Respiratory System
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
90 Terms
What are the four stages of respiration
Pulmonary ventilation
External respiration
Gas Transport
Internal respiration
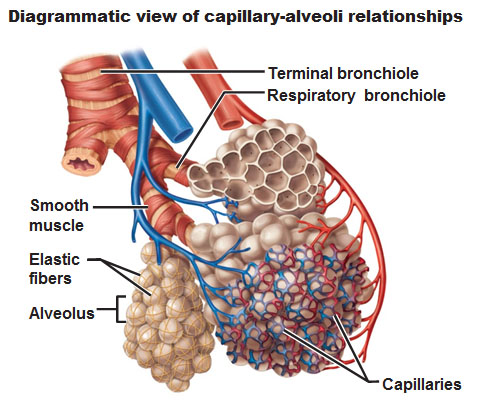
What are the two zones of the respiratory system
Respiratory zone
Conducting zone
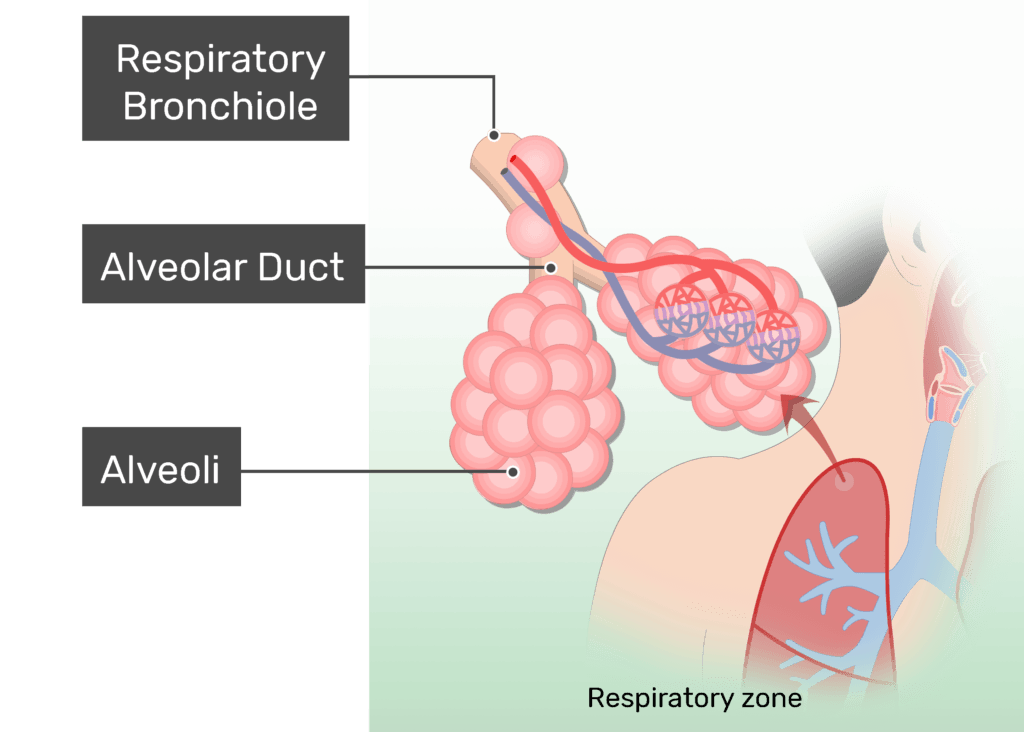
Explain the respiratory zone.
It is the site of gas exchange, consisting of bronchioles, alveolar ducts, and alveoli.
Explain the conducting zone.
IT provides rigid structures for air to reach the sites of gas exchanges, it includes nose, nasal cavity, pharynx, trachea.
What is the function of the nose?
IT provides an airway for respiration and filters , warms the entering air, houses olfactory receptors
Name the structures of the external nose.
Bridge: Connection to frontal bone
Apex: Cartilage tip
Philtrum: Shallow grove inferior to apex
What is the “roof” of the nasal cavity
ethmoid and sphenoid bones f
What is the “floor” of the nasal cavity
Formed by the hard & soft palets
What lines the interior walls of the nasal cavity.
Conchae & nasal mucosa which fiilter, heat, and moisten air.
What are the names of mucosa that line the nasal cavity?
Olfactory mucosa: contains smell receptors
Respiratory mucosa: secretes mucus w/ lysozyme
What are the Paranasal Sinuses?
They are sinuses in bones that surround the nasal cavity, belong to light the skull, warm and moisten the air.
What skin cell are sinus lines with?
Lined with a mucous membrane of
pseudostratified ciliated columnar epithelium
What is the Pharynx
It is the funnel shaped passage of skeletal muscles connecting the nasal cavity and larynx
List the three regions of the Pharynx
Nasopharynx
Oropharynx
Laryngopharynx
Describe the responsibilities of the Nasopharynx.
Acts as an air-only passageway.
Contains the adenoid (pharyngeal) tonsils and openings of the auditory (Eustachian) tubes.
Closes during swallowing to prevent food from entering the nasal cavity.
Describe the responsibilities of the Oropharynx .
Serves as a common passageway for both food and air.
Opens into the oral cavity.
Houses the palatine tonsils, lingual tonsil, and the tongue.
Describe the responsibilities of the Laryngopharynx.
Serves as a common passageway for both food and air.
Extends to the larynx where digestive & respiratory pathways diverge.
What is the larynx and where is it located?
The larynx (voice box) attaches to the hyoid bone, opens into the laryngopharynx above, and is continuous with the trachea below.
What are the three main functions of the larynx?
Provides a patent (open) airway
Acts as a switch to route air and food correctly
Produces sound for voice (not speech)
What are the 3 main cartilages of the larynx?
Thyroid cartilage – largest, forms Adam’s apple
Cricoid cartilage – ring-shaped, under thyroid cartilage
Arytenoid, cuneiform, corniculate – small paired cartilages
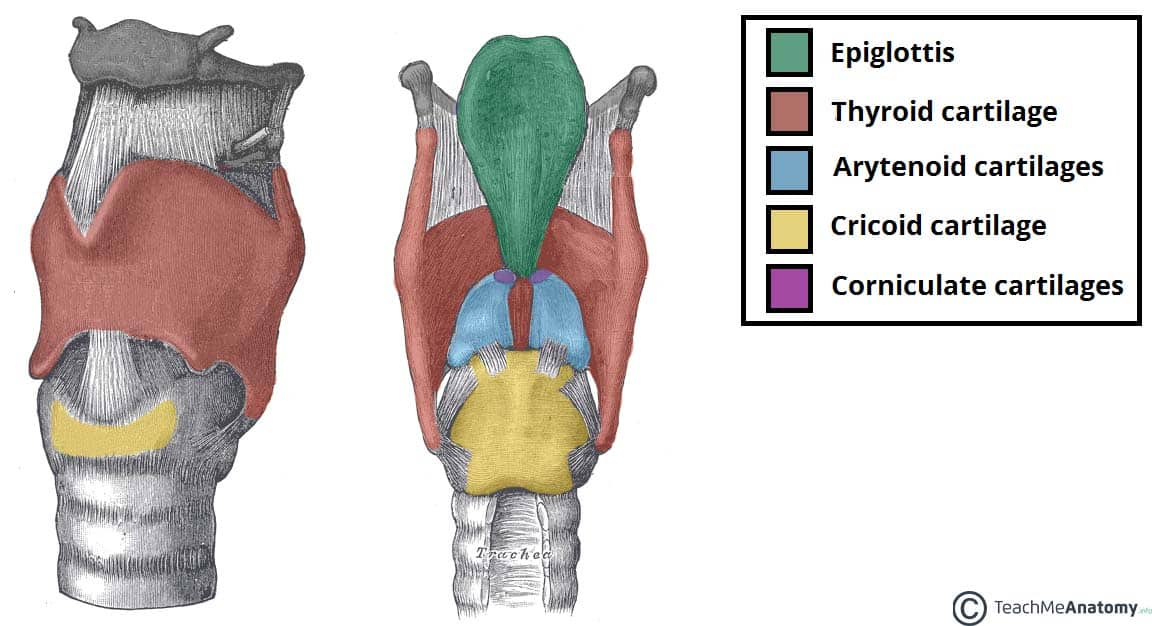
What is the function of the epiglottis?
The epiglottis is elastic cartilage that covers the glottis during swallowing to prevent food from entering the airway.
What are the three layers of the trachea
Mucosa: ciliated epithelium
Submucosa: connective tissue under mucosa
Adventitia
What is the mucocillary escalator?
A mechanism that uses cilia to transport mucus up the trachea to the throat.
What do vocal ligaments connect and what are they made of?
They connect arytenoid cartilages to thyroid cartilage and are made of elastic fibers that form the true vocal cords.
What is the glottis?
The glottis is the medial opening between the true vocal cords, where sound is produced as air passes through.
What are false vocal cords (vestibular folds)?
They are mucosal folds located above the true vocal cords and do not contribute to sound production.
How is speech produced?
Speech occurs through intermittent release of expired air while the glottis opens and closes.
What determines the loudness of the voice?
Loudness depends on the force of air rushing across the vocal cords.
What determines the pitch of the voice?
Pitch is determined by the length and tension of the vocal cords.
When is the larynx closed?
During coughing, sneezing, and Valsalva’s maneuver.
What is Valsalva’s maneuver?
A maneuver where the glottis is closed and abdominal muscles contract to increase intra-abdominal pressure.
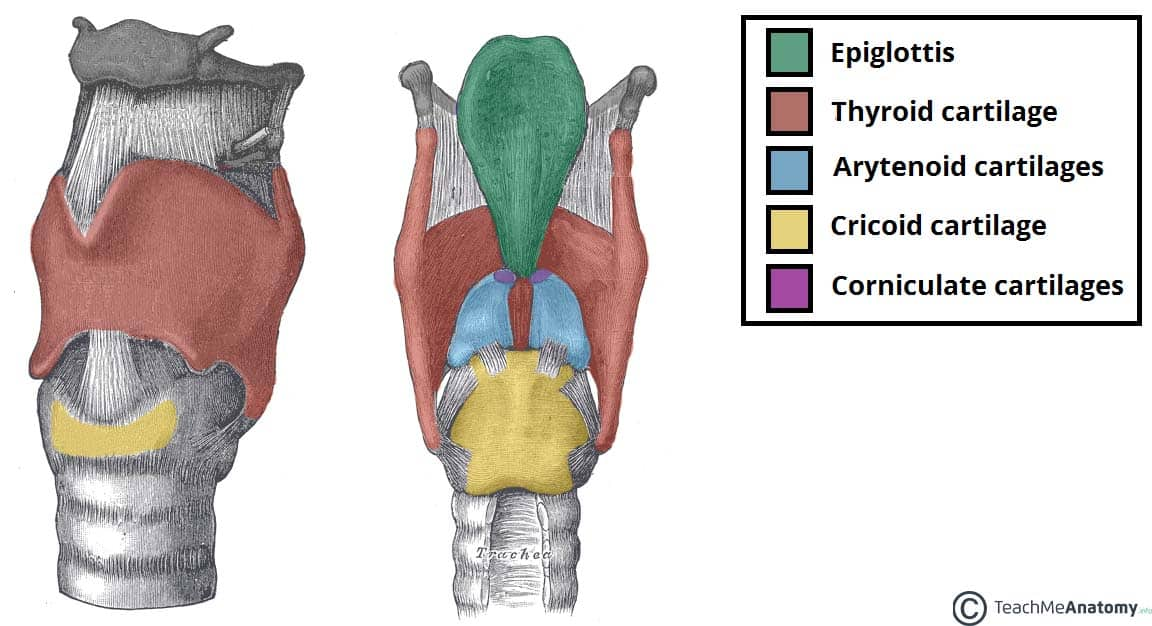
What forms the bronchial tree?
The bronchial tree is formed by the branching of the trachea.
What are the primary bronchi?
The right and left bronchi; the right is shorter, wider, and more vertical than the left.
How do bronchi branch within the lungs? (SEQ)
Primary bronchi → Secondary (2°) bronchi (to each lung lobe) → Tertiary (3°) bronchi (to lung segments)
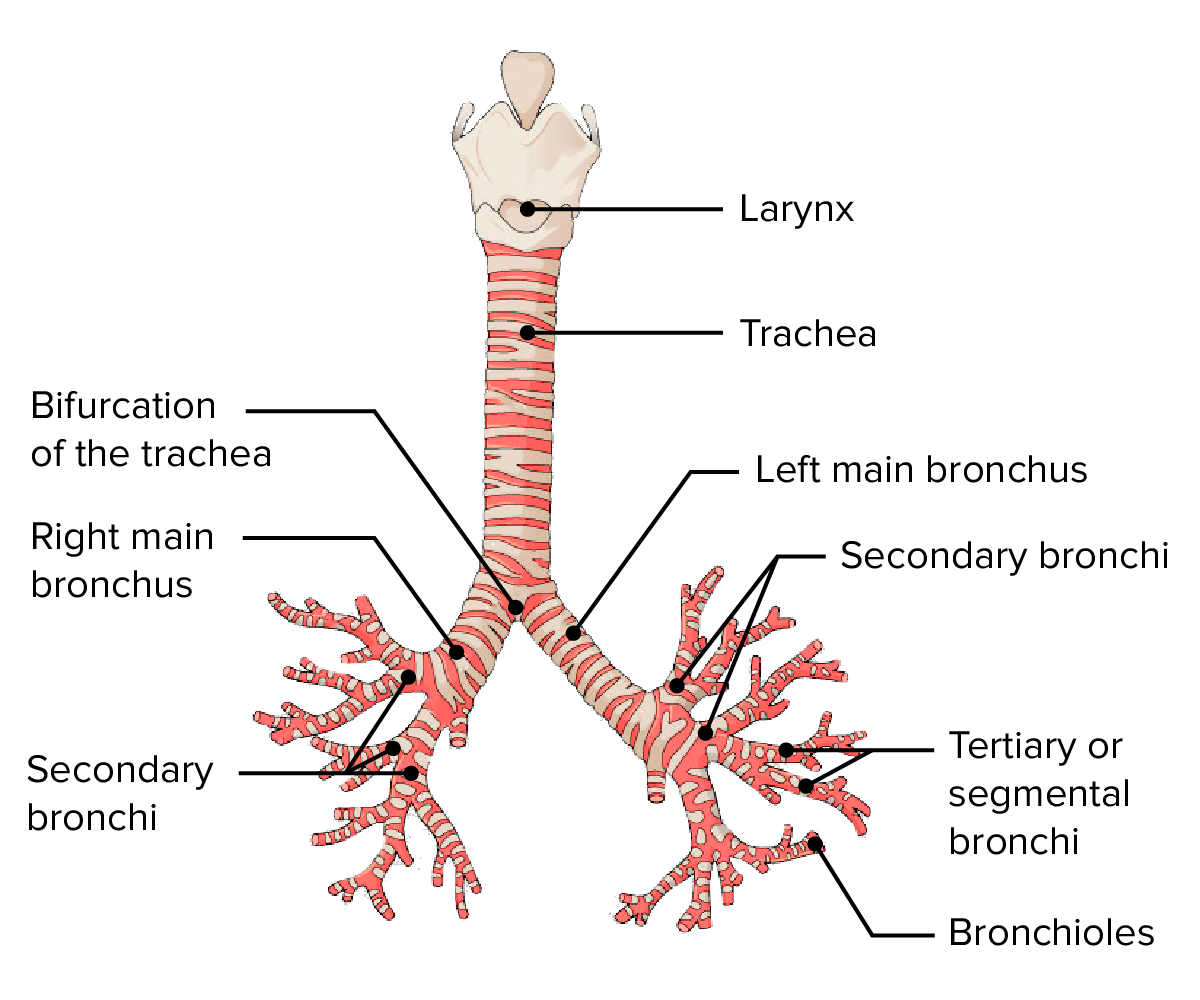
What are terminal bronchioles?
The smallest branches of the bronchi, made of cuboidal epithelium, with smooth muscle but no cartilage or mucus-producing cells.
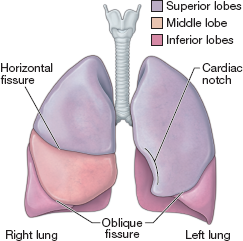
Which lung is slightly bigger and has more lobes
The right lung has 3 lobes and is bigger, left has 2 lobes.
Where does the respiratory zone begin?
Where alveoli are present. Terminal bronchioles feed into respiratory bronchioles, which lead to alveolar ducts and then alveolar sacs.
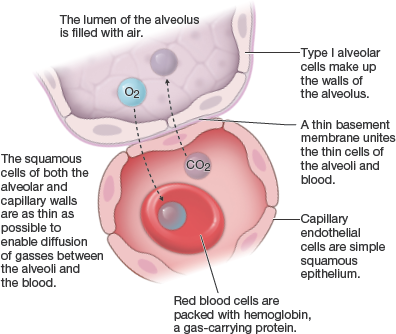
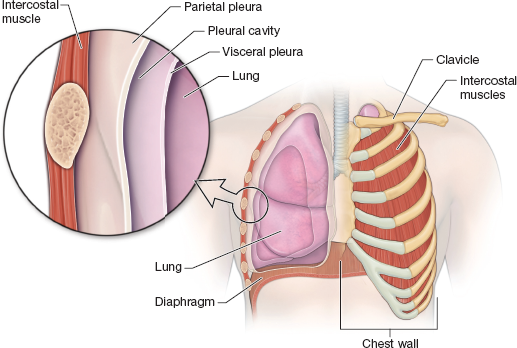
What composes the Respiratory Membrane? (Air-Blood Barrier)
Alveolar walls – very thin to allow gas exchange by simple diffusion.
Capillary walls – closely associated with alveoli.
Fused basement membranes – connect alveolar and capillary walls.
Also present in alveoli:
Type II cells – secrete surfactant to reduce surface tension and prevent alveolar collapse.
Type III cells – alveolar macrophages that remove debris and pathogens.
What are Alveoli?
Alveoli are hollow spheres with open pores that connect to other alveoli. These pores help equalize air pressure throughout the lungs and allow for efficient gas exchange.
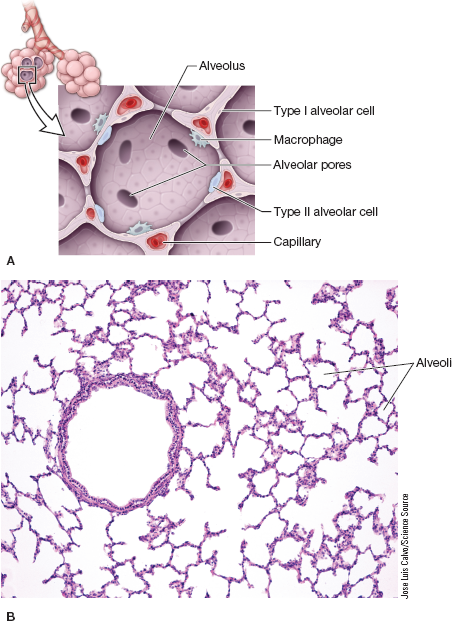
What kind of skin cell makes up alveoli?
Single layer squamous epithelium cells.
Describe the gross anatomy of the lung. (Root, Hilus, Apex, Base, Cardiac notch)
Root: site of vascular and bronchial attachments
Hilus: indentation that contains pulmonary & systemic blood vessels
Apex: narrow superior tip; projects above the clavicles
Base: inferior surface that rests on the diaphragm
Cardiac notch: indentation on the medial surface of the left lung that accommodates the heart
What 2 circulations are responsiuble for perfusing the lungs w/ blood? (O2 & CO2)
Pulmonary
Bronchial
Describe the pulmonary circulation in the lungs.
Pulmonary arteries carry deoxygenated blood from the heart to the lungs, feeding the capillary networks around alveoli for gas exchange. Pulmonary veins carry oxygenated blood from alveoli back to the heart.
Describe the Bronchial circulation in the lungs.
Bronchial circulation oxygenates the lung tissues. (except the alveoli). Bronchial arteries supply oxygenated blood to structures like the bronchi and bronchioles.
Can you list the 2 layers that make up the pleurae ( lung walls)
Parietal pleura: Lines thoracic cavity, forming outer layer of pleural sac
Visceral pleura: covers the external surface of the lungs, directly attached to lung tissue.
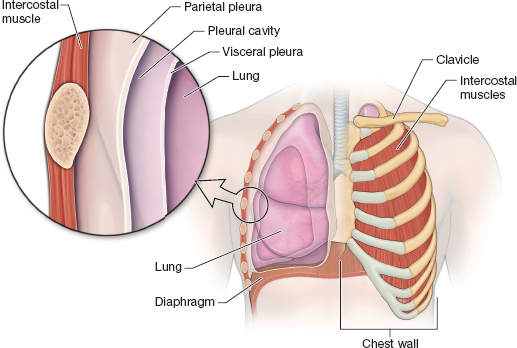
What is the pleural cavity and its function?
The pleural cavity is the space between the parietal and visceral pleurae.
It contains serous fluid that reduces friction during breathing.
The negative pressure in this cavity helps the lungs expand as the thoracic cavity moves.
What is the relationship between volume and pressure?
Boyle’s Law, Volume changes lead to pressure changes, which
lead to the flow of gases to equalize pressure
Sequence the steps of Inspiration
Diaphragm & Intercostal muscles contract, ribcage rises
Lungs become stretched, increasing intrapulmonary volume and decreasing IP pressure below atm (-1mm Hg)
Air flows into the lungs down the pressure gradient until IP pressure equals atmospheric pressure.
Sequence the steps of Expiration
Diaphragm & intercostal muscles relaxes, ribcage descends
Intrapulmonary Volume decrease and IP pressure increases above atm pressue (+1 mm Hg)
Air flows out of lungs until atm and IP pressures equalize.
What is Forced Inspiration?
The use of additional muscles to increase Intrapulmonary Volume like scalene, pectoralis minor,
What is Forced Expiration?
The use of additional muscles to decrease Intrapulmonary volume like Transverse & oblique muscles
What is intrapulmonary pressure (Ppul)?
It is the pressure within the alveoli that always equalizes with atmospheric pressure eventually.
What is intrapleural pressure (Pip)?
It is the pressure within the pleural cavity and is always less than both intrapulmonary and atmospheric pressure.
What causes Lung Collapse?
IT is caused by the equalization intrapleural pressure (Pip) with intrapulmonary pressure (Ppul)
What is transpulmonary pressure and why is it important?
Transpulmonary pressure = Ppul – Pip; it keeps the airways open, avoid lung collapse.
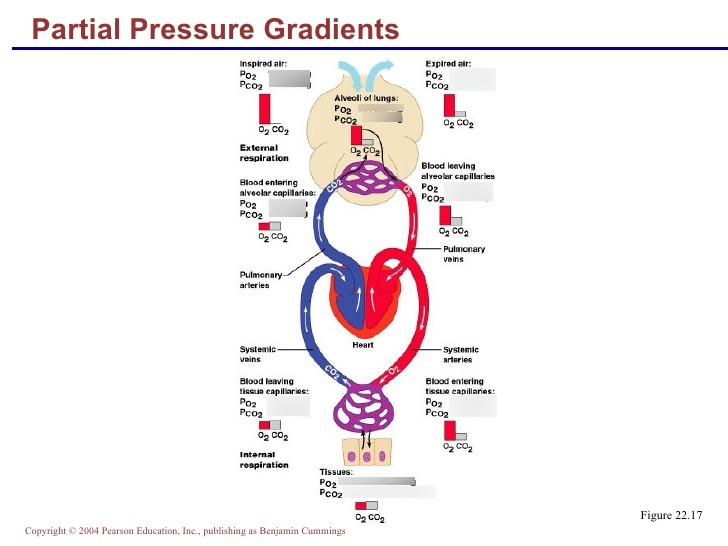
Explain the O2 partial pressure gradient in the lungs.
O2 = 40mm Hg of partial pressure in the venous blood
Alveoli = 104 mm Hg of partial pressure
This steep gradient causes O2 to move from alveoli to capillaries
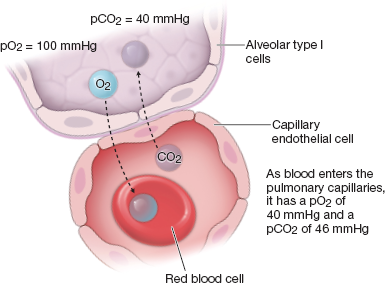
Explain the CO2 partial pressure gradient in the lungs.
CO2 = 45mm HG of partial pressure in the blood
Alveoli = 40mm Hg of partial pressure
This gradient causes co2 to move from blood to alveoli
How does solubility assist CO2 leaving the blood?
CO₂ is highly soluble in plasma, meaning it dissolves easily in the blood and diffuses readily into the alveoli, even though its partial pressure gradient is smaller than that of oxygen.
What is Dalton’s law of Partial Pressure?
Dalton’s Law states that the total pressure of a gas mixture is the sum of the partial pressures of each individual gas. Each gas exerts pressure independently, proportional to its percentage in the mixture.
A higher concentration of a gas results in greater pressure contribution.
What is Henry’s Law
Henry’s Law states that gases will dissolve in a liquid in proportion to their partial pressure, solubility, and the temperature of the liquid.
Higher pressure or solubility increases gas dissolution, while higher temperature usually decreases it.
What is internal respiration?
Exchange of gases between blood in the systemic capillaries and body tissues.
Oxygen (O₂) diffuses from the blood into the tissues, because tissue cells have a lower Partial Pressure O₂.
Carbon dioxide (CO₂) diffuses from the tissues into the blood, because tissues have a higher Partial Pressure CO₂.
What is ventilation in the lungs?
movement of air into and out of the lungs
What is perfusion in the lungs?
flow of blood in the pulmonary capillaries reaching the alveoli.
What happens to bronchioles when alveolar CO2 levels are high?
Bronchioles dilate to increase airflow.
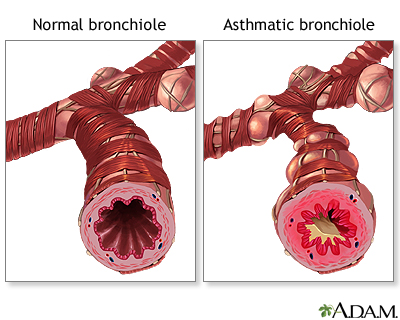
What happens to bronchioles when alveolar CO2 levels are low?
Bronchioles constrict to reduce airflow.
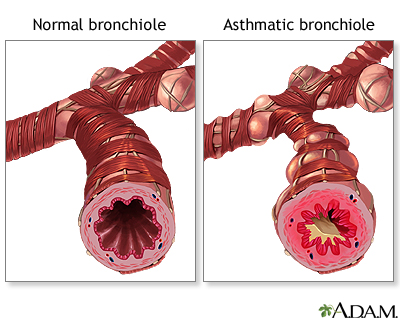
What is the result of changing diameters in bronchioles and arterioles?
Synchronization of alveolar ventilation and pulmonary perfusion, optimizing gas exchange.
What is hemoglobin and how does it carry oxygen?
Its a protein in red blood cells that binds up to four oxygen molecules in a rapid, reversible process.
When all four heme groups are bound to oxygen, it’s fully saturated; with fewer, it’s partially saturated.
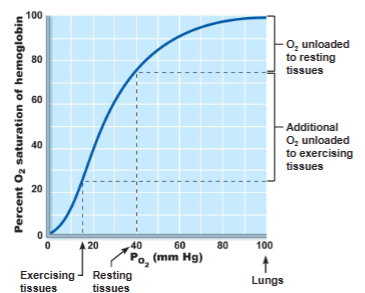
What is the oxygen—hemoglobin dissociation curve?
a graph that plots the percentage of oxygen saturation of hemoglobin vs the partial pressure of oxygen
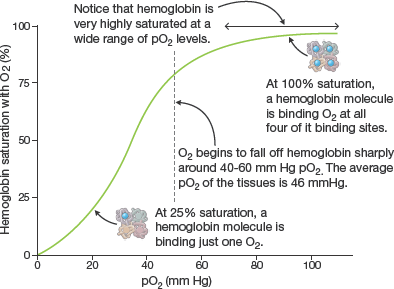
What stands out about the plateau in the hemoglobin dissociation curve?
The plateau of the curve (at PO₂ ~70–100 mmHg) shows that hemoglobin remains highly saturated with oxygen even if oxygen levels drop slightly.
What factors other than PO₂ affect the oxygen–hemoglobin dissociation curve
Temperature, H⁺ (pH), PCO₂, and BPG all influence hemoglobin’s affinity for oxygen by modifying its structure.
How do increases in temperature, H⁺, PCO₂, and BPG affect hemoglobin’s oxygen binding?
They decrease hemoglobin’s affinity for oxygen, enhancing oxygen unloading in tissues.
Why does hemoglobin release more oxygen in areas with high temperature or metabolism?
