Solute & Water Handling, pt.1 - Transport of Sodium & Chloride
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
How does the kidneys help maintain the body's ECF volume?
via regulating amount of Na+ in urine
Which solute is most important contributor to osmolality of ECF?
Na+ ==> water follows wherever Na+ goes
True or False: The normal daily urinary excretion of Na+ is only a small fraction of the total Na+ filtered by the kidneys.
True
By the time the tubule fluid reaches the renal pelvis, the kidneys reabsorbs _____________% of the filtered Na+.
approx 99.6%
which part of the nephron reabsorbs the largest fraction of filtered Na+?
Proximal Convoluted Tubule ==> approx 67% Na+ reabs here
If the majority of Na+ is reabsorbed in the Proximal Convoluted Tubule, why don't diuretics typically target transporters in this area?
b/c the effects on osmolarity of the ECF/blood will be too severe
How much Na+ is reabsorbed in the loop of henle?
approx 25%
True or False: The segments between the distal convoluted tubule and the cortical collecting tubule reabsorb 25% of filtered Na+ load.
False ==> reabs approx 5%
How much of the filtered Na+ does the medullary collecting duct reabsorb?
approx 3%
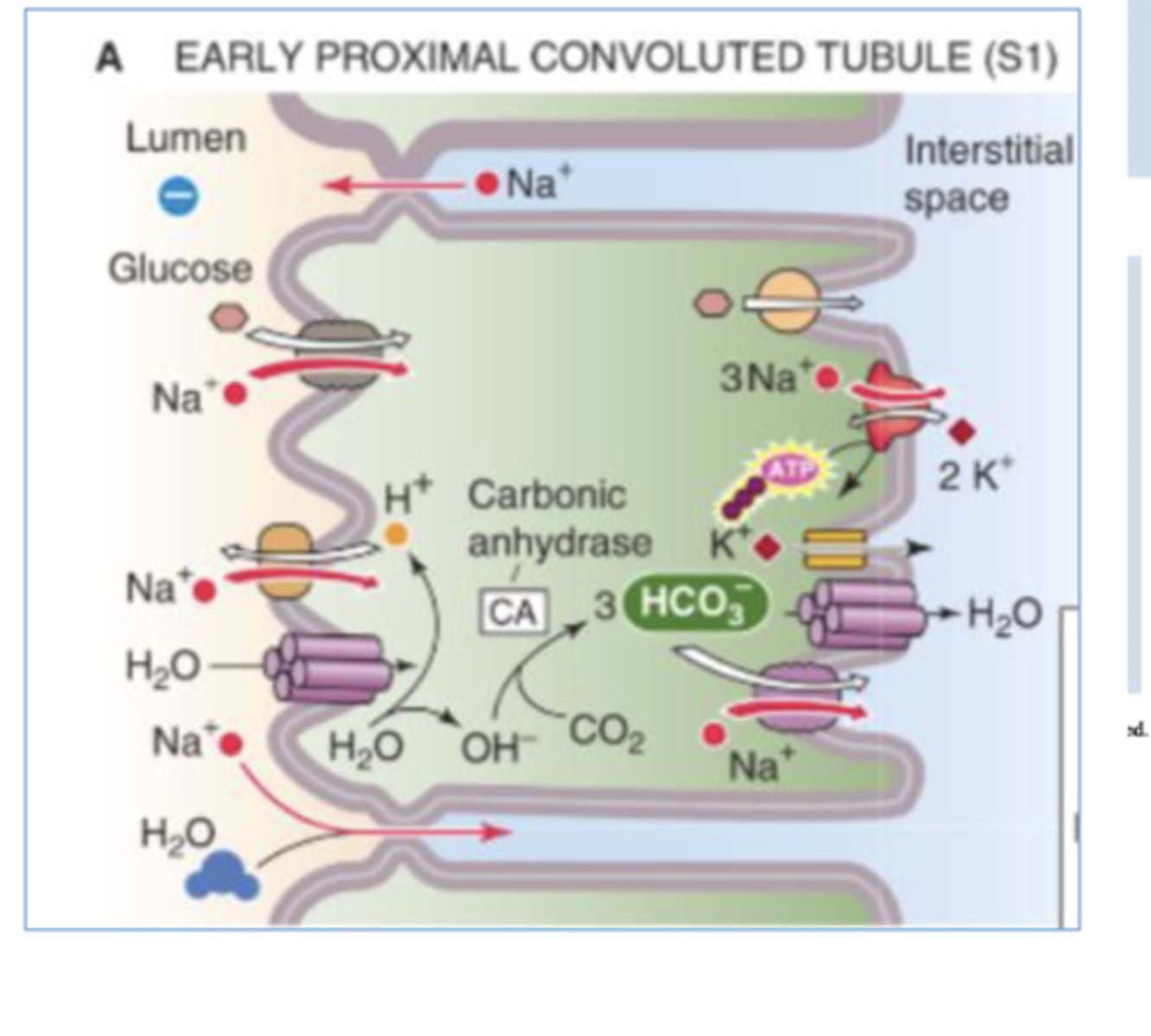
Describe the two ways that a tubule can reabsorb Na+ & Cl-
-transcellular pathway --> cross the apical & basolateral membranes before entering blood (depends on electrochem gradients, ion channels, & transporters)
-paracellular pathway --> move thru tight junctions bwtn cells (extracellular
Which solutes are reabsorbed with Na+ in the first half of the Proximal Convoluted Tubule?
