A+P II Chp 25 (pt 1): Urinary System
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
What are 4 urinary system organs?
1) kidneys
2) urinary bladder
3) paired ureters
4) urethra
What do the kidneys do?
form urine
What is the function of the urinary bladder?
stores urine temporarily
What do the paired ureters do?
transport urine from kidneys to bladder
What does the urethra do?
transports urine from the bladder out of the body
For the kidney,
a) is it retroperitoneal or intraperitoneal
b) what region is it located in
c) which kidney is lower
d) what 2 surfaces does it have
a) retroperitoneal
b) superior lumbar region
c) right kidney
d) convex lateral surface, concave medial surface
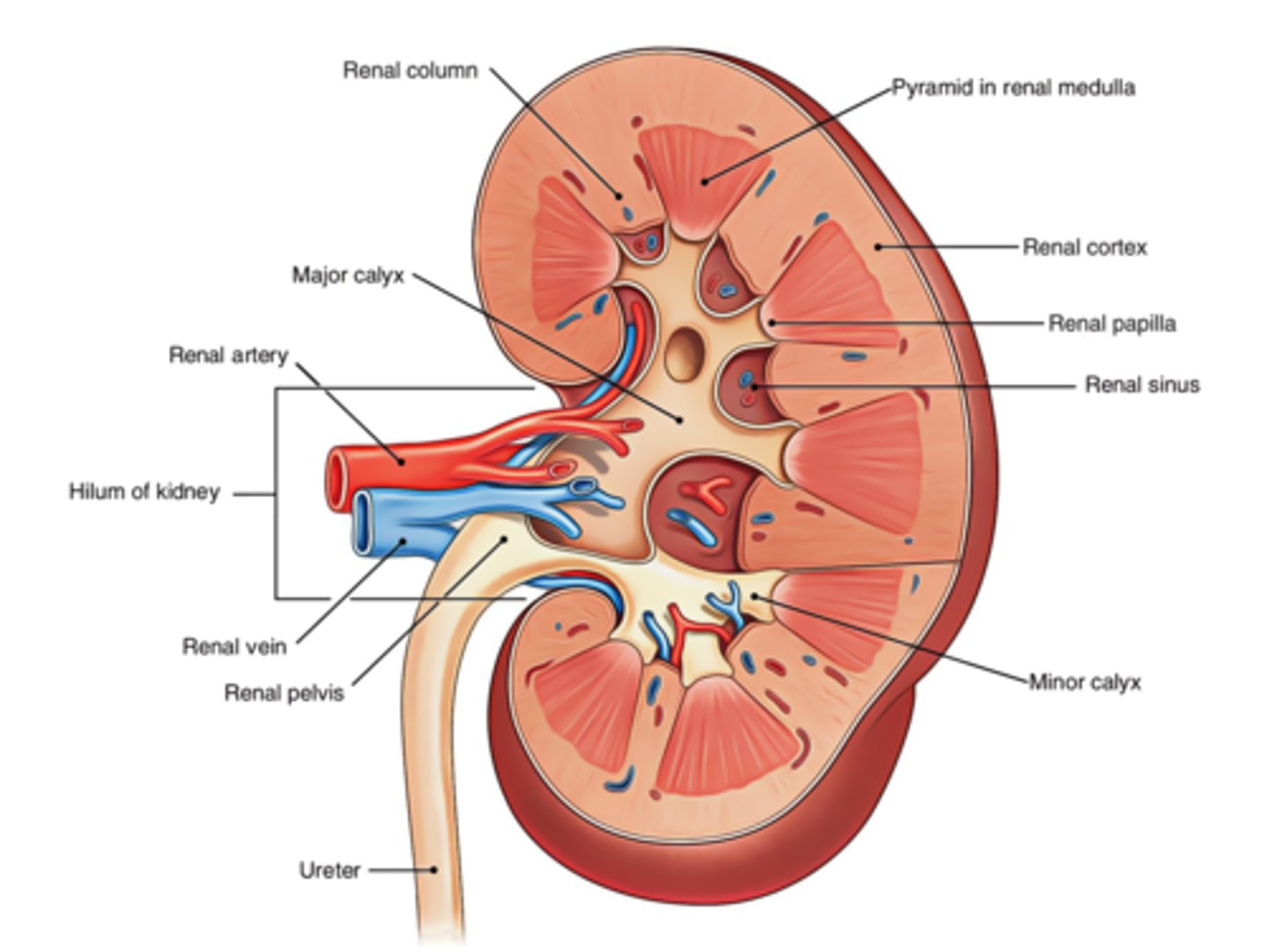
What is the renal hilum?
- leads to renal sinus
- where ureters, blood vessels, lymphatics, and nerves enter/exit
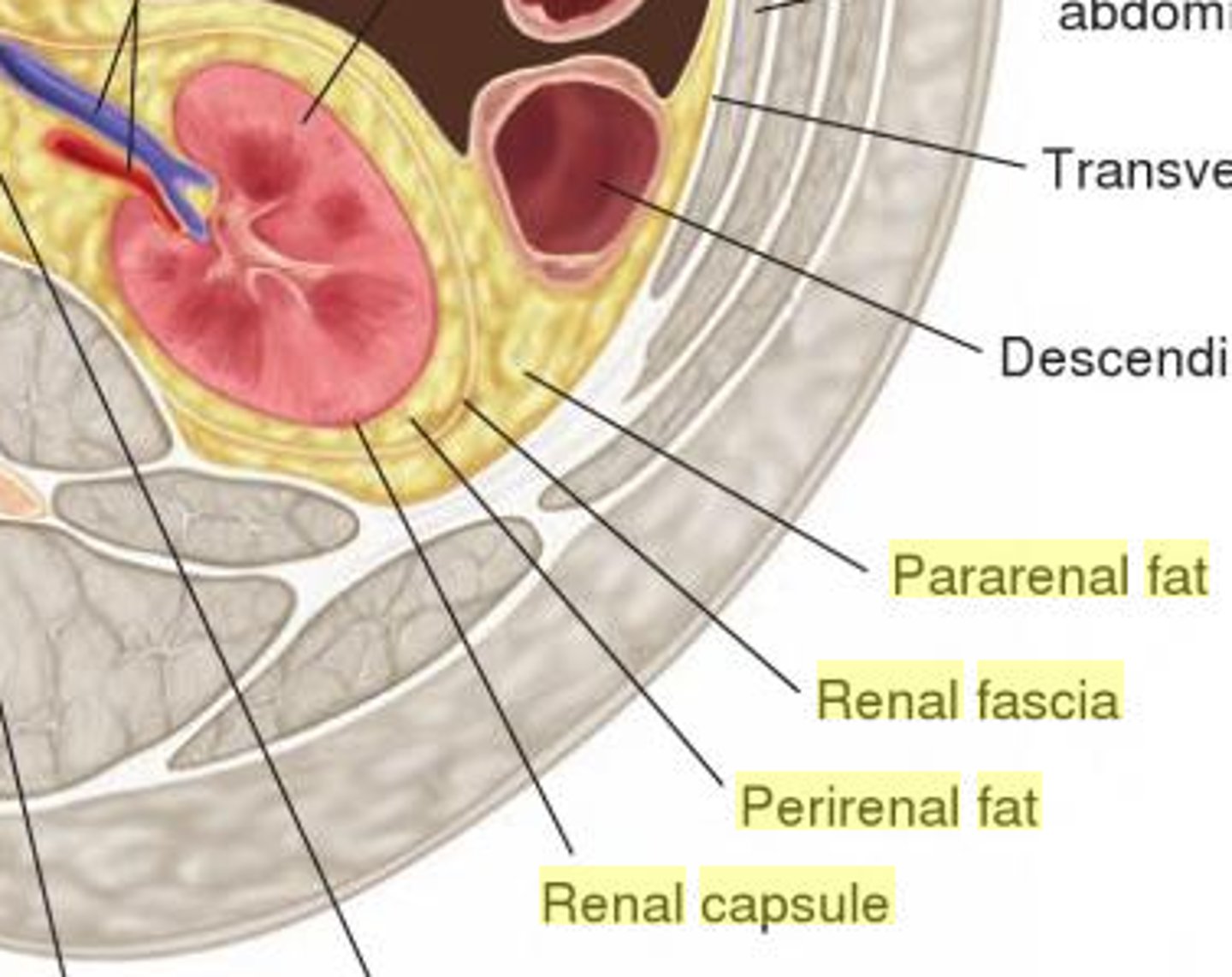
What are the 3 layers of supportive tissue in the kidneys?
1) renal fascia: outer layer of dense CT
2) perirenal fat capsule: fatty cushion
3) fibrous capsule: prevents infection
What are the 3 regions of the internal kidney?
1) renal cortex: granular superficial region
2) renal medulla: deep to cortex
3) renal pelvis: funnel-shaped tube within renal sinus
What 3 things is the renal medulla composed of?
1) medullary (renal) pyramids
2) renal columns
3) 8ish lobes
What are the 2 parts of the medullary pyramids?
1) broad base faces cortex
2) papilla (tip) points internally
What do renal columns do?
separate renal pyramids
What is a kidney lobe?
medullary pyramid + surrounding cortical tissue
The renal pelvis is continuous with _________.
ureter
What are the 2 parts of the kidney that flow into the renal pelvis?
1) minor calyces: collect urine from papillae
2) major calyces: collect urine from minor calyces and empty into renal pelvis
What is the pathway of urine flow through the kidney?
1) renal pyramid (and papillae)
2) minor calyx
3) major calyx
4) renal pelvis
5) ureter
What is the blood supply for the kidneys?
1) renal arteries: deliver 1/4 of cardiac output
2) venous flow out of kidney
What is the nerve supply for the kidneys?
sympathetic fibers from the renal plexus
What is the path of blood flow through the renal blood vessels?
1) aorta
2) renal artery
3) segmental artery
4) interlobar artery
5) arcuate artery
6) cortical radiate artery
7) afferent arteriole
8) glomerulus (capillaries)
9) efferent arteriole
10) peritublar capillaries/vasa recta
11) cortical radiate vein
12) arcuate vein
13) interlobar vein
14) renal vein
15) inferior vena cava
Where is each located?
a) segmental artery
b) interlobar artery/vein
c) arcuate artery/vein
d) cortical radiate artery/vein
a) renal sinus
b) renal columns
c) border of cortex and medulla
d) in the cortex
Which 3 renal blood vessels are part of the renal corpuscle?
1) afferent arteriole
2) glomerulus (capillaries)
3) efferent arteriole
What is the nephron?
structural and functional unit that forms urine
What are the 2 main parts of the nephron?
1) renal corpuscle: glomerulus (capillaries) + Bowman's/renal capsule
2) renal tubule
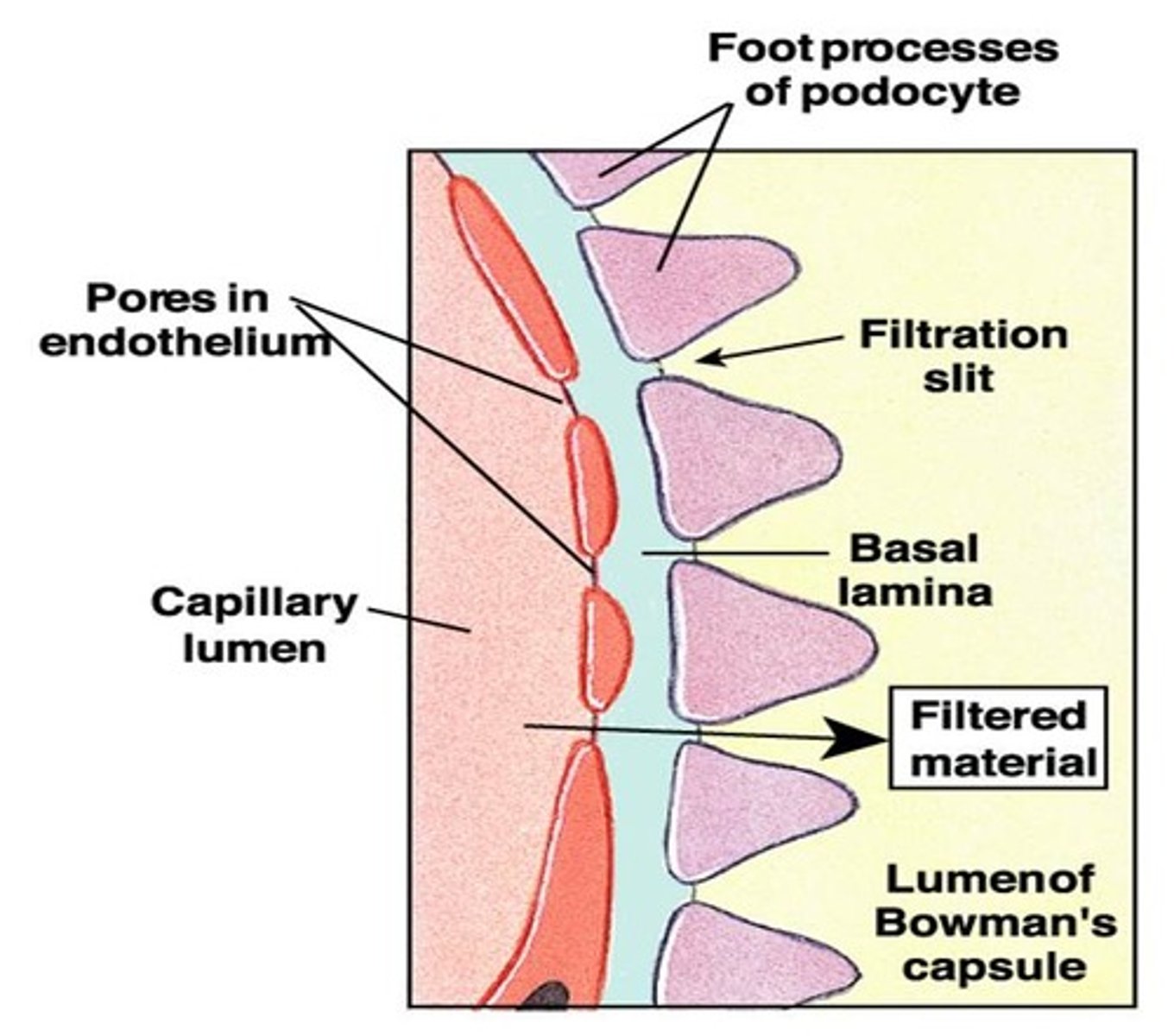
What are the 2 layers of the glomerular capsule (aka Bowman's capsule)
1) parietal layer: simple squamous epithelium
2) visceral layer: branching epithelial podocytes
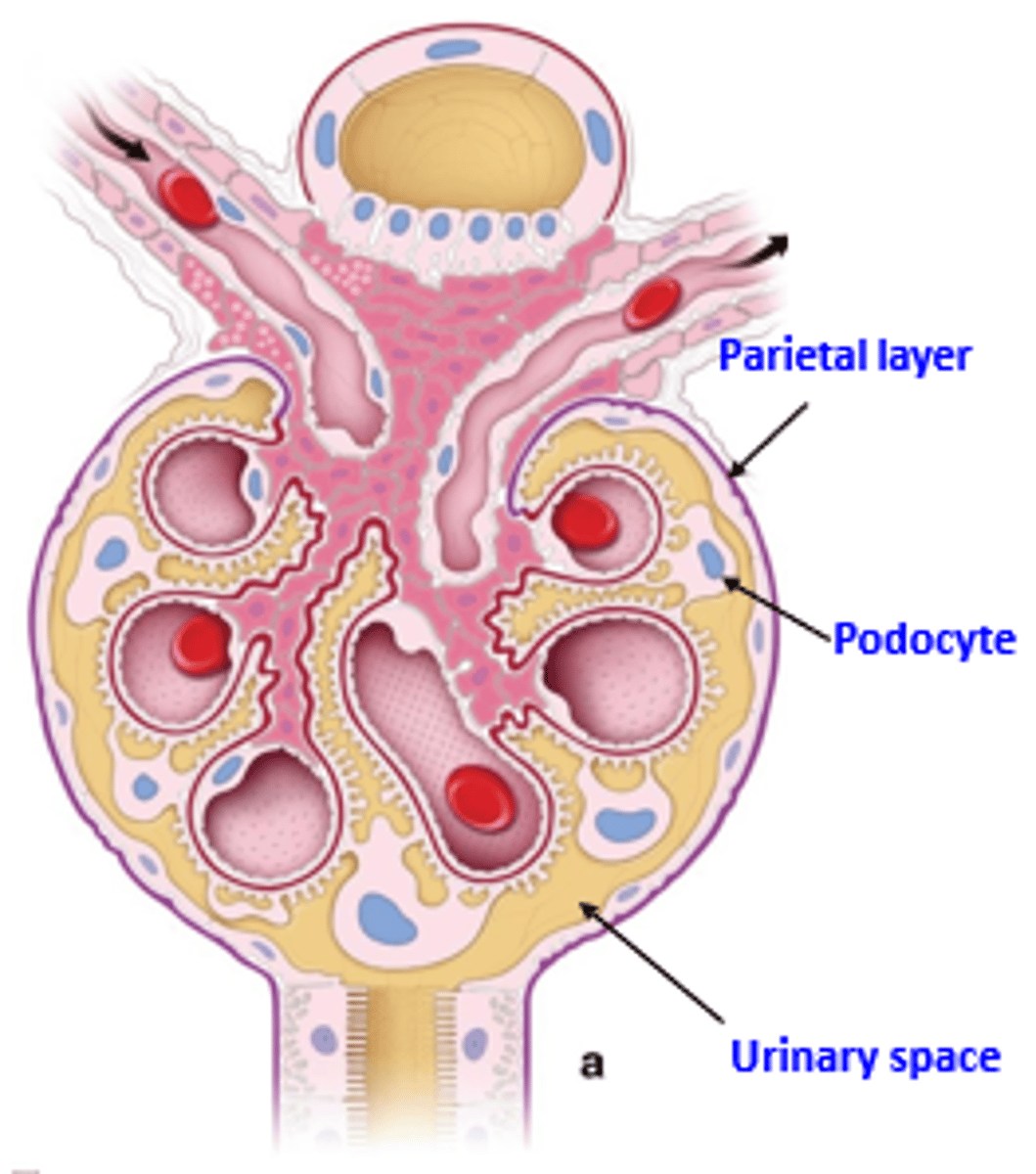
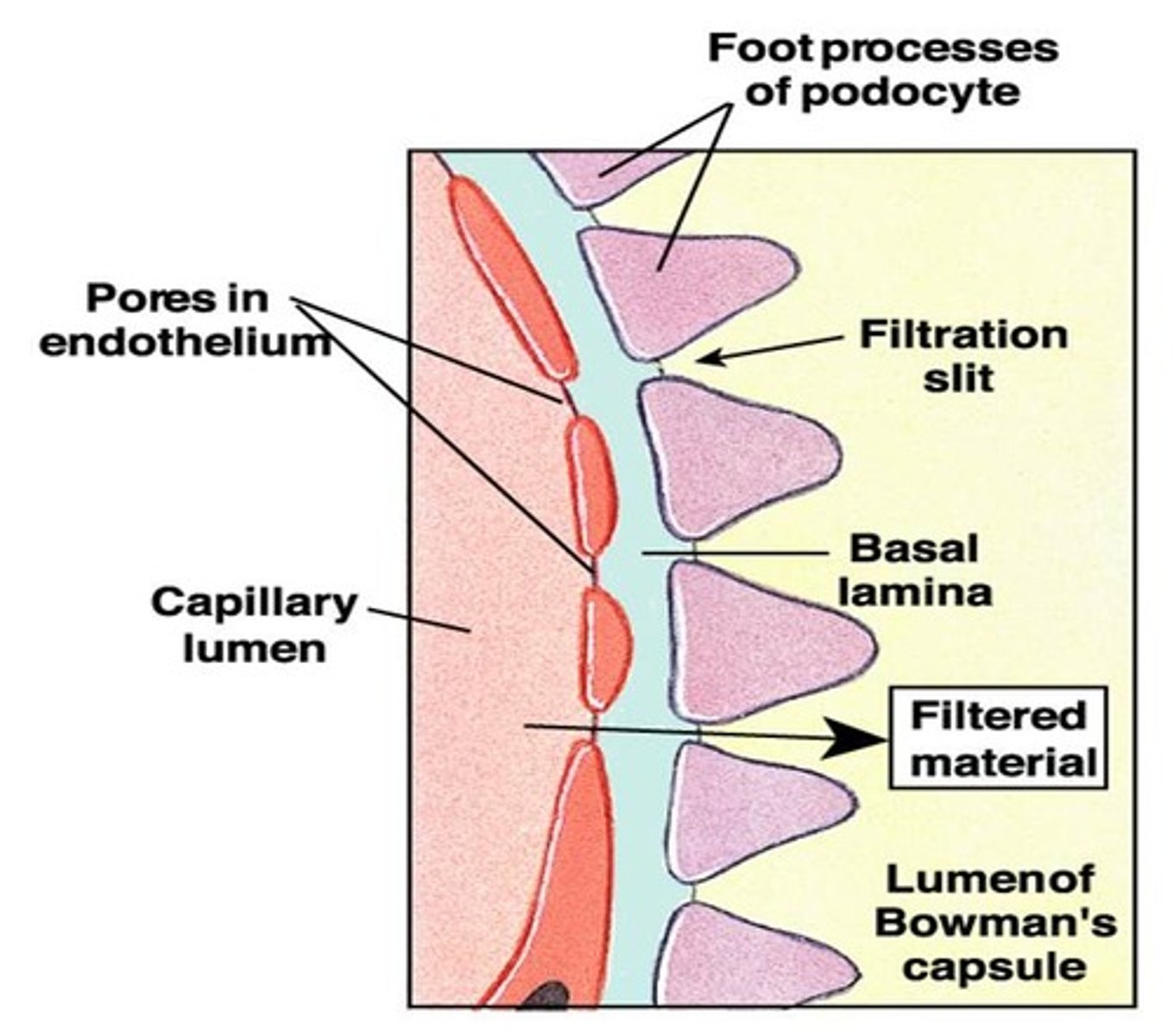
What are 2 characteristics of podocytes?
1) foot processes cling to basement membrane
2) filtration slits allow filtrate to pass through
What are the 3 major parts of the renal tubule?
1) proximal convoluted tubule (PCT)
2) nephron loop/loop of Henle (ascending + descending loops)
3) distal convoluted tubule (DCT)
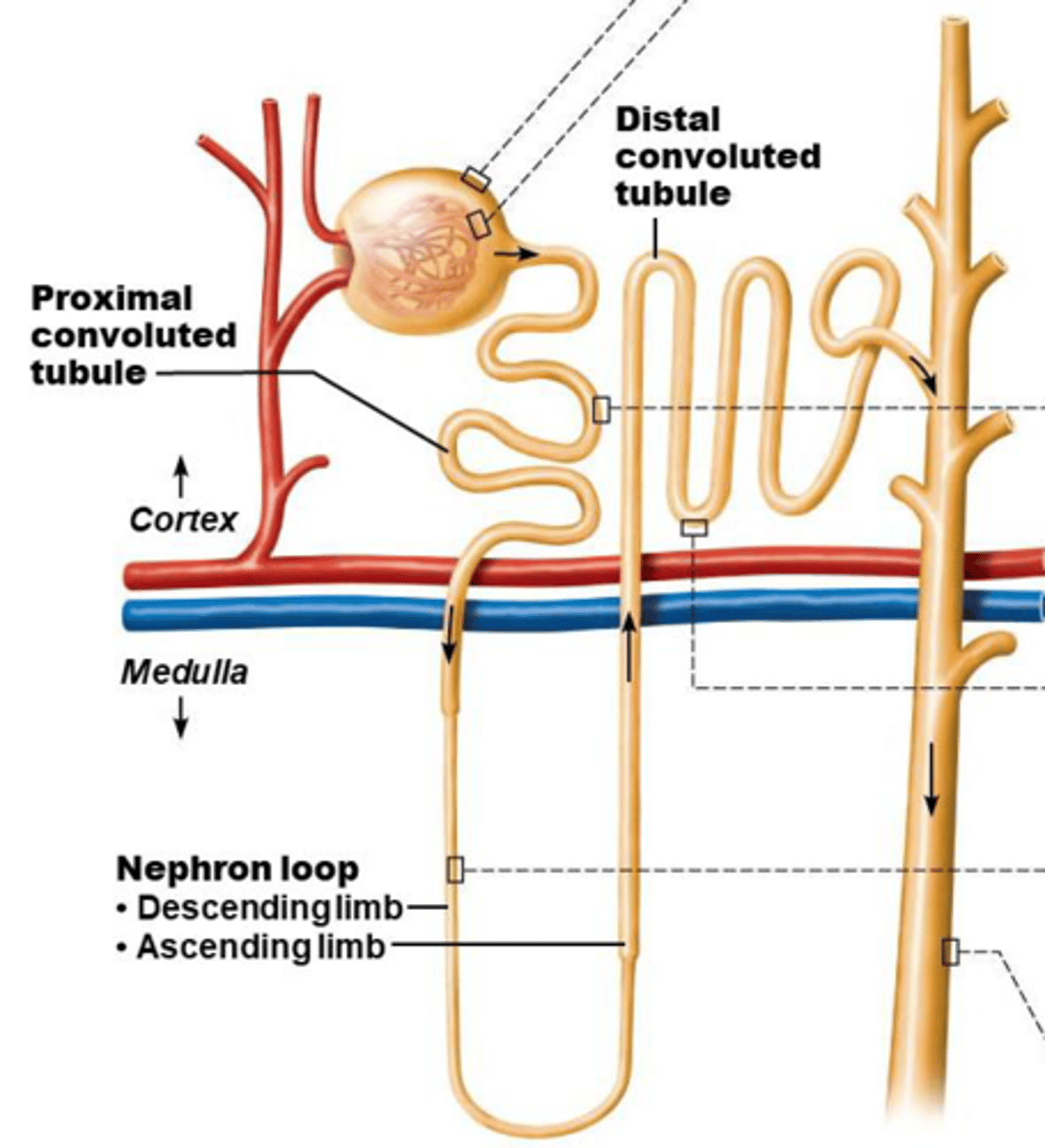
For the PCT,
a) what is the histology
b) what is the function
c) where is it located
a) cuboidal cells with dense microvilli
b) reabsorption and secretion
c) confined to cortex
For the nephron loop,
a) what is the histology + function of the descending limb
b) what is the histology of the ascending limb
a) thin, simple squamous epithelium, permeable to water
b) thick, cuboidal to columnar cells
For the DCT,
a) what is the histology
b) what is the function
c) where is it located
a) cuboidal cells with very few microvilli
b) more secretion than reabsorption
c) confined to cortex
Regarding collecting ducts,
a) what forms them
b) what do they form
a) many nephrons
b) fuse together to deliver urine through papillae into minor calyces
What are the 2 types of cells in the collecting ducts?
1) intercalated cells
2) principal cells
For intercalated cells,
a) what is the histology
b) what is the function
a) cuboidal cells with microvilli
b) maintain acid-base balance
For principal cells,
a) what is the histology
b) what is the function
a) cuboidal cells without microvilli
b) maintain body's water/salt balance
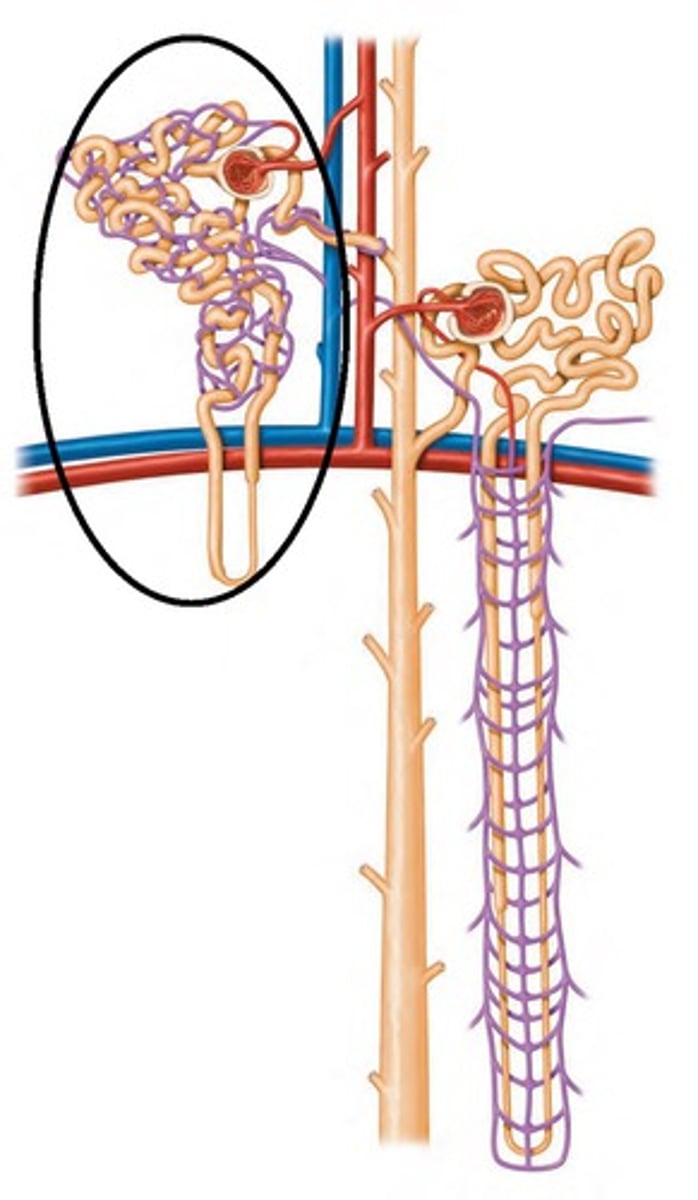
What are the 2 types of nephrons?
