ANXIETY DISORDERS AND OCD (ch 6)
1/46
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
anxiety disorders
specific phobias
social phobia
panic disorder and agoraphobia
generalized anxiety disorder
OCD and OCD related disorders
fear vs anxiety
fear = a normal, immediate reaction to an environmental stimulus
rxn to real, experienced danger
intensity builds quickly
helps behav responses to threats
anxiety = not as immediate, more of a period of that feeling. can be irrational or unprovoked
anticipation of future problems
general / diffuse emotional reactions
emotional experience is disproportionate to the threat
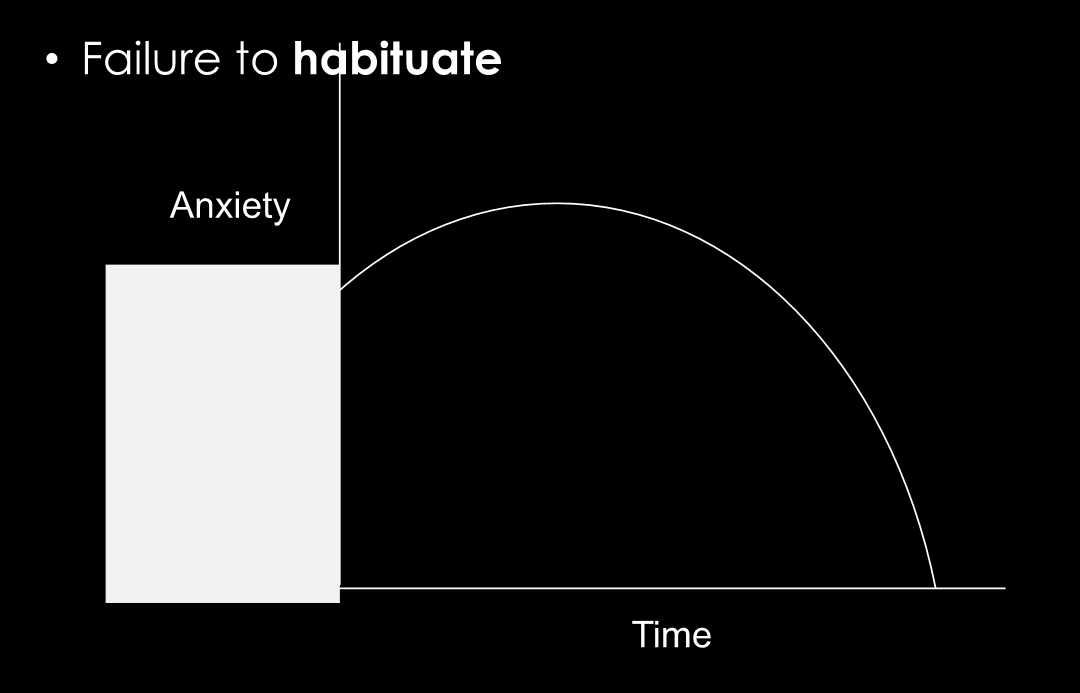
commonality across all anxiety disorders?
failure to habituate: anxious feelings dont go away, person does not get used to situation. anxiety levels stay high even after much time has passed
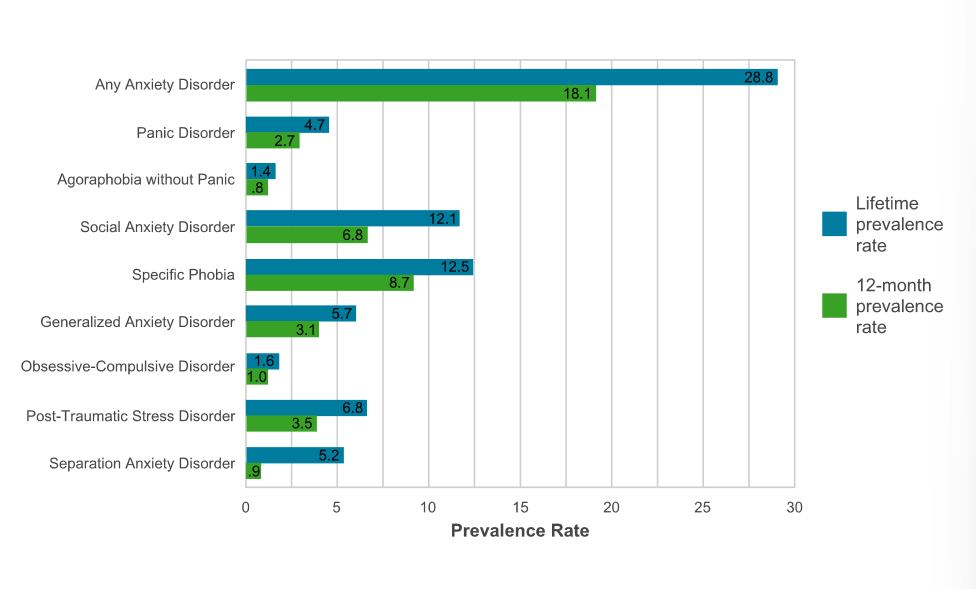
lifetime prevalence of anxiety disorders
any anxiety disorder = 28.8% lifetime prevalence
most common disorders = social anxiety and specific phobia
social factors - anxiety disorders
stressful life events
involving danger, deprivation of resources, insecurity, family, discord
in contrast, depression stressful life events involve LOSS
childhood adversity
abuse, neglect
exposed to more anxiety in parents
caregivers who are more anxious more likely to have kids that are more anxious (not necessarily genetics — behavior modeling)
biological factors — anxiety disorders
genetics: nonspecific for mood and anxiety disorders
cant find lots of specifics. lots of comorbid btwn mood and anxiety disorders
behavioral inhibition temperament
person has a more inhibited temperament
again, not v specific to anxiety
the amygdala — anxiety disorders
amygdala = fear and emotions
increased amygdala activity associated w increased anxiety reaction, especially w specific phobia

the insula — anxiety disorders
connected to autonomic nervous system
critical for interoception: how we interpret our bodily sensations (bodily perception) — some ppl more sensitive/intuitive of these than others
increased activity of this brain region in anxiety
phobia
Persistent, irrational, narrowly defined fears that are associated with a specific object or situation
Characterized by avoidance and reactions that are irrational and unreasonable to the situation/object
types of phobia disorders
specific phobia
social phobia
agoraphobia (**considered under panic disorder bc highly linked)
specific phobia DSM-5 criteria:
marked and persistent fear that is excessive or unreasonable cued by the presence of anticipation of a specific object or situation
exposure tho the phobic stimulus = immediate anxiety response (possible panic attack)
phobic situation is avoided (or endured w intense anxiety and distress)
fear, anxiety, or avoidance is persistent, typically lasts 6 months or more
*avoidance or distress interferes significantly w the persons routine, occupational functioning, or social activities
DSM-5 specific phobia subtypes
animal
natural environment
blood-injection-injury
situational
other
specific phobia epidemiology
very common
lifetime prevalence = 12%
3x more common in women than in men
blood-injection-injury phobia occurs in ab 3-4% of pop
age of onset varies widely typically bc there is some triggering event
etiology of phobias (risk factors)
evolutionary adaptation: phobias may have been adaptive at some point in human history/development
classical conditioning: phobia may be a result of repeated pairing of stimulus
preparedness theory of phobias:
we are biologically prepared for associations / anxious responses
prepared associations learned in one trial and are very difficult to extinguish.
easy to condition fear to fearful objects (snakes, spiders, etc), but more difficult to condition neutral objects.
