body fluids & electrolytes pt. 2
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
key components of bone
calcium (Ca2+), phosphorus (as phosphate, PO43-), & magnesium (Mg2+). calcium is most abundant
bone structure
organic matrix (~30%): gives bone resiliency. inorganic mineral salt (~70%): embedded in the organic matrix, made of hydroxyapatite crystal (calcium & phosphate).
calcium (Ca2+)
bone & teeth formation, nerve & brain function (signal conduction), neuromuscular excitability, muscle contraction, cofactors for blood coagulation & many enzymes. most abundant electrolyte. 99% in bone/teeth, 1% in blood/soft tissue. normal range: 8.6-10 mg/dL (total)
calcium is present in plasma in 3 forms:
protein bound (mainly albumin)
complexed (anions = phosphate or citrate)
ionized or “free” (iCa2+), RR: 4.4-5.3 mg/dL, ~47%, the only one that’s physiologically active & is closely regulated (by PTH)
total calcium
affected by serum albumin level (b/c binding): low albumin → low even w/ normal iCa2+, high albumin → high even w/ normal iCa2+. not affected by acute changes in acid-base balance
ionized calcium
active form. affected by acute changes in acid-base balance b/c pH alters binding to proteins. acidic pH → high b/c H+ competes w/ Ca2+ for binding sites, less Ca2+ bound to proteins. alkaline pH → low b/c less H+ competing, more Ca2+ is bound to proteins. not affected by changes in albumin
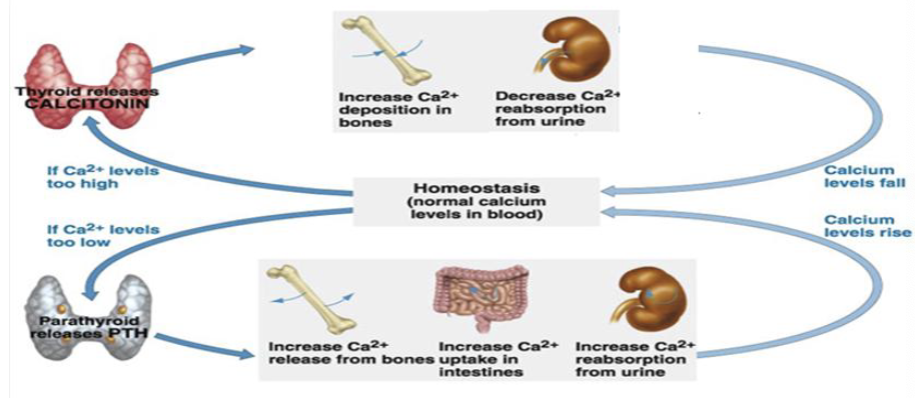
calcium homeostasis
the body’s calcium is in a state of constant flux b/t blood, GI tract, kidney, & bone. maintained by an endocrine system involving 3 hormones & 3 organs

3 major hormones that maintain calcium homeostasis
parathyroid hormone (PTH, most important), vitamin D (important), calcitonin (not as important)
3 organ systems that maintain calcium homeostasis
GI tract: vit D inc absorption of dietary Ca2+
bone: PTH & vit D inc bone resorption (breakdown), releasing Ca2+ into blood
kidney: PTH inc reabsorption of Ca2+ from ultrafiltrate, vit D inc reabsorption of both
parathyroid hormone (PTH)
secreted from parathyroid glands. active portion is where the N-terminal segment is on the single polypeptide chain. most important regulator of plasma Ca2+ & phosphate levels. synthesis regulated primarily by plasma Ca2+ levels
how does low Ca2+ influence PTH secretion?
increase PTH secretion
how does high Ca2+ influence PTH secretion?
decrease PTH secretion (negative feedback)
how does PTH increase blood Ca2+?
stimulates small intestine to absorb dietary Ca2+ (& phosphate) indirectly thru activation of vit D. stimulates bone to inc bone resorption, releasing Ca2+ (& phosphate) into blood. stimulates kidney to inc renal reabsorption of Ca2+, & dec renal reabsorption of phosphate, activate vit D
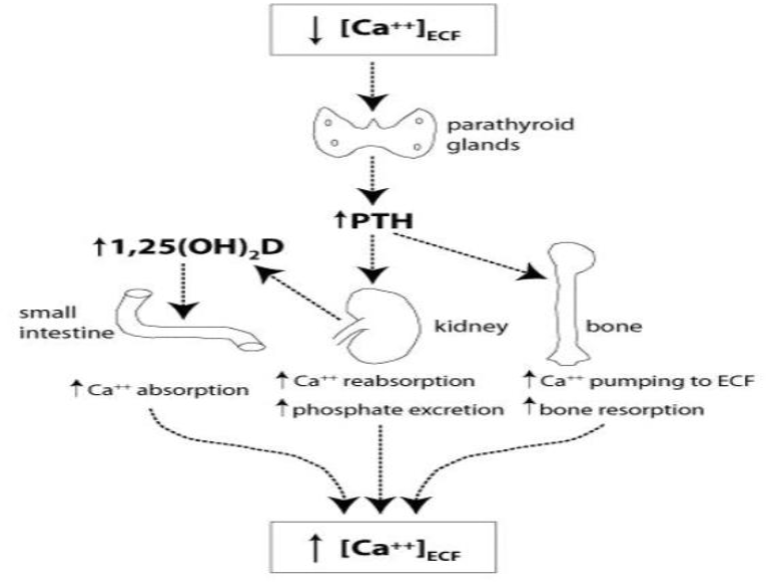
why does the kidney decrease renal reabsorption of phosphate to increase blood Ca2+?
it lowers blood phosphate levels. inverse relationship between blood Ca2+ & phosphate levels
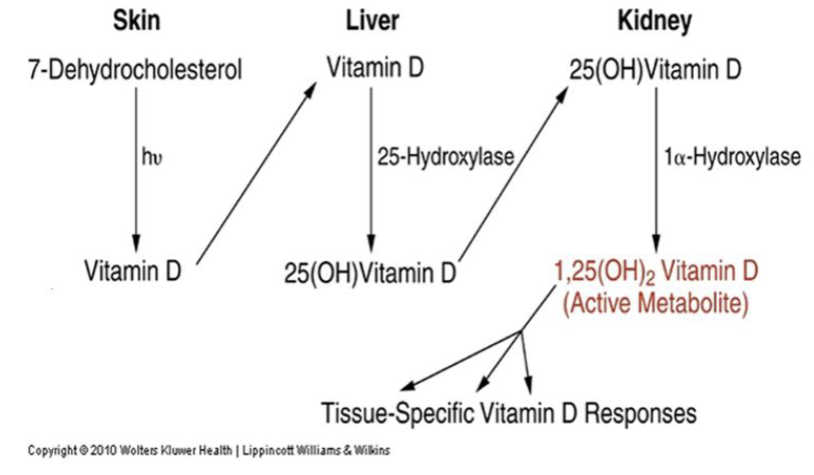
vitamