Chapter 14 Anatomy 1
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
Spinal Cord and Spinal Nerves Functions:
Primary Function: Link the Brain and Body
Serves as a structural and functional connection between the brain and the rest of the body.
Relays sensory input (from receptors like skin/muscle/joint sensors) to the brain for interpretation.
Relays motor output (initiated in the brain) to effectors (muscles and glands) to control movement (e.g., walking, picking up an object).
Information travels along neuron pathways through the spinal cord and spinal nerves
Spinal Cord and Spinal Nerves Functions:
Secondary Function: Spinal Reflexes
Involves spinal reflexes, which are nervous system responses that do not require the brain.
The spinal cord acts as the integration center for these reflexes, demonstrating functional independence.
Initiates the quickest reactions to a stimulus (e.g., rapidly pulling hand away from a hot stove).
Conscious perception (e.g., feeling pain) only occurs after the sensory input reaches the brain.
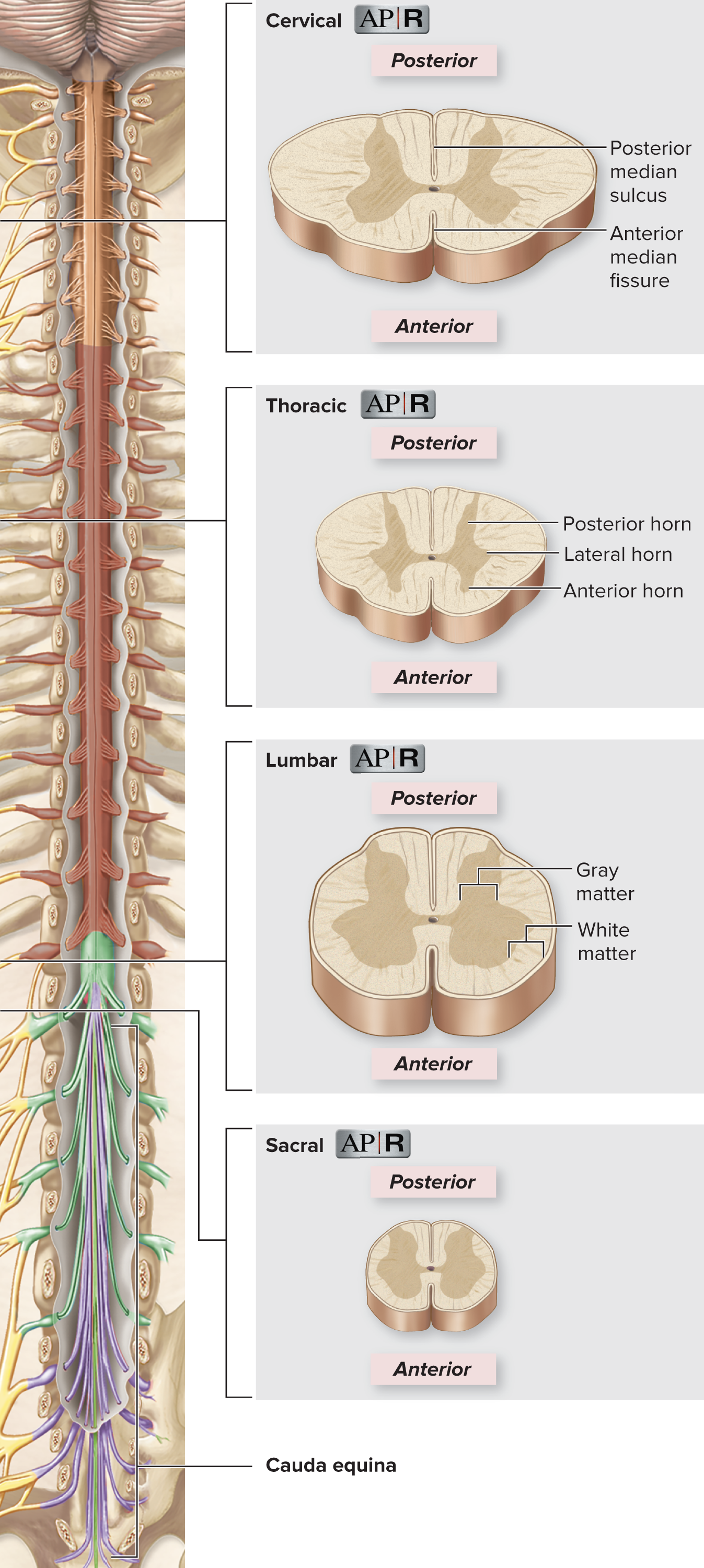
Spinal Cord Location and Shape:
The spinal cord is a roughly cylindrical structure (slightly flattened front-to-back).
It extends from the medulla oblongata (brain) down through the vertebral column.
It typically ends at the L1 vertebra (does not extend the full length of the vertebral column).
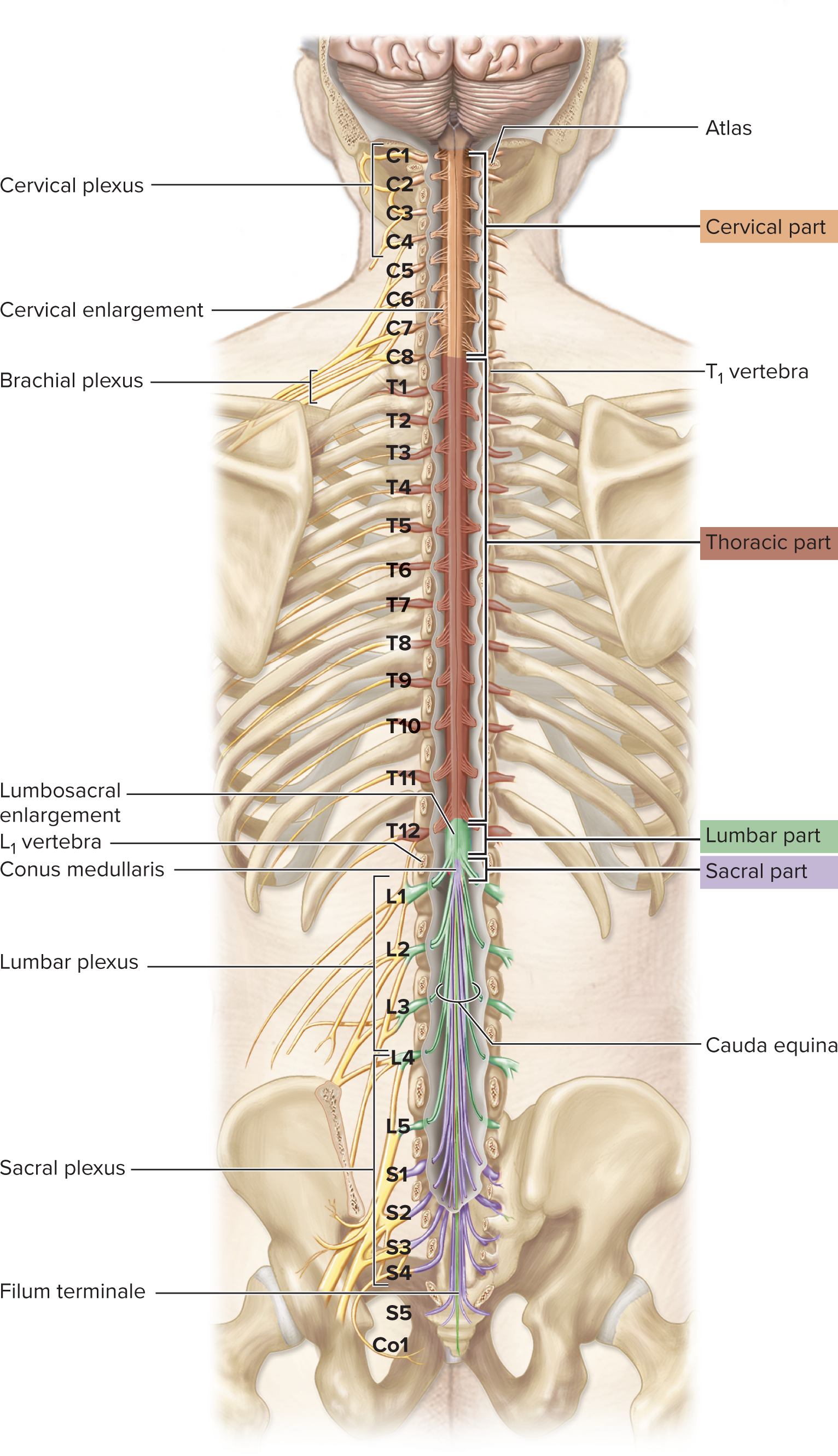
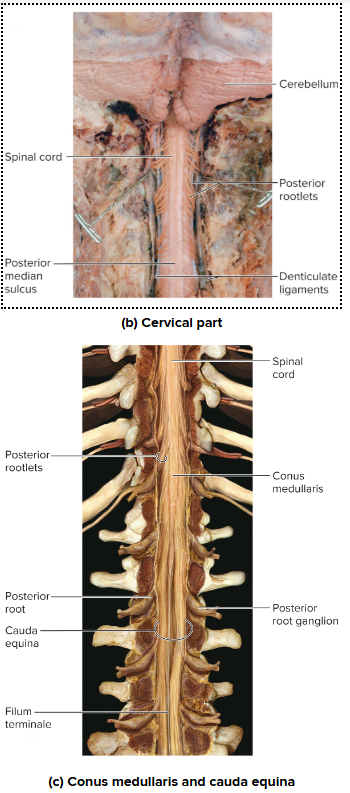
Spinal Cord, Inferior Structures:
The inferior end narrows to form the conus medullaris (cone-shaped end).
Inferior to the conus medullaris, the roots of the lumbar, sacral, and coccygeal nerves form the cauda equina ("horse's tail").
The filum terminale (a thin strand of pia mater) anchors the conus medullaris to the coccyx.
Spinal Cord, Dimensions and Surface Features:
The spinal cord is typically 16 to 18 inches (42–45 cm) long and about 3/4 inch wide.
It has two grooves running its length: the posterior median sulcus (narrow) and the anterior median fissure (wider).
Spinal Cord, Five Parts (Regions):
The spinal cord is subdivided into five parts, each containing neurons for its associated spinal nerves (sensory and motor):
Cervical: Superiormost, continuous with the medulla.
Thoracic: Inferior to the cervical part.
Lumbar: Shorter segment.
Sacral: Inferior to the lumbar part.
Coccygeal: Most inferior tip.
Spinal Cord, Enlargements (Wide Areas):
Cervical enlargement: Wider area in the cervical part; contains extra neurons for the upper limbs.
Lumbosacral enlargement: Wider area in the lumbar/sacral parts; contains extra neurons for the lower limbs.
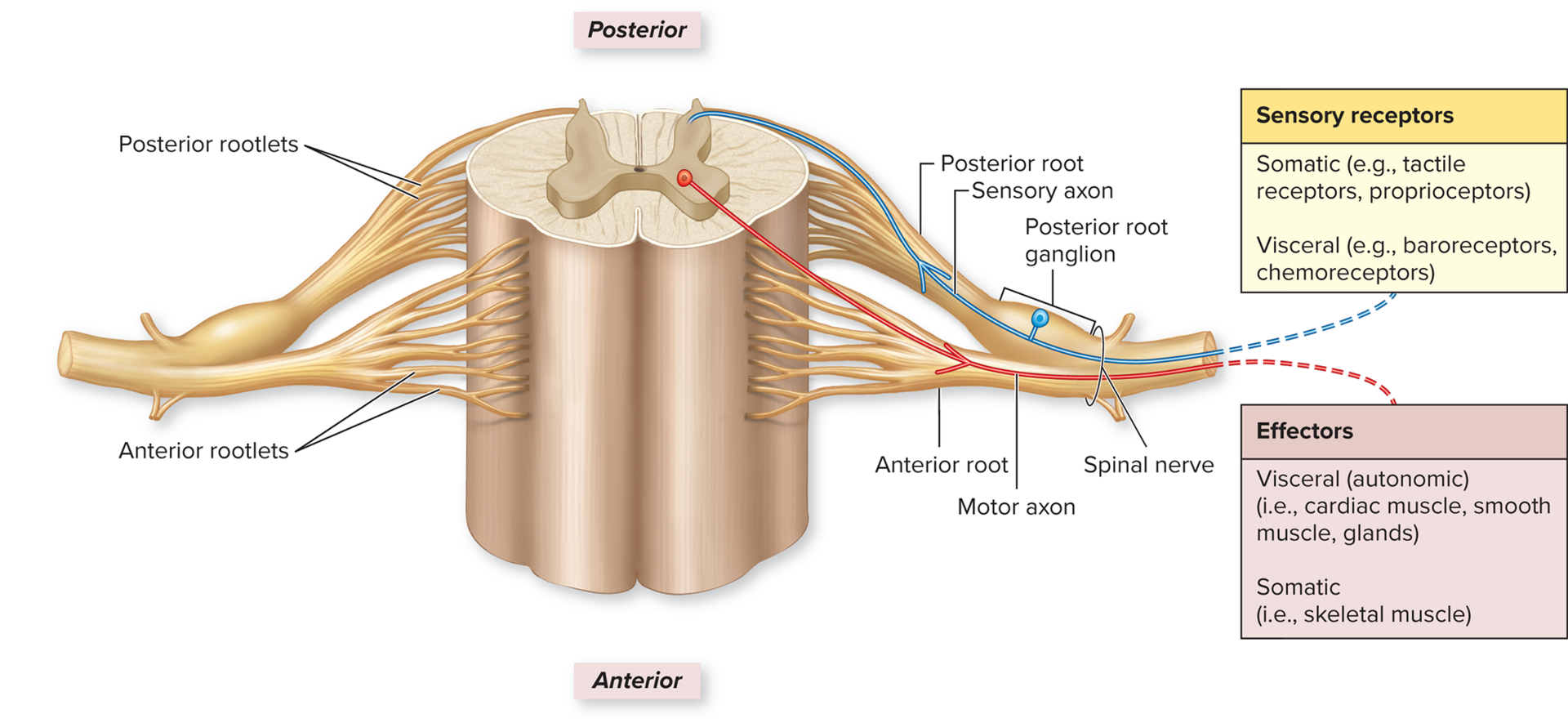
Spinal Nerves, General Nerve Structure:
A nerve is a cable-like organ made of a bundle of axons.
It has three connective tissue coverings (like layers of insulation):
Epineurium: Ensheaths the entire nerve.
Perineurium: Encloses a fascicle (bundle of axons).
Endoneurium: Electrically insulates each individual axon.
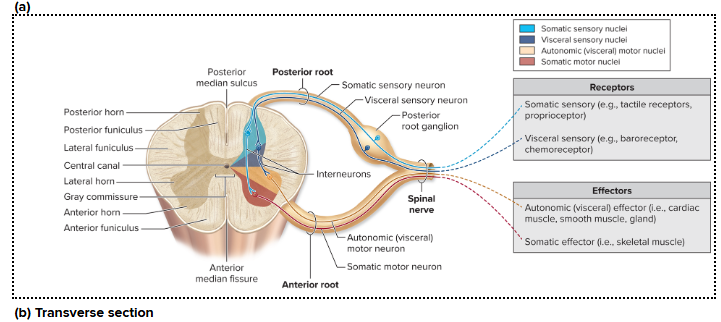
Somatic receptors:
Somatic (tactile receptors, proprioceptors)
Visceral (baroreceptors, chemoreceptors.
Effectors:
Visceral (autonomic) (cardiac muscle, smooth muscle, glands)
Somatic (skeletal muscle)
Spinal Nerves, Naming and Number of Spinal Nerves:
There are 31 pairs of spinal nerves, named by the spinal cord region they attach to:
Cervical (C): 8 pairs (C1–C8).
Thoracic (T): 12 pairs (T1–T12).
Lumbar (L): 5 pairs (L1–L5).
Sacral (S): 5 pairs (S1–S5).
Coccygeal (Co): 1 pair (Co1).
Cranial nerves (from the brain) are named differently (e.g., CN I or olfactory nerve).
A nerve plexus (e.g., brachial plexus) is a network formed by groups of spinal nerves.