1) cortical nephrons: 85%
2) juxtamedullary nephrons: 15%
For the cortical nephron,
a) where is it located
b) how long is the loop of Henle
c) where is the glomerulus located
d) what does the efferent arteriole supply
a) entirely in cortex
b) short
c) further from corticomedullary junction
d) peritubular capillaries
For the juxtamedullar nephron,
a) where is it located
b) how long is the loop of Henle
c) where is the glomerulus located
d) what does the efferent arteriole supply
a) mostly deep in medulla
b) long
c) closer to corticomedullary junction
d) vasa recta
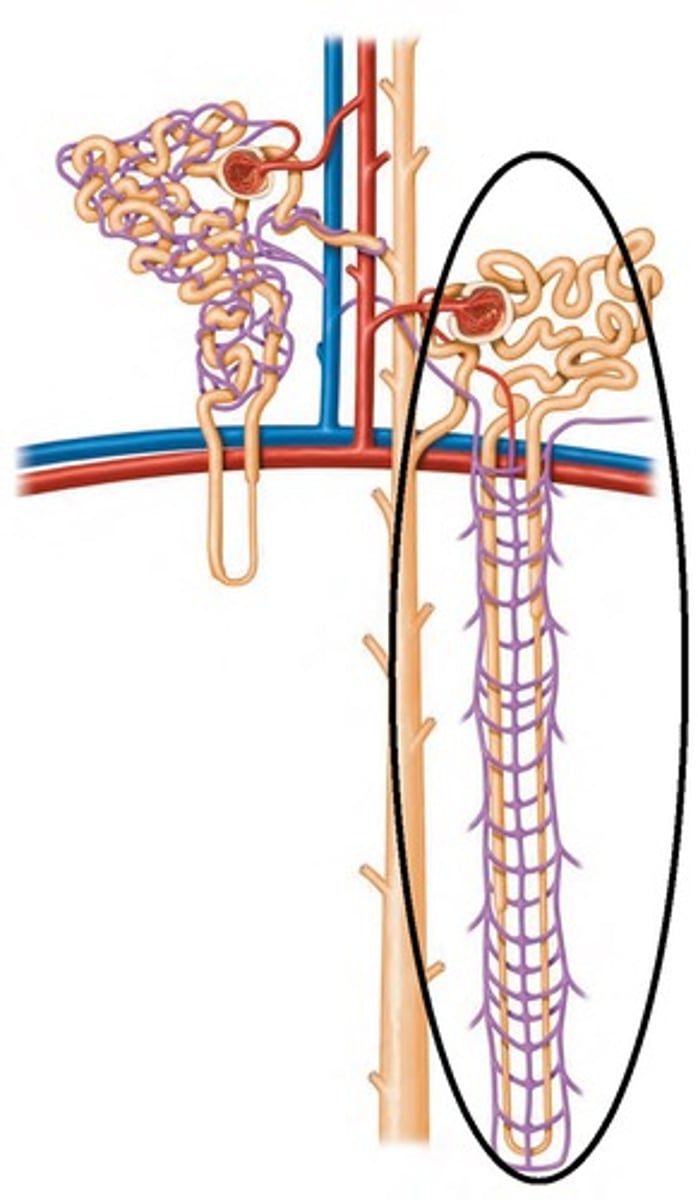
For juxtamedullary nephrons,
a) are the segments thick or thin?
b) what is their main function
a) thin
b) production of concentrated urine
Which 2 capillary beds are the renal tubules of each nephron associated with?
a) cortical nephron
b) juxtamedullary nephrons
a) glomerulus + peritubular capillaries
b) glomerulus + vasa recta
For the glomerulus,
a) what is the pathway through it
b) what is its function
c) are they high or low pressure
a) afferent arteriole --> glomerulus --> efferent arteriole
b) filtration
c) high BP
Why is the BP high in the glomerulus? (3 reasons)
1) afferent arterioles have a larger diameter than efferent arteriole
2) arteriole are high-resistance vessels
3) to filter all the blood
For peritubular capillaries,
a) are they high or low pressure
b) what is their function
c) what blood vessel do they arise from
d) what do they empty into
a) low
b) absorption
c) efferent arterioles
d) venules (cortical radiate vein)
For vasa recta,
a) from where do they arise
b) what is their function
a) efferent arterioles of juxtamedullary nephrons
b) concentration of urine
Each nephron has one juxtaglomerular apparatus (JGA). What is the JGA important for?
regulation of filtrate formation + BP
What are the 2 modified portions of the JGA?
1) distal portion of ascending limb
2) afferent arteriole
What are the 2 cell types of the JGA?
1) granular/juxtaglomerular cells
2) macula densa
For JG cells,
a) what are they
b) what do they contain
c) what is their function
a) smooth muscle cells of arteriole
b) renin
c) mechanoreceptos: sense BP
For macula densa,
a) what are they
b) what is their function
a) cells of the ascending limb
b) chemoreceptors: sense NaCl content in filtrate
What is the kidney's filtration membrane?
porous membrane between the blood (glomerular capillaries) + the capsular space
What are the 3 layers of the filtration membrane (from innermost to outermost)?
1) fenestrated endothelium: glomerular capillaries
2) gel-like basement membrane: fused basal lamina
3) visceral membrane (of glomerular capsule): podocytes
For ureters,
a) what do they do
b) are they retroperitoneal or intraperitoneal
c) how do they enter the bladder
a) convey urine from kidneys to bladder
b) retroperitoneal
c) enter the base through posterior wall
As bladder pressure increases, what do ureters do?
distal ends close, preventing backflow of urine
What are the 3 layers of the ureter wall?