Higher temperatures (from active cellular respiration) promote hemoglobin-oxygen dissociation, making oxygen more available to cells.
What happens to oxygen unloading when temperature, H⁺, PCO₂, and BPG levels decrease?
Hemoglobin’s affinity for oxygen increases, reducing oxygen unloading.
What is an example of hemoglobin releasing more oxygen in areas with high temp/metabolism?
During exercise, active muscles generate heat and CO₂, lowering pH and increasing temperature—causing hemoglobin to release more oxygen where it’s most needed.
How does active metabolism in cells affect oxygen unloading from hemoglobin?
As cells metabolize glucose, they release CO₂ and heat, which increases PCO₂, H⁺, and temperature—lowering blood pH (Bohr effect) and promoting BPG synthesis in RBCs. These changes decrease hemoglobin’s affinity for O₂, enhancing oxygen unloading to tissues.
Example: Actively contracting muscles during exercise produce more CO₂ and heat, ensuring they get more oxygen from hemoglobin.
What are the three forms in which carbon dioxide (CO₂) is transported in the blood?
Dissolved in plasma – 7–10%
Chemically bound to hemoglobin – ~20% as carbaminohemoglobin
As bicarbonate ion (HCO₃⁻) – ~70%, formed in red blood cells and transported in plasma
What is the Haldane effect?
Reduced hemoglobin has a greater ability to bind CO₂ and buffer H⁺. This means that as O₂ is released, hemoglobin can carry more CO₂.
How does the Bohr effect relate to CO₂ transport?
Increased CO₂ and H⁺ in tissues causes hemoglobin to release O₂ more readily, promoting oxygen unloading where it’s needed.
What happens to CO₂ in red blood cells?
CO₂ + H₂O → H₂CO₃ (carbonic acid) → H⁺ + HCO₃⁻ (bicarbonate)
This reaction is catalyzed by carbonic anhydrase.
What happens to bicarbonate in tissues?
Bicarbonate diffuses out of RBCs into plasma. To maintain charge balance, chloride ions (Cl⁻) move into RBCs — this is called the chloride shift.
What happens to CO₂ transport in the lungs?
The process reverses:
Bicarbonate re-enters RBCs,
Combines with H⁺ to form carbonic acid,
Which breaks down into CO₂ and H₂O,
CO₂ is then exhaled.
What are the 2 Medullary Respiratory Centers?
Ventral respiratory group (VRG)
Dorsal respiratory group (DRG)
Explain the responsibility of Ventral respiratory group (VRG)
It is the rhythm-generating center & controls nerves:
Inspiratory neurons excite the diaphragm via phrenic nerve and intercostal muscles via intercostal nerve
Expiratory neurons inhibit the inspiratory neurons
Explain the responsibility of Dorsal respiratory group (DRG)
It receives input from chemoreceptors and sends it to the VRG
How does PCO₂ affect depth and rate of breathing?
Rising PCO₂ (hypercapnia) increases breathing rate and depth.
CO₂ diffuses into cerebrospinal fluid, forming carbonic acid → H⁺.
H⁺ is not buffered in CSF, so chemoreceptors in the brainstem respond strongly.
Main regulator of breathing at rest.
How does arterial pH affect breathing if CO₂ and O₂ are normal?
Decreased pH (acidosis) stimulates increased breathing rate and depth.
Causes: CO₂ retention, lactic acid buildup, or excess ketones (e.g., in diabetes).
Respiratory system compensates by "blowing off" CO₂ to raise pH.
When does PO₂ become a major stimulus for breathing?
When arterial PO₂ drops below 60 mmHg.
Detected by aortic and carotid bodies.
Triggers hypoxic drive to increase ventilation.
How do chemoreceptors detect changes in PCO₂?
Chemoreceptors in the brainstem detect H⁺ from CO₂ conversion in CSF.
This prompts increased ventilation to expel excess CO₂.
How do hypothalamic controls influence breathing?
They act through the limbic system to change respiratory rate and depth.
Examples: Breath holding during anger or emotional stress, gasping in pain.
Increased body temperature → faster breathing.
What are corex controls of respiration?
They are voluntary controls from the cerebral motor cortex that can bypass the medulla.
Examples: Voluntarily holding your breath, conscious deep breathing