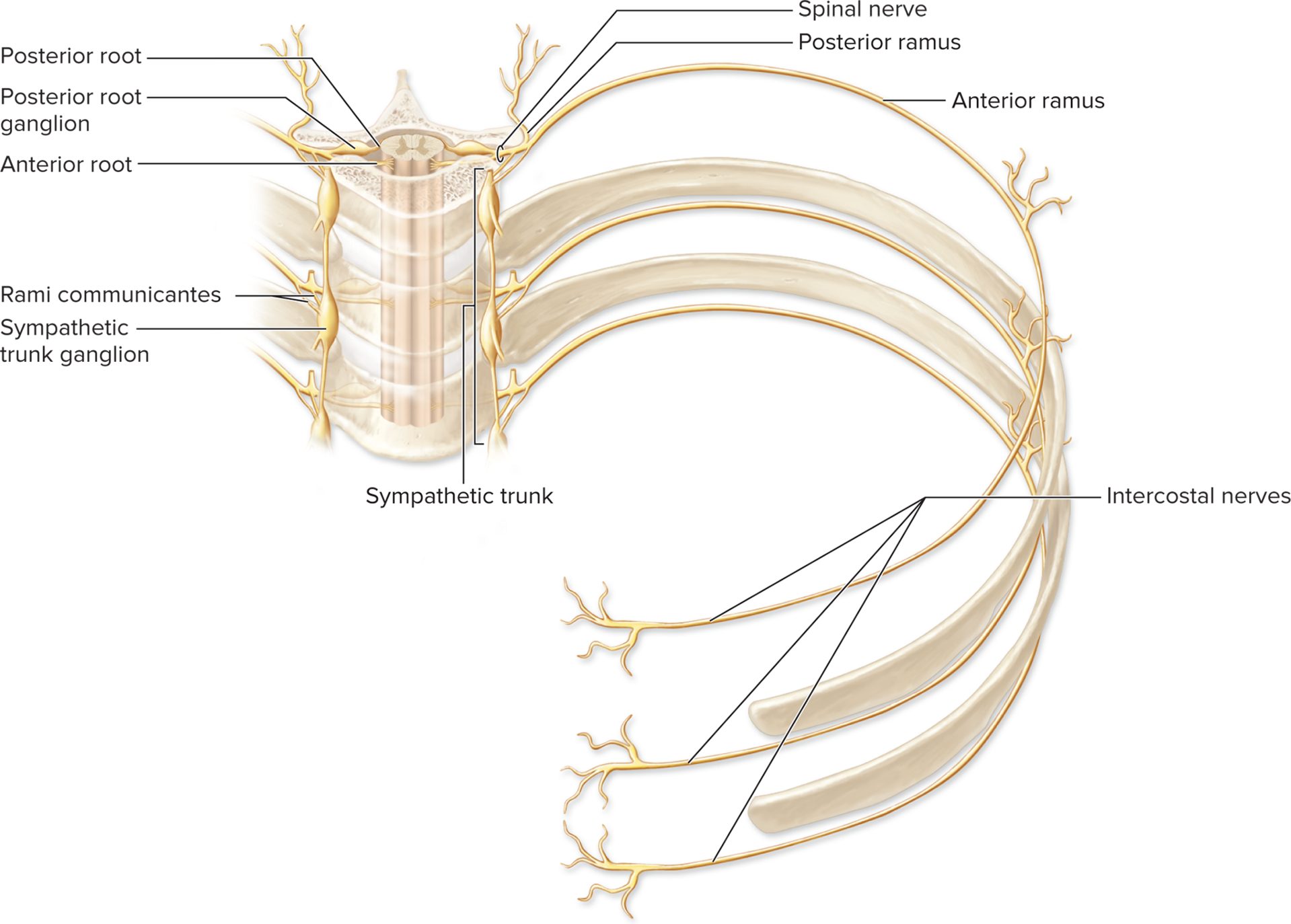
Spinal Nerves, Gross Anatomy of a Spinal Nerve:
Each spinal nerve attaches to the spinal cord via two roots: the posterior root and the anterior root.
Spinal nerves are mixed nerves because they contain both sensory and motor axons.
Component | Content | Neuron Type | Location of Cell Body | Function |
Posterior Root | Sensory axons | Unipolar | Posterior Root Ganglion (external to the spinal cord) | Relays sensory input to the spinal cord. |
Anterior Root | Motor axons | Multipolar | Within the spinal cord | Relays motor output from the spinal cord to effectors (muscles/glands). |
Spinal Nerves, Cauda Equina:
Because the spinal cord ends high (at L1 vertebra) as the conus medullaris, the roots for the lower nerves must travel down.
The cauda equina ("horse's tail") is the bundle of descending anterior and posterior nerve roots that form the lower spinal nerves (most lumbar, all sacral, and all coccygeal).
It contains both sensory and motor components.
The spinal cord is protected by three main components:
bone (vertebral column), connective tissue layers (meninges), and fluid (cerebrospinal fluid).
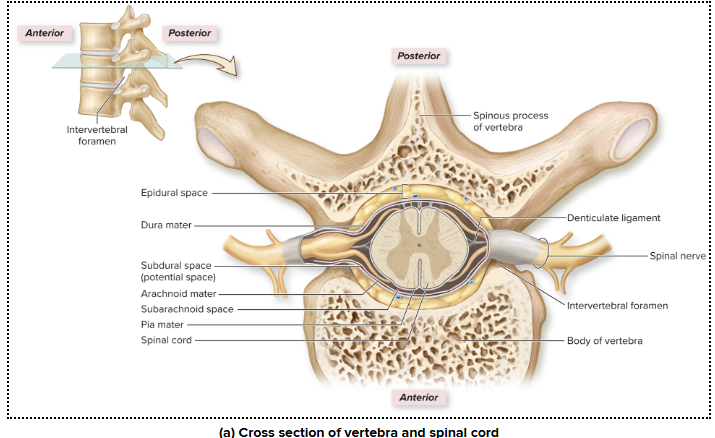
Bony Protection (Vertebral Column)
The vertebral column (26 stacked vertebrae and intervertebral discs) is the bony protection for the spinal cord.
The stacked vertebral openings form the vertebral canal, which houses the spinal cord and cauda equina.
Important Discrepancy: The spinal cord segments (e.g., Lumbar part of the cord) do not align exactly with the vertebrae of the same name because the spinal cord stops growing before the vertebral column does.
Spinal Nerve Exit
Each spinal nerve exits the vertebral canal through an intervertebral foramen (a lateral opening between adjacent vertebrae).
Cervical Nerves (C1–C7): Exit superior to the vertebra of the same number.
Cervical Nerve 8 (C8) and all nerves inferior to it (T1, L1, etc.): Exit inferior to the vertebra of the same number.
The roots for lower nerves (lumbar, sacral, coccygeal) must travel down as the cauda equina before exiting.
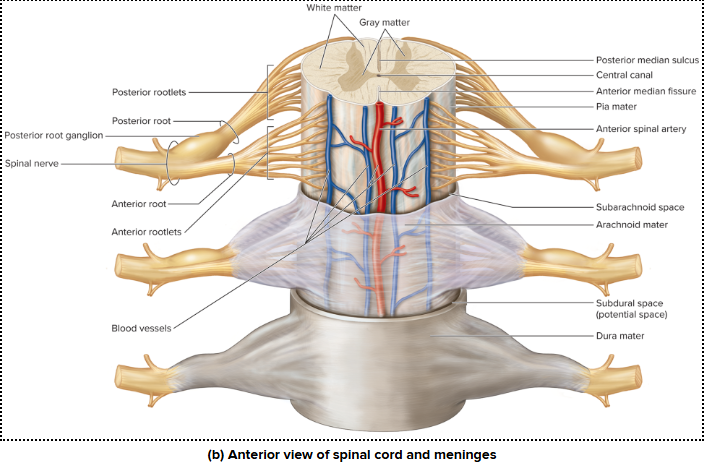
Spinal Meninges and Spaces (Outermost to Innermost)
The meninges are continuous connective tissue membranes that protect the spinal cord.
Vertebra (Bone)
Epidural Space:
Location: Between the dura mater and the inner bone of the vertebra.
Content: Contains connective tissue, fat (adipose), and blood vessels.
Clinical Use: Site for administering anesthetics or steroids.
Dura Mater (Tough Mother):
Outermost meningeal layer; made of dense irregular connective tissue.
Has only one layer (unlike the brain's dura mater).
Subdural Space:
A potential space between the dura mater and the arachnoid mater.
Arachnoid Mater (Spider Mother/Web-like):
Middle layer; contains fine fibers called arachnoid trabeculae.
Subarachnoid Space:
Location: Deep to the arachnoid mater.
Content: Cerebrospinal fluid (CSF) circulates here.
Clinical Use: CSF can be removed via a lumbar puncture for testing.
Pia Mater (Tender Mother):
Innermost layer; thin layer of connective tissue that adheres directly to the spinal cord surface.
Forms the denticulate ligaments that anchor the spinal cord laterally.
Forms the filum terminale that anchors the cord's inferior tip to the coccyx.
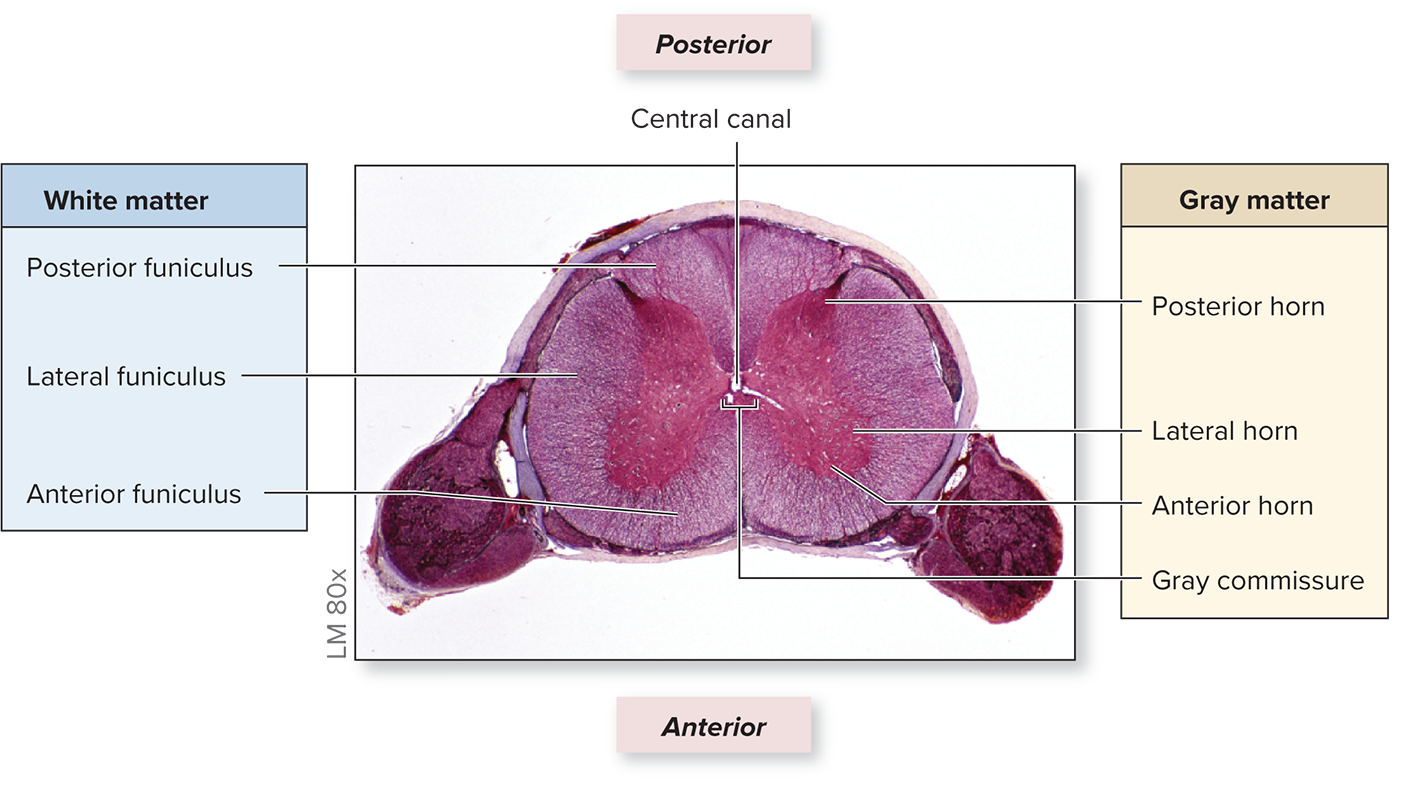
Spinal Cord in Cross-Section (Internal View)
When viewed in a cross-section, the spinal cord is a roughly cylindrical structure that is slightly flattened on the front and back.
Spinal Cord in Cross-Section (Internal View)
It has two visible grooves:
Posterior median sulcus: A narrow groove on the back side.
Anterior median fissure: A slightly wider groove on the front side.
The spinal cord is internally divided into two main areas:
Inner Gray Matter: Contains cell bodies and unmyelinated axons.
Outer White Matter: Contains myelinated axons.
Spinal Cord Gray Matter Structure and Function
The spinal cord's gray matter is centrally located, shaped like an "H" or a butterfly, and functions primarily as a processing center. It mainly consists of neuron dendrites and cell bodies.
H-Shaped Subdivisions (Horns)
The gray matter is divided into horns (on each side) and a connecting bar (commissure):
Subdivision | Contents & Location | Function/Type of Neuron |
Posterior Horns | Dendrites and cell bodies of Interneurons. | Sensory Processing: Where sensory neurons synapse (connect) with interneurons. |
Anterior Horns | Dendrites and cell bodies of Somatic Motor Neurons. | Voluntary Movement: Axons control skeletal muscle (conscious movement). Targeted by poliovirus. |
Lateral Horns | Dendrites and cell bodies of Autonomic Motor Neurons. | Involuntary Control: Axons control autonomic effectors (cardiac muscle, smooth muscle, glands). Only found in spinal segments T1–L2. |
Sensory and Motor Nuclei
Posterior Horn Nuclei (Sensory Input):
Somatic Sensory Nuclei: Receives input from somatic sensory neurons (e.g., touch receptors in skin/limbs).
Visceral Sensory Nuclei: Receives input from visceral sensory neurons (e.g., receptors in internal organs).
Anterior Horn Nuclei (Motor Output):
Somatic Motor Nuclei: Controls voluntary skeletal muscle.
Lateral Horn Nuclei (Motor Output):
Autonomic Motor Nuclei: Controls involuntary smooth muscle, cardiac muscle, and glands.
Connecting Structures (Gray Commissure)
Gray Commissure: A horizontal bar of gray matter that connects the left and right horns.
Primarily houses unmyelinated axons.
Acts as a communication route between the two sides of the spinal cord.
Central Canal: A small channel in the center of the gray commissure that runs the length of the cord and contains Cerebrospinal Fluid (CSF).
Summary of Spinal Roots
Posterior Root: Contains all Sensory Neurons (Somatic and Visceral).
Anterior Root: Contains all Motor Neurons (Somatic and Autonomic).
Spinal Cord White Matter Structure and Function
The spinal cord's white matter is located external (outside) to the gray matter. It is primarily made of myelinated axons and functions to relay nerve signals (pathways).
Organization into Funiculi (Columns)
The white matter on each side of the spinal cord is partitioned into three regions called funiculi (meaning 'cords'):
Posterior Funiculus: Located between the posterior gray horns and the posterior median sulcus.
Lateral Funiculus: Located on the lateral (side) of the spinal cord.
Anterior Funiculus: Located between the anterior gray horns and the anterior median fissure.
The two anterior funiculi are connected by the white commissure.
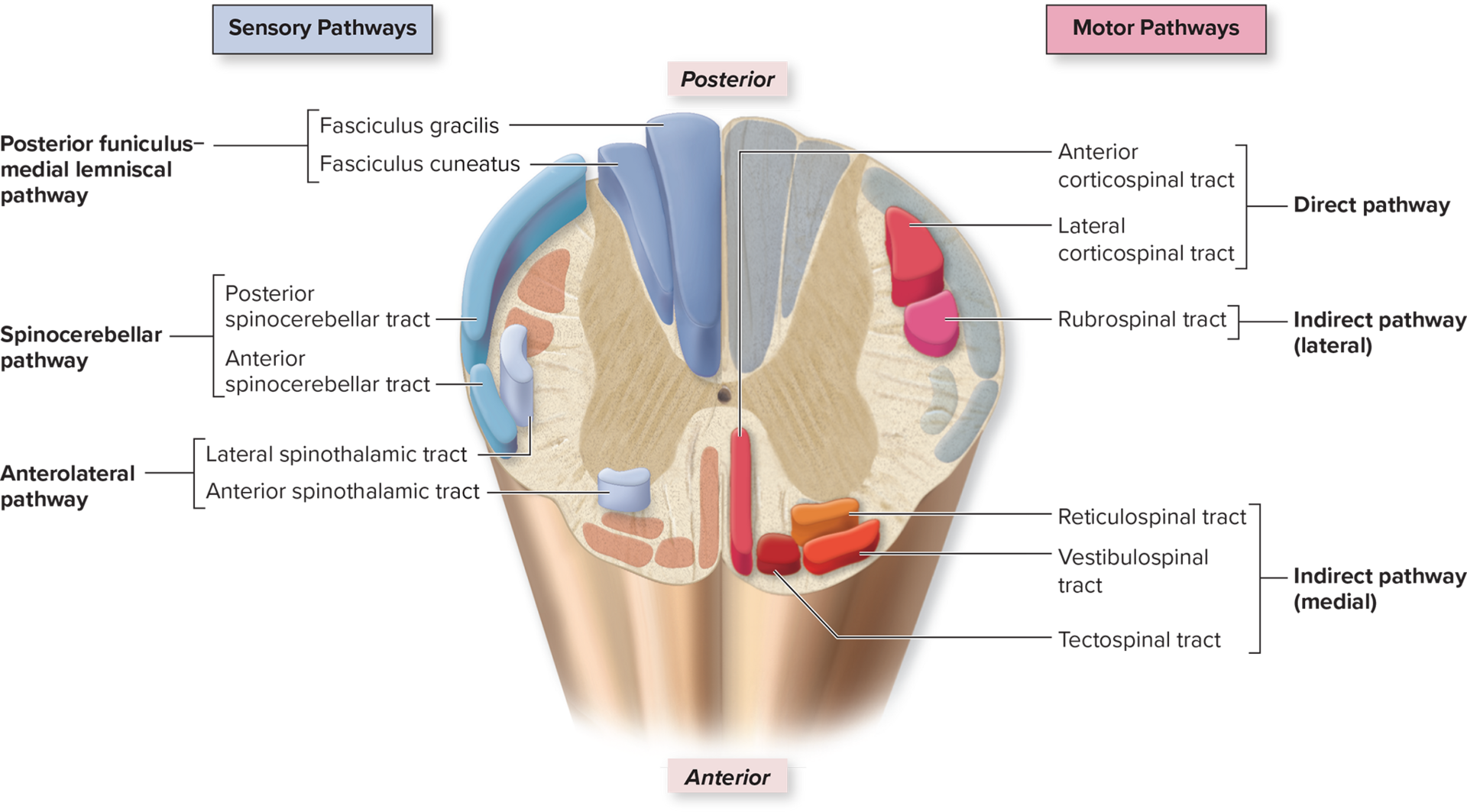
Axons Organized into Tracts
Axons within each funiculus are organized into bundles called fasciculi.
