Brain, Mind, and Behavior - Exam 3
1/225
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
226 Terms
Psychiatric disorders
disorders of psychological function sufficiently severe to require treatment
Difficulties in diagnosing psychiatric disorders
1. biological tests for psychiatric disorders are not developed enough to actually diagnose someone
2. we have to rely on patients' symptoms
a. patients with the same disorder may display different symptoms
b. patients with different disorders may display the same symptoms
How does the National Institute of Health deal with psychological disorders?
Instead of diagnosing psychological disorders, it diagnoses people with particular features/symptoms
DSM 5
the current edition of the Diagnostic and Statistical Manual of the American Psychiatric Association
Inclusion criteria
characteristics that patients must have in order to qualify for a specific diagnosis (eg. symptoms of hallucinations and delusions for schizophrenia)
Exclusion criteria
characteristics of patients that prevent them from being given a specific diagnosis (i.e. is there another reason why this patient might have these symptoms)
Three general ways of treating psychopathology
- behavioral methods/counseling
- medication/drug treatment/nutrition
- neurosurgery/stimulation treatments
Schizophrenia
- psychotic disorder involving distortions in thoughts, perceptions, and/or emotions
- affects approx. 1 percent of the population
Schizophrenia positive symptoms
symptoms that seem to represent an excess of typical function
includes delusions, hallucinations, disorganized speech, inappropriate affect (emotions), and other odd behavior
Schizophrenia negative symptoms
symptoms that seem to represent a reduction/loss of typical function
Affective flattening - diminished emotional expression
Avolition - reduction or absence of emotion
Catatonia - remaining motionless for long periods of time
Genetic/environmental influences on schizophrenia
genes have been identified that might predispose individuals to schizophrenia, but environmental influences explain why schizophrenia is eventually developed (typically through epigenetic mechanisms)
Brain changes associated with schizophrenia
- enlarged ventricles
- loss in cortical volume, especially in temporal lobes and dorsal peak
- hypofrontality
- shrinking and disorganization of the hippocampus
Hypofrontality
reduced activation of the cortex of the frontal lobes of the brain
Dopamine hypothesis of schizophrenia
the theory that schizophrenia is caused by too much activation of dopamine (D2) receptors and, conversely, that antipsychotic drugs exert their effects by decreasing dopamine levels
Evidence for dopamine hypothesis
- drug-induced psychosis risk is very high with drugs that increase synaptic dopamine availability: cocaine, amphetamines
- typical antipsychotics were found to affect dopamine activation
Binding affinity
a high affinity means a drug binds strongly to a receptor; the high affinity of competitive antagonists allows them bind to receptors and block neurotransmitters
D2 dopamine receptors
type of dopamine receptor that is suspected to have the greatest impact of parkinson's/schizophrenia
Problems with the dopamine theory of schizophrenia
- antipsychotic drugs don't treat the negative symptoms of schizophrenia
- people with schizophrenia seem to have normal levels of dopamine
- some drugs (like atypical antipsychotics) work effectively without affecting D2 dopamine receptors
Treatments for schizophrenia include
1. antipsychotic drugs
2. psychotherapy
3. cognitive behavioral therapy
Cognitive behavioral therapy
a popular integrative therapy that combines cognitive therapy (changing self-defeating thinking) with behavior therapy (changing behavior)
Antipsychotic (neuroleptic) drugs
drugs used to treat symptoms of schizophrenia and bipolar disorder
Psychosis
psychological symptoms where a person loses contact with reality, experiencing irrational ideas and distorted perceptions (not necessarily caused by schizophrenia)
Typical antipsychotics
the first generation of antipsychotic drugs, which work as dopamine antagonists
Chlorpromazine
a typical antipsychotic that is a competitive antagonist at dopamine receptors; this blockage sends a signal back to the presynaptic neuron to release more dopamine because there is not enough...however, this dopamine will be prevented from binding to the receptor and will get broken down in the synaptic cleft
Haloperidol
competitive antagonist at dopamine D2 receptors
Reserpine
another early antipsychotic drug; the active ingredient of the snakeroot plant; breaks down synaptic vesicles of the dopamine neurotransmitter
Atypical antipsychotics
second generation of antipsychotic drugs; do not have a strong binding affinity with D2 dopamine receptors; generally work by blocking serotonin 5-HT2 receptors
Common atypical antipsychotics include
clozapine and risperidone
Glutamate hypothesis of schizophrenia
proposal that schizophrenia relates to deficient activity at glutamate synapses
Psychotomimetic
a drug that induces a state resembling schizophrenia
Classical hallucinogens
- LSD, mescaline, psilocybin
- agonize serotonin
- mimic schizophrenia's positive symptoms
Dissociative hallucinogens
- ketamine, PCP
- antagonize glutamate
- mimic schizophrenia's negative symptoms
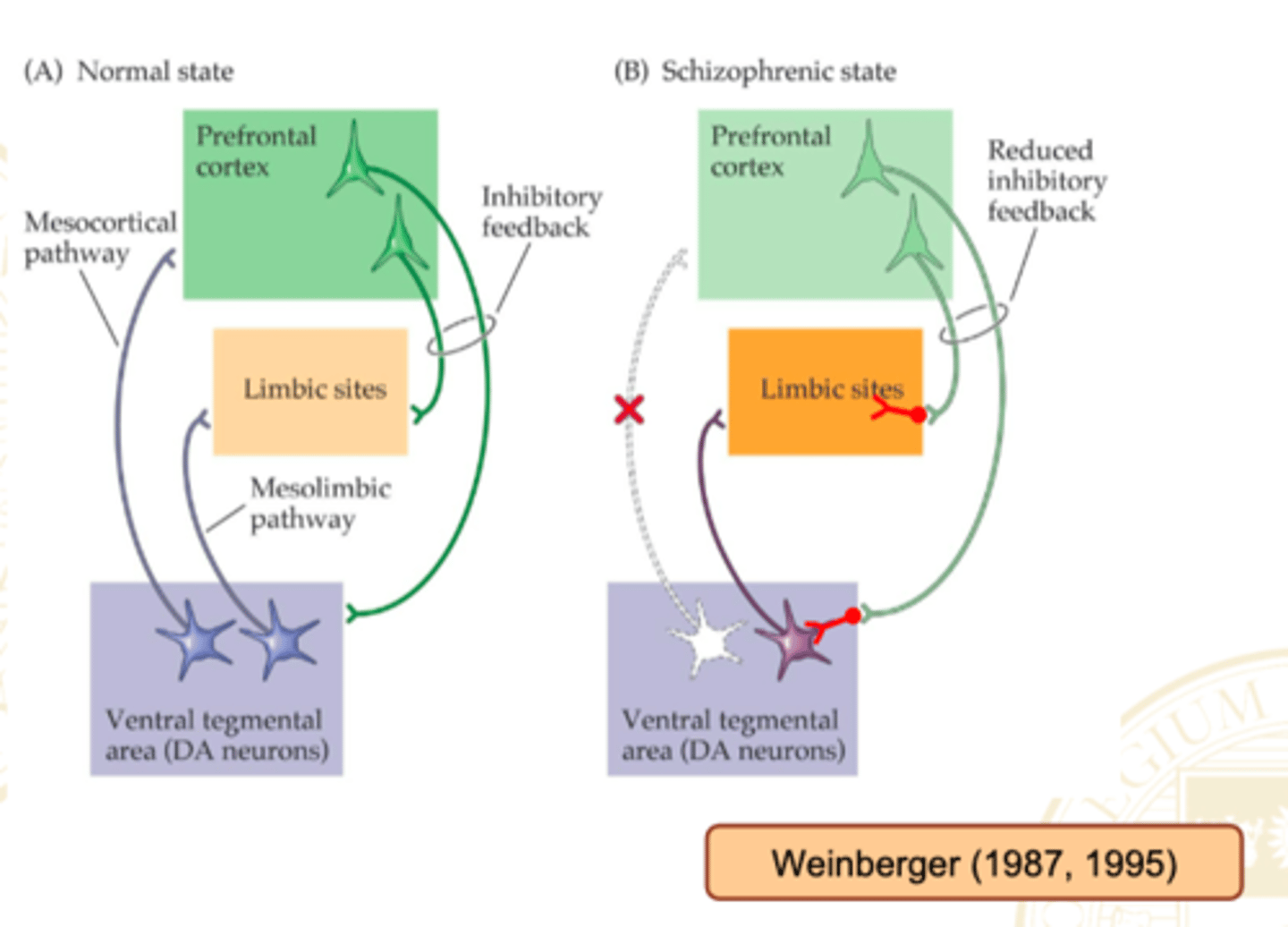
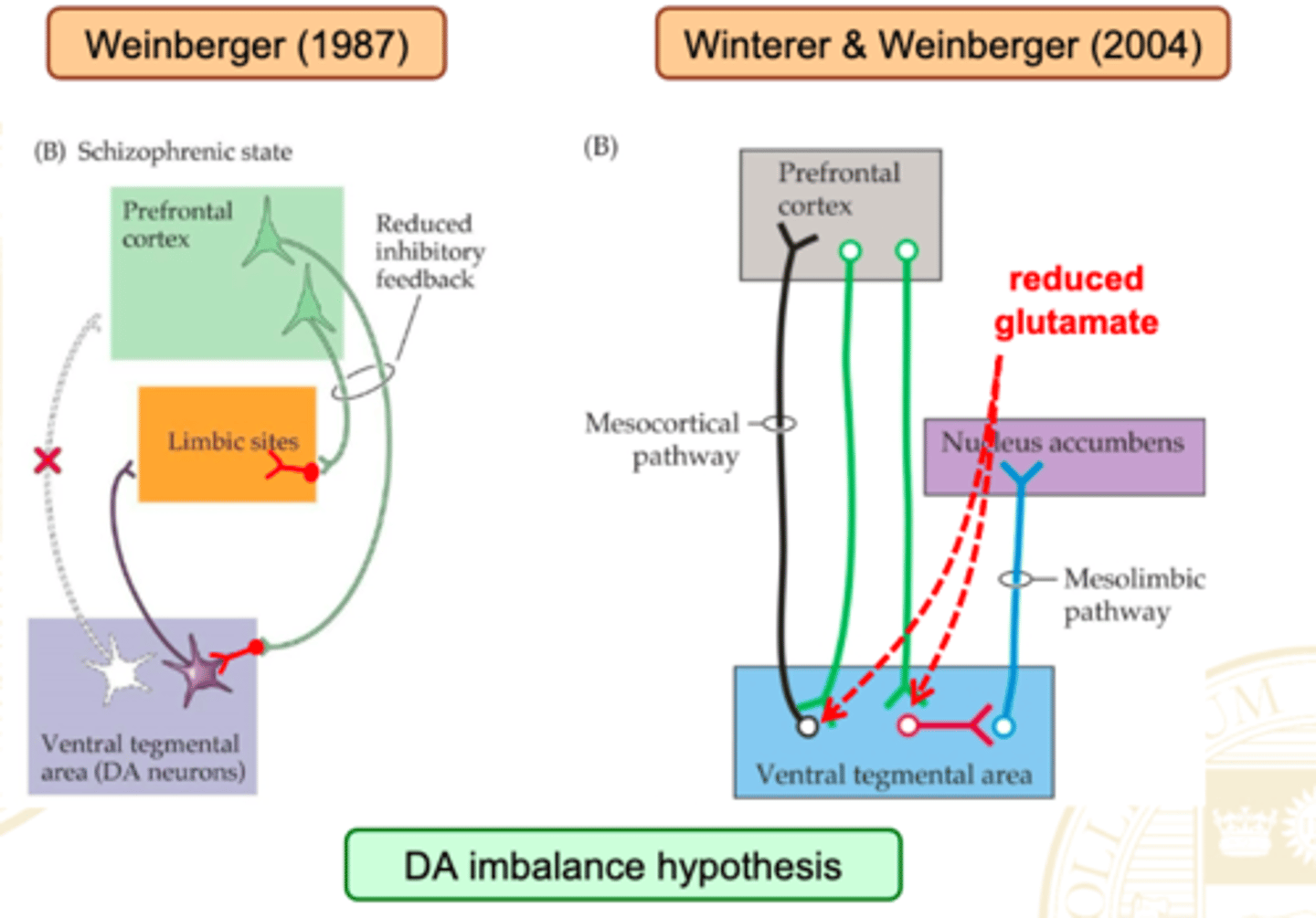
Weinberger's original neurodevelopmental model of schizophrenia
Suggests that the dopamine projection from the VTA to the prefrontal cortex doesn't develop correctly in schizophrenics. This would cause underactivation of PFC, and thus an overactivation of limbic system and specifically the nucleus accumbens (since one of the jobs of PFC is to inhibit the NA).
Newer dopamine imbalance theory
Also says that schizophrenia results from an underactive prefrontal cortex and an overactive limbic system. However, this theory argues that this is a result of a faulty glutamate system. Since the descending signals from PFC to NA are mediated by glutamate, synapsing on GABAergic interneurons in the NA, then it will poorly inhibit this structure
Major depressive disorder
depression that is so severe that it is difficult for the patient to meet the essential requirements of daily life (aka. clinical/unipolar depression)
Symptoms of major depressive disorder
-Decreased energy, interests, concentration
-Altered sleeping and eating behavior
-Irritability, physical exhaustion, continuous anxiety
-Anhedonia
Anhedonia
not finding pleasure in things anymore
Reactive depression
depression triggered by an obvious negative experience
no longer an exclusion criteria on the DSM-5!
Cell loss in patients predisposed to depression
amygdala and medial prefrontal cortex
Cell loss in patients diagnosed with depression
besides the previous areas, also the hippocampus and cingulate gyrus
Treatments for depression
- counseling and psychotherapy
- antidepressant medication
- stimulation techniques like electroconvulsive shock therapy, transcranial magnetic stimulation, and deep brain stimulation
Monoamine theory of depression
the theory that depression is due to deficient activity at serotonin and norepinephrine synapses in the brain (developed after observing how some antidepressants worked)
Up-regulation
a compensatory increase in receptor availability at the synapses of a neuron where there was an insufficient amount of it
Problems with monoamine theory of depression
- not everyone is helped by monoamine-targeting medication (studies show slight effectiveness of this type of medication)
- medication can take weeks to have effects
- atypical antidepressants can be effective
Monoamine Oxidase Inhibitors (MAOIs)
antidepressant medications that indirectly agonize monoamines like serotonin and norepinephrine by blocking their breakdown
Cheese effect
dangerous side effect of MAO inhibitors caused by an inability to break down tyramine-rich foods such as wine, cheese, and pickles
Iproniazid
the first MAO inhibitor
Tricyclic antidepressants
antidepressant drugs that block the reuptake of serotonin and norepinephrine
Imipramine (Tofranil)
commonly prescribed tricyclic antidepressant
Selective Serotonin Reuptake Inhibitors (SSRIs)
antidepressant drugs that agonize serotonin by blocking its reuptake; currently primary medication for depression
Common SSRIs
Prozac, Paxil, Zoloft, and Luvox
Selective Norepinephrine Reuptake Inhibitors (SNRIs)
antidepressant drugs that are similar to SSRIs, except they block the reuptake of norepinephrine
Common SNRI
Reboxetine
Atypical antidepressants
catch-all class of antidepressant drugs that have many modes of action
Bupropion (Wellbutrin or Zyban)
atypical antidepressant that blocks dopamine and norepinephrine reuptake and antagonizes nicotinic acetylcholine receptors
Ketamine
dissociative hallucinogen that also works as an atypical antidepressant by antagonizing the glutamate NMDA receptor
Neurogenesis theory of depression
an explanation of depression that proposes that neurogenesis, the growth of new neurons in the hippocampus is suppressed during depression, and can be resumed by increasing serotonin or norepinephrine
BDNF (brain-derived neurotrophic factor)
regulates neuronal survival and differentiation during development and is associated with depression (targeted by new depression therapies)
Neurotrophins
chemicals that attract/repel Axon growth, help prevent cell death, and/or promote Axonal branching
neuroplasticity theory of depression
Depression results from a decrease of neuroplastic processes in the prefrontal cortex, hippocampus, amygdala, and other brain structures which leads to neuron loss and other forms of neural pathology
Electroconvulsive shock therapy
a biomedical therapy for severely depressed patients in which a brief electric current is sent through the brain of an anesthetized patient
Transcranial magnetic stimulation (TMS) in depression
involves the delivery of repetitive magnetic pulses to enhance or depress specific cortical areas in an effort to relieve depression; usually in the prefrontal cortex
Deep brain stimulation
antidepressive measure in which electrical stimulation is applied through surgically implanted electrodes that are usually implanted in the anterior cingulate cortex or the prefrontal cortex
Cingulotomy
lesions that interrupt pathways between the anterior cingulate cortex and the prefrontal cortex in order to treat depression (and other psychopathology)
Bipolar disorder
a category of psychiatric disorders that involves alternate bouts of depression and mania or hypomania
Hypomania
a mild mania characterized by a reduced need for sleep, high energy, and positive affect
Mania
hypomania taken to extreme; also involves delusions of grandeur, overconfidence, and distractibility
Bipolar disorder type I
involves alternate bouts of depression and mania
Bipolar disorder type II
involves alternate bouts of depression and hypomania
Rapid-cycling bipolar disorder
characterized by at least 4 mood cycles in a year
Cyclothymia
disorder that consists of mood swings from moderate depression to hypomania
Treatments for bipolar disorder
psychotherapy and mood stabilizing medication
Mood stabilizing medications
1. Lithium
2. Anti-convulscant medications
3. Anti-psychotic medications
Lithium
an accidentally discovered mood stabilizer that is thought to work by agonizing serotonin
Possible causes of bipolar disorder
1. HPA-axis dysregulation
2. Circadian rhythm dysfunction
3. Monoamine and amino acid neurotransmitter dysregulation
HPA axis dysregulation
includes the hypothalamus, pituitary, and adrenal glands; causes an abnormal pattern of cortisol release
Reward hypersensitivity theory of bipolar disorder
bipolar disorder results from a dysfunctional brain reward system that overreacts to rewards or the lack thereof, explains that repeatedly rewarding individuals with BPD for their activities leads to excessive goal seeking and mania or hypomania, and explains that when people with bipolar disorder fail to achieve their goals this leads to an excessive decrease in reward seeking and depression.
Anxiety disorder
anxiety so severe that it disrupts functioning; associated with feelings and with physiological responses (ex. high heartbeat)
Generalized Anxiety Disorder (GAD)
extreme feeling of anxiety or fear about a large numbers of activities or events
Specific phobias
strong fear or anxiety about a specific object or situation
Panic disorder
recurrent rapid-onset attacks of extreme fear and severe symptoms of stress; the severe physiological symptoms of stress can also occur with the previous three disorders
Treatments for anxiety
- psychotherapy
- behavioral therapy
- anti-anxiety medication
Anxiolytic (anti-anxiety) drugs include
- benzodiazepines
- SSRIs
- buspar
Benzodiazepines
common anxiolytic that stimulates GABA-A receptors primarily in the hippocampus and amygdala (eg. Valium, Xanax)
Buspar
anxiolytic drug that is a direct 5-HT-1A serotonin agonist
Causes of anxiety
- underactivity of similar brain areas as depression, although little brain shrinkage is observed
- an overactive amygdala
Learning
a relatively permanent change in behavior due to experience
Non-associative learning
learning about a stimulus, such as sight or sound, in the external world; includes habituation and sensitization
Habituation
reduced response intensity with repeated presentation (ex. tuning out the sound of a fan)
Sensitization
increased response due to a salient event (ex. becoming jumpy after receiving an electric shock)
Dishabituation
the restoration to full strength of a response after a change of stimulus that had previously become weakened through habituation
Other-race effect in infants
infants can better detect changes in facial features in faces belonging to their own race; they also habituate quicker to faces belonging to their own race
Associative learning
learning the relationship between two pieces of information; includes classical and operant conditioning
Classical conditioning as a concept
when we learn that a stimulus predicts another stimulus
Ivan Pavlov
Russian scientist who discovered classical conditioning through his work with dog salivation
Classical conditioning mechanisms
if you pair a neutral stimulus (NS) with an unconditioned stimulus (US) that already triggers an unconditioned response (UR) that neutral stimulus will become a conditioned stimulus (CS), triggering a conditioned response (CR) similar to the original unconditioned response
Neutral stimulus (NS)
in classical conditioning, a stimulus that elicits no response before conditioning
Unconditioned stimulus (US)
in classical conditioning, a stimulus that unconditionally—naturally and automatically—triggers a response (meat powder)
Unconditioned response (UR)
in classical conditioning, the unlearned, naturally occurring response to the unconditioned stimulus (US) (dogs salivating to the meat powder)
Conditioned stimulus (CS)
in classical conditioning, an originally irrelevant stimulus that, after association with an unconditioned stimulus, comes to trigger a conditioned response (the bell)