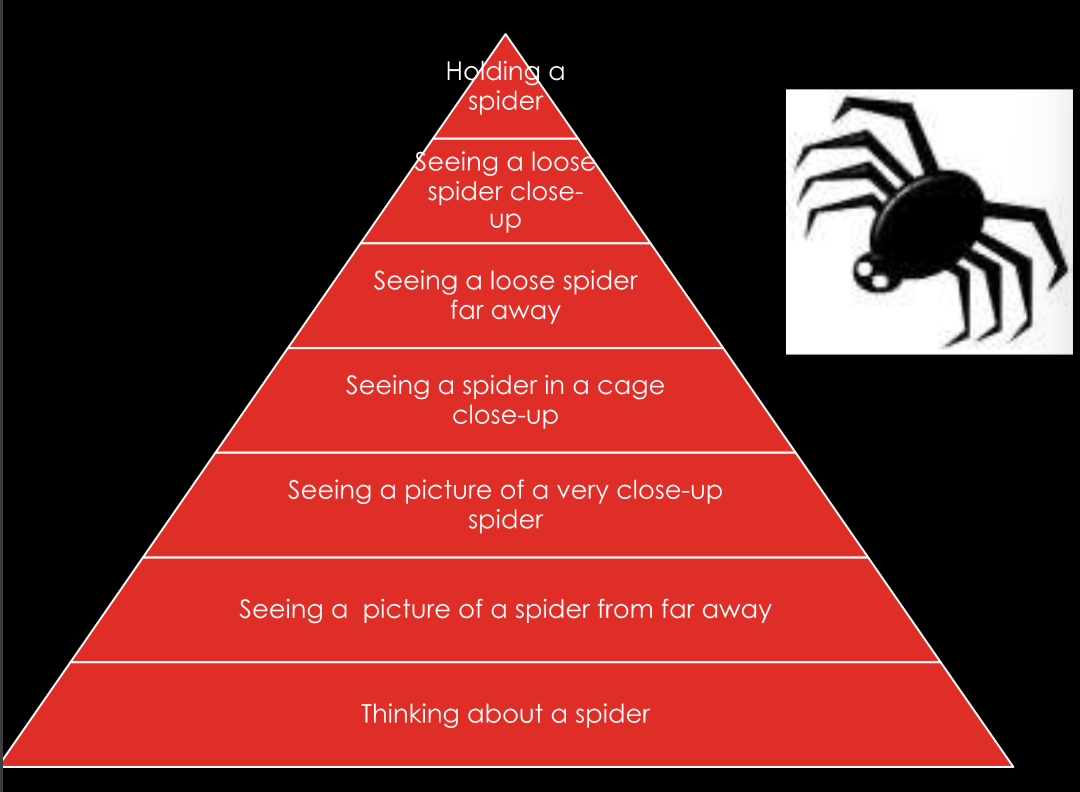
phobia treatments
exposure therapy
may be paired w SSRI or something for the anxiety
many different forms, but often in a fear hierarchy
imagination, observation, virtual reality, viewing, touching, experiencing, etc
Social anxiety disorder (SAD)
level of fear of social situations that leads to impairment
in education, employment, family relationships, marriage/romantic relationships, and friendships
DSM-5 criteria:
marked and persistent fear of one or more social or performance situations
fear of being scrutinized or embarrassing oneself
feared situations are avoided or endured with great distress
fears significantly interfere with funcitoning
subtypes of social anxiety disorder
specific: 1-3 feared situations
most common form is fear of public speaking
ex: eating in public, performing in public, etc
generalized: 4+ feared situations
ex: eating in public, using bathroom, parties, maintaining conversations, meeting strangers, etc
prevalence of Social anxiety disorder
lifetime: 12.1%
12 month prevalence: 6.8%
rates higher in women (15.5%) than men (11%)
early age of onset: childhood to mid-adolescence
high comorbidity w other anxiety disorders, and depression
etiology (risk factors) of Social anxiety disorder
genetic risk:
tendency toward high negative affect or low positive affect (—or—) low extraversion and high neuroticism levels
environmental risk factors:
bullying in childhood — directionality unknown
childhood neglect / abuse
parenting style: maternal overprotection
Cognitive behavioral theory of Social Anxiety Disorder (Rapee and Heimberg)
thoughts = “i’m not good enough”
feelings = sadness and loneliness
behaviors = avoidance of social situations
beliefs: negative self-evaluation; being liked is fundamentally important
behaviors of hyper-vigilance
hyper-vigilance in social anxiety disorder
heightened attention to signs of social threat / cues in the social environment
hyperaware
eye-tracking studies show that ppl w generalized social anxiety disorder are constantly scanning ppls faces a lot more than others
treatment — social anxiety disorder
medication:
SSRI often prescribed need a constant treatment for the anxiety
sometimes benzodiazepines
psychotherapy:
group or individual CBT is most supported
attention bias retraining
cognitive behavioral therapy:
cognitive restructuring
social exposures
fear hierarchy
work up towards higher feared situations
panic attack symptoms
**note: symptoms must peak in 10 minutes
palpitations
sweating
trembling or shaking
sensations of shortness of breath
feeling of choking
chest pain
nausea
dizziness
derealization
fear of losing control
numbness
fear of dying
chills / flushes
relationship between panic attack and panic disorder
first attack frequently follows distress of highly stressful life circumstances
many adults who experience a single panic attack do not develop a panic disorder
20% of college students have attack, but don’t develop disorder
how you respond to the initial attack dictates whether or not one develops the disorder
DSM-5 criteria for panic disorder
recurrent, unexpected panic attacks
sudden, overwhelming experience of terror or fright
more focused than anxiety
“false alarm”
common in other anxiety disorders too
at least one panic attack followed by 1 month (or more) of 1 (or more) of the following
persistent concern about having another attack
worry about the implications of the attack
significant change in behavior related to the attacks
DSM-5 criteria for agoraphobia — highly linked to panic disorder
anxiety about being in situations from which escape might be difficult or in which help might not be available if panic like symptoms develop