These bundles are also called tracts, which share a common origin, destination, and function.
Sensory Tracts (Ascending): Relay signals from the spinal cord to the brain.
Found in the posterior, lateral, and anterior funiculi.
Usually begin with spino− (e.g., Spinothalamic tract).
Motor Tracts (Descending): Relay signals from the brain to the spinal cord.
Found only in the lateral and anterior funiculi (not posterior).
Usually begin with cortico− (from the cortex) or the name of a brainstem nucleus (e.g., Corticospinal tract).
Variation Along the Spinal Cord
The size and shape of the spinal cord cross-section change along its length.
The relative amounts of gray and white matter vary depending on the function of that region.
Example: The lumbar part has a greater amount of gray matter because it contains more neuron cell bodies for nerves supplying the lower limbs.
Nervous System Pathways (General Description)
A nervous system pathway is a series of neurons and their associated structures.
Its purpose is to relay signals between the brain and a specific body part (torso and limbs).
Pathways that connect the brain to the torso and limbs involve components located in:
The Brain (e.g., the cerebrum).
The Spinal Cord (as tracts or fasciculi in the white matter).
Spinal Nerves (individual neurons).
Pathways also include integration and processing centers (gray matter) where neurons connect (synapse) at various locations.
Characteristics of Nervous System Pathways
Nervous system pathways are classified based on the direction signals travel relative to the brain.
Pathway Types
Sensory Pathways (Ascending):
Relay sensory input from receptors upward to the brain.
Motor Pathways (Descending):
Relay motor output from the brain downward to effectors (muscles and glands).
General Characteristics of Pathways
Paired Tracts: For every tract on one side of the CNS, there is a matching tract on the opposite side.
Composed of Multiple Neurons: Most pathways use a series of two or three neurons to relay signals:
Sensory pathways use primary, secondary, and sometimes tertiary neurons.
Motor pathways use an upper motor neuron and a lower motor neuron.
General Characteristics of Pathways
Neuron Cell Body Locations: Cell bodies are found in specific locations:
Posterior root ganglion (sensory).
Gray horns (spinal cord).
Nuclei (brain).
Axon Locations: Axons travel through:
Spinal nerves.
Spinal cord (as named tracts/fasciculi in white matter).
Brain.
Decussation (Crossover):
Most neurons (over 90%) cross over (decussate) from one side of the body to the other in the brain or spinal cord.
This results in contralateral control: the left side of the brain handles the right side of the body, and vice versa.
Ipsilateral Pathways (Limited):
A small percentage (about 10%) of neurons remain on the same side of the body (ipsilateral).
Sensory Pathways: Somatosensory System
Sensory pathways relay input from general sense receptors to the brain. These receptors are throughout the body (not just the head) and are split into two groups:
Somatosensory Receptors: Found in skin/mucous membranes (tactile receptors) and muscles/joints (proprioceptors).
Visceral Sensory Receptors: Found in internal organs/blood vessels (detect stretch, etc.).
Sensory pathways are classified as Somatosensory (skin/limb input) or Viscerosensory (organ input).
General Neuron Chain
Sensory pathways use a chain of 2 or 3 neurons (ascending to the brain):
Primary Neuron (1st-Order): Extends from the sensory receptor to the CNS (spinal cord or brain).
Secondary Neuron (2nd-Order): An interneuron extending from the primary neuron to the thalamus or cerebellum.
Tertiary Neuron (3rd-Order): An interneuron extending from the secondary neuron to the cerebrum (for conscious perception). Pathways to the cerebellum do not have a tertiary neuron.
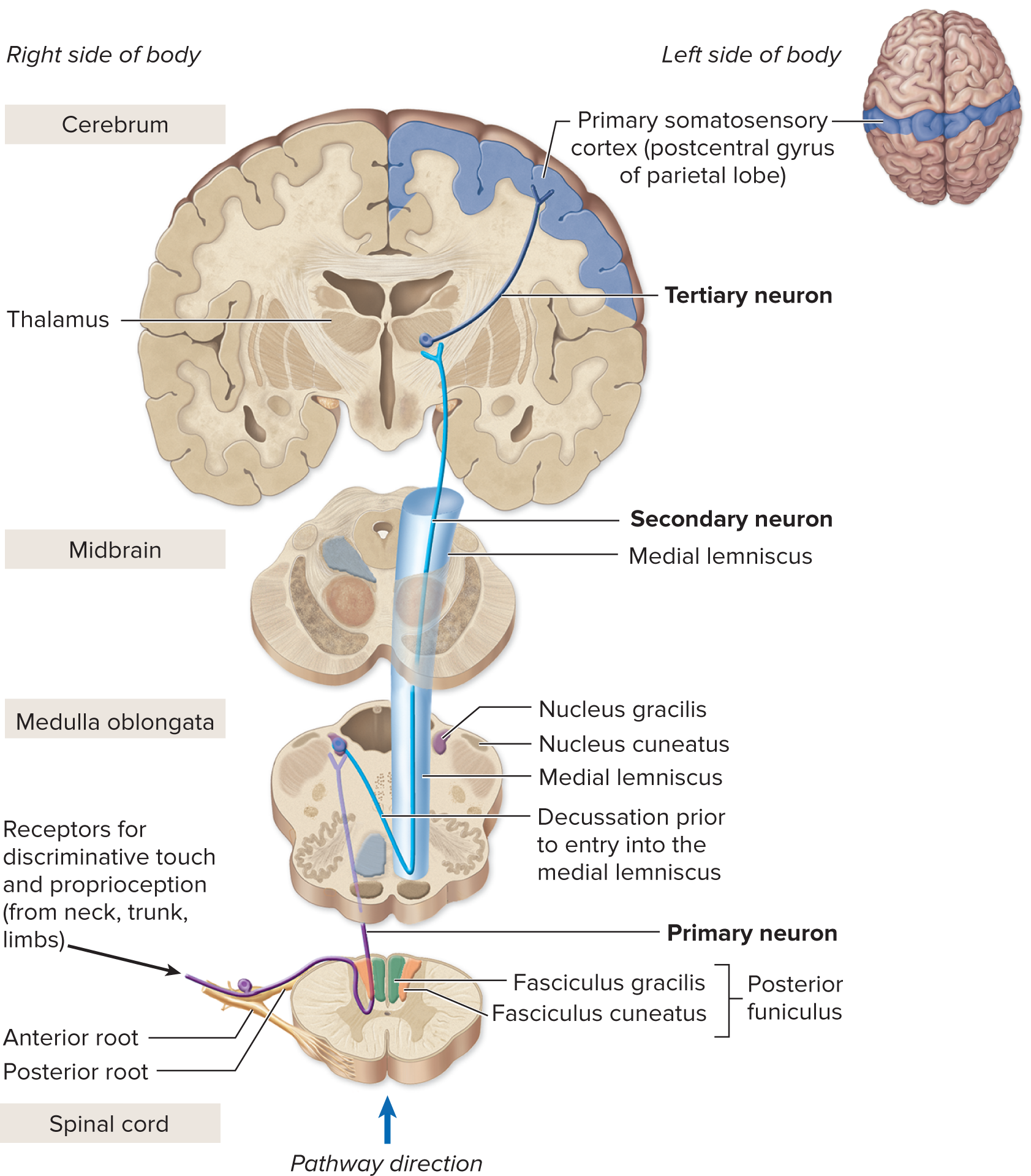
I. Posterior Funiculus–Medial Lemniscal Pathway (Conscious Proprioception & Fine Touch)
This pathway uses three neurons and relays discriminative (fine) senses to the cerebral cortex for conscious awareness.
Feature | Details |
Senses Relayed | Discriminative Touch (texture, shape) and Conscious Proprioception (body position/movement). |
Receptors | Tactile receptors in skin/mucous membranes, and Proprioceptors in joints/muscles. |
Neuron Chain Summary | 1. Primary Axon: Enters spinal cord, ascends in the posterior funiculus (e.g., Fasciculus gracilis/cuneatus) to synapse in the Medulla Oblongata. 2. Secondary Axon: Decussates (crosses over) in the brainstem, ascends via the Medial Lemniscus to synapse in the Thalamus. 3. Tertiary Axon: Projects from the Thalamus to the Primary Somatosensory Cortex (Parietal Lobe). |

II. Anterolateral Pathway (Crude Touch, Pain, & Temperature)
Also known as the Spinothalamic Pathway, this route uses three neurons and relays crude senses to the cerebral cortex.
Feature | Details |
Senses Relayed | Crude Touch, Pressure, Pain, and Temperature (e.g., itch, tickle). |
Receptors | Somatosensory receptors in the skin and mucous membranes. |
Neuron Chain Summary | 1. Primary Axon: Enters spinal cord and synapses immediately with the secondary neuron in the Posterior Horn. 2. Secondary Axon: Decussates (crosses over) within the spinal cord and ascends in the Anterolateral funiculus (Spinothalamic Tract) to synapse in the Thalamus. 3. Tertiary Axon: Projects from the Thalamus to the Primary Somatosensory Cortex (Parietal Lobe). |
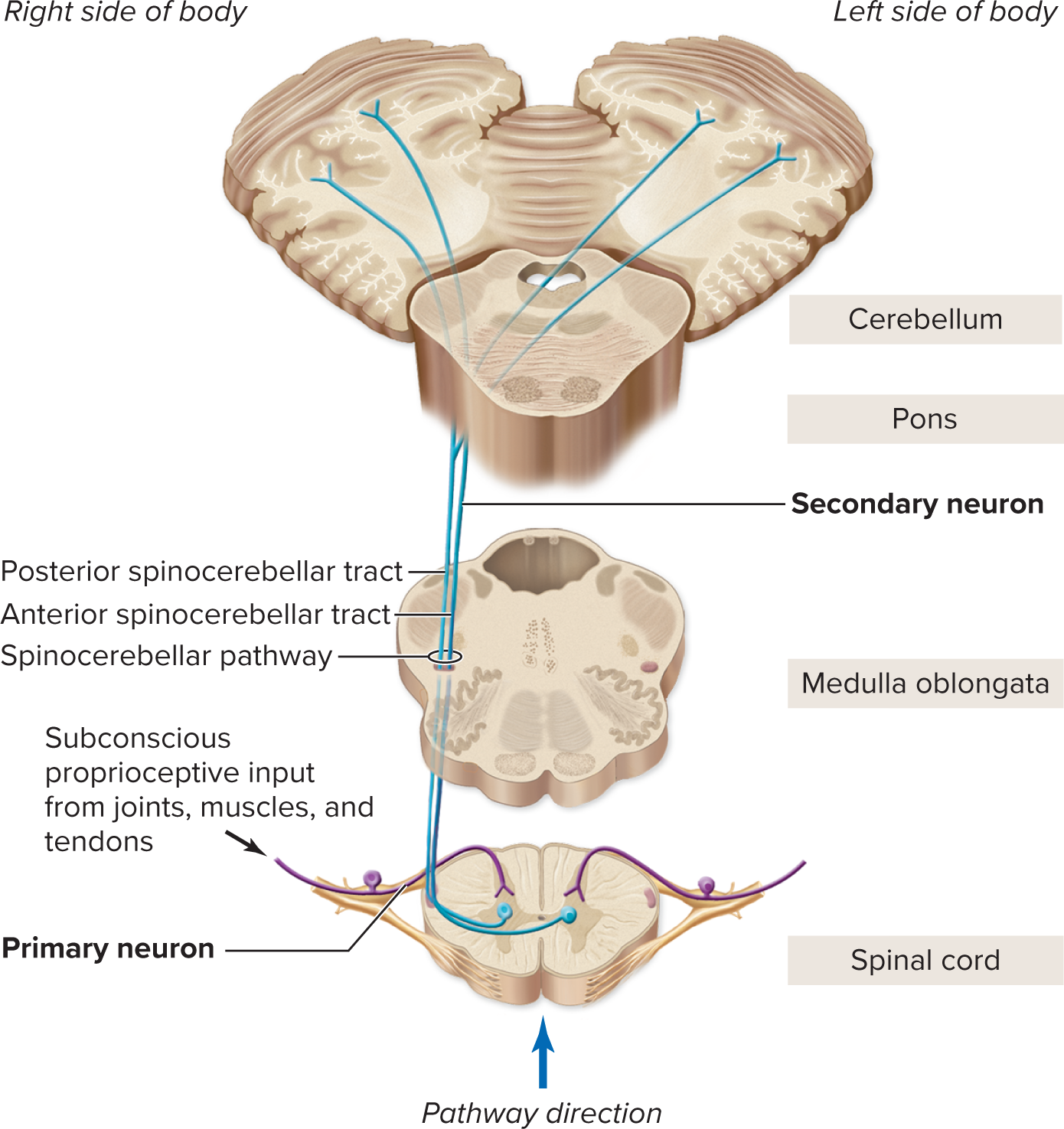
III. Spinocerebellar Pathway (Subconscious Proprioception)
This pathway uses two neurons and relays proprioceptive information to the cerebellum, bypassing the cortex.
Feature | Details |
Senses Relayed | Subconscious Proprioception (postural input for balance and posture). |
Receptors | Proprioceptors (muscles, tendons, joints). |
Neuron Chain Summary | 1. Primary Axon: Enters spinal cord and synapses in the Posterior Horn. 2. Secondary Axon: Ascends in the Lateral Funiculus (Spinocerebellar Tract) to the Cerebellum. Note: Does not have a tertiary neuron. (Some fibers decussate, others do not). |
Posterior Funiculus–Medial Lemniscal
Functions:
Sensory input for discriminative touch and for conscious perception of body position.
Relays input from upper limb, superior trunk, neck, posterior head.
Relays input from inferior trunk, lower limb
Components of Pathway
Fasciculus Cuneatus
Fasciculus Gracilis
Primary neuron | Extends from receptor to medulla oblongataCell bodies within posterior root ganglion | |
Secondary neuron | Extends from medulla oblongata to thalamusCell bodies within medulla oblongata (nucleus cuneatus or nucleus gracilis) | |
Tertiary neuron | Extends from thalamus to primary somatosensory cortex of the parietal lobeCell bodies within thalamus | |
Structures involved in decussation | Axons of secondary neurons decussate just prior to medial lemniscus | |
Anterolateral
Components of Pathway:
Anterior Spinothalamic Tract
Lateral Spinothalamic Tract
Function:
Sensory input from tactile receptors for conscious perception of crude touch, pressure, pain, and temperature.
Relays input for crude touch and pressure.
Relays input for pain and temperature.
Primary Neuron:
Extends from receptor to spinal cord.
Cell bodies within posterior root ganglion.
Secondary Neuron:
Extends from spinal cord to thalamus.
Cell bodies within spinal cord (posterior horn)
Tertiary Neuron:
Extends from thalamus to primary somatosensory cortex of the parietal lobe.
Cell bodies within thalamus
Structures involved in decussation:
Axons of secondary neurons decussate within spinal cord at level of entry.
Spinocerebellar
Components of Pathway:
Anterior Spinocerebellar Tract
Posterior Spinocerebellar Tract
Function:
Sensory input from proprioceptors to cerebellum for subconscious interpretation.
Relays input from inferior regions of trunk and lower limbs.
Relays input from upper limbs, regions of trunk, and lower limbs.
Primary Neuron:
Extends from receptor to spinal cord.
Cell bodies within posterior root ganglion
Secondary Neuron:
Extends from spinal cord to cerebellum.
Cell bodies within spinal cord (posterior horn).
Tertiary Neuron:
N/A
Structures involved in decussation:
Axons decussate in spinal cord, ascend, and then recross at the level of the superior cerebellar peduncle.
Axons do not decussate.

Motor Pathways: Descending Control of Skeletal Muscle
Motor pathways are descending pathways that originate in the brain and control skeletal muscle (neck, torso, and limbs).
Motor Neuron Chain
Motor pathways use at least two motor neurons to relay output from the brain to the muscle:
Upper Motor Neuron (UMN):
Location of Cell Body: Cerebral cortex, cerebral nuclei, or brainstem nuclei.
Function: Axons travel down and synapse on the lower motor neuron (directly or via interneurons). They excite or inhibit the lower motor neuron activity.
Lower Motor Neuron (LMN):
Location of Cell Body: Anterior horn of the spinal cord.
Function: Axons exit the spinal cord via the anterior root and innervate a specific skeletal muscle. LMNs always excite the muscle fiber, causing contraction.
Direct Pathway (Conscious Control)
Also called the Pyramidal Pathway, it provides conscious control over skeletal muscles and uses a chain of only two neurons (one UMN and one LMN).
Origin: Primary motor cortex of the cerebrum.
Tracts: Axons of the UMN travel through the corticospinal tracts in the spinal cord.
Subdivisions based on Function & Decussation:
Lateral Corticospinal Tract (85%):
Control: Skilled movements in appendicular muscles (limbs, e.g., typing, playing music).
Decussation: Occurs in the Medulla Oblongata (at the pyramids).
Anterior Corticospinal Tract (15%):
Control: Movements in axial muscles (neck and torso).
Decussation: Occurs at the level of the spinal cord segment.
II. Indirect Pathway (Subconscious/Reflexive Control)
The indirect pathway provides subconscious (reflexive) and regulatory control over muscle activity, originating in the brainstem nuclei. It modifies LMN activity (excites or inhibits) to control gross movements and muscle tone.
Lateral Pathway:
Function: Regulates precise, discrete movements and tone in flexor muscles of the limbs (e.g., gently placing an object).
Tract Example: Rubrospinal Tracts (from the Red Nucleus in the midbrain).
Medial Pathway:
Function: Regulates reflexive muscle tone and gross movements of the head, neck, trunk, and proximal limbs (related to posture and balance).
Tract Examples (all from brainstem nuclei):
Reticulospinal Tracts: Controls reflexive movements for posture and balance.
Tectospinal Tracts: Regulates reflexive changes in position (head, neck, eyes, upper limbs) in response to visual and auditory stimuli.
Vestibulospinal Tracts: Regulates reflexive activity to maintain balance (during sitting, walking, etc., based on inner ear input).
Principal Motor Pathways
Tract | Manner of Decussation | Destination of Upper Motor Neurons | Termination Site | Function |
|---|---|---|---|---|
DIRECT PATHWAY | ||||
Lateral corticospinal tracts | All decussate at the pyramids | Lateral funiculus | Gray matter region between posterior and anterior horns; anterior horn; all levels of spinal cord | Voluntary movement of appendicular muscles |
Anterior corticospinal tracts | Decussation occurs in spinal cord at level of lower motor neuron cell body | Anterior funiculus | Gray matter region between posterior and anterior horns; anterior horn; cervical part of spinal cord | Voluntary movement of axial muscles |
Corticonuclear tracts1 | All cranial nerve motor nuclei receive bilateral (both ipsilateral and contra-lateral) input except CN VI, VII to the face, and XII (these nerves receive only contralateral input) | Brainstem only | Cranial nerve nuclei; reticular formation | Voluntary movement of the head and face muscles |
Principal Motor Pathways
INDIRECT PATHWAY | ||||
Lateral Pathway | ||||
|---|---|---|---|---|
Rubrospinal tract | Decussate at ventral tegmentum of midbrain | Lateral funiculus | Lateral region between posterior and anterior horns; anterior horn; cervical part of spinal cord | Regulates and controls precise, discrete, reflexive movements and tone in flexor muscles of the limbs |
Medial Pathway | ||||
Reticulospinal tract | No decussation (ipsilateral) | Anterior funiculus | Medial region between posterior and anterior horns; anterior horn; all parts of spinal cord | Controls reflexive movements related to posture and maintaining balance |
Tectospinal tract | Decussate at dorsal tegmentum of midbrain | Anterior funiculus | Medial region between posterior and anterior horns; anterior horn; cervical part of spinal cord | Regulates reflexive positional changes of the upper limbs, eyes, head, and neck due to visual and auditory stimuli |
Vestibulospinal tract | Some decussate (contralateral) and some do not (ipsilateral) | Anterior funiculus | Medial region between posterior and anterior horns; anterior horn; medial tracts to cervical and superior thoracic parts of spinal cord; lateral tracts to all parts of spinal cord | Regulates reflexive muscular activity that helps maintain balance during sitting, standing, and walking |
Spinal Nerves: Composition and Distribution
There are 31 pairs of spinal nerves (C1–C8, T1–T12, L1–L5, S1–S5, and Co1).
All spinal nerves are considered mixed nerves because they contain two types of axons:
Sensory Axons: Extend from sensory receptors to the spinal cord via the posterior root. (Cell bodies are in the posterior root ganglia).
Motor Axons: Extend from the spinal cord to effectors (muscles and glands).
The peripheral distribution describes how these nerves branch out to supply the body.
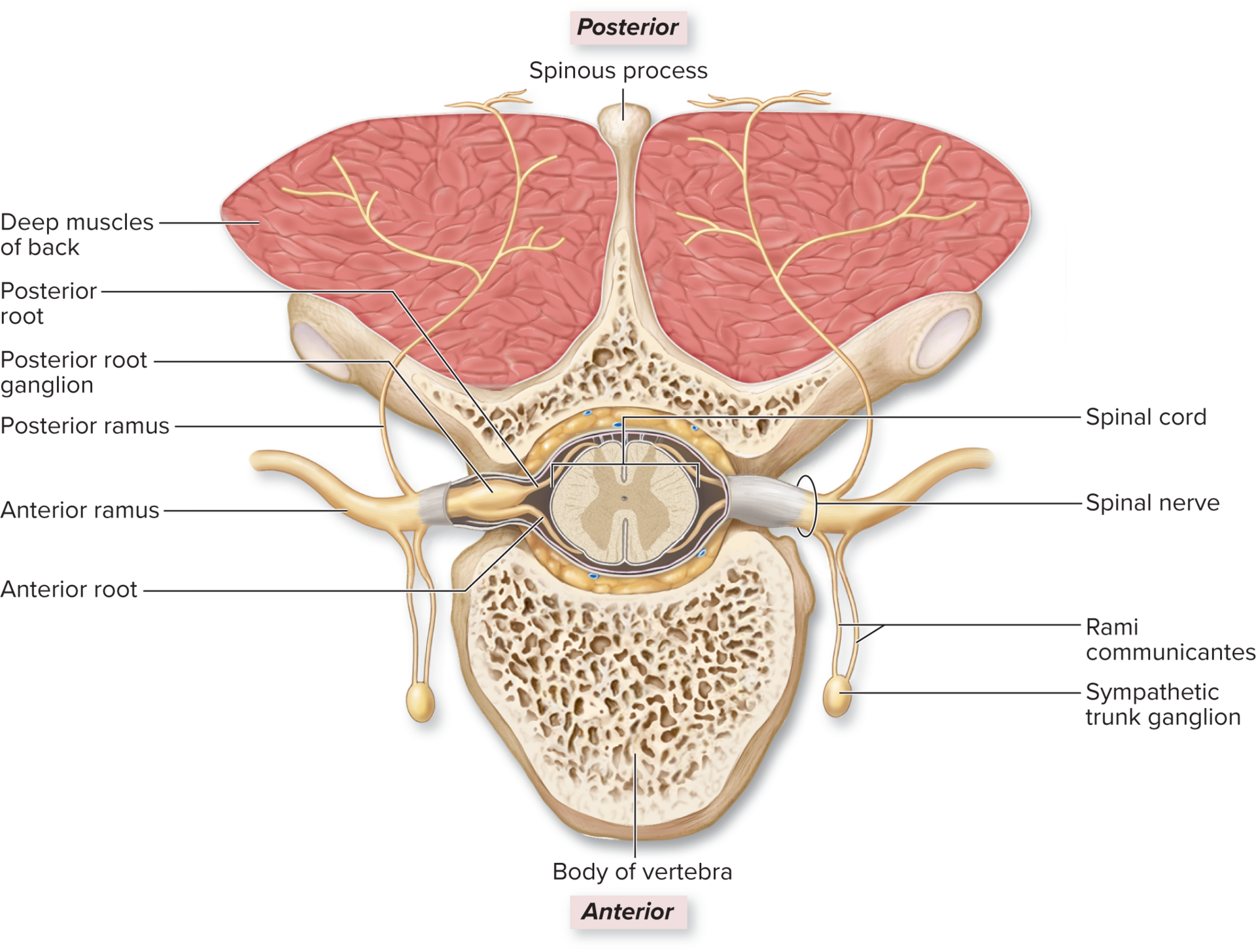
Peripheral Distribution of Spinal Nerves
Each spinal nerve (except C1 and Co1) quickly splits into branches called rami upon exiting the intervertebral foramen.
Spinal Nerve Branches (Rami)
Ramus | Size | Innervates | Function/Note |
Posterior (Dorsal) Ramus | Smaller branch | Deep muscles and skin of the back. | Supplies the posterior trunk. |
Anterior (Ventral) Ramus | Larger branch | Skin and skeletal muscles of the anterior/lateral trunk, upper limbs, and lower limbs. | Often forms nerve plexuses (networks). |
Rami Communicantes | Additional branches | Autonomic Nervous System (ANS) axons. | Connect the spinal nerve to the sympathetic trunk ganglia (part of the ANS). |
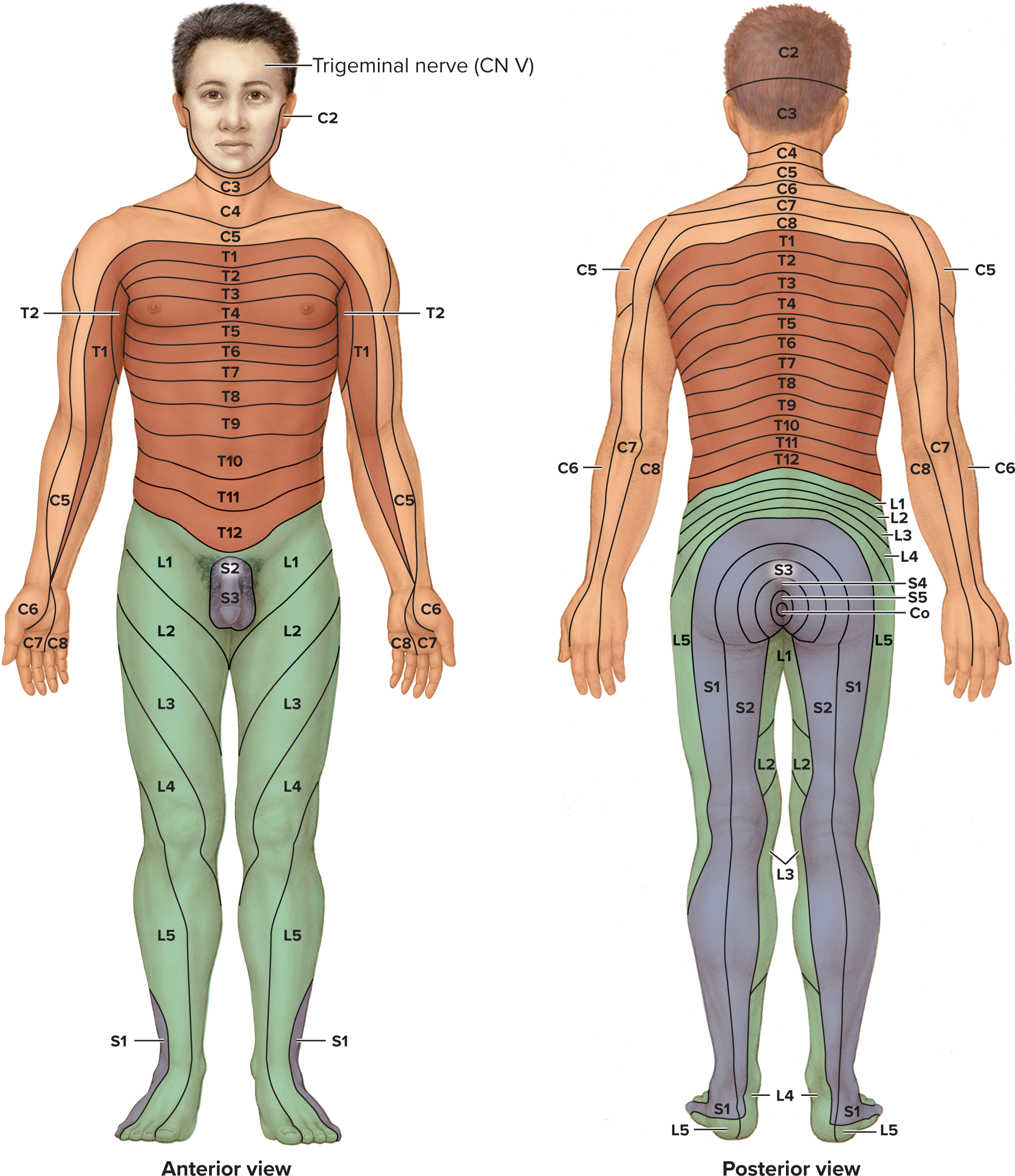
Dermatomes (Innervation Maps)
A dermatome is a specific segment of skin that is supplied by a single spinal nerve. (All spinal nerves except C1 innervate skin).
A dermatome map shows the segmented pattern of skin innervation across the body (e.g., T10 innervates the navel area)
Clinical Importance:
Spinal Nerve Damage: Numbness (anesthesia) in a specific dermatome (e.g., C8 area of the arm) indicates damage to that nerve.
Shingles: The rash typically follows the path of one or several dermatomes.
Referred Visceral Pain: Pain from an internal organ can be mistakenly perceived in a distant, corresponding dermatome (e.g., appendix pain (T10 region) is felt near the navel, not the actual organ site).
Nerve Plexuses and Spinal Nerve Distribution
A nerve plexus (meaning "a braid") is a network of interweaving anterior rami (branches) of several spinal nerves.
Most anterior rami form plexuses on both sides of the body, which then divide into specific, named nerves.
Major Plexuses:
Cervical Plexus
Brachial Plexus
Lumbar Plexus
Sacral Plexus
Advantage of Plexuses:
Each final, terminal nerve in a plexus contains axons from multiple different spinal nerves.
This means damage to a single spinal nerve or spinal cord segment usually does not cause complete loss of movement or sensation for a body part.
Nerves That Do Not Form Plexuses:
Most thoracic spinal nerves (T1–T12) continue as individual nerves (Intercostal Nerves).
Spinal nerves S5–Co1 also generally do not form a major plexus.
Thoracic Spinal Nerves (Intercostal Nerves)
The anterior rami of spinal nerves T1–T11 are called intercostal nerves because they run between adjacent ribs (in the intercostal space). T12 is the subcostal nerve (runs below the ribs).
Thoracic Spinal Nerves (Intercostal Nerves)
Key Features and Innervation
No Plexus Formation: With the exception of some T1 axons, the intercostal nerves do not form plexuses.
General Function: They innervate the torso wall (muscles and skin).
Thoracic Spinal Nerves (Intercostal Nerves)
Nerve(s) | Function / Area Innervated |
T1 | Contributes axons to the Brachial Plexus (arm), and the rest form the first intercostal nerve. |
T2 | Innervates muscles of the second intercostal space. Also relays sensory input from the skin of the axilla (armpit) and medial arm. |
T3–T6 | Innervates the intercostal muscles and relays sensory input from the anterior and lateral chest wall. |
T7–T12 | Innervates the lower intercostal spaces. Also innervates the abdominal muscles and relays sensory input from the overlying skin. |
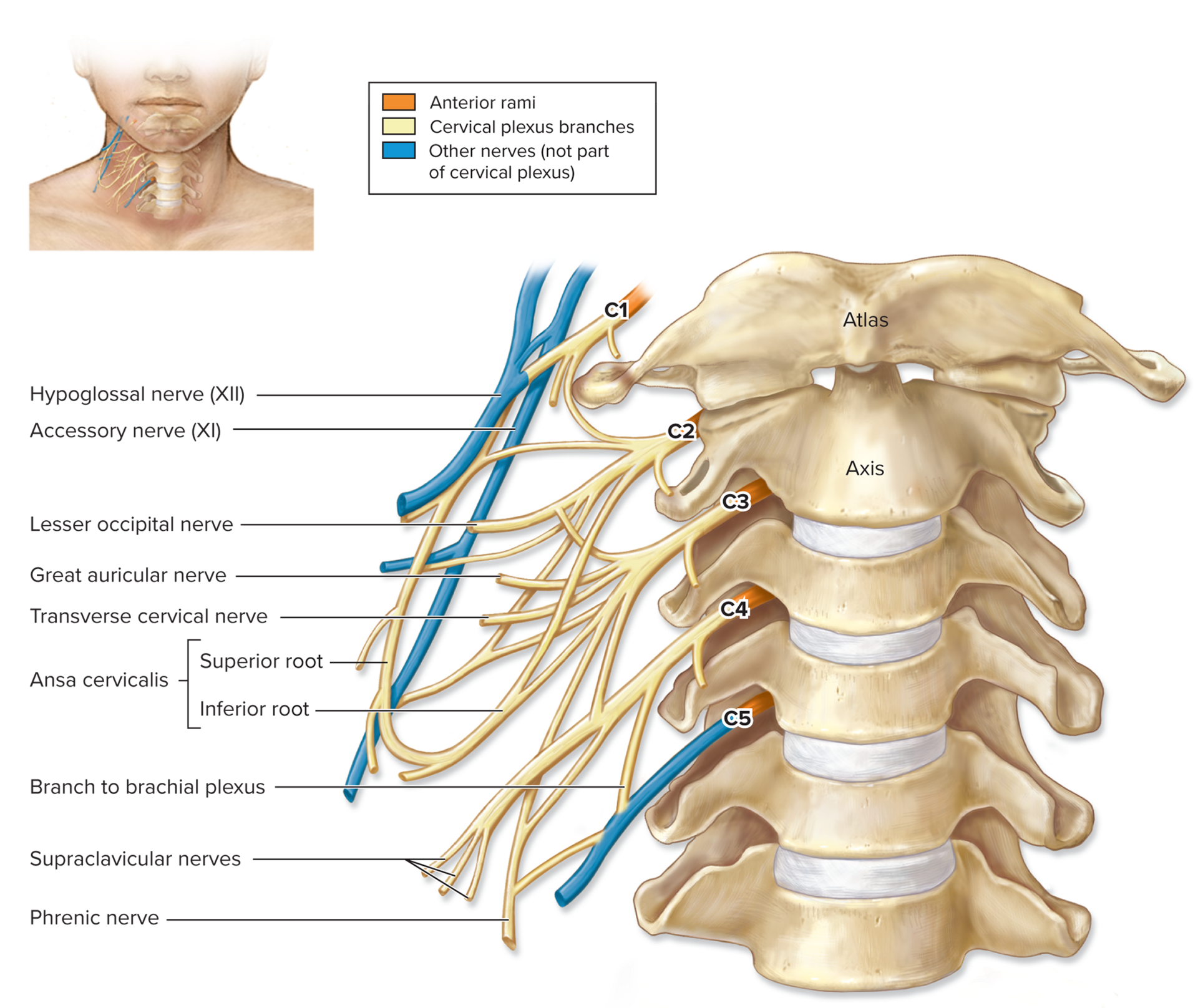
Cervical Plexus (C1–C4)
The cervical plexuses (left and right) are located deep in the neck, lateral to cervical vertebrae C1–C4.