-HCO3-
-glucose
-amino acid
-phosphate
-lactate
-sulfate
-mono & dicarboxylic acids
-etc
*variety of cotransporters in the apical membrane couples Na+ influx down it's conc gradient to uptake of solutes going against their gradient
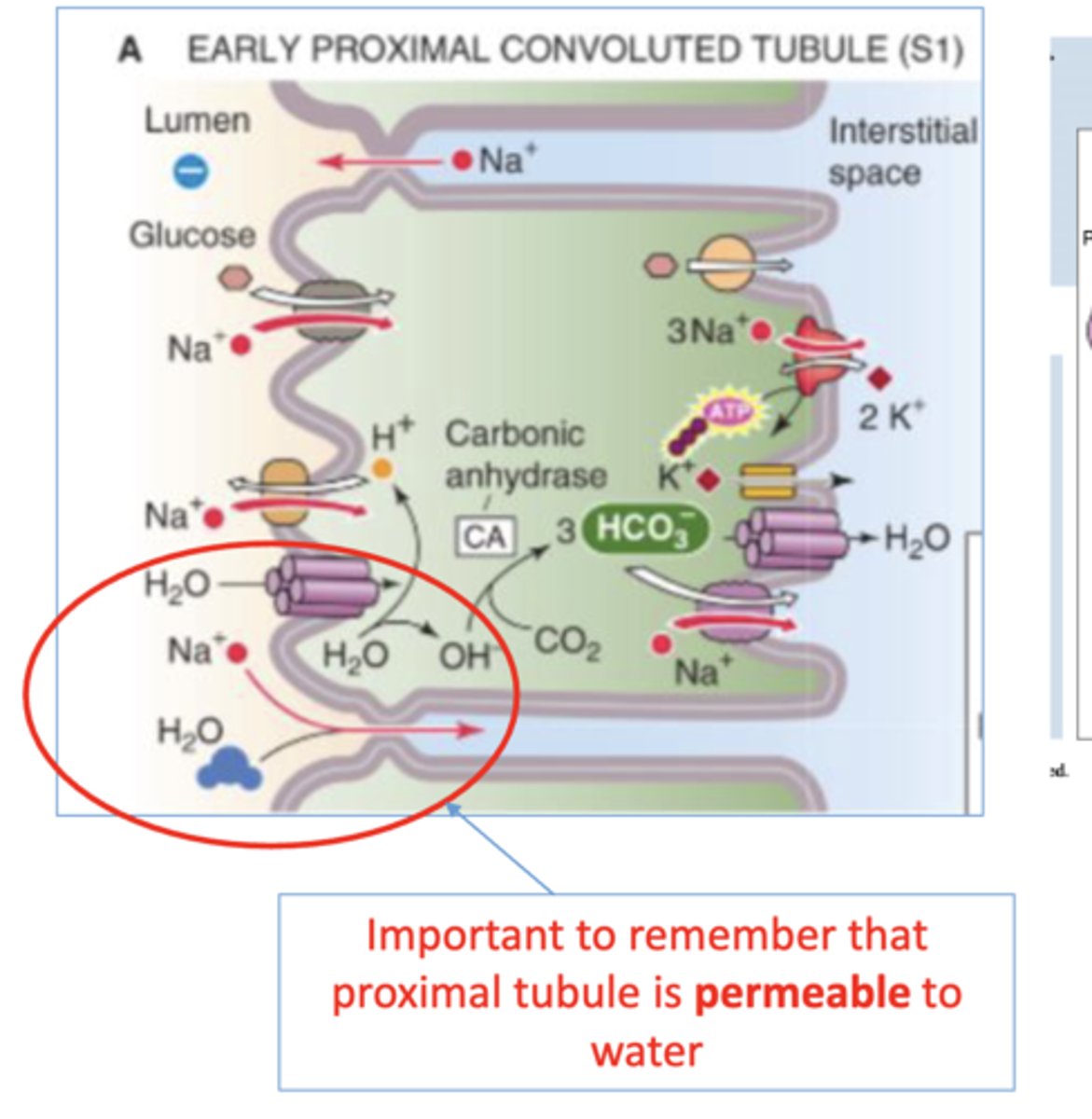
Which solutes are reabsorbed with Na+ in the second half of the Proximal Convoluted Tubule?
-mainly reabs w/ Cl-
-also variety of cotransporters in apical membrane to couple uptake of many solutes to uptake of Na+ (like in 1st half of PCT)
-Na+ uptake coupled to excretion of H+
True or False: The Proximal Convoluted Tubule is permeable to water
True
Faconi Syndrome
hereditary or acquired renal disease that results from impaired ability of PCT to reabs HCO3-, phosphate, amino acids, glucose, & low molecular wt proteins ==> increased urinary excretion of these b/c downstream tubules can't reabs these.
*see polyaminoacidouria --> all types of low molecular wt AA & proteins in urine
Mannitol
osmotic diuretic that gets filtered into the tubular space at PCT--> increases tubular fluid osmolarity --> attracts water into lumen--> decreases reabs of fluid (water) --> increases excretion of water
*used to tx brain edema
Why are osmotic diuretics like mannitol only effective at the proximal convoluted tubule?
permeable to water
Describe how bicarbonate (HCO3-) is reabsorbed.
primarily reabs at PCT==> H+ secreted into tubular lumen --> combines w/ filtered HCO3- --> forms H2CO3 --> carbonic anhydrase converts into CO2 & H2O --> CO2 enters PCT cell --> combines with H2O --> forms H2CO3 --> HCO3- & H+ --> HCO3- exits basolateral membrane to be reabs --> H+ secreted into tubule lumen
carbonic anhydrase inhibitors
inhibits the reabs of bicarcbonate by blocking carbonic anhydrase from converting H2CO3 into CO2 & H2O in PCT lumen --> increased excretion of bicarbonate
*can cause metabolic acidosis
*used to Tx glaucoma sense ocular fluid & CSF production depend on carbonic anhydrase (not usually given to induce diuresis)
What are the 2 major mechanisms for taking up Na+ at the Thick Ascending Limb of Loop of Henle?
-Na+/K+/2Cl- cotransporter (NKCC2) --> all reabs; drives inward movement of ions via Na+ & Cl- moving down its conc gradient
-Na+/H+ antiporter (NHE3) --> Na+ influx in exchange for H+ efflux
True or False: Furosemide inhibits the Na+/Cl- cotransporter in the distal convoluted tubule.
False ==> inhibits the Na+/K+/2Cl- in the thick ascending loop of henle.
bumetanide
loop diuretic that inhibits the Na+/K+/2Cl- cotransporter in the thick ascending limb of loop of henle
True or False: The thick ascending limp of the loop of henle is permeable to water.
False ==> impermeable to water
*reuptake of Na+ & Cl- in the thick ascending loop makes the tubular fluid hypoosmotic
why is the thick ascending loop of henle called the "diluting segment"?
b/c it is not permeable to water, but reuptakes Na+ & Cl- from tubular lumen --> dilutes tubular fluid
Where in the nephron would you expect to find the most diluted urine?
@ the end of the thick ascending loop of henle = beginning of DCT
Where in the nephron would you expect to find the most concentrated urine?
@ the tip of the thin descending loop of henle (the bottom of the loop of henle)
In which part of the nephron is water normally reabsorbed to concentrate the urine?
thin descending loop of henle
How is Na+ reabsorbed in the distal convoluted tubule?
Na+/Cl- cotransporter in apical membrane
True or False: Distal Convoluted Tubule is permeable to water
False
True or False: Thiazide diuretics inhibit sodium reabsorption in the distal convoluted tubule.
True ==> inhibits the Na+/Cl- cotransporter in apical membrane of DCT
ex: hydrochlorothiazide
How is Na+ reabsorbed in the cortical collecting tubules?
epithelial Na+ channels (ENaCs) @ apical membrane of the principal cells
*changing the levels of aldosterone or vasopressin/ADH may modulate the # of Na+ channels that are open in apical membrane
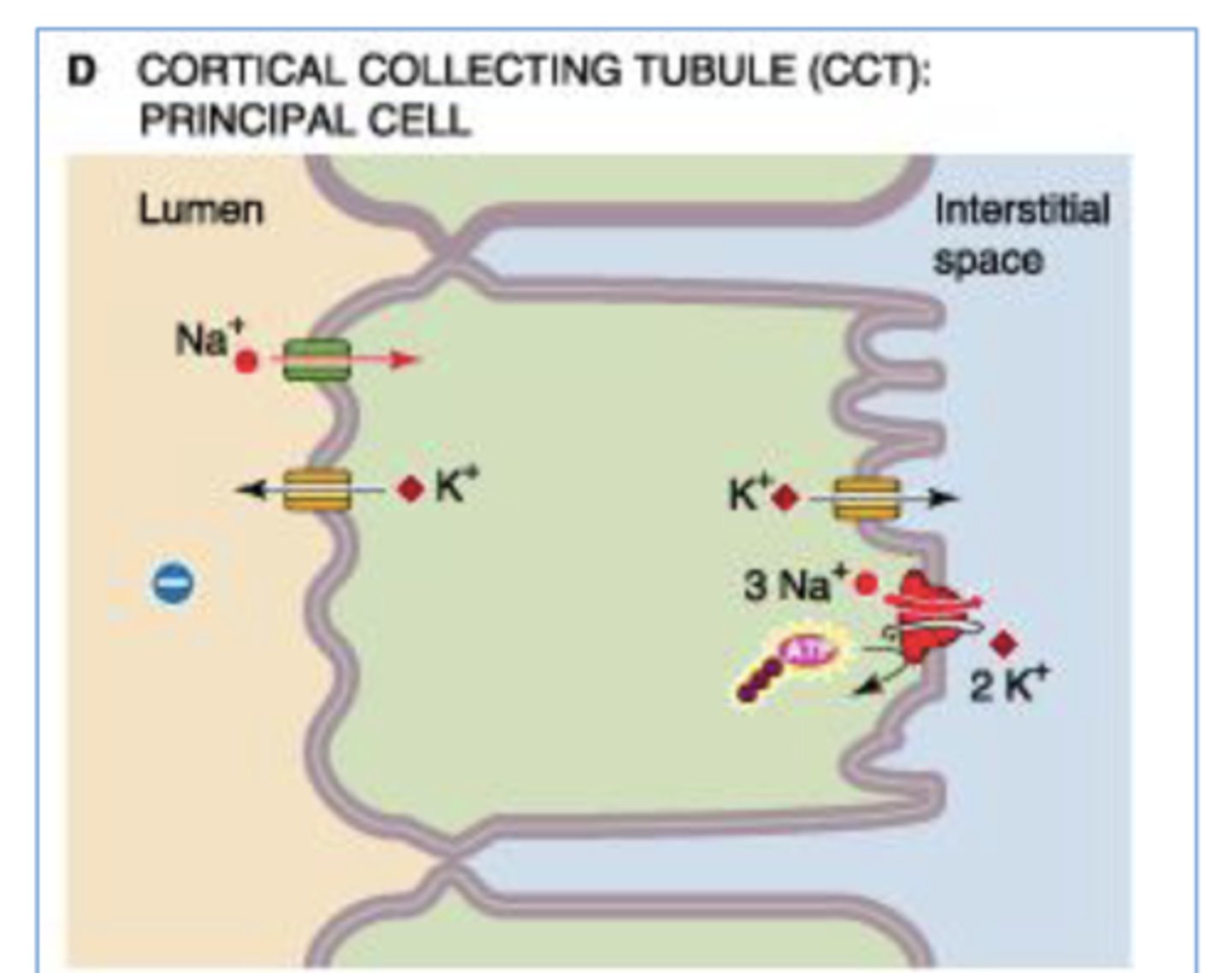
What determines how much K+ is secreted at the collecting duct?
the amount of Na+ introduced to ENa channels at collecting duct
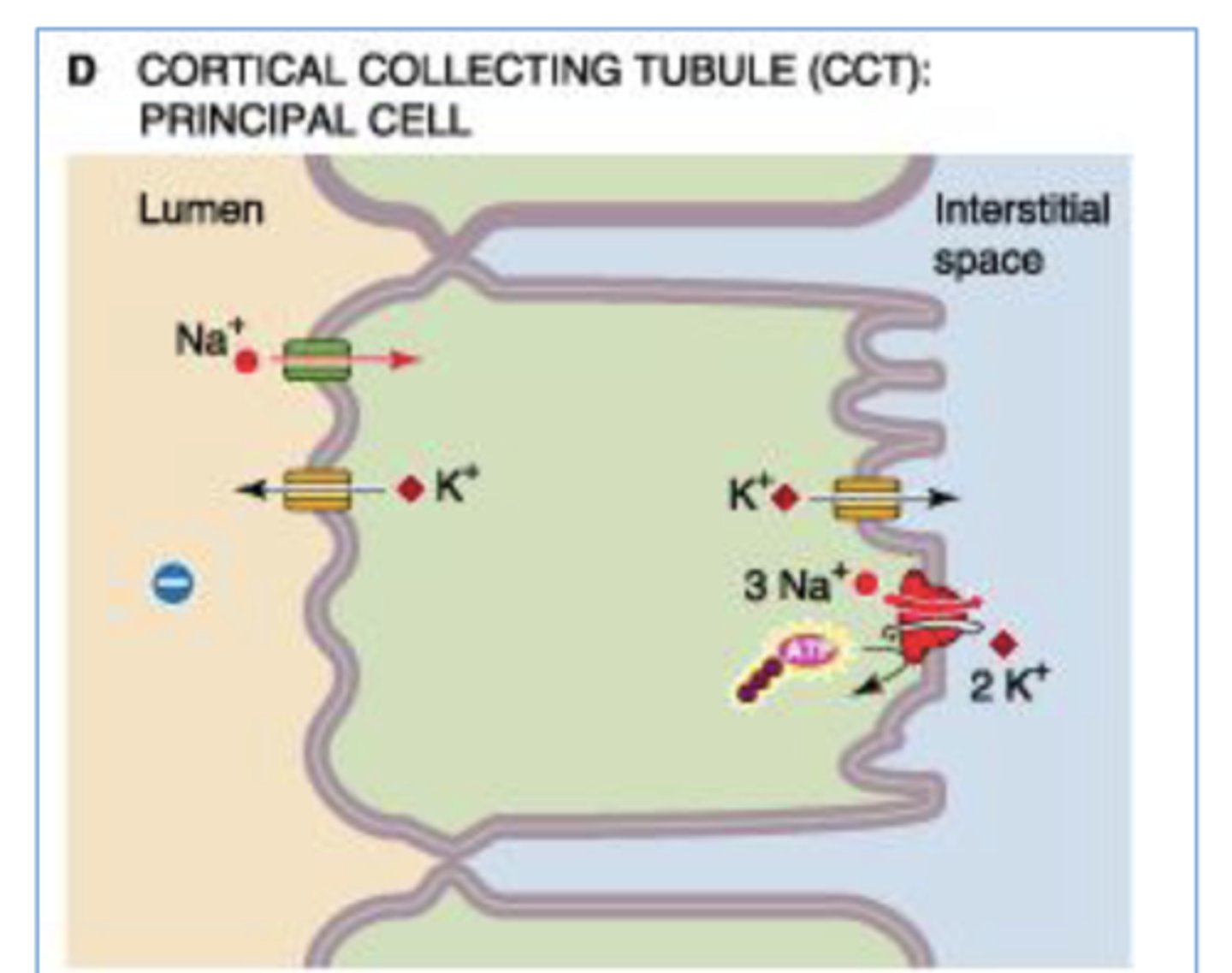
Amiloride
K+ sparing diuretic that blocks epithelial Na+ channels @ apical membrane of collecting duct
*mild diuretic b/c not much Na+ reabs happens in collecting duct (better use to prevent hypokalemia in combo w/ other diuretics)
True or False: Changing the levels of aldosterone or vassopressin/ADH may modulate the number of epithelial Na+ channels that are open in the apical membrane of cortical tubule principal cells
True
Which tubulary part of the nephron consumes the highest amount of ATP?
PCT ==> does the highest amount of transport/reabs via ATPase pumps at basolateral surface (transport from tubular cell to peritubular capillaries)
Why does renal oxygen consumption parallel with Na+ reabsorption?
all Na+ transport ultimately depends on the activity of ATP-driven Na+/K+ pump so it's dependent on generation of ATP b oxidative metabolism
* kidneys responsible for 7-10% of total O2 consumption
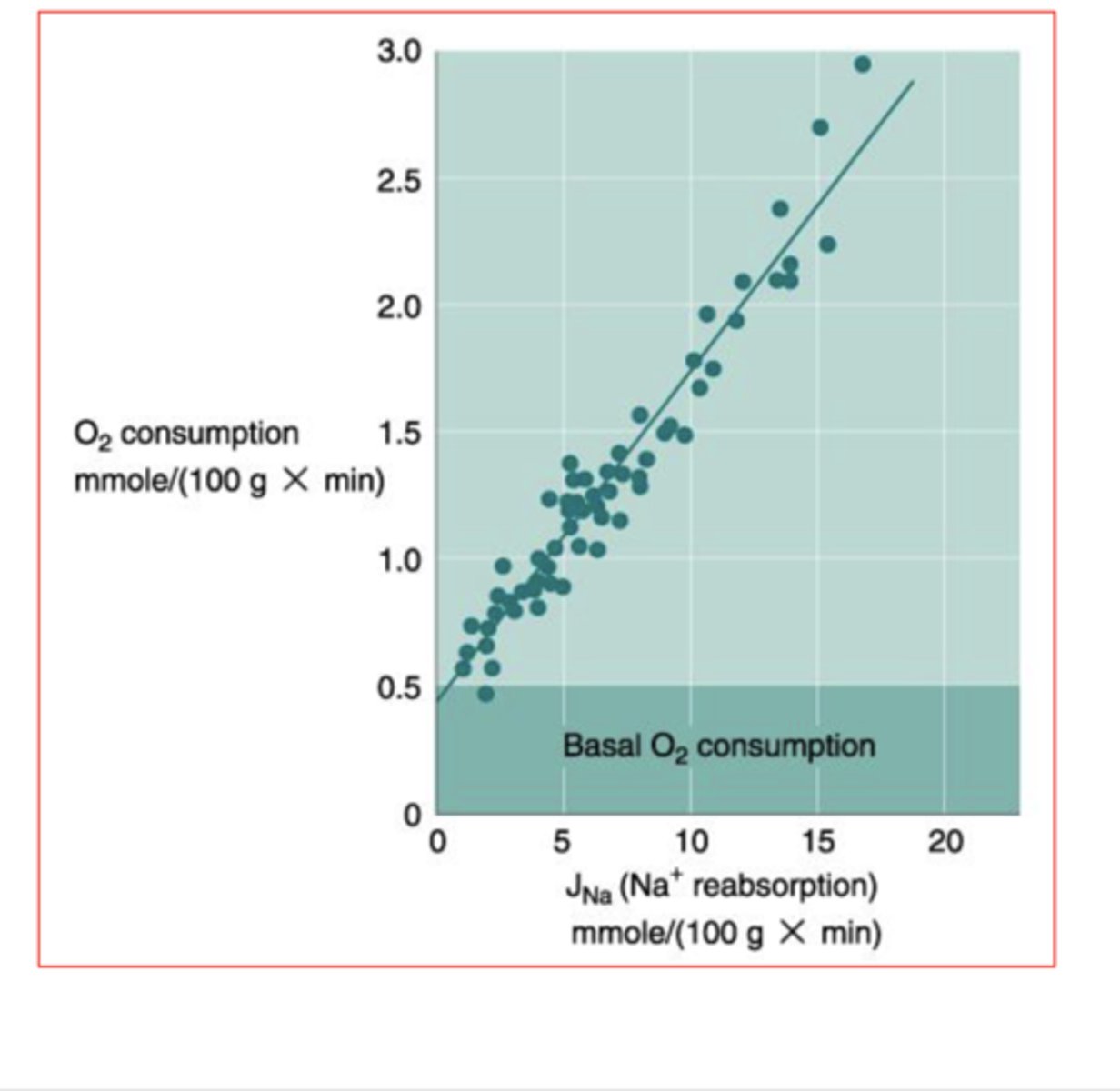
Kidneys are responsible for ___________% of total O2 consumption.
7-10%

Plasma Na+ is 140mEq/L and the filtered load is found to be 18mEq/min. The predicted Na+ remaining in the tubule at the end of the descending limb of loop of henle is which of the following?
6mEq/min
*descending limb of loop of henle is not permeable to Na+, so the conc Na+ in filtrate will be dependent on Na+ remaining in filtrate after passing thru PCT --> 67% of Na+ reabs in PCT --> approx 1/3 Na+ left behind
18 x (1/3) = 18/3 = 6
AQP1
water channels on the apical & basolateral membranes of PCT ==> reason PCT is permeable to water & can reabs water and Na+ in an isosmolar proportion
True or False: Na+ and water are reabsorbed in an isosmolar proportion at the proximal convoluted tubule
True ==> b/c PCT is permeabel to water so it's able to follow the Na+ that gets reabs
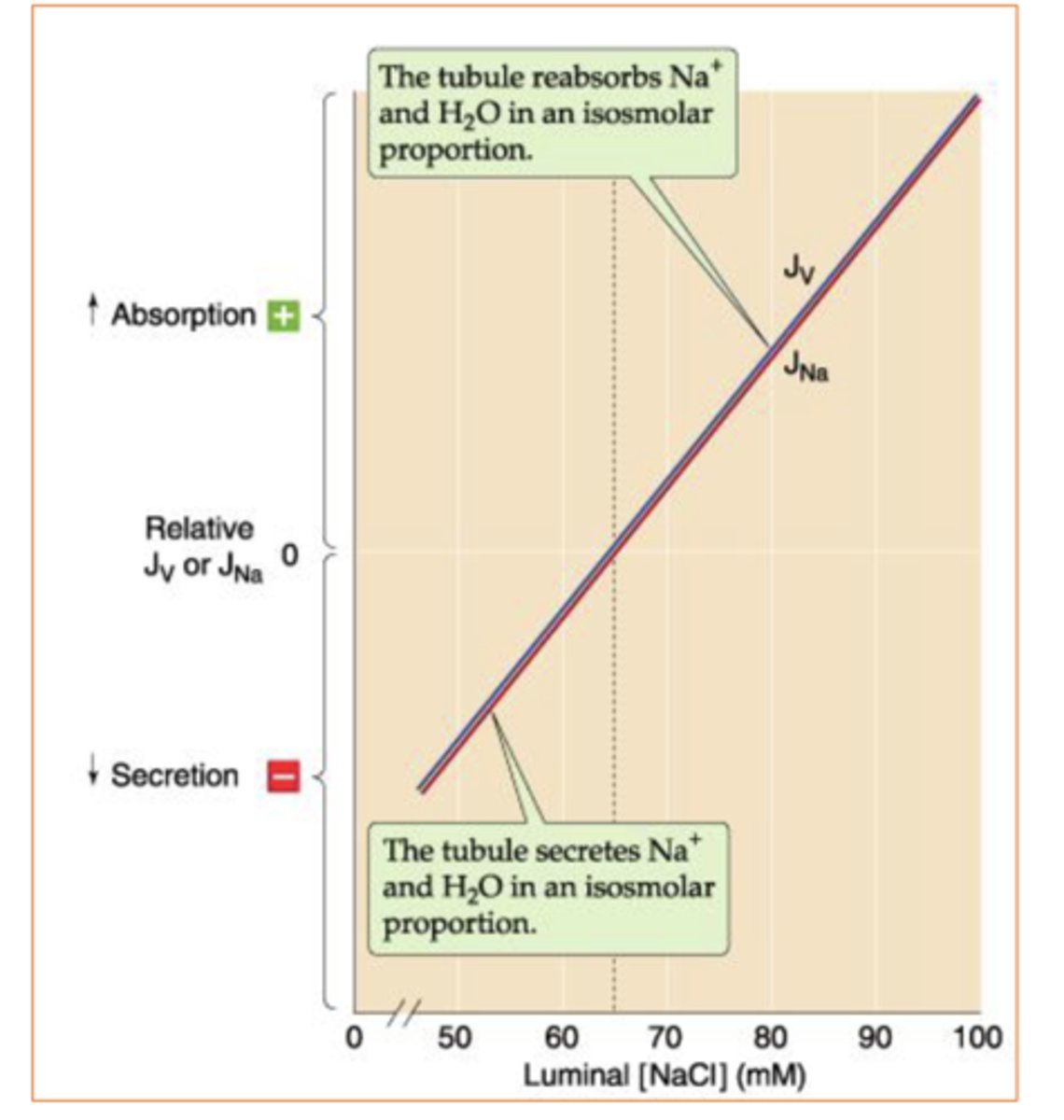
Normally luminal Na+ concentration does not change along the proximal tubule. What is the exception that causes luminal Na+ conc to change?
osmotic diuresis (when poorly permeable substances are present in the plasma --> glomerular filtrate) ==> attract water into lumen & dilutes solutes (including Na+ conc)
ex: -infusion of sucrose & mannitol
-untreated diabetes mellitus
True or False: The Thick Ascending Loop of Henle & all downstream segments have relatively low water permeability in the absence of arginine vassopressin/ADH.
True
The body regulates Na+ excretion via what 3 major mechanisms?
-glomerulotubular balance ==> fractional Na+ reabs; changes in renal hemodynamics alter the Na+ load presented to kidneys & modulate rate of Na+ reabs in PCT (modulate urine production based on body's blood volume & needs --> ex: decreased urine when hemorrhaging)
-Renin-Angiotensin, AVP/ADH, SNS stimulation ==> increase Na+ reabs
-Local Vasodilators==> ANP, prostaglandins, bradykinin, & dopamine decrease Na+ reabs
How is the volume of the extracellular fluid monitored?
detected via baroreceptors & stimulate system to increase or decrease fluid reabs.
-central vascular receptors (very important) --> cardiac atria & pulmonary vasculature
-high pressure (less important) --> carotid sinus, aortic arch, juxtaglomerular apparatus/renal afferent arteriole)
-sensors in CNS (less important)
-sensors in liver (less important)
Glomerulotubular Balance
major mechanism that regulates Na+ excretion==> when hemodynamic changes alter GFR & Na+ load presented to the nephron the PCT respond by reabsorbing a constant fraction of Na+ load
-excessive Na+ loss ==> contracts ECF vol --> decreased renal perfusion --> decreased GFR --> PCT excretes constant fraction of Na+ & water that's smaller to prevent additional Na+ & water loss
-excessive Na+ retention ==> expands ECF --> increase GFR --> PCT excretes a constant fraction of filtered Na+ that's bigger to correct volume expansion
How does glomerulotubular balance respond to excessive Na+ loss?
PCT excretes constant fraction of Na+ & water that's smaller to prevent additional Na+ & water loss
How does glomerulotubular balance respond to excessive Na+ retention?
PCT excretes a constant fraction of filtered Na+ that's bigger to correct volume expansion
Bartter Syndrome
set of autosomal recessive genetic diseases that cause inactivating mutations in gene coding for Na+/K+/2Cl- symporter in the thick ascending loop of henle ==> characterized by hypokalemia, metabolic alkalosis, & hyperaldosteronism
*mutated Na+/K+/2Cl- symporter in thick ascending loop --> decreases Na+, Cl-, K+ reabs --> decreases blood osmolarity & blood K+ conc --> decreased blood volume + hypokalemia--> increases aldosterone secretion = hyperaldosteronism --> increase Na+/H+ exchange in apical tubular cells of DCT & collecting duct -->increases Na+ reabs & H+ secretion (excretion) --> increases blood H+ --> metabolic alkalosis