Calcium lectures 19/20
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
What is the difference between intracellular and extracellular calcium
Intracellular calcium is maintained at v low concentrations
Extracellular calcium is present much higher concentrations
functions of extracellular calcium
allows bone mineralisation
maintains normal activity of excitable tissues
normal range for calcium
2.1-2.6 mmol/L
exists in ionised calcium and as albumin-bound calcium
what can cause low or high albumin
low albumin - by infection, malignancy, malnutrition
high albumin - by dehydration
Calcium balance changes throughout life
growth = needs +ve calcium balance
adulthood = neutral balance
ageing = slow negative calcium balance esp in menopause
What do osteoblasts do
responsible for bone matrix mineralisation
sit close to each other and work together to respond
What happens in bone matrix mineralisation
takes several months - usually a delay of several days before osteoid is mineralised
mineralisation of osteoid depend on calcitriol
What provides rigidity and resistance to compression in bone
tiny crystals surrounding collagen fibres
what happens in vitamin D deficiency
failure to mineralise = rickets in children and osteomalacia in adults
Alkaline phophatase (ALP) mineralisation
ALP expressed on surface of differentiated osteoblasts
released ino ECF
releases inorganic phosphate ions via hydrolysis
how does ALP promote mineralisation
increases local concentration of inorganic phosphate ions
hydrolyses pyrophosphatase (key inhibitor of mineralisation) to 2 phosphate ions
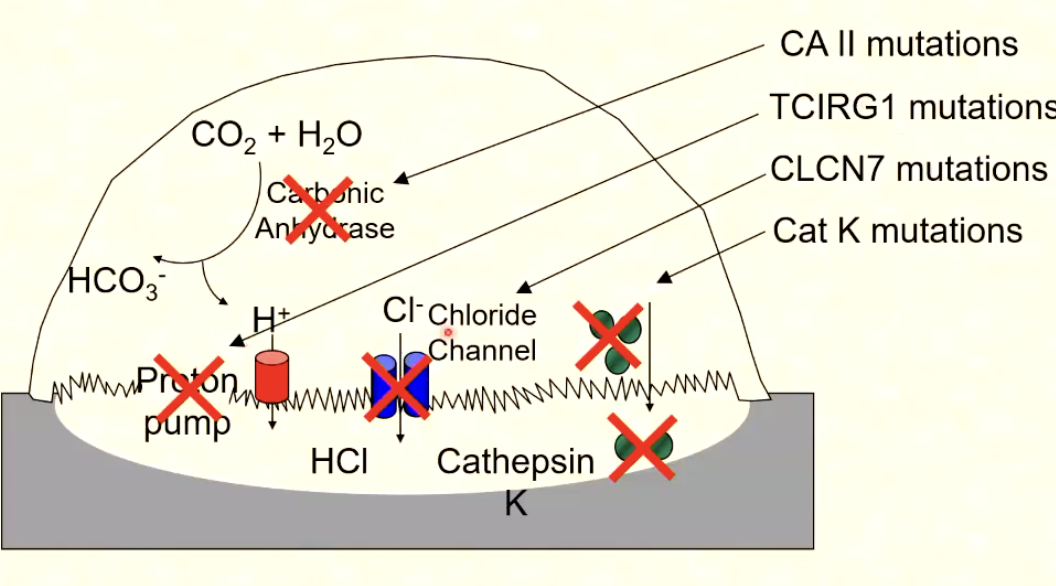
What are osteoclasts
responsible for bone resorption
multinucleated, motile cells
secrete H+ ions and enzymes in their ruffled border
express lots of carbonic anhydrase II (for H+ generation)
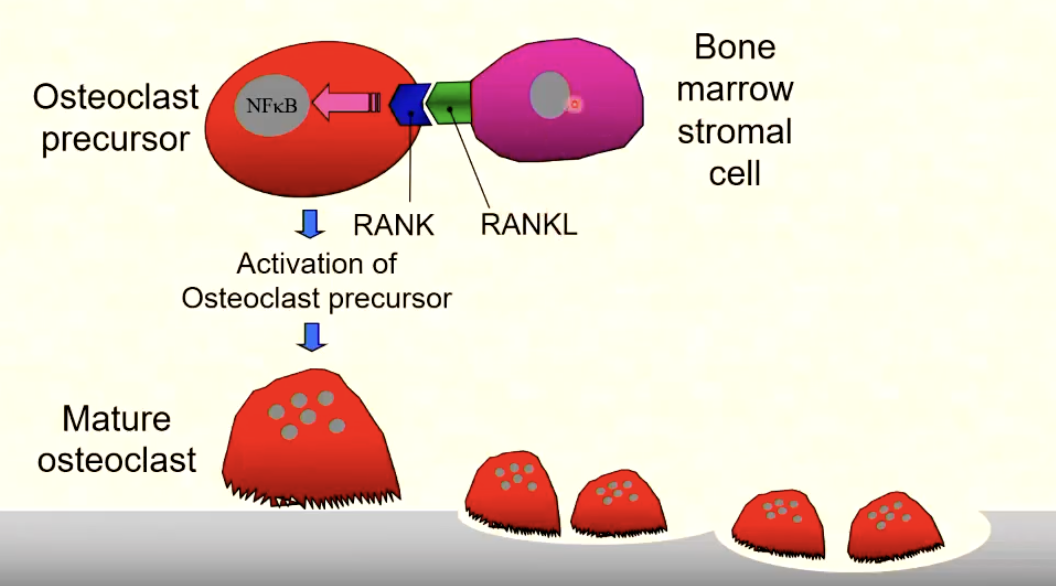
What is RANK-RANKL?
A pathway essential for osteoclast differentiation and activation
RANKL (on osteoblasts) binds to RANK receptors (on osteoclast precursors) to promote maturation and activation
How do osteoclasts resorb bone
they demineralise and chew through bone via secretion of an acid and enzymes that break down bone matrix components
What is osteopetrosis
Failure of matrix degradation by osteoclasts
occurs due to proton pump failure » chloride channel defects
= abnormally dense bones that are brittle
What are bone functions
Spport the body and protext organs
leverage system for movement
site of hematopoiesis (new blood cell formation)
endocrine function
mineral homeostasis
What are osteocytes
Most abundant cell type in bone - mechanosensors
What is the bone remodelling cycle
quiescence - no active bone turnover occuring
resorption - osteoclasts activate and resorb bone (small cavity)
Reversal - osteoclasts apoptose and replaced by osteoblasts
formation - osteoblasts secrete osteoid which mineralises = new tissue
mineralisation -
How is ionised calcium regulated
PTH and calcitriol in endoccrine feedback loops
PTH physiology
Regulated calcium
In low Ca2+ » PTH increases
high Ca2+ feeds back to Parathyroid to suppress PTH in negative feedback
tightly contrlled
Calcium-sensing receptors on cell surfaces detect Ca2+ levels to regulate secretion
Ca2+ binding activations G-protein coupled receptors
What does PTH do
stimulates effluc of Ca2+ from bone
stimualtes renal tubule reabsorption of calcium
promotes phosphate and bicarb loss from kidney
indirectlt stimulats intensinal absorption of Ca2+
Calcitonin
secreted by thyroid C cells
hormone
lowers plasma calcium by inhibition of bone resorption and increasing calcium deposition in bone
Vitamin D metabolism action in liver
Skin: Uv light » 7-dehydrocholesterol converted to cholecalciferol (vitaminD3)
Liver: 25 -hydroxylase converts VitD3 to 25-hydroxycholecalciferol (calcidiol)
Kidney: 1-alpha-hydroxylase converts calcidiol » 1,25(OH)2 D (calcitriol (active form)
PTH stimulates 1alpha-hydroxylase in low Ca2_
where does Vit D come from in diet
Oily fish, butter, eggs, margarine
Cholecalciferol present in foods are activated by liver and kidney to form calcitriol (1,25-dihydroxycholecalciferol) - active form
What is calcitriol needed for
long-term maintenance of calcium levels, normal bone growth, mineralisation
Mechanism of calcitriol Action
Calcitriol binds to vitamin D receptor = VDR-calcitriol complex (VDRC)
VDRC » acts to regulate calcium and phosphate metabolism
Stimulates osteoclasts = ^^ Ca2+ efflux from bone (^^renal Ca2+ reabsoprtion
Phosphate regulation
calcium balance and mineralisation
PTH and vit D interact to maintain phosphate levels
Kidney: acts with PTH to conserve calcium
PTH secretion
Increased blood Ca2+ = decreased PTH secretion
maintains normal Ca2+ homeostasis in negative feedbacl
What does PTH act to do
increase bone resorption, decrease urinary calcium loss, increase calcitriol production in kidney
Effects of 25(OH)D deficiency on Ca2+ metabolism
↓ intestinal Ca²⁺ absorption → ↓ blood Ca²⁺.
↓ Ca²⁺ → ↑ PTH (secretion ↑).
↑ PTH → phosphate wasting in kidneys.
Result = bone de-mineralisation and secondary hyperparathyroidism
PTH vs calcitriol
Function | PTH | Calcitriol (1,25(OH)₂D) |
Timescale | Minute-by-minute | Longer-term |
Plasma Ca²⁺ effect | Increases ionised Ca²⁺ | Maintains plasma Ca²⁺ |
Phosphate effect | ↓ plasma phosphate | ↑ plasma phosphate |
Major site of action | Kidney + bone | Gut + bone + kidney |
Stimulus for secretion | ↓ Ca²⁺ | ↑ PTH or ↓ phosphate |
Interaction of PTH and calcitriol
Co-operative action:
PTH promotes 1α-hydroxylase activity → ↑ calcitriol.
Both required for osteoclast activation and bone remodelling.
Feedback inhibition:
^^ calcitriol = ^ 24-hydroxylase → inactivation pathway.
Calcitriol can switch off PTH gene transcription via vitamin D receptor (VDR) in parathyroid cells.
Disorders of Calcium (high calcium)
Stones, bones, abdominal moans, psychic groans
muscle weakness - (competition with Na+ movement)
CNS (anoerxia, nausea)
renal, bone, abdominal effects
ECG changes
What is false hypercalcaemia
Dehydration = Raised calcium due to high plasma albumin
so must check ionised calcium
What is primary hyperparathyroidism
Autonomous and inappropriate overproduction of PTH
raised calcium » low Phosphate and bicarb
ALP normal or slightly high
imaging of PTH
Primary hyperparathyroidism causes
Caused by adenoma, hyperplasia, or carcinoma
Treatment of prumary hyperparathyroidism
Acute management:
Treat high ionised calcium with rehydration or drugs.
Definitive treatment:
Surgical removal of parathyroid adenoma.
Mild cases:
Managed with follow-up of serum calcium and PTH levels.
If surgery not possible:
Use drugs to lower calcium (e.g. calcimimetics).
2ndary vs 3ary hyperparathyroidism
2ndary - appropriate increase in PTH due to hypocalcaemia caused by renal failure or malabsorption
3rary hyperparathyroidism - overactive hyperPTH gland = v high PTH = hypercalcaemia. caused by worsening of secondary HPT (CKD)
Malignant Disease and hypercalcaemia
20–30% of cancer patients develop hypercalcaemia during their illness.
Mechanisms of tumours leading to hypercalcaemia
Tumours secreting PTH-peptide = hypercalcaemia of malignancy (hodgkins ly,phoma synthesis calcitriol
metastatic tumour in bone stimulate osteoclast activation (bone resorption) (usually from lung and breast cancer)
what is multiple myeloma
blood cancer from too many plasma cells in bone marrow
plasma cells release cytokine and activate osteoclasts = hypercalcemia from bone resporption
Diagnosing malignant hypercalcaemia
^calcium + suppressed PTH
^ phosphate and ALP
Hydrate patient or use drugs to lower blood calcium to trwat
Causes of hypercalcaemia
granulomatous disease - affect lung and skin = high calcium normal PTH
»» caused by hydroxylation of vitamin D in granulomas
Exogenous vitamin D excess.
Hypocalciuric hypercalcaemia:
Calcium-sensing receptor on PT glands less sensitive to calcium.
Altered set point for PTH/Ca²⁺ interaction.
PTH slightly raised, ionised calcium raised, urine calcium low.
Drugs (e.g. thiazides, lithium).
Other endocrine diseases: Addison’s disease, thyrotoxicosis.
Prolonged immobilisation.
Low blood calcium causes
high neuromuscular excitability
Neuromuscular symptoms: numbness, anxiety, fatigue, muscle cramps, seizures.
Mental state changes: personality change, mental confusion, psychoneurosis, impaired intellect.
ECG changes, eye problems (cataracts, papilloedema).
Chvostek’s sign: tapping facial nerve → eye/mouth twitch.
Trousseau’s sign: carpal spasm after BP cuff inflation.
Factitious hypocalcaemia
due to low plasma albumin (liver disease, nephrotic syndrome (albumin lost in urine))
dietary lack of protein
treated via IV or oral calcium, close monitoring
what happens if low vitD
↓ Vitamin D → ↓ calcium uptake in gut → triggers PTH secretion → phosphate wasting → weak bones.
or
Less calcium absorption → secondary hyperparathyroidism → phosphate loss → bone weakening.
i.e low calcium phosphate and high ALP and PTH
= osteomalacia or rickets
What are inheritied cause of rickets
deficient 1-hydroxylase enzyme
defective vitamin D receptor
What is osteomalacia
Bone disorder associated with vitamin D deficiency.
Osteoid laid down by osteoblasts is not adequately calcified.
Osteoid content in bone ↑ at the expense of normal mineralised bone.
Bones softened, weak, and fracture-prone.
causes of hypoparathydrodism
surfical damage to PT glands
suppressed secretion
genetics
What is osteoporosis
reduced bone mineral density - shows up as normal ca, phosphate, ALP)
Caused by more bone resorption over formation
occurs in age, post-menopause
diagnosed with x-ray (DEXA scan)
Managemne of osteoporosis
life - weight decrease, stop smoking, higher calcium and vit D intake
Pharmacological:
Bisphosphonates (inhibit bone resorption).
Selective oestrogen receptor modulators (SERMs).
Calcitonin, denosumab, or PTH analogues in severe cases.