epithelial tissue, connective tissue, cell junctions
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
define histology
the study of cells and tissue by microscopy (investigating structural differences of tissues)
what is the benefit of microscopy
allows us to zoom into structures and can even allow us to see individual organelles – gives us a lot of information
how do we prepare sample tissues for histology and explain this process
via sectioning
deciding how best to cut the sample tissue - can cut into different anatomical planes depending on the location of the structures we are interested in
why do we have to stain histological sections
to make them visible
different stain techniques used to create contrasts in order to see different structures clearly
define epithelial cells/tissue
layer or layers of cells that cover body surfaces or line body cavities
what are the 2 main subtypes of epithelium
1) covering and lining external and internal body surfaces (skin, organs, body cavities)
2) forms the secretory portion of glands (sweat glands and thyroid glands)
what are a few roles of the epithelium (6)
protection
secretion
absorption
filtration
excretion
sensory perception
explain how the different types of epithelium in the body relates to its structure
there are different types of epithelium in the body (in the lungs for gas exchange or in the oral cavity for protection)
the different types have slightly different structures to make it adapted for its particular function
state and explain the main features of epithelial cells (7)
cellular - (epithelial tissue)
good regeneration capacity - (under physical stress, so able to renew/repair/regenerate itself very quickly)
sits on basal lamina - (in close contact with the connective tissue)
avascular - (doesn’t have its own blood supply)
innervated - (very good nerve supply - especially in the epithelium in the skin)
tightly joined together
is polar - (has 2 distinct opposing sides - one is the apical (free) surface and one is the basal lamina)