hallmark feature: these situations are avoided or else endured with distress
80-90% of diagnoses are female
range of severity associated w disorder
prevalence and course of panic disorders
lifetime prevalence = 3.5% of adult pop
twice as prevalent in females
chronic: 50% recover in 12 years
average age of onset = 23-24 years old
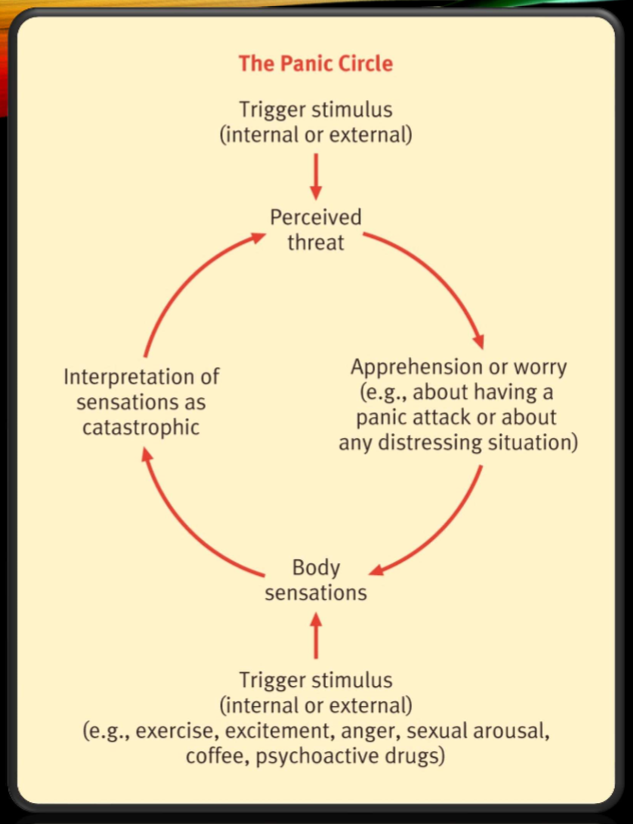
catastrophic misinterpretation — cognitive factors in panic disorder
panic attacks are triggered by internal stimuli
anxious mood leads to physiological sensations
narrowed attention and increased awareness of bodily sensations
person misinterprets bodily sensations as catastrophic event
“fear of fear”
the panic circle — cognitive factors in panic disorder
trigger stimulus → perceived threat → worry → bodily sensations → interpretation of sensations as catastrophic → go thru circle again
panic disorder treatment
85% of ppl w panic disorders show up repeatedly at emergency rooms
interoceptive exposure therapy: helps u revisit those feared internal stimuli that u experience in a panic attack —- (exposure to feared bodily sensations associated w panic)
cognitive therapy: target catastrophic automatic thoughts
psychoeducation
with treatment, 70-90% recover
** benzodiazepines make relapse more frequent :(
General anxiety disorder DSM-5 criteria
excessive anxiety and worry (apprehensive expectation) occurring more-days-than-not for at least 6 months, about a number of events or activities
person finds it difficult to control the worry
the anxiety and worry are associated with 3 or more of the following 6 symptoms (with at least some symptoms present for more-days-than-not for the past 6 months)
restlessness or feeling keyed up / on edge
being easily fatigued
difficulty concentrating or mind going blank
irritability
muscle tension
sleep disturbance (difficulty falling or staying asleep, or restless unsatisfying sleep)
causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
GAD vs MDD — differential diagnosis
must have evidence that GAD exists outside of depressed episodes
differential must be made, bc these two disorders are highly comorbid
GAD-specific symptoms (vs MDD)
worry
cognitive biases
intolerance of uncertainty (difficulty w ambiguous and uncertain possiblilities)
GABA / benzodiazepine receptor dysfunction
worry vs GAD
worry:
uncontrollable
negative emotional thoughts
concerned with possible future threats or dangers
usually verbal rather than visually expressed
when it becomes GAD:
frequency
control
range of topics
valence (how extreme it is)
prevalence and comorbidity of GAD
lifetime prevalence = 5.7%
age of onset: 31-33
GAD and MDD correlate 0.59-0.70 ——> high correlation
Tri-Partite model of mood and anxiety disorders
relates mood and anxiety disorders to broad underlying traits of positive and negative affect as well as autonomic arousal
negative affect (mood and anxiety)
positive affect (MDD only)
physiological hyper-arousal (anxiety specific)
GAD etiology:
cognitive = “intolerance of uncertainty”
difficulty with ambiguous and uncertain possibilities
biological:
GABA / benzodiazepine receptor dysfunction
treatments for GAD
medications:
SSRIs
benzodiazepines — effective but rarely prescribed bc side effects and addictiveness
CBT: new treatments that target avoidance of emotion:
self-monitoring
interpersonal and emotional processing therapy
antecedent cognitive reappraisal
target cognitive biases (overestimate likelihood of negative events and underestimate ability to cope)
mindfulness-based CBT for GAD
emotion regulation therapy
emotional awareness training — prevention of emotional avoidance
