might convert the patient’s rhythm back to normal sinus.
complete heart block
patients who have a heart rhythm that demonstrates 3rd degree av block can progress to cardiac arrest. carefully monitor and perform cpr if needed
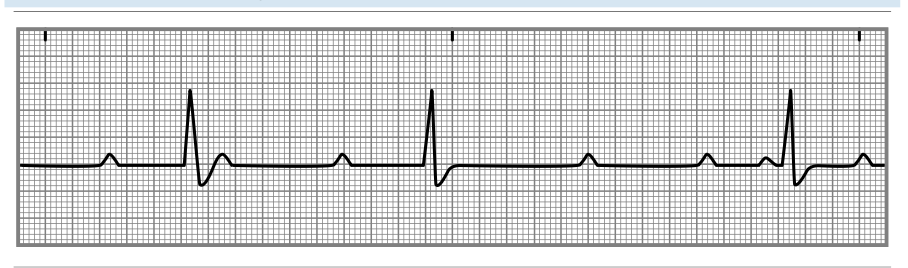
p wave
Represents atrial depolarization on an EKG, indicating atrial contraction. When reviewing the EKG, observe the consistency in shape and note whether a P wave occurs prior to each QRS waveform. Normal P waves have a positive deflection. Variances in the shape of the P wave or missing P waves could indicate electrical conduction pathway abnormalities.
qrs complex or interval
Represents ventricular depolarization on an EKG, indicating ventricular contraction. atrial repolarization isnt visible but occurs during this phase. Evaluate the height of each QRS complex for uniformity. Measure it from the end of the PR interval, which is also the beginning of the Q wave, to the J point. The normal QRS interval ranges from 0.04 to 0.10 seconds. Abnormalities in the width of the QRS complex are usually very noticeable and indicate ventricular dysfunction.
j point
Represents the exact point in time where ventricular depolarization stops and ventricular repolarization starts. The J point is at the end of the QRS complex, or where the ST segment begins, and is the EKG landmark to use when measuring the end of QRS complex. During myocardial ischemia, the J point can elevate or depress below the baseline.
t wave
Represents ventricular repolarization. T waves should follow each QRS complex after a brief pause following the J point. The T waves should appear uniform in configuration.
u wave
Not always visible but represents a repolarization of the bundle of His and the Purkinje fibers. It is a small upward curve and usually follows the T wave. Electrolyte imbalances can sometimes be the cause of U waves appearing on the EKG.
pr interval
Represents the time it takes for the SA node to fire, the atria to depolarize, and electricity to travel through the AV node—or the time from the beginning of atrial depolarization to the beginning of ventricular depolarization. It starts at the beginning of the P wave and ends at the beginning of the Q wave. The normal PR interval ranges from 0.12 to 0.20 seconds.
p-p interval
Represents the amount of time between atrial depolarization cycles (between P waves). Measure the P-P interval from the beginning of one P wave to the beginning of the next P wave. It is valuable when analyzing rate and rhythm.
r-r interval
Represents the amount of time between ventricular depolarization cycles (between R waves). Measure the R-R interval from the beginning of one R wave to the beginning of the next R wave. It is valuable in analyzing rate and rhythm.
qt interval
Represents one complete ventricular cycle—in other words, one complete cycle of ventricular depolarization and repolarization. Measure the QT interval from the beginning of the Q wave to the end of the T wave.
pr segment
Begins at the end of the P wave and ends at the beginning of the Q wave. It represents the time between the end of atrial contraction and the beginning of ventricular contraction. This slight delay is the time period when the AV node has received the impulse from the SA node and slows the impulse to allow the ventricles to fill prior to contracting.
st segment
Represents the early phase of ventricular repolarization. The shape of the ST segment is very important when looking for patterns of ischemia. It starts at the end of the S wave and ends at the beginning of the T wave. It represents the time from the end of ventricular depolarization to the beginning of ventricular repolarization.
the hearts three pacemakers
sa node: the natural, primary pacemaker. within the wall of the ra.
av node: junctional pacemaker, between the artia and ventricles. it fires impulses at a rate of 40-60/min
purkinje fibers: these are the terminal pacemakers of the heart, located in the ventricular myocardium, firing impulses at a rate of 20 to 40/min. this pacemaker is not very effective and only tends to fire when the other two have failed.
sinus dysrhythmias
sinus bradycardia, sinus tachycardia, sinus dysrhythmia & sinus arrest.
sinus dysrhythmia
A variation in heart rate due to changes in the breathing cycle, characterized by alternating periods of faster and slower heart rates.
sinus arrest
A temporary cessation of electrical activity in the heart, leading to a pause in heartbeats. not significant unless arrest lasts longer than 6 seconds.