They are formed primarily by the anterior rami of spinal nerves C1 through C4. (C5 contributes some axons but isn't considered part of the main plexus).
Function:
Innervate the anterior neck muscles.
Innervate the skin of the neck, and parts of the head and shoulders.
Motor branches relay motor output to muscles.
Cutaneous branches relay sensory input from the skin.
Cervical Plexus (C1–C4)
Key Branch: Phrenic Nerve
The phrenic nerve is formed primarily from C4 with contributions from C3 and C5.
Function: It is crucial because it innervates the thoracic diaphragm, the primary muscle required for breathing.
Branches of the Cervical Plexuses
Nerves | Anterior Rami | Innervation |
|---|---|---|
MOTOR BRANCHES | ||
Ansa cervicalis
|
| Geniohyoid; infrahyoid muscles (omohyoid, sternohyoid, sternothyroid, and thyrohyoid) |
CUTANEOUS BRANCHES | ||
Greater auricular | C2, C3 | Skin on ear; connective tissue capsule covering parotid gland |
Lesser occipital | C2 | Skin of scalp superior and posterior to ear |
Supraclavicular | C3, C4 | Skin on superior part of chest and shoulder |
Transverse cervical | C2, C3 | Skin on anterior part of neck |
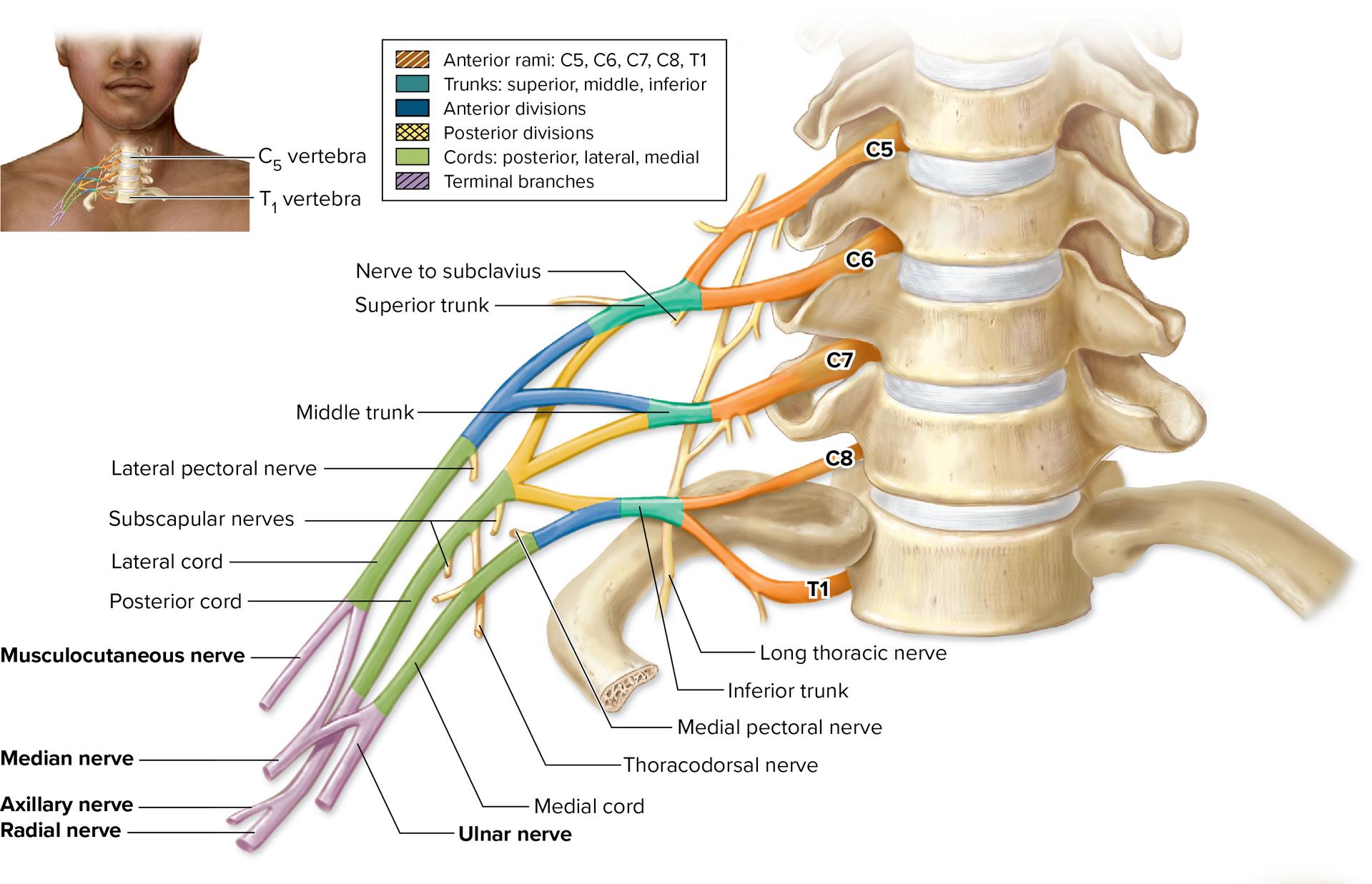
Brachial Plexus (C5–T1)
The left and right brachial plexuses are complex networks of nerves that innervate the entire upper limb and pectoral girdle.
They are formed by the anterior rami (roots) of spinal nerves C5 through T1.
The plexus extends from the neck, over the first rib, and into the axilla (armpit).
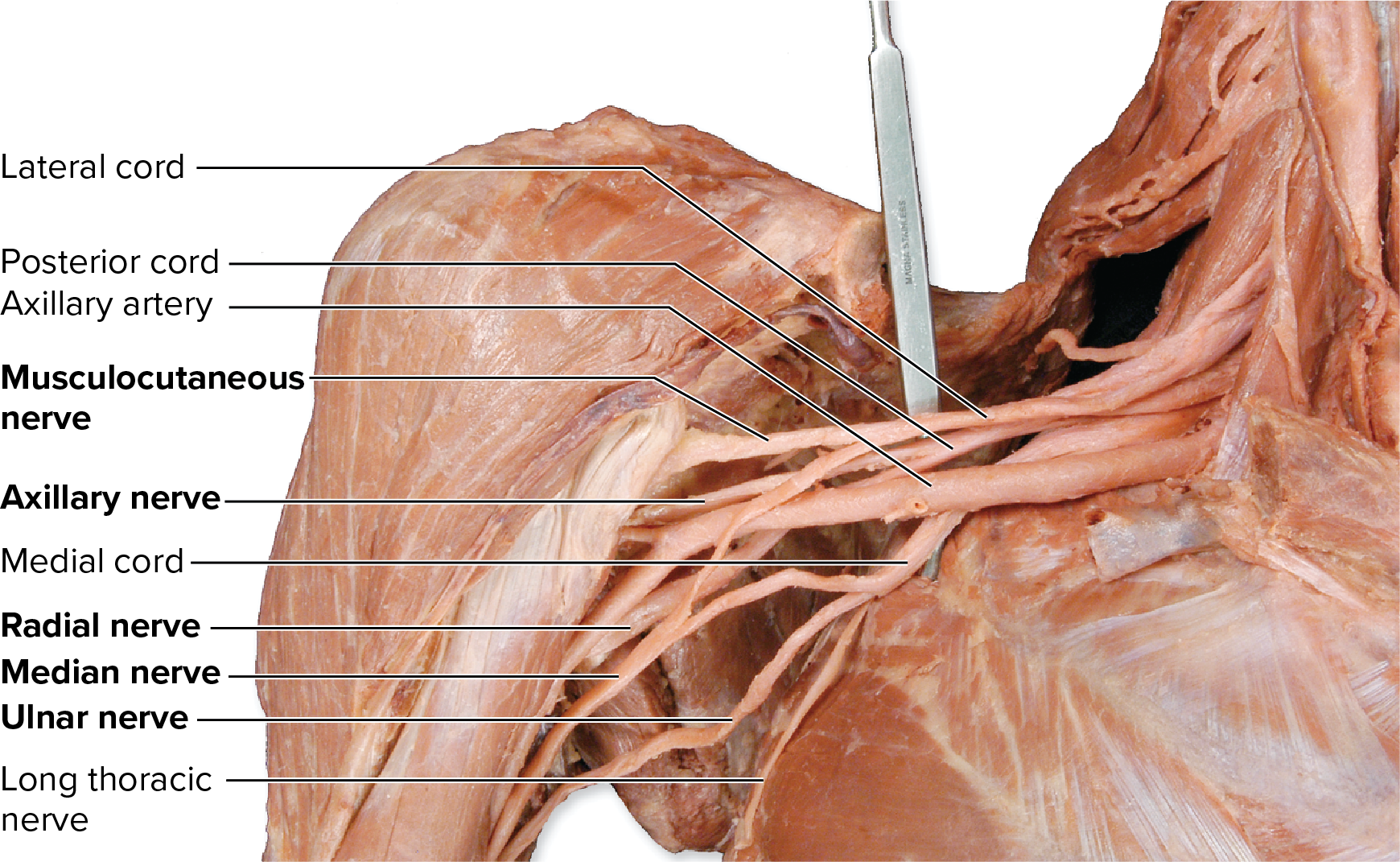
Structure of the Brachial Plexus (Medial to Lateral)
The plexus is organized into five main components: Roots, Trunks, Divisions, Cords, and Terminal Branches.
Roots (Anterior Rami C5–T1):
The starting components, emerging from the intervertebral foramina.
Trunks (in the neck):
Superior Trunk: Formed by C5 and C6 rami.
Middle Trunk: Formed by C7 ramus.
Inferior Trunk: Formed by C8 and T1 rami.
Divisions (deep to the clavicle):
Each trunk splits into an Anterior Division and a Posterior Division.
Anterior Divisions contain axons for the anterior (flexor) upper limb muscles.
Posterior Divisions contain axons for the posterior (extensor) upper limb muscles.
Cords (in the axilla):
Named based on their position relative to the axillary artery:
Posterior Cord: Formed by all three Posterior Divisions (contains C5–T1).
Medial Cord: Formed by the Anterior Division of the Inferior Trunk (contains C8–T1).
Lateral Cord: Formed by the Anterior Divisions of the Superior and Middle Trunks (contains C5–C7).
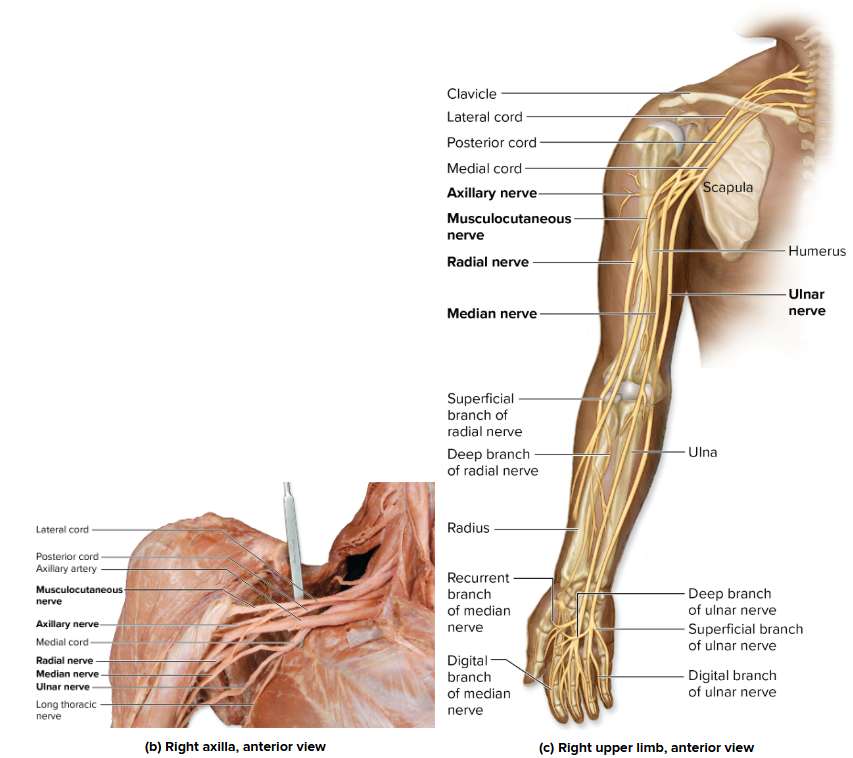
Brachial Plexus: Terminal Branches (Cords to Nerves)
The three cords of the brachial plexus ultimately form five major terminal branches that supply the upper limb.
Terminal Nerve | Originating Cord(s) | Motor Innervation (Muscles) | Sensory Innervation (Skin Area) |
Axillary Nerve | Posterior Cord | Deltoid and Teres Minor muscles (shoulder movement). | Superolateral part of the arm (over the shoulder). |
Median Nerve | Medial & Lateral Cords | Most anterior forearm muscles (flexors), thenar muscles (thumb pad), and lateral lumbricals. | Palmar side of the lateral 3½ fingers (thumb, index, middle, half of ring). |
Musculocutaneous Nerve | Lateral Cord | Anterior arm muscles (Coracobrachialis, Biceps Brachii, Brachialis) (flexion of arm/forearm). | Lateral surface of the forearm. |
Radial Nerve | Posterior Cord | Posterior arm and forearm muscles (extensors of forearm, wrist, and digits; supinator). | Posterior arm/forearm surface and dorsolateral side of the hand. |
Ulnar Nerve | Medial Cord | Some anterior forearm muscles (medial flexors) and most intrinsic hand muscles (hypothenar, interossei, medial lumbricals). | Dorsal and palmar aspects of the medial 1½ fingers (pinky and medial half of ring). |
Minor Branches: The brachial plexus also gives off many smaller nerves that innervate parts of the pectoral girdle and upper limb, in addition to these five major branches.
Branches of the Brachial Plexus
Terminal Branch | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Axillary NerveFormed from posterior cord, posterior division of the brachial plexus  | C5, C6 | Deltoid (abducts, flexes, and/or extends arm)Teres minor (laterally rotates arm) | Superolateral arm  |
Branches of the Brachial Plexus
Median Nerve Formed from medial and lateral cords, anterior division of the brachial plexus  | C6–T1 | Most anterior forearm muscles (pronate forearm, flex wrist and digits)
Thenar (thumb) muscles (move thumb)
Lateral 2 lumbricals (flex MP joints and extend PIP and DIP joints) | Palmar aspects and dorsal tips of lateral 3½ digits (thumb, index finger, middle finger, and ½ of ring finger) 
 |
Branches of the Brachial Plexus
Musculocutaneous NerveFormed from the lateral cord, anterior division of the brachial plexus  | C5–C7 | Anterior arm muscles (flex arm, flex forearm, supinate forearm)
| Lateral region of forearm   |
Branches of the Brachial Plexus
Radial NerveFormed from the posterior cord, posterior division of the brachial plexus  | C5–T1 | Posterior arm muscles (extend forearm)
Posterior forearm muscles (supinate forearm, extend wrist, extend digits, one muscle abducts thumb)
Brachioradialis (flexes forearm) | Posterior region of armPosterior region of forearmDorsal aspect of lateral 3½ digits (except their distal tips)  |
Branches of the Brachial Plexus
Ulnar NerveFormed from the medial cord, anterior division of the brachial plexus  | C8–T1 | Anterior forearm muscles (flex wrist and digits)
Intrinsic hand muscles
| Dorsal and palmar aspects of medial 1½ digits (little finger, medial aspect of ring finger)   |
Terminal Branches of the Brachial Plexus
Other Branches of the Brachial Plexus | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Dorsal scapular | C5 | Rhomboids, levator scapulae | |
Long thoracic | C5–C7 | Serratus anterior | |
Lateral pectoral | C5–C7 | Pectoralis major | |
Medial pectoral | C8–T1 | Pectoralis major, pectoralis minor | |
Medial cutaneous nerve of arm | C8–T1 | Medial side of arm | |
Medial cutaneous nerve of forearm | C8–T1 | Medial side of forearm | |
Nerve to subclavius | C5–C6 | Subclavius | |
Suprascapular | C5–C6 | Supraspinatus, infraspinatus | |
Subscapular nerves | C5–C6 | Subscapularis, teres major | |
Thoracodorsal (nerve to latissimus dorsi) | C6–C8 | Latissimus dorsi |
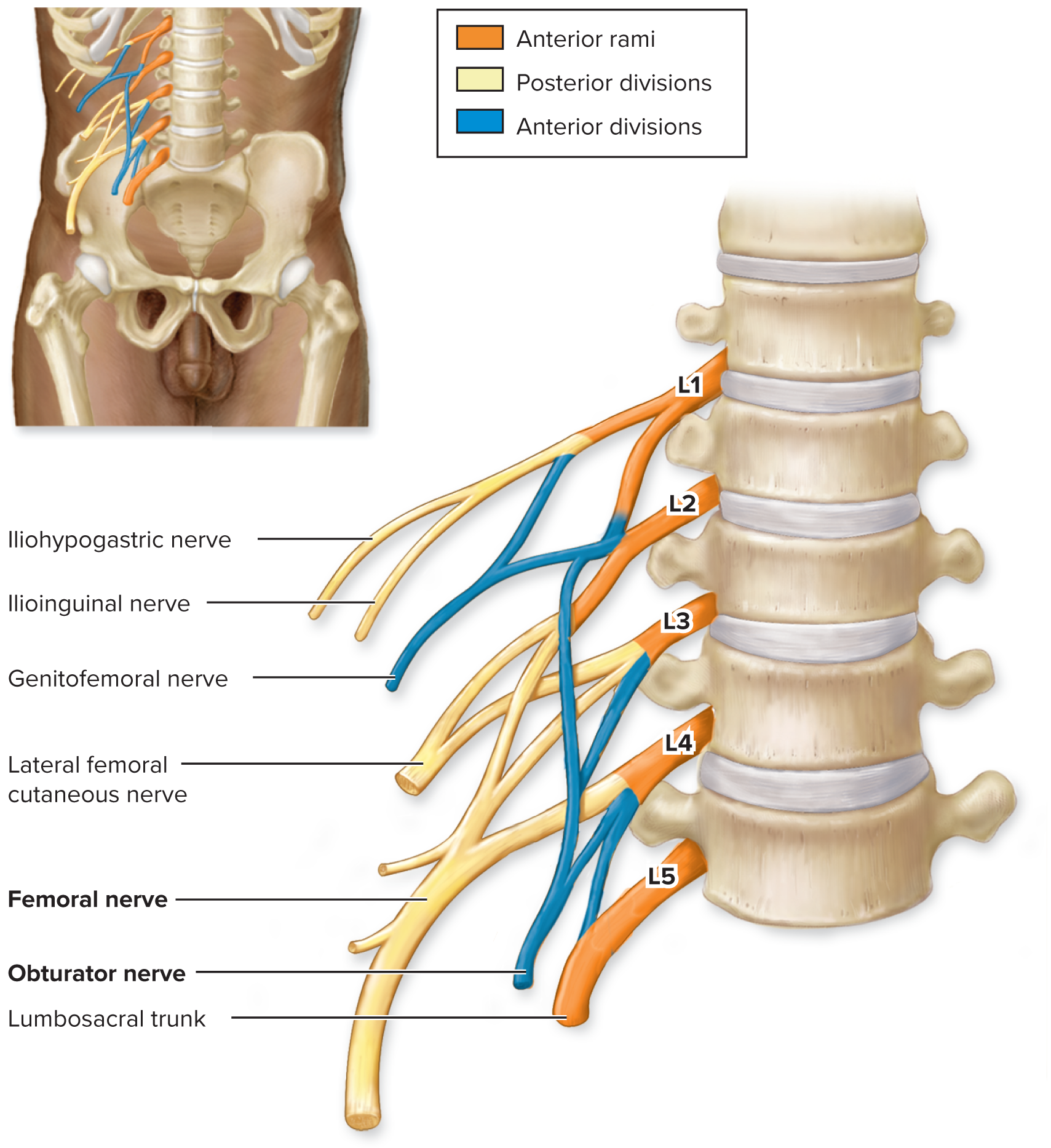
Lumbar Plexus (L1–L4)
The left and right lumbar plexuses are networks of nerves formed from the anterior rami of spinal nerves L1 through L4.
Location and Function: They innervate the:
Inferior abdominal wall.
Anterior and medial thigh.
Skin of the medial leg.
Structure: It is less complex than the brachial plexus but is divided into a posterior division and an anterior division.
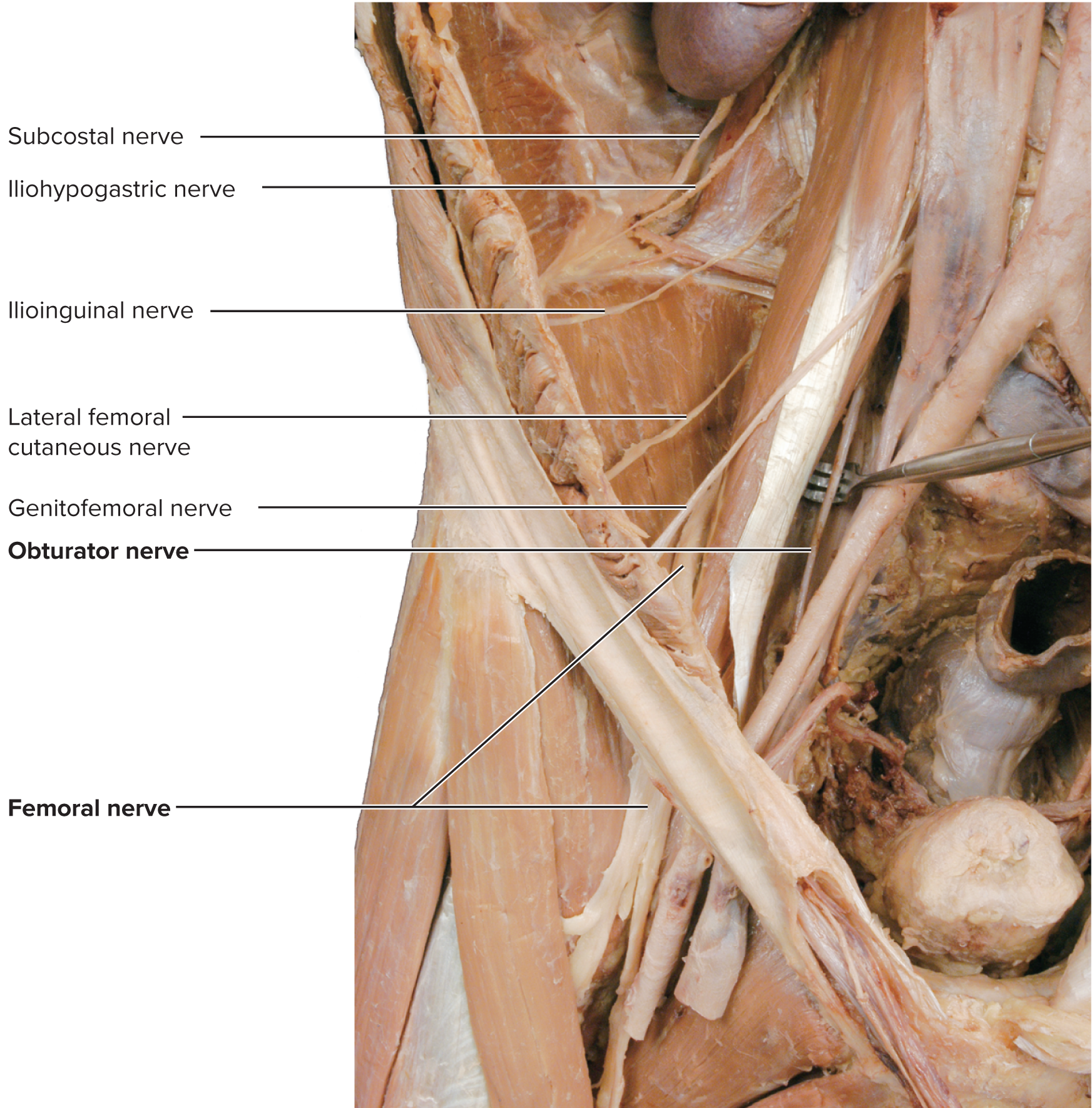
Lumbar Plexus (L1–L4)
Major Terminal Nerves
Nerve | Originating Division | Motor Innervation (Muscles) | Sensory Innervation (Skin Area) |
Femoral Nerve | Posterior Division | Anterior thigh muscles (e.g., Quadriceps femoris for knee extension; Hip flexors like Iliacus/Psoas). | Anterior and inferomedial thigh and medial leg. |
Obturator Nerve | Anterior Division | Medial thigh muscles (thigh adductors). | Superomedial skin of the thigh. |

Lumbar Plexus (L1–L4)🦵
Other Branches: Smaller nerves from the plexus supply the abdominal wall, external genitalia, and lower abdominal muscles.
Branches of the Lumbar Plexus
Main Branch | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Femoral Nerve  | L2–L4 | Anterior thigh muscles
|
 |
Branches of the Lumbar Plexus
Obturator Nerve  | L2–L4 | Medial thigh muscles (adduct and flex thigh at hip)
| Superomedial thigh  |
Lumbar Plexus (L1–L4)
Smaller Branches of the Lumbar Plexus | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Iliohypogastric | L1 | Partial innervation to abdominal muscles (flex vertebral column) | Superior lateral gluteal regionInferior abdominal wall |
Ilioinguinal | L1 | Partial innervation to abdominal muscles (flex vertebral column) | Inferior abdominal wallScrotum or labia majora |
Genitofemoral | L1, L2 | Small area in anterior superior thighScrotum or labia majora | |
Lateral femoral cutaneous | L2, L3 | Anterolateral thigh |
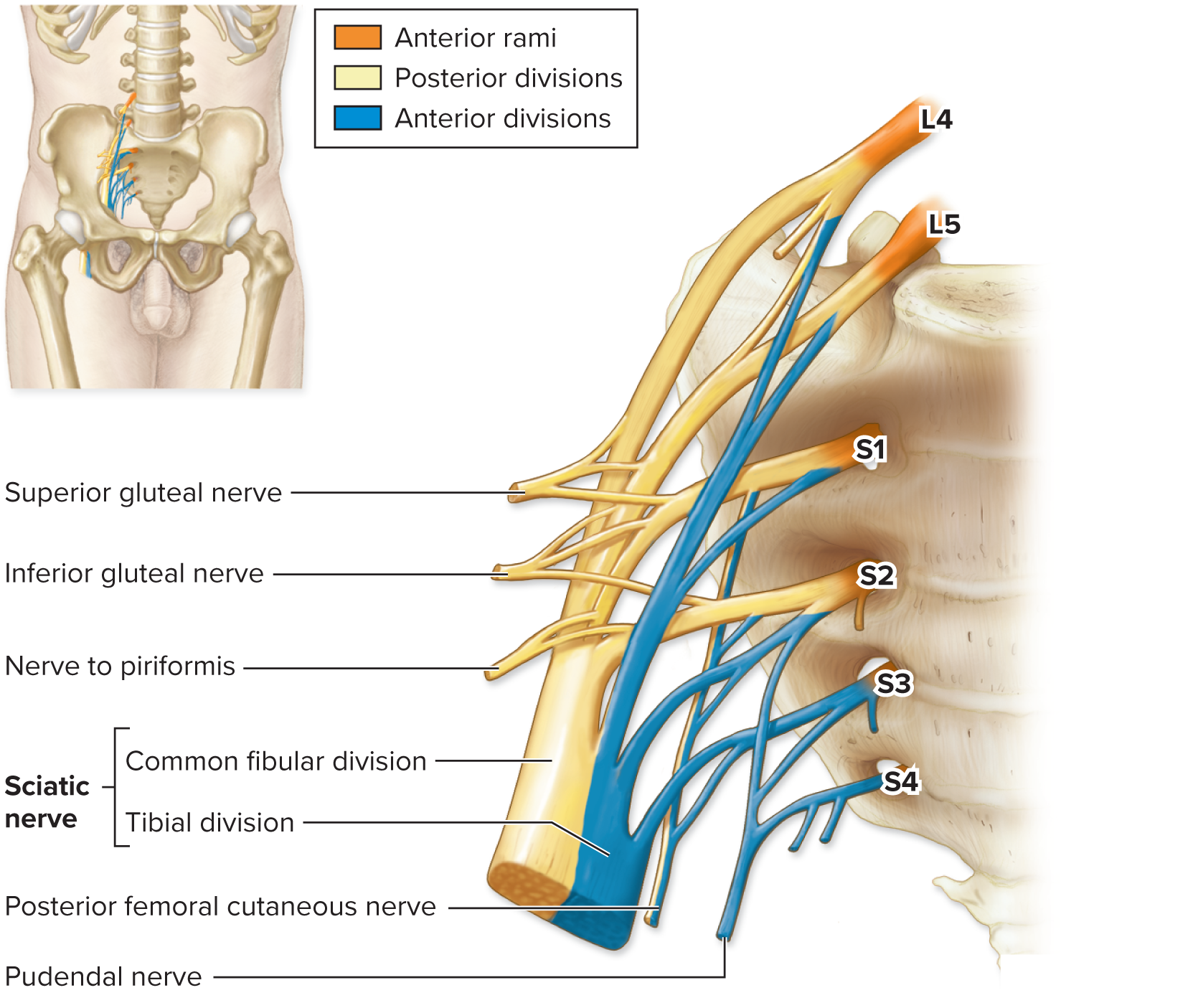
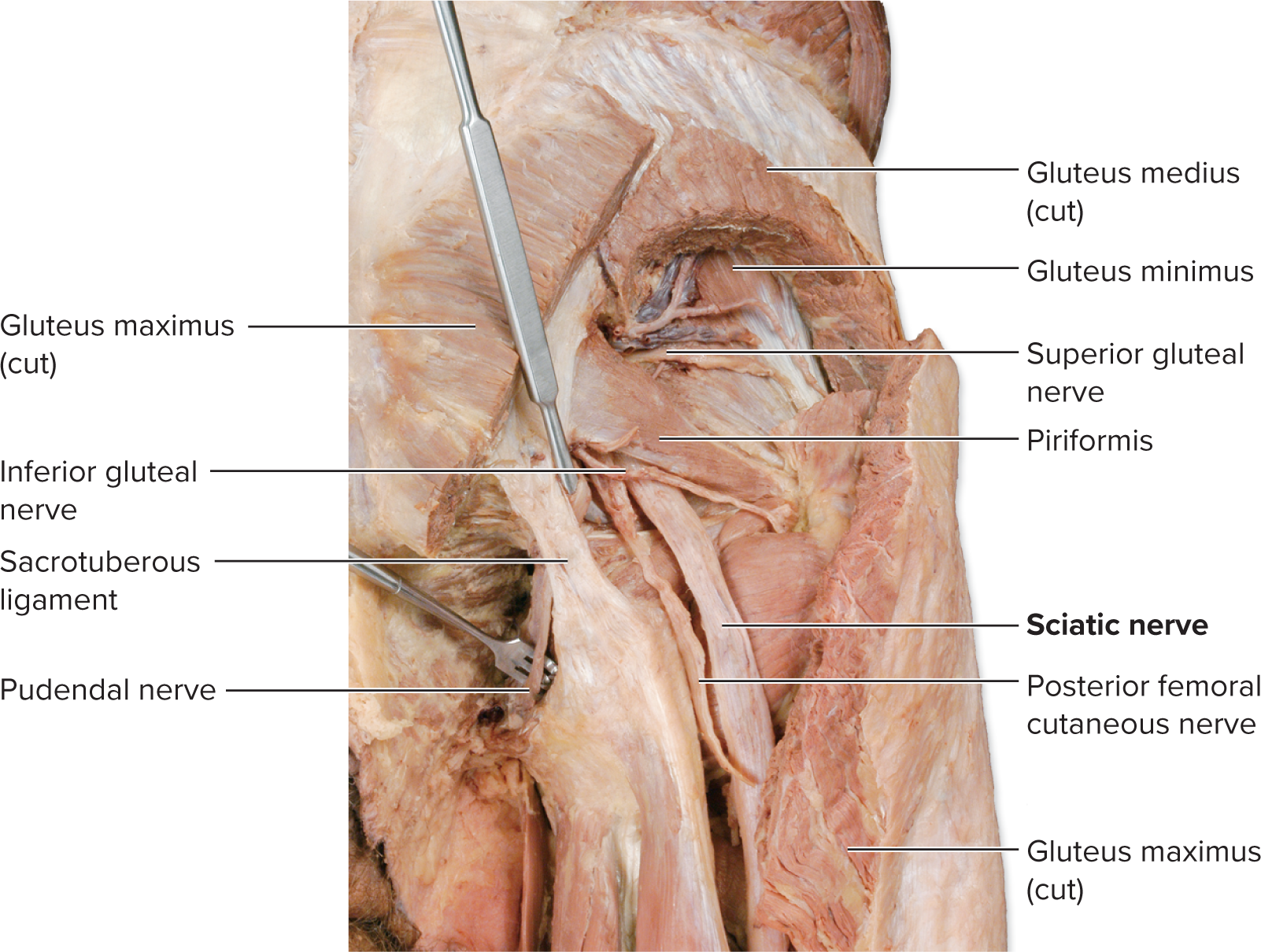
Sacral Plexus (L4–S4) 🦶
The left and right sacral plexuses are formed by the anterior rami of spinal nerves L4 through S4. They are located inferior to the lumbar plexuses (sometimes grouped as the lumbosacral plexus).
Innervation: They supply the pelvis, perineum, gluteal region, posterior thigh, leg, and foot.
Structural Division: The rami are organized into an anterior division and a posterior division:
Anterior Division Nerves: Tend to innervate muscles that flex (or plantar flex) the lower limb.