1) transitional epithelium
2) smooth muscle muscularis: contracts due to stretch
3) adventitia: fibrous CT
For the urinary bladder,
a) what is it
b) is it retroperitoneal or intraperitoneal
c) what gland surrounds its neck in males
d) where is it located in females
a) muscular sac that temporarily stores urine
b) retroperitoneal
c) prostate gland
d) anterior to vagina and uterus
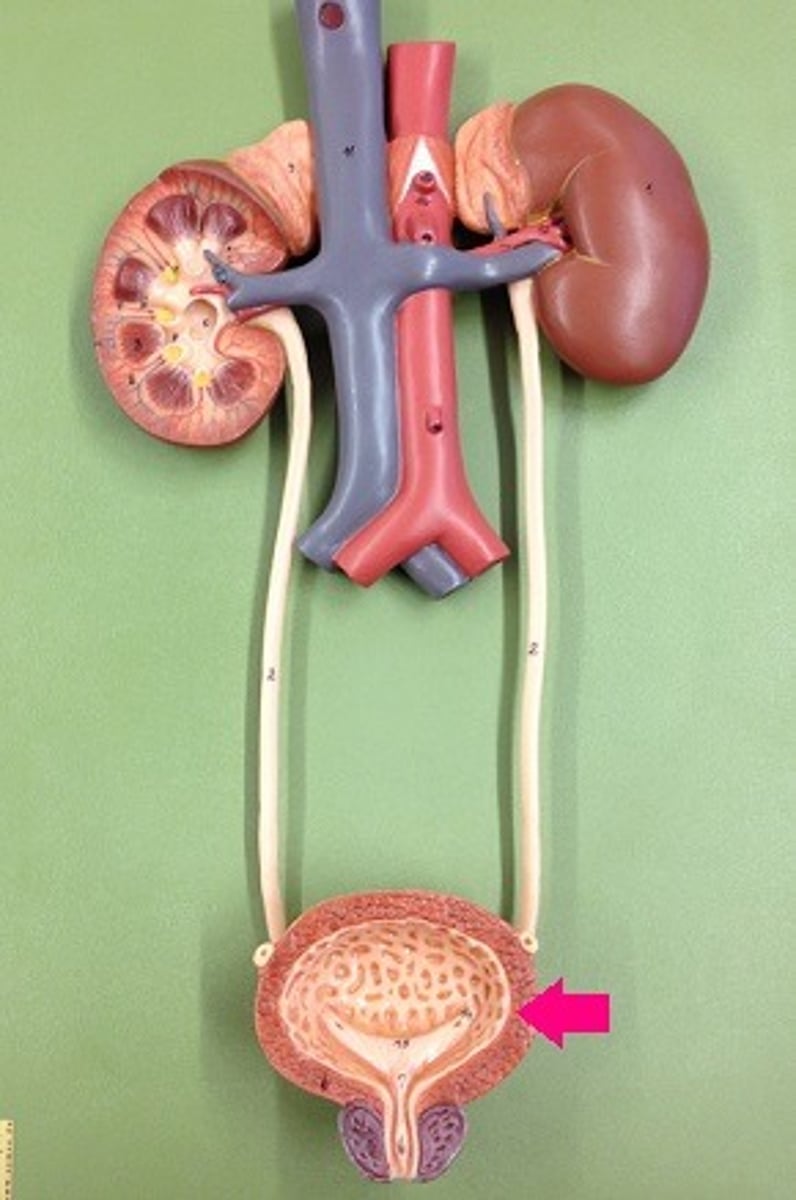
What is the trigone?
- part of the urinary bladder
- triangular area: 2 opening for ureters at top, 1 opening for urethra at bottom
- infections persist here
What are the 3 layers of the bladder wall?
1) transitional epithelial mucosa
2) detrusor muscle (smooth muscle)
3) fibrous adventitia
When do rugae in the urinary bladder appear?
when the urinary bladder is empty/collapses
What is the importance of the urogenital diaphragm?
it supports the urethra and maintains urinary/reproductive functions (ex: peeing and ejaculation)
The urethra is a muscular tube. What is its histology? (it changes)
- mostly pseudostratified columnar epithelium
- transitional epithelium near bladder
- stratified squamous epithelium near external urethral orifice
What are the 2 sphincters of the urethra (and what muscle makes up each)?
1) internal urethral sphincter: involuntary/smooth muscle
2) external urethral sphincter: voluntary/skeletal muscle
Where is each sphincter located?
a) internal urethral sphincter
b) external urethral sphincter
a) contracts to open at bladder-urethra junction
b) where the urethra passes through the pelvic floor
What are 2 differences between the female and male urethra?
1) male urethra is longer
2) male urethra carries both semen and urine (female urethra only carries urine)
For the female urethra,
a) what is it bound to
b) what is the external urethral orifice located between
a) anterior vaginal wall
b) anterior to vaginal opening, posterior to clitoris
What are the 3 regions of the male urethra? (from superior to inferior)
1) prostatic urethra
2) membranous urethra
3) spongy urethra
Where is each region of the male urethra located?
a) prostatic urethra
b) membranous urethra
c) spongy urethra
a) prostate gland
b) passes through urogenital diaphragm
c) passes through penis to open via external urethral orifice