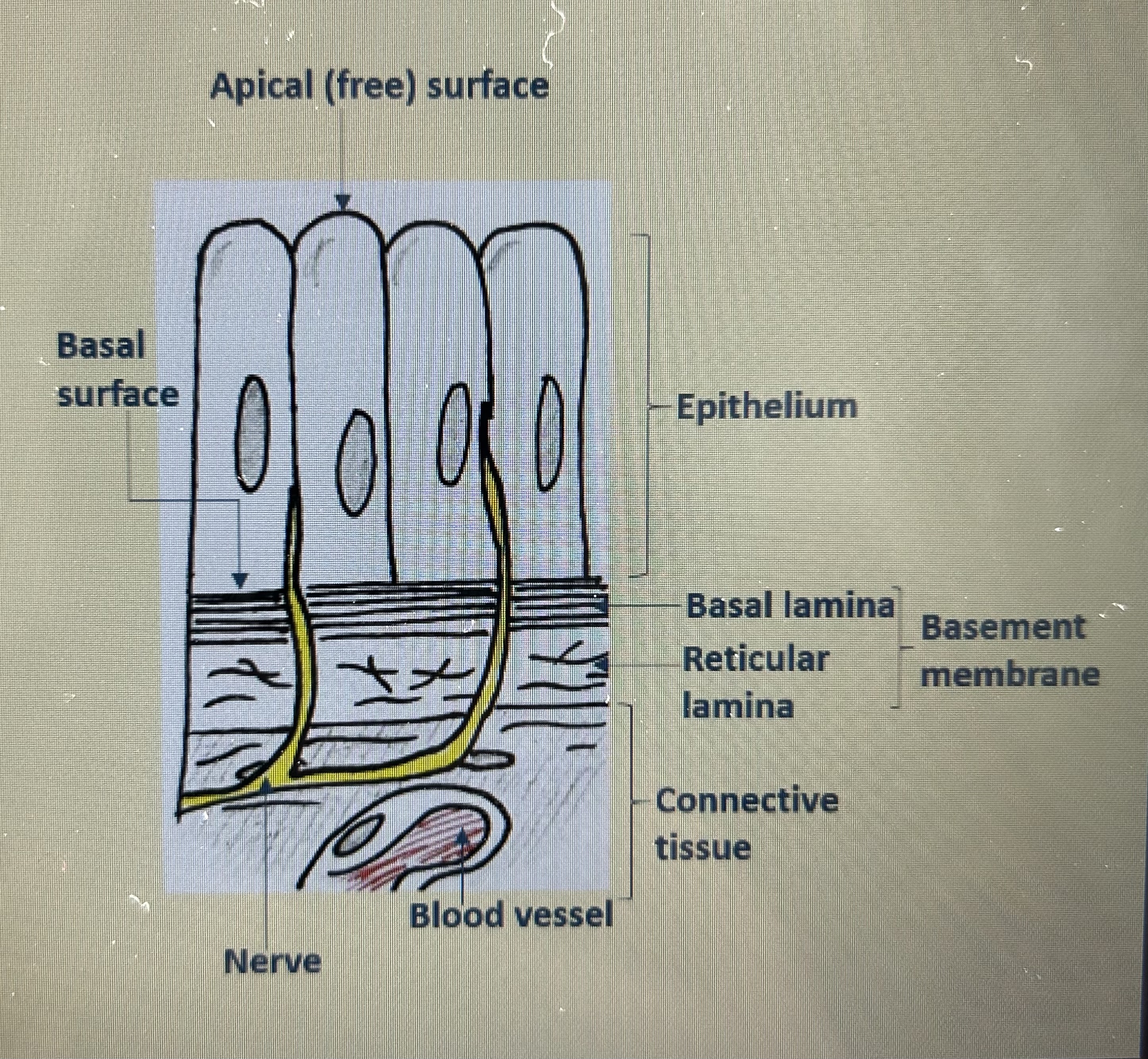
where does the epithelial get its nutrients from - as it is avascular
from the underlying connective tissue that it sits on
connective tissue is in close contact with blood vessels
blood vessels facilitate the diffusion of nutrients to the surrounding tissue which then diffuse to the epithelial cells
what are 3 ways we can categorize/classify the different epithelial cells
by arrangement/number of layers, shape, adaptations or not
explain number of layers in epithelial cells (3)
can be…
simple - a single layer
stratified - 2 or more layers
pseudostratified - a single layer, but looks like multiple layers as nuclei lie at different levels in the tissue and not all cells reach the apical surface
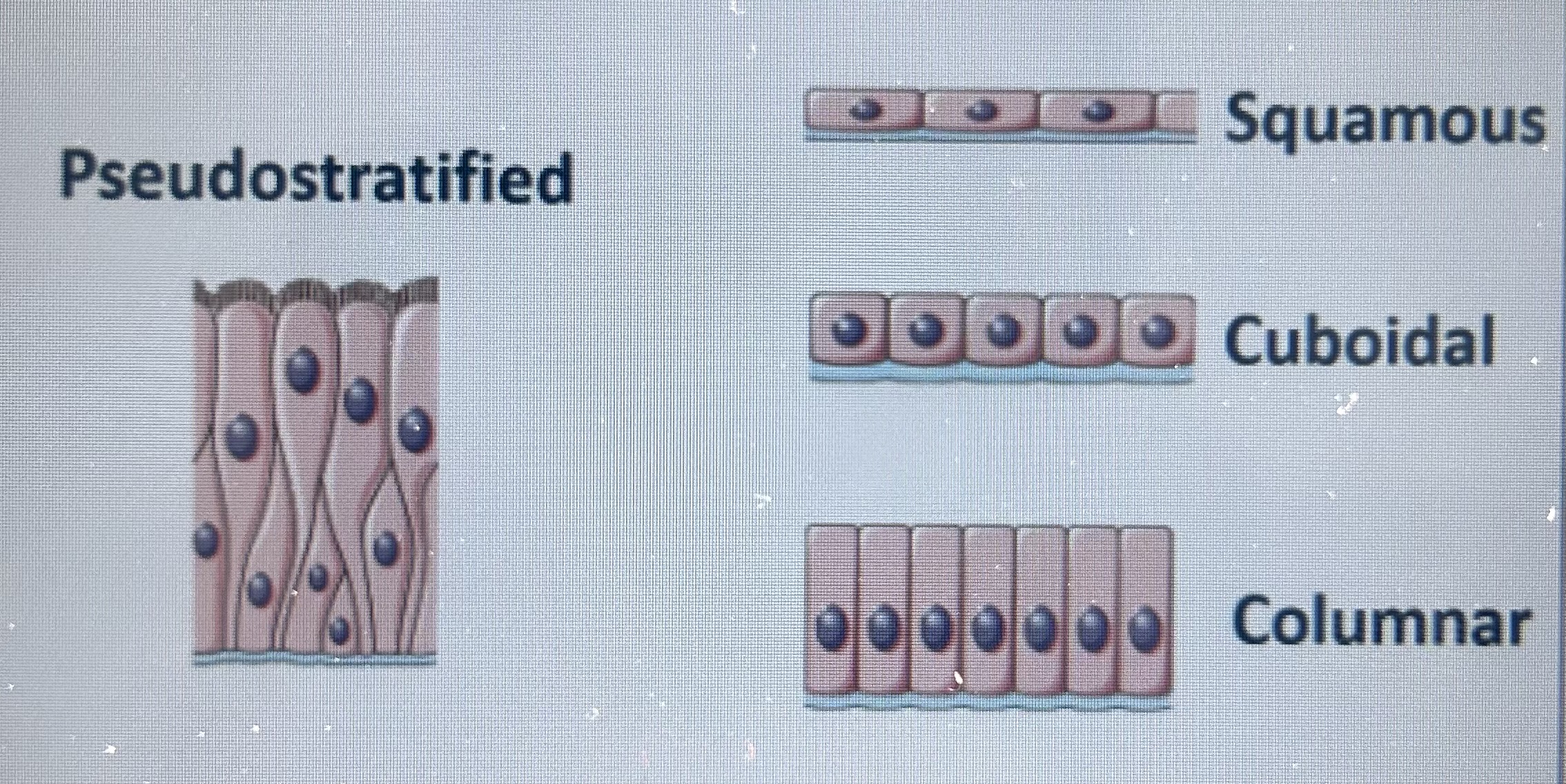
explain shape in epithelial cells
can be…
squamous - squashed, thin
cuboidal - same height and width all around - like a cube
columnar - much taller than they are wide - like a column