atrial dysrhythmias
atrial flutter & atrial fibrillation
artial flutter
A type of atrial dysrhythmia characterized by rapid, regular atrial contractions, typically at a rate of 240 to 340 beats per minute, leading to inefficient blood flow.
atrial fibrillation
A common type of atrial dysrhythmia that involves rapid and irregular beating of the atria, resulting in ineffective blood pumping and increased risk of stroke.
junctional dysrhythmias
premature junctional complex (pjc), junctional escape rhythm, accelerated junctional rhythm, junctional tachycardia rhythm, supraventricular tachycardia (svt)/ narrow complex tachycardia
premature junctional complext (pjc)
A type of heart rhythm disturbance originating from the junctional tissue, characterized by an earlier-than-normal heartbeat that disrupts the regular cardiac cycle.
junctional escape rhythm
reflects an impulse originating from the AV junction that is acting as the backup pacemaker. The atria and ventricles receive the impulse simultaneously, which can result in an absent or inverted P wave. The heart rate does not exceed 60/min. The patient might show signs of a decrease in cardiac output due to the slower heart rate and the lack of atrial kick causes in the conduction of the electrical impulse to allow the atria to fill with blood.
accelerated junctional rhythm
the same as the escape rhythm except that the rate is 60 to 100/min. However, it is unlikely that the patient will show signs of a decrease in cardiac output.
junctional tachycardia rhythm
the same as the escape and accelerated rhythm, but the heart rate is 100 to 150/min. The faster the rate, the more likely the patient is to feel palpitations or fluttering.
supraventricular tachycardia
a rapid heart rate originating above the ventricles, typically characterized by a heart rate of 150 to 250 beats per minute. It can result in palpitations, chest pain, or shortness of breath and often requires medical intervention for management.
ventricular dysrhythmias
premature ventricular complexes, ventricular tachycardia, ventricular fibrillation
premature ventricular complexes
are early heartbeats originating in the ventricles, disrupting the normal heart rhythm. They can be benign or indicative of underlying heart disease, often felt as a skipped heartbeat.
ventricular tachycardia
a fast heart rhythm that originates in the ventricles and can lead to serious complications, potentially compromising blood flow.
ventricular fibrillation
a life-threatening condition where the ventricles quiver instead of pumping effectively, leading to ineffective blood circulation and requiring immediate medical intervention.
idioventricular rhythm
is a type of heart rhythm where the ventricles are the primary pacemaker, usually occurring when the heart's normal conduction pathways are disrupted, resulting in a slower heart rate.
agonal rhythm
a very slow and irregular heart rhythm often associated with severe hypoxia or cardiac arrest, indicating a critical state of the heart.
left bundle branch block
is a condition in which there is a delay or blockage along the pathway that electrical impulses travel to the left side of the heart. This can lead to an abnormal heart rhythm and increased risk of heart failure.
right bundle branch block
is a condition characterized by a delay or blockage in the electrical conduction pathway to the right side of the heart, potentially leading to an abnormal heart rhythm and increased risk of heart complications.

1st degree av block
is a condition where there is a prolonged delay in the conduction of electrical impulses from the atria to the ventricles, often observed on an EKG as a longer than normal PR interval.
2nd degree av block type 1
is a condition where there are intermittent failures in the conduction of electrical impulses from the atria to the ventricles, typically seen on an EKG as progressively prolonged PR intervals followed by a dropped QRS complex.
2nd degree av block type 2
is a condition characterized by sporadic failure of electrical impulses from the atria to the ventricles, usually resulting in some QRS complexes being dropped without a progressive change in PR interval length.
3rd degree av block
is a complete block of electrical conduction between the atria and ventricles, leading to a dissociation between the atrial and ventricular contractions. This can be observed on an EKG with independent P waves and QRS complexes.