staying in present moment, stop behavioral avoidance, engage w emotions as they come
DSM-5 criteria for obsessions (OCD)
recurrent and persistent thoughts, impulses, and images
experienced as intrusive, inappropriate, unwanted
case marked anxiety or distress (& impairment)
thoughts r not simple excessive worries ab real life problems
person attempts to ignore / suppress thoughts
person recognizes that the thoughts are a product of his or her own mind (not imposed from the outside)
DSM-5 criteria for compulsions (OCD)
repetitive behaviors or mental acts that the person feels driven to perform
in response to an obsession, or according to rules that must be applied rigidly
behavs aimed at preventing or reducing distress, or preventing some dreaded event or situation
behavs not connected in a realistic way w what they are designed to prevent, or are clearly excessive
examples of obsessions and compulsions
obsessions:
contamination fears
fear of harming oneself or others
lack of symmetry
pathological doubt
compulsions:
cleaning
checking
repeating
ordering / arranging
counting
DSM-5 definition of OCD
presence of obsessions, compulsions, or both
person recognizes that obsessions or compulsions are excessive or unreasonable
cause marked distress, are time consuming (More than 1 hour per day), or interfere w persons functioning
OCD epidemiology
lifetime prevalence = 2.3%
affects both genders about equally
age of onset: adolescence or early adulthood
OCD etiology (causes / risk factors)
psychological — learned behavior:
avoidance learning: neutral stimuli associated w frightening thoughts or experiences through classical conditioning
once association is made, person may find anxiety is reduced w compulsive behavior —> association btwn compulsive behav and reduced anxiety
difficult to extinguish these responses
cognitive — thought suppression:
thought suppression: if u tell someone to not think ab something, they will only think ab it more — for OCD, this happens w their intrusive thoughts. if try to suppress, think ab twice as frequently
genetics:
moderate heritability
nonspecific neurotic predisposition (general heritability of a neurotic temperament)
biologically based variant of OCD = PANDAS
some forms have chronic motor tics
related to Tourette’s Syndrome
23% of individuals w Tourette’s have OCD
seems to be related to specific molecular genetic variants
treatment of OCD
exposure and response prevention: expose individual to upsetting stimuli and prevent their typical response (expose to obsessions —> prevent compulsions or anxiety)
goal: to sever the link btwn obsessions and compulsions
anxiety will habituate — let the individual sit w anxiety until they get used to it
50-70% show a positive response. 76% maintain these gains after treatment
SSRIs:
40-60% show reduction of 25-35% of symptoms
high relapse rates
beneficial but not as effective as exposure and response prevention
cross-cultural comparisons of anxiety disorders
Yoruba (Nigeria): GAD presentation is different; creating and maintaining a family, fertility, importance of dreams (bewitched)
Koro (China & Southeast Asia): intense, acute fear that the penis is retracting into the body and death will result
Also occurs in women with response to nipples
Attributed to contaminated food
Variant of shrinking in West Africa - fertility problems not death concerns
Taijin Kyofusho (Japan): fear of interpersonal relationships (similar to social phobia; but moreso a fear of offending others), but no fear of criticism
Prevention of anxiety disorders
build ability to control situations that might lead to anxiety
education ab dangerous vs nondangerous situations
change negative thoughts
practicing skills in real life situations