transitional - change shape from cuboidal to squamous and back, as tissues stretch and then collapse (in the bladder)
what are specializations of epithelial cells
adaptations that can exist in certain epithelial cells to help them function in a certain way
state and explain the 3 adaptations of epithelial cells
1 - microvilli - membranous finger like projections that increase the SA of plasma membranes for absorption
2 - cilia - tiny hair like structures, that are motile (move around) and sweep debris and mucus (on the apical surface)
3 - keratin - a protein that helps protect skin from heat, microbes and chemicals
define connective tissue
most abundantly and widely distributed tissue in the body
the space filing tissue
2 sub types of connective tissue
1) mature:
connective tissue proper (dense / loose)
cartilage
bone
blood
2) embryonic
what are the 2 parts that actually make up connective tissue
cellular
extracellular matrix
explain the cellular components that make up connective tissue (3)
fibroblasts - most abundant cell type, secrete fibers and ground substance (which makes up the extracellular matrix - link)
adipocytes
white blood cells - involved in immunity
explain the extracellular matrix that makes up connective tissue (2)
fibers:
collagen, elastic and reticular fibers
ground substance:
fluid or gel like, binds everything together (fills the space), component of connective tissue that lies between the cells and fibers
explain collagen fibers (4)
collagen is a protein - most abundant protein in body
very strong, but not stiff (flexible)
produced mainly by fibroblasts (and released by it)
different types of collagen: 10 different subtypes, 8 different types of collagen found in the eye
what determines the different types of collagen
change in order / sequence of amino acids which changes structural properties slightly
explain what the ground substance of the extracellular matrix is (4)
a combination of…
water
glycosaminoglycans (GAGs) - long linear polysaccharides chains - traps water (skincare hyaluronic acid)
proteoglycans - proteins that has a carb attached to it
adhesion proteins (fibronectin) - promote stickiness and adhesion
explain the difference in loose and dense connective tissue (in terms of appearance, what types of structure they make up)
loose - lots of gaps, not a lot of extracellular matrix / in structures that are elasticated, flexible and that expand and collapse easily
dense - packed together neatly, more organized structure / aorta to withstand high blood pressure
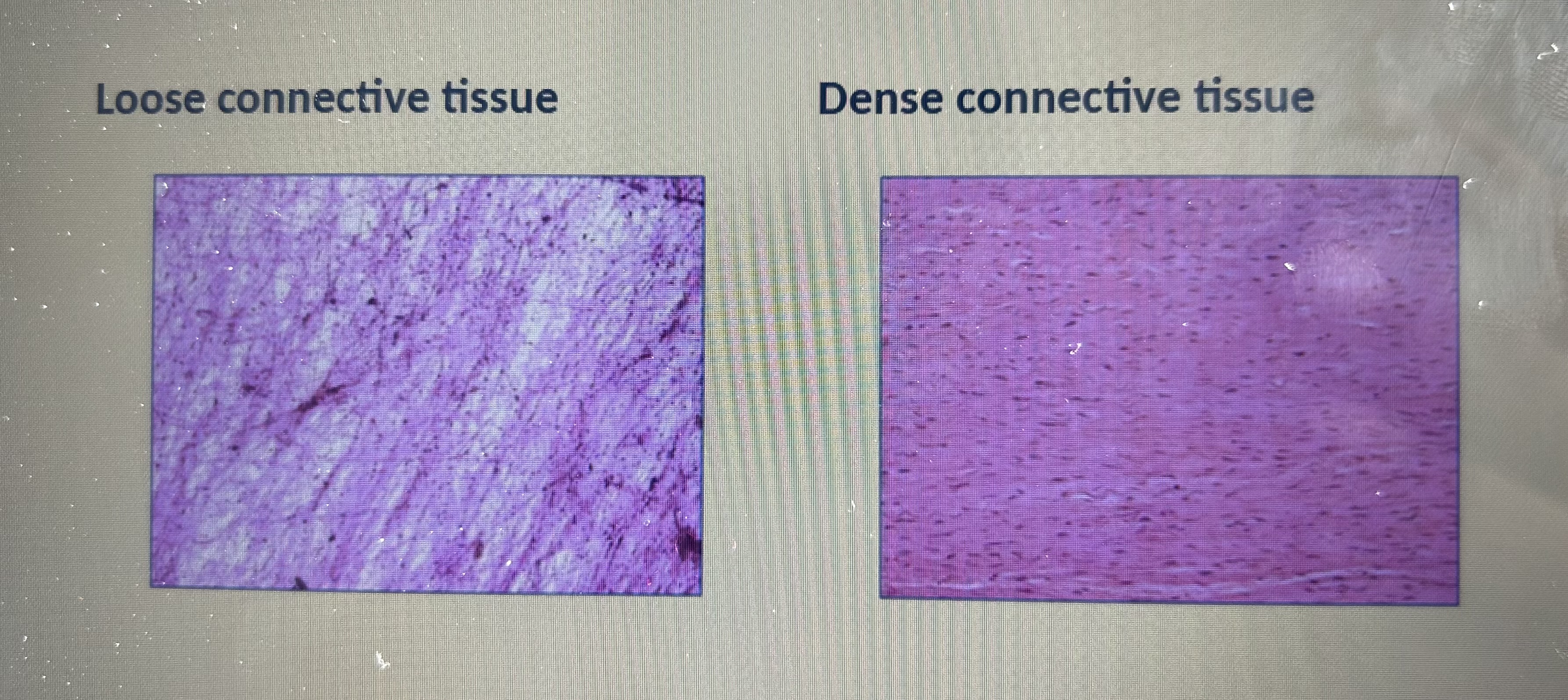
how do we have loose and dense tissue if they are made up of the same thing
due to the proportions of different structures it contains - which gives it different properties
eg: loose has less collagen and less cells whereas dense has more collagen and cells
what is the role of cell junctions (exist mainly in epithelial cells) (3)
help neighboring cells adhere to each other (the plasma membranes of adjacent cells are joined together)
allow adjacent cells to communicate with each other - efficient transfer of substances in the tissue
aid or inhibit the movement of substances between or past cells
what are the 3 types of cell junctions
1 - tight junctions
2 - desmosomes
3 - gap junctions
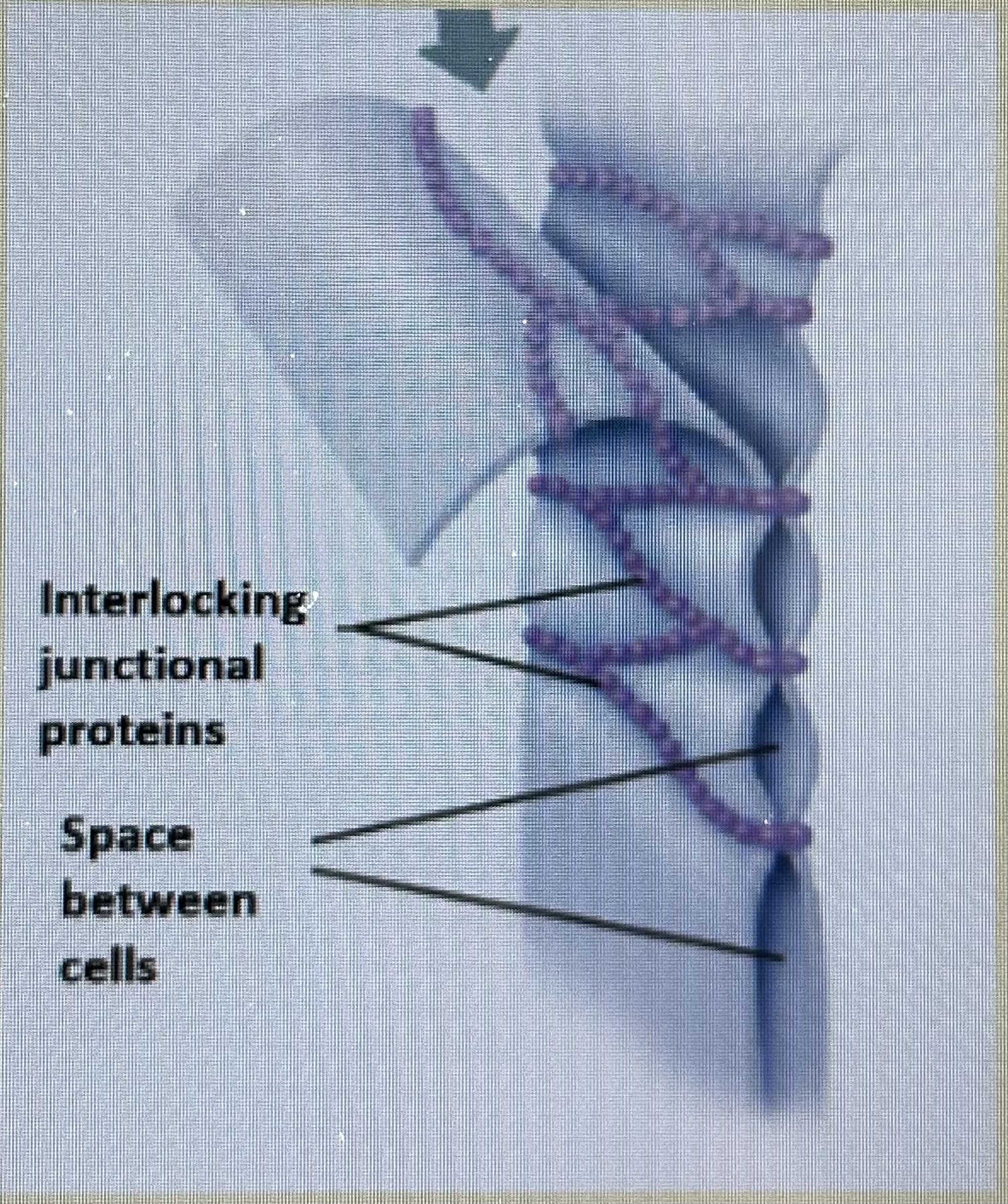
explain tight junctions and their function
water tight seal
(formed by special) integral membrane proteins from neighboring cells that fuse together - like a zip
this forms an impermeable junction / continuous seals around the cell
TJ helps prevent molecules from passing through the extracellular space between cells
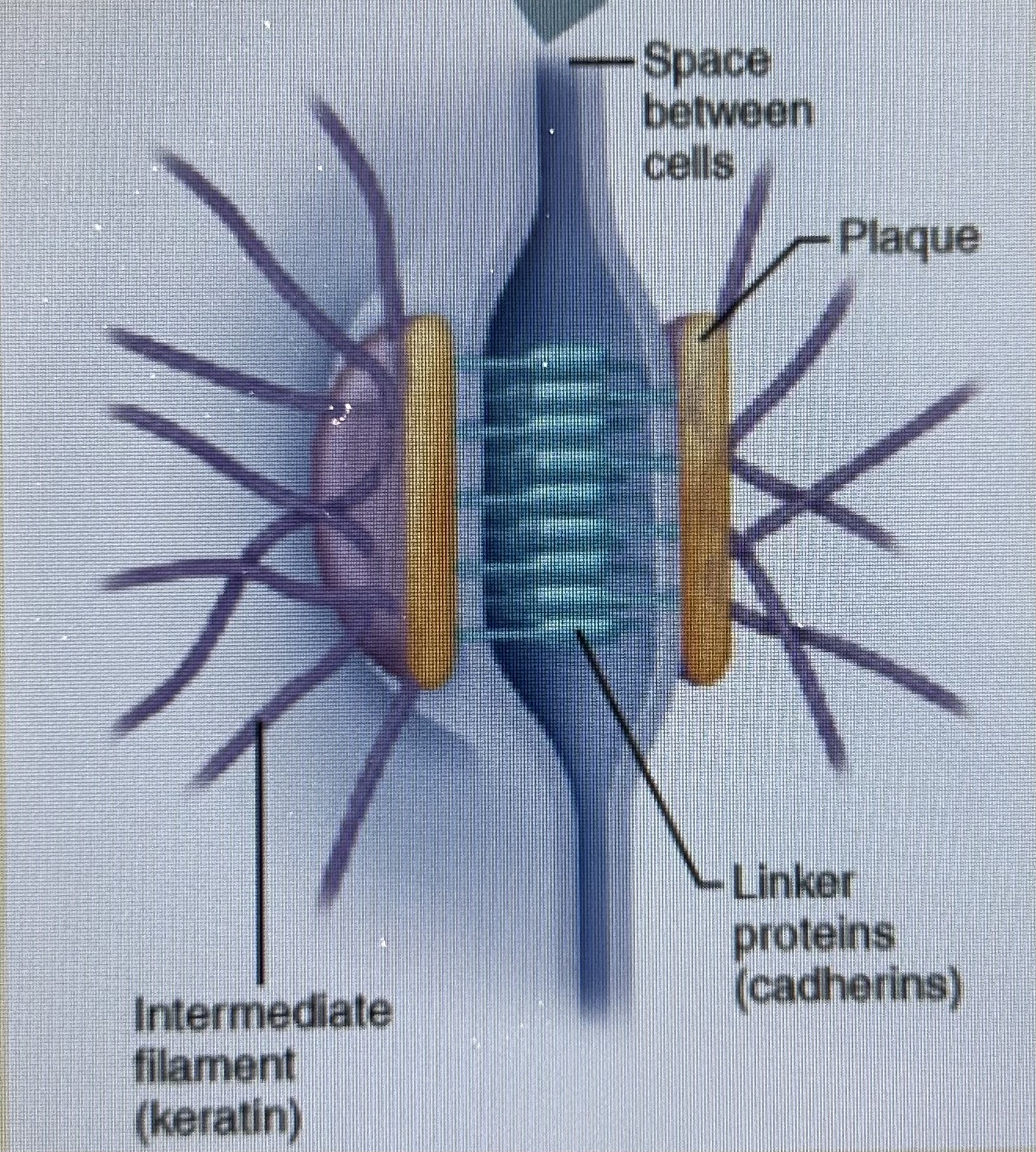
explain desmosomes and their function
spot wells
the anchoring junctions
prevent adjacent cells from separating from each other / bind adjacent cells to each other / maintain its integrity and structure
found in abundance in tissue exposed to mechanical stress (muscle tissue) - helps prevent cellular layers from tearing apart under mechanical stress
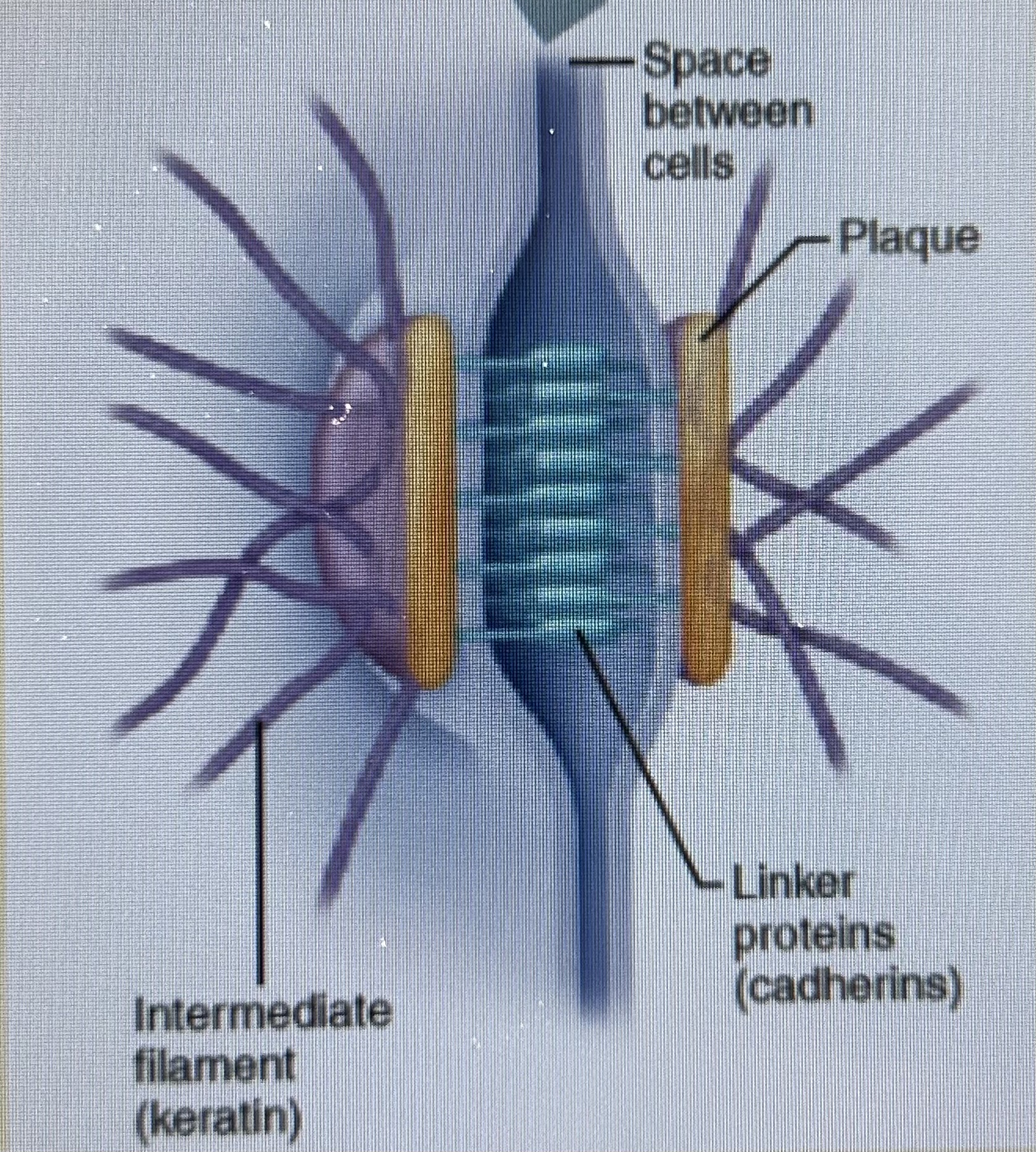
explain what the mechanism of attachment involves (2)
plaque - a small area of thickened plasma membrane on the cytosolic (inside of cell) side of the bilayer
linker proteins (cadherins) - extend out from the plaque and fit together with the linker protein of the adjacent cell (like a molecular velcro)
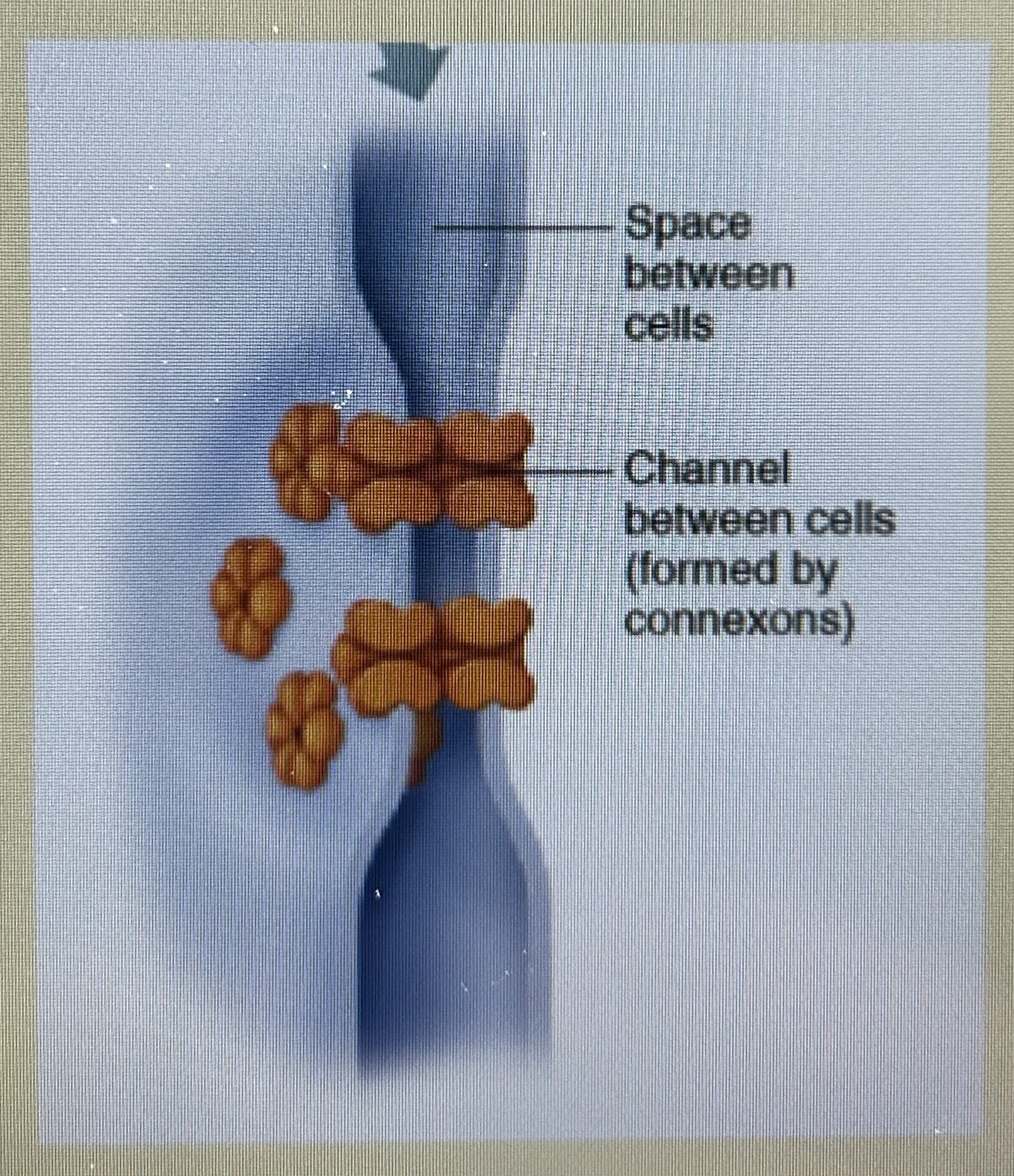
explain the function of the gap junction
tunnel
the communicating junction/permeable - allows adjacent cells to share material and and communicate with each other
adjacent plasma membranes come into close contact - not direct contact via a mechanism
found in abundance in electrically excitable tissues - ones that spread APs
explain the mechanism that allows adjacent plasma membranes to come into close contact (GJs)
hollow channels (connexins) from both plasma membranes connect with each other
connexins are composed of integral proteins - depending on type it will be different integral proteins that make it up