standard ekg
grid: each small box counts 40milliseconds or 0.04 seconds and each larger box represents 200 milliseconds or 0.2 seconds
speed: 25 mm/second
amplitude: 0.1 mV per mm vertically/10mm per 1 mV
calibration: positively deflected, rectangular standard marking that measures 100mm tall by 5mm wide
einthoven’s triangle
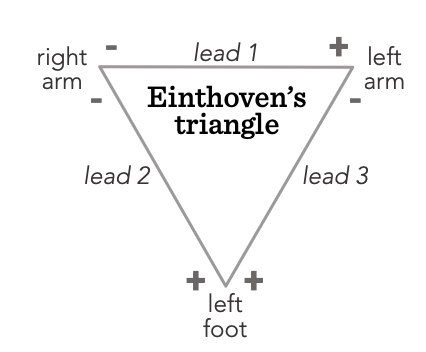
unipolar leads
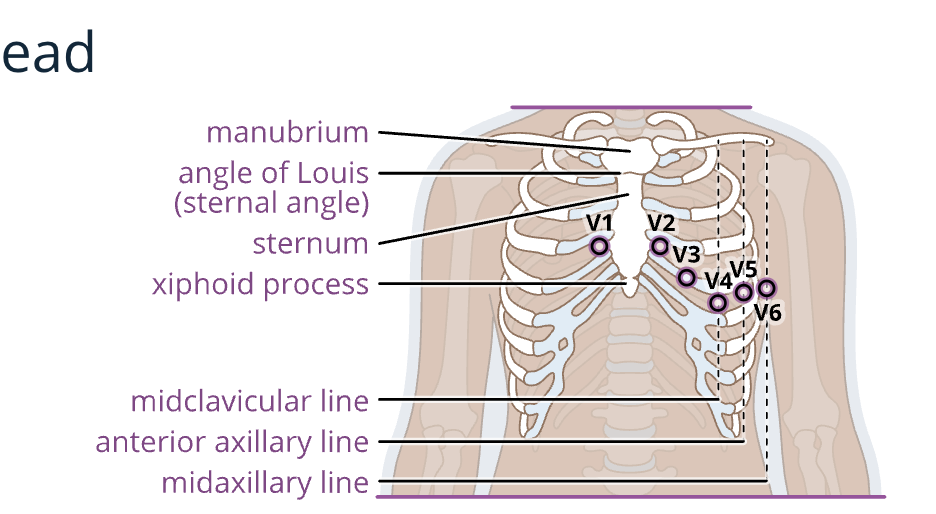
Unipolar leads are those that the machine measures in only one direction. Examples are the precordial or chest leads, V1 to V6.
augmented leads
Augmented leads are also unipolar. The angle of measurement makes the voltage low in these leads, so the machine must make the waveforms larger for them to be readable. The combination of the three augmented leads and the bipolar leads constitute the six limb leads of the EKG. They record activity along the frontal plane relative to the heart as augmented voltage to the right arm (aVr), augmented voltage to the left arm (aVl), and augmented voltage to the left leg or foot (aVf).
bipolar leads
Bipolar leads have two poles: one positive and one negative. The standard limb leads are bipolar, with the EKG tracing measuring and recording the potential difference between the poles. The equilateral triangle these three leads form with the heart in the center is Einthoven’s triangle.
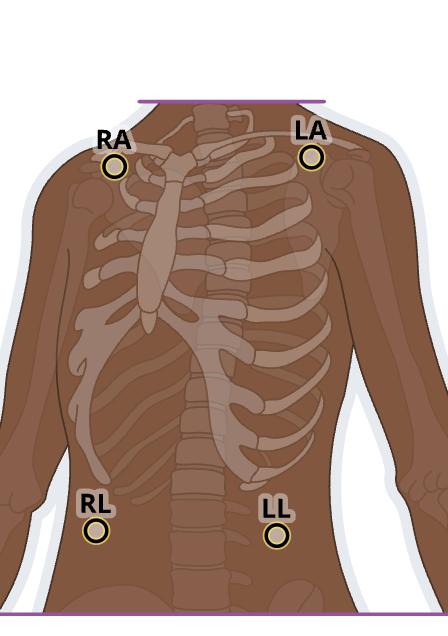
3 lead ekg
white: right shoulder
black: left shoulder
red: left lower abdominal
green: right lower abdominal
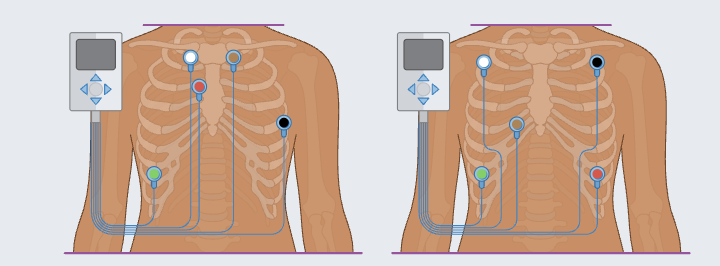
5 lead ekg
white: right sternal border, first rib
red: left sternal border, third rib
black: left side, anterior axillary line, fifth rib
brown: left sternal border, first rib directly opposite the white lead
green: right lower thoracic area anywhere on ribcage
or
white: right chest, about 2in below clavicle
red: left chest, lower rib cage area
black: left chest, opposite of white lead
brown: right chest, fourth rib
green: right lower chest, over a rib
12 lead
white: right arm, 2-3 inches below the clavicle
black: left arm, 2-3 inches below the clavicle
red: left leg, above the ankle
green: right leg, above the ankle
brown: V1, 4th intercostal space, right of sternum
orange: V2, 4th intercostal space, left of sternum
yellow: V3, midway between V2 and V4
purple: V4, 5th intercostal space, left midclavicular line
pink: V5, left anterior axillary line, same level as V4
light blue: V6, left midaxillary line, same level as V4.