Posterior Division Nerves: Tend to innervate muscles that extend (or dorsiflex) the lower limb.
Sacral Plexus (L4–S4)
Major Terminal Nerves
1. Sciatic Nerve (Ischiadic Nerve)
The largest and longest nerve in the body.
Formed from portions of both the anterior and posterior divisions of the sacral plexus.
Extends through the posterior thigh. It is actually two nerves (tibial and common fibular) encased in a common sheath.
Nerve | Originating Division | Motor Innervation (Muscles) | Sensory Innervation (Skin Area) |
Tibial Nerve | Anterior Division of Sciatic | Hamstrings (except short head of biceps femoris), plantar flexors of the foot, and toe flexors. | Splits into medial and lateral plantar nerves to supply muscles and skin of the sole (bottom) of the foot. |
Common Fibular Nerve | Posterior Division of Sciatic | Short head of the biceps femoris (hamstring). | Splits into two nerves near the lateral knee. |
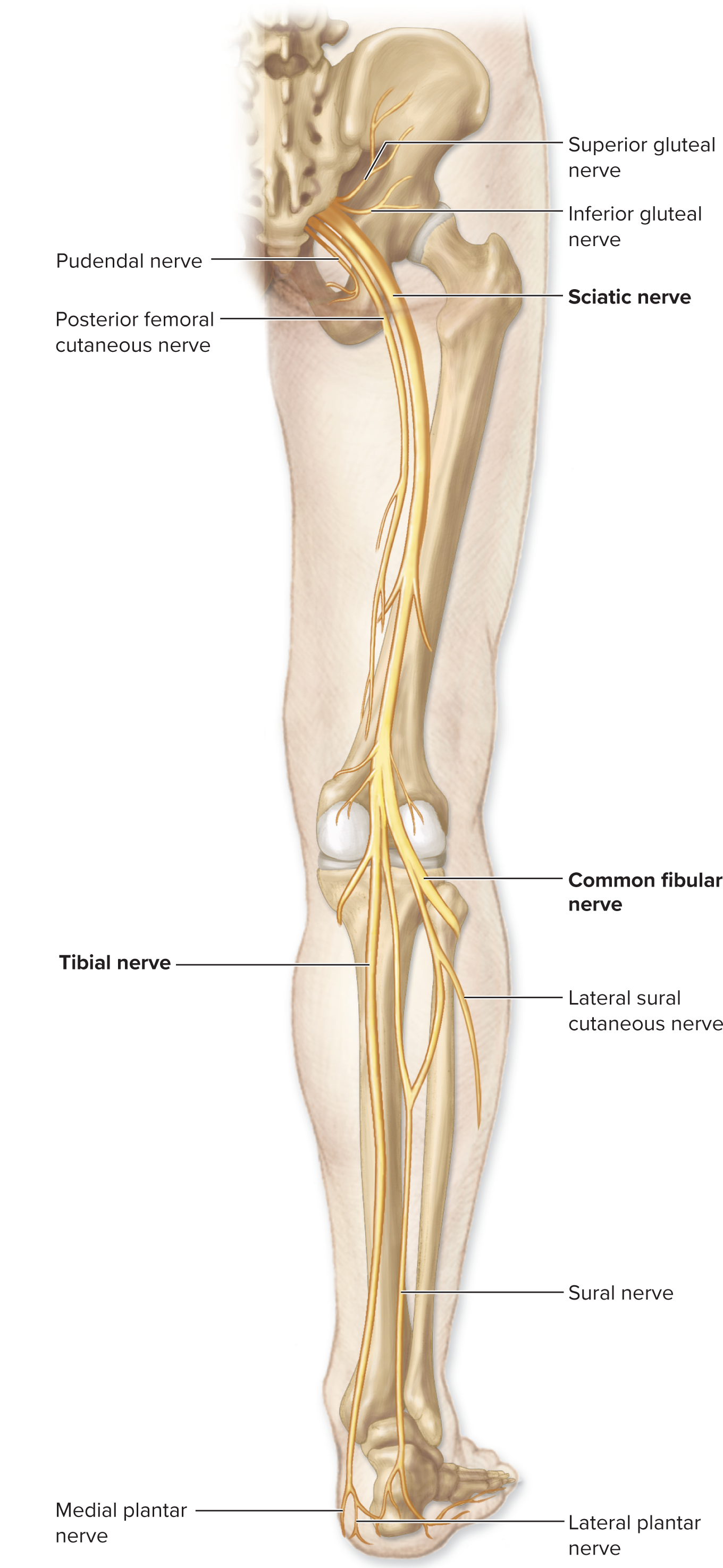
Sacral Plexus (L4–S4)
2. Branches of the Common Fibular Nerve
Branch | Originating Division | Motor Innervation (Muscles) | Sensory Innervation (Skin Area) |
Deep Fibular Nerve | Posterior Division of Sciatic | Anterior leg muscles (dorsiflexors of the foot, extensors of toes). | Skin between the first and second toes on the dorsal foot. |
Superficial Fibular Nerve | Posterior Division of Sciatic | Lateral leg muscles (foot evertors and weak plantar flexors). | Most of the dorsal surface of the foot and anteroinferior leg. |
Branches of the Sacral Plexus
Main Branch | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Sciatic Nerve(Composed of tibial and common fibular divisions wrapped in a common sheath) | L4–S3 | (See tibial and common fibular nerves) | (See tibial and common fibular nerves) |
Tibial Nerve  | 4–S3 | Posterior thigh muscles (extend thigh at hip and flex leg at knee)
Posterior leg muscles (flex leg at knee and plantar flex foot)
Plantar foot muscles (via medial and lateral plantar nerve branches) | Branches to the heel, and via its medial and lateral plantar nerve branches (which innervate the sole of the foot)  |
Common Fibular Nerve(Divides into deep fibular and superficial fibular branches)  | L4–S2 | Short head of biceps femoris (flexes leg at knee); see also deep fibular and superficial fibular nerves | (See deep fibular and superficial fibular nerves) |
Deep Fibular Nerve  | L4–S1 | Anterior leg muscles (dorsiflex foot, extend toes)
Dorsum foot muscles (extend toes)
| Dorsal interspace between first and second toes  |
Superficial Fibular Nerve  | L5–S2 | Lateral leg muscles (evert foot and weakly plantar flex foot)
| Anteroinferior part of leg; most of dorsum of foot  |
Sacral Plexus (L4–S4)
Smaller Branches of the Sacral Plexus | Anterior Rami | Motor Innervation | Cutaneous Innervation |
|---|---|---|---|
Inferior gluteal nerve | L5–S2 | Gluteus maximus (extends thigh) | |
Superior gluteal nerve | L4–S1 | Gluteus medius, gluteus minimus, and tensor fasciae latae (abduct thigh) | |
Posterior femoral cutaneous nerve | S1–S3 | Skin on posterior thigh | |
Pudendal nerve | S2–S4 | Muscles of perineum, external anal sphincter, external urethral sphincter | Skin on external genitalia |
Reflexes
the components of a reflex arc, the classification of reflexes, the different spinal reflexes, and how reflexes are tested in a clinical setting.
Characteristics of Reflexes 🏃♀
A reflex is a rapid, preprogrammed, involuntary response of muscles or glands to a stimulus, serving as a survival mechanism (like quickly pulling your hand from a hot stove).
Key Features of All Reflexes
Stimulus Required: A stimulus is always needed to initiate the reflex.
Rapid Response:
Involves few neurons to minimize the time delay at synapses.
Allows a quick reaction to a harmful situation.
Awareness (conscious thought) of the stimulus occurs after the reflex action is complete.
Preprogrammed Response: The action occurs the same way every time the stimulus is applied.
Involuntary Response:
Requires no conscious intent or effort.
Usually cannot be suppressed.
The Reflex Arc: Pathway of a Reflex
A reflex arc is the neural pathway that executes a reflex. It begins in the PNS, communicates with the CNS, and ends at a peripheral effector.
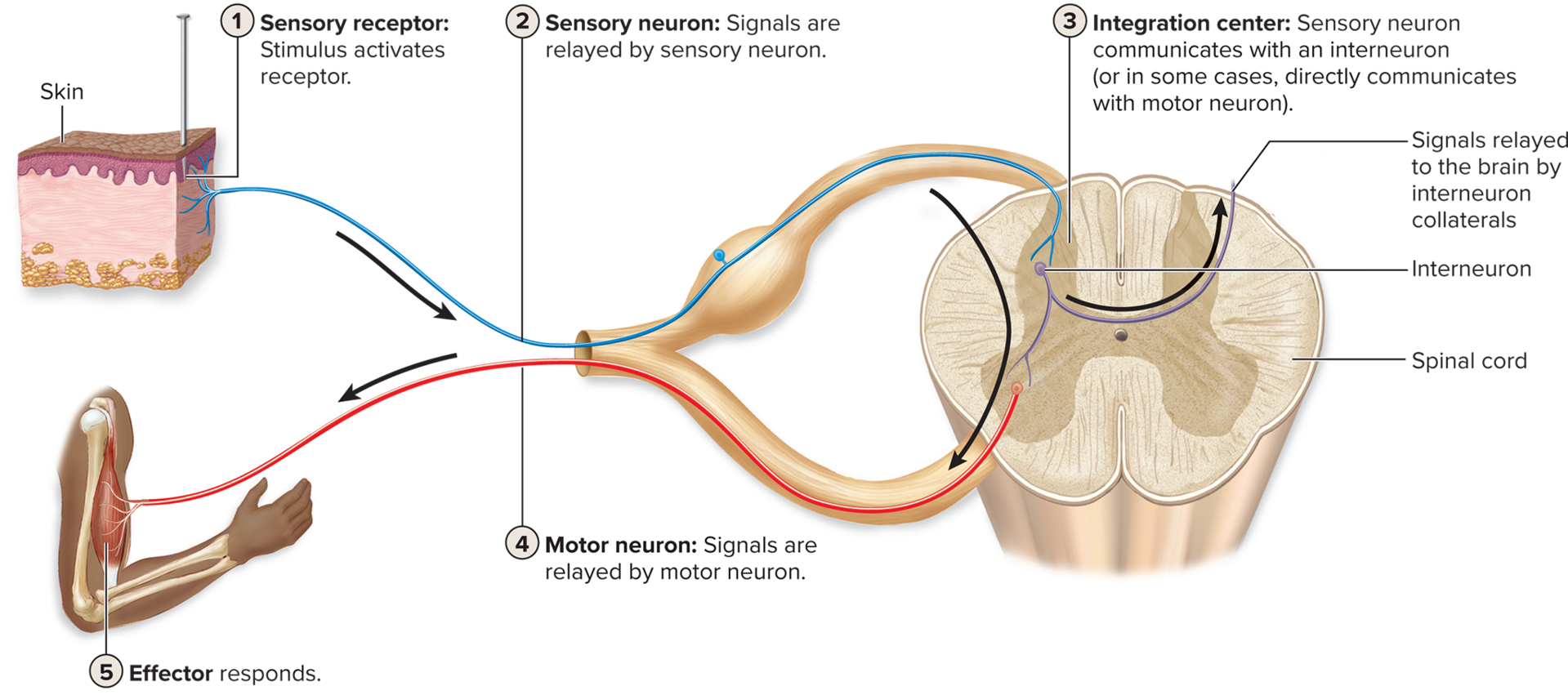
Five Steps in a Reflex Arc
The pathway involves the following general steps:
Stimulus Activates a Sensory Receptor:
A sensory receptor (e.g., in the skin or muscle) detects an external or internal change (like heat or stretch).
Sensory Neuron Relays Signal to the CNS:
The sensory neuron transmits the signal from the receptor to the spinal cord (or brain).
Information is Processed in the Integration Center (CNS):
Interneurons within the CNS gray matter integrate the incoming signal and decide on a response.
Note: The simplest reflexes are monosynaptic (sensory neuron synapses directly onto the motor neuron), lacking an interneuron.
Motor Neuron Relays Signal to an Effector:
The motor neuron transmits the outgoing signal from the CNS to the effector organ.
Effector Responds to the Signal:
The effector (a muscle or a gland) carries out the final response, which is intended to counteract the original stimulus.
Classification of Reflexes
Reflexes can be categorized in five different ways based on their components and characteristics:
Integration Region of the CNS (Processing Site)
Type of Effector Stimulated
Number of Neurons in the Reflex Arc (Complexity)
Relative Location of Receptor and Effector (Side of Body)
Whether the Reflex is Present at Birth or Learned
Integration Region of the CNS (Processing Site)
Spinal Reflexes: The integration center is the spinal cord.
Cranial Reflexes: The integration center is the brain.
Type of Effector Stimulated
Somatic Reflexes: The effector is skeletal muscle (voluntary muscle).
Visceral (Autonomic) Reflexes: The effector is cardiac muscle, smooth muscle, or a gland (involuntary effectors).
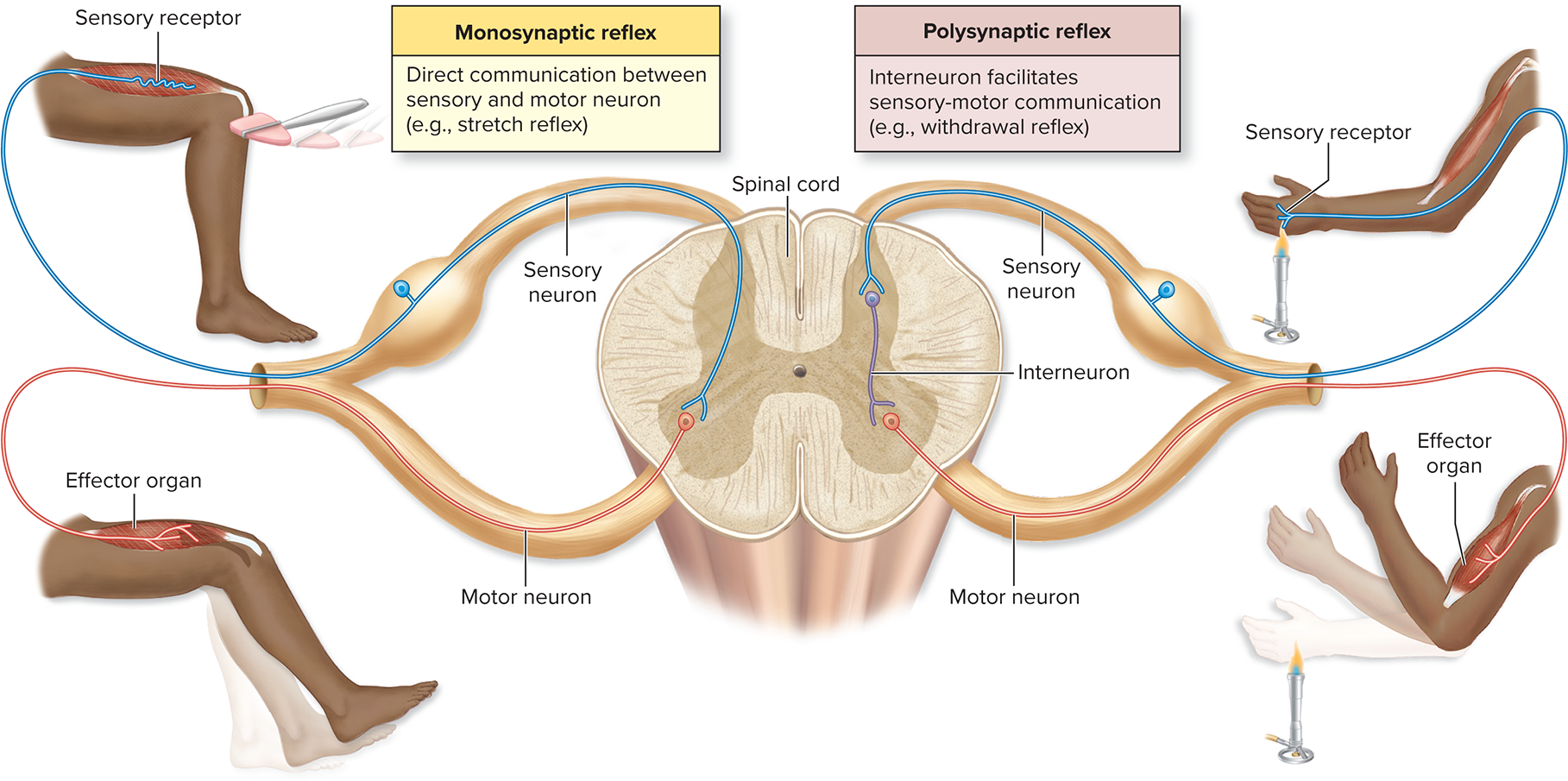
Number of Neurons in the Reflex Arc (Complexity)
Monosynaptic Reflex:
The simplest and most rapid reflex.
Involves only two neurons (one sensory and one motor).
The sensory neuron axon synapses directly on the motor neuron (only one synapse).
Polysynaptic Reflex:
More complicated and less rapid.
Involves one or more interneurons positioned between the sensory and motor neurons.
Relative Location of Receptor and Effector (Side of Body)
Ipsilateral Reflex: The receptor and the effector are on the same side of the spinal cord/body (e.g., pulling your left hand from a hot object).
Contralateral Reflex: The receptor and the effector are on opposite sides of the body (e.g., shifting balance to your right leg when your left foot steps on something sharp). Applicable only to reflexes involving the limbs.
Whether the Reflex is Present at Birth or Learned
Innate Reflex: A reflex that is present at birth (unlearned).
Acquired Reflex: A reflex that is developed (learned) after birth.
Somatic Spinal Reflexes (Skeletal Muscle Effectors)
All of the reflexes discussed here are somatic reflexes (effector is skeletal muscle) and spinal reflexes (integration center is the spinal cord). They are initiated by proprioceptors or pain receptors.
I. Proprioceptor-Initiated Reflexes
These reflexes maintain muscle tone and protect muscles/tendons from damage.
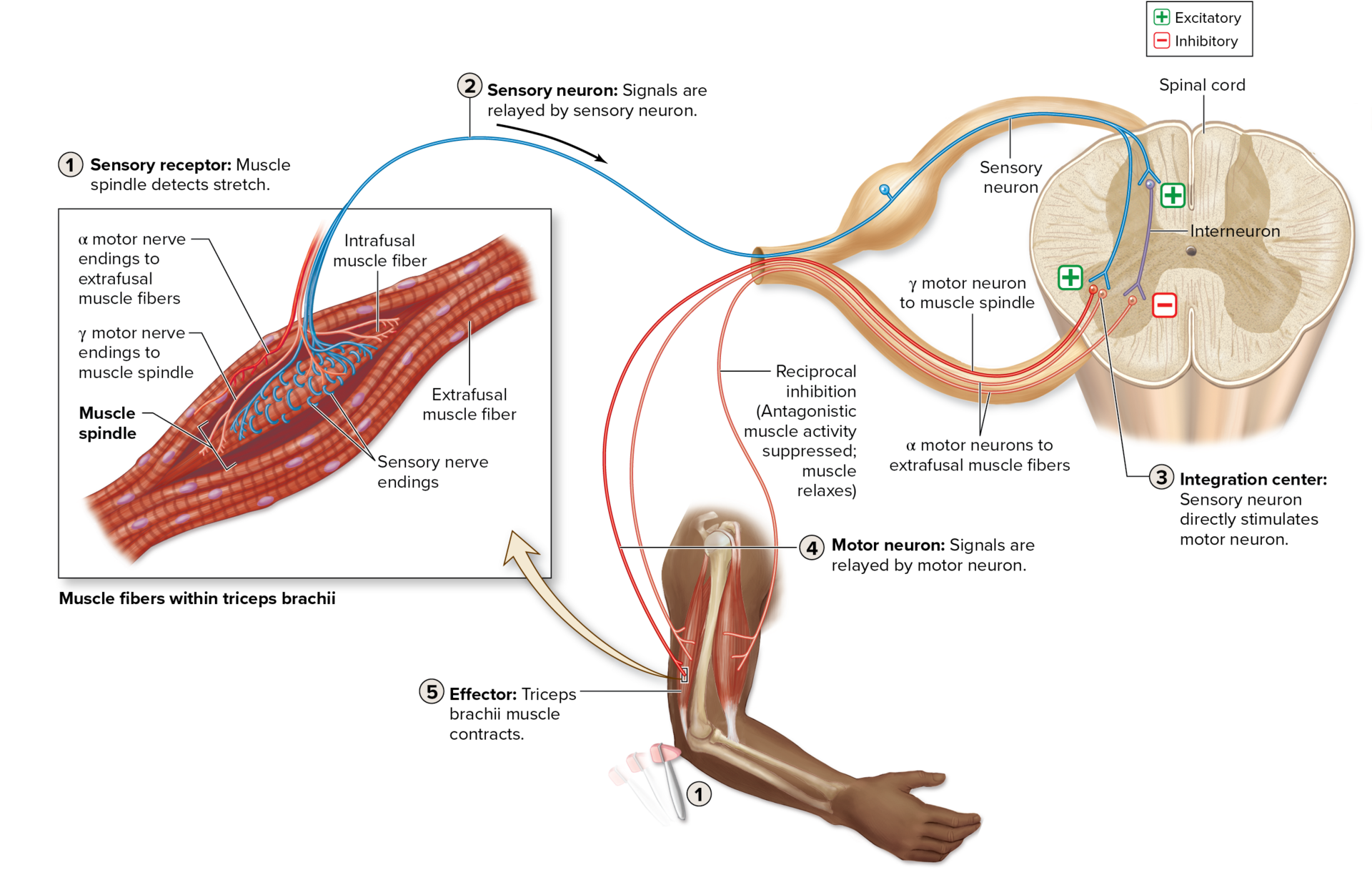
A. Stretch Reflex (Monosynaptic)
Proprioceptor: Muscle Spindle (detects change in muscle stretch).
Action: Muscle reflexively contracts in response to being stretched (prevents excessive stretching).
Example: Triceps reflex (tap on tendon → triceps contracts).
Classification: Spinal, Somatic, Monosynaptic (sensory neuron directly stimulates motor neuron), Ipsilateral, Innate.
Associated Action: Reciprocal Inhibition: Simultaneously, interneurons inhibit the contraction of the antagonistic muscle (e.g., biceps is inhibited during triceps contraction) so movement is unimpeded.
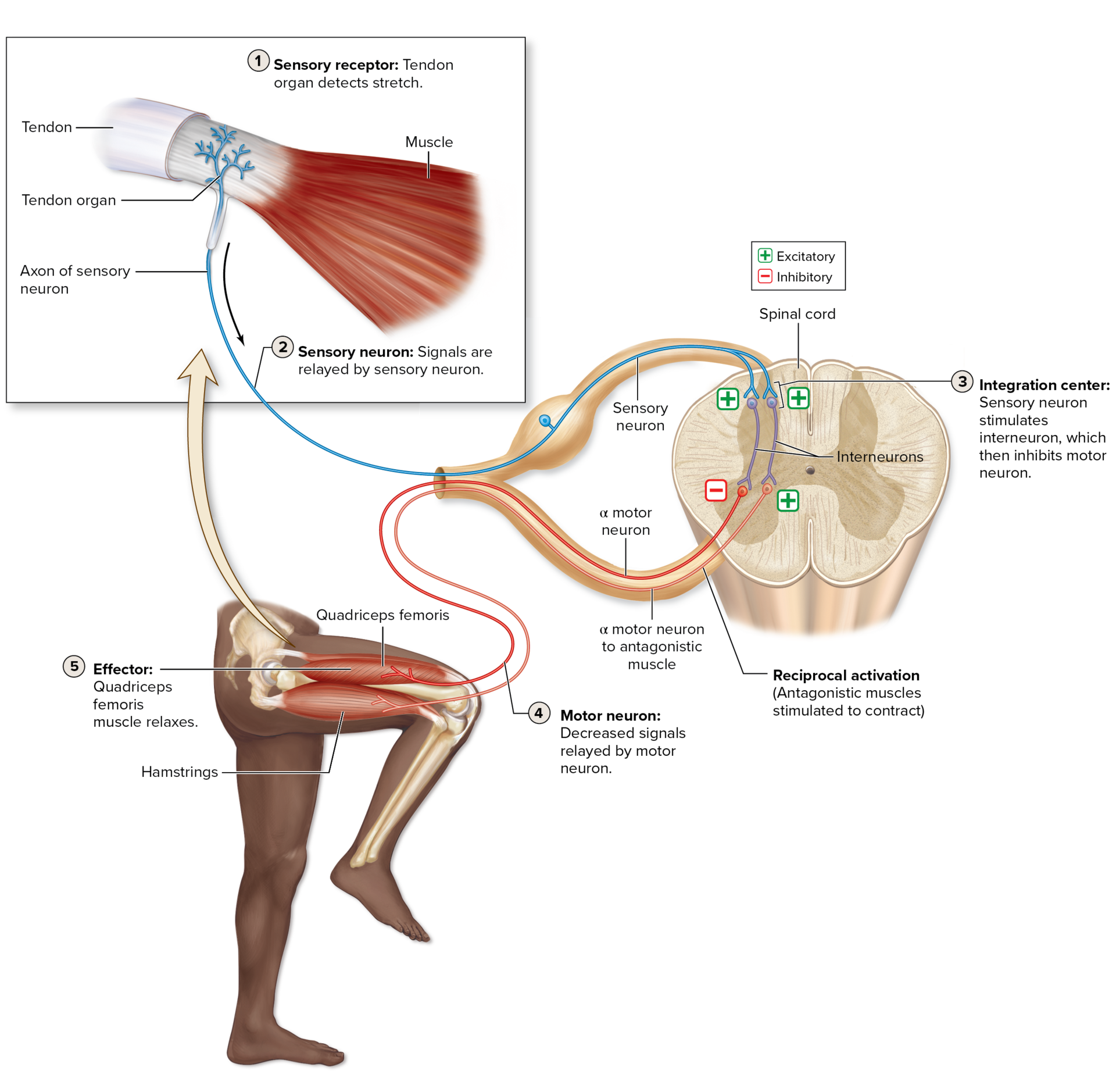
I. Proprioceptor-Initiated Reflexes
B. Tendon Reflex (Polysynaptic)
Proprioceptor: Tendon Organ (detects change in muscle tension).
Action: Muscle reflexively relaxes in response to excessive tension (prevents tearing of muscle/tendon).
Mechanism: Increased tendon tension → Sensory neuron stimulates inhibitory interneurons in spinal cord → Inhibition of the α motor neuron to that muscle → Muscle relaxes.
Associated Action: Reciprocal Activation: Simultaneously, the antagonistic muscle is stimulated to contract (e.g., hamstrings contract while quadriceps relax).
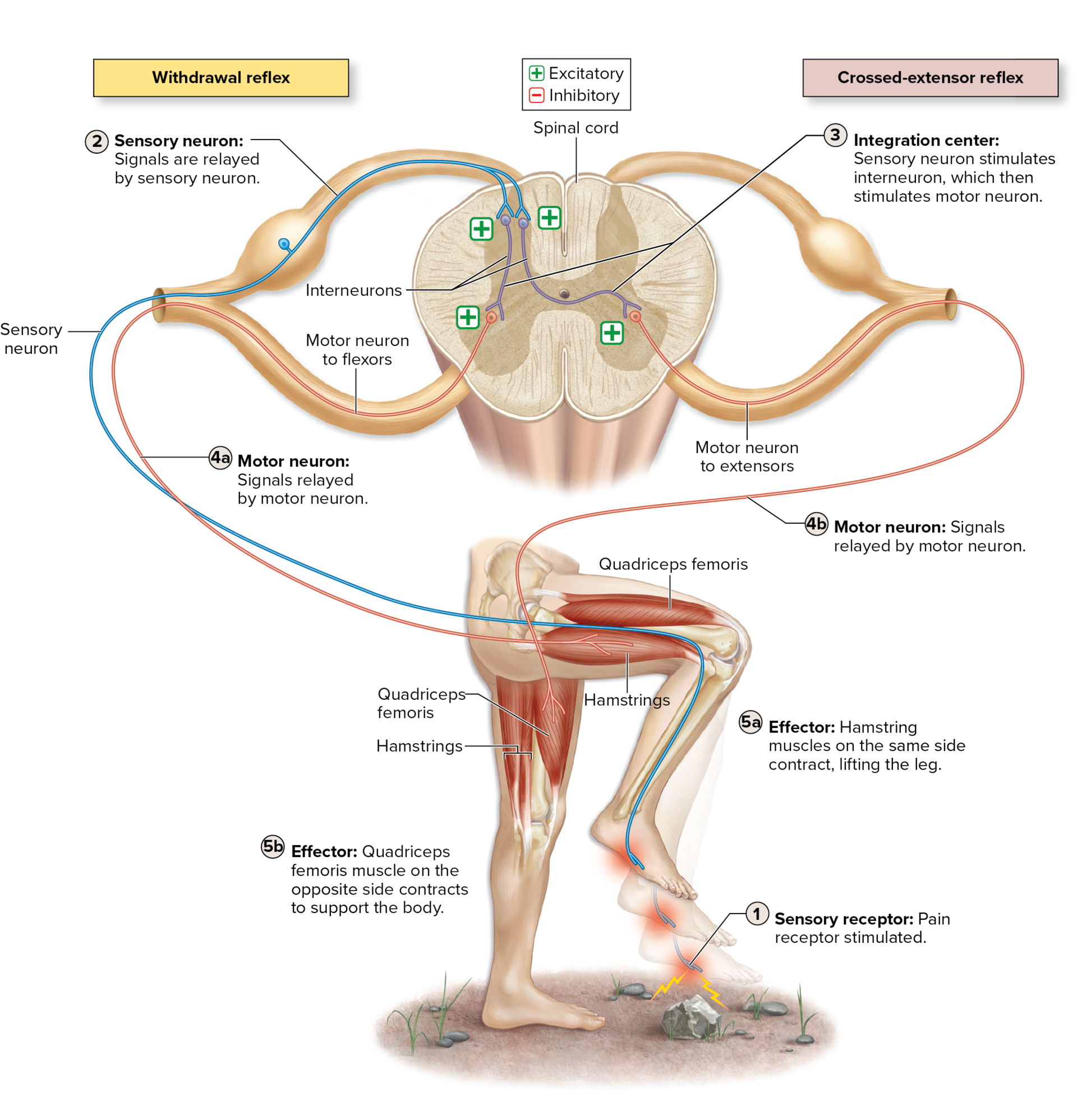
II. Pain Receptor-Initiated Reflexes
These reflexes protect the body from a painful or damaging stimulus.
A. Withdrawal Reflex (Flexor Reflex)
Receptor: Nociceptors (pain receptors).
Action: Involves muscles contracting to immediately withdraw the body part from a painful stimulus (e.g., pulling a hand from a hot object, lifting a foot from a sharp object).
Mechanism: Pain stimulus → Sensory neuron stimulates interneurons → Stimulation of α motor neurons for flexor muscles → Limb moves away.
Associated Action: Reciprocal inhibition of the antagonistic (extensor) muscles ensures the withdrawal is fast and unimpeded.
II. Pain Receptor-Initiated Reflexes
B. Crossed-Extensor Reflex (Contralateral)
Action: Occurs simultaneously with the withdrawal reflex in the opposite, weight-bearing limb.
Mechanism: Sensory input from the injured side crosses over through the gray commissure to the opposite side → Stimulates α motor neurons for extensor muscles on the opposite limb → The opposite limb contracts to extend and bear body weight, helping to maintain balance.
Classification Note: This is an example of a Contralateral Reflex.
Some Clinically Important Reflexes
Reflex | Spinal Nerve Segments Tested | Clinically Normal Action of Effector |
|---|---|---|
Biceps reflex | C5, C6 | Flexes forearm at the elbow joint when biceps brachii tendon is tapped |
Triceps reflex | C6, C7 | Extends forearm at the elbow joint when triceps brachii tendon is tapped |
Abdominal reflexes | T8–T12 | Contract abdominal muscles when one side of the abdominal wall is briskly stroked |
Cremasteric reflex | L1, L2 | Elevates testis (due to contraction of cremaster muscle in scrotum) when medial side of thigh is briskly stroked |
Patellar (knee-jerk) reflex | L2–L4 | Extends leg at the knee joint when patellar ligament is tapped |
Ankle (Achilles) reflex | S1 | Plantar flexes foot at the ankle joint when calcaneal tendon is tapped |
Plantar reflex | L5, S1 | Flexes toes when plantar side of foot is briskly stroked1 |
A reflex response may be normal, hypoactive, or hyperactive.
Hypoactive Reflex
is a reflex response that is diminished or absent. A hypoactive spinal reflex may indicate damage to a segment of the spinal cord, or it may suggest muscle disease or damage to the neuromuscular junction.
Hyperactive Reflex
is an overly strong response. A hyperactive spinal reflex may indicate damage somewhere in either the brain or spinal cord, especially if it is accompanied by clonus (klō′nŭs; klonus = tumult), rhythmic oscillations between flexion and extension, when the muscle reflex is tested.
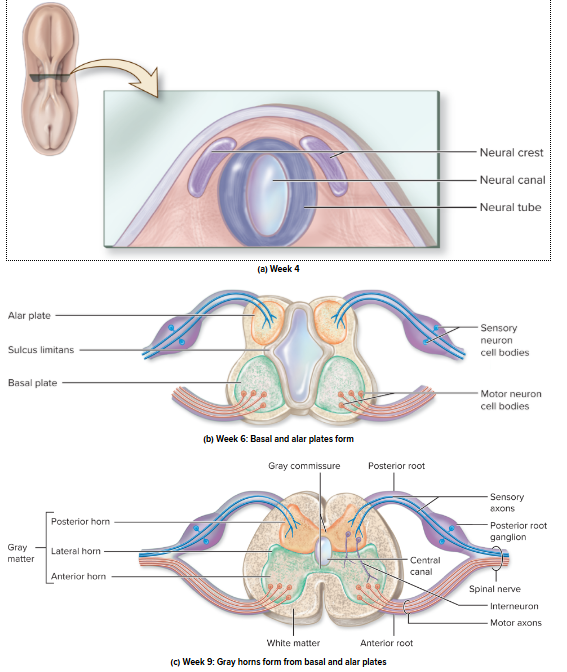
Development of the Spinal Cord
The spinal cord develops from the caudal (inferior) part of the neural tube during embryonic development.
Development of the Spinal Cord
Internal Differentiation (Gray Matter)
The hollow neural canal within the neural tube develops into the narrow central canal of the spinal cord.
By the sixth week, a horizontal groove called the sulcus limitans divides the lateral walls of the neural tube into two regions:
Basal Plates (Anterior): Develop into the anterior and lateral horns of the gray matter (motor functions).
Alar Plates (Posterior): Develop into the posterior horns of the gray matter (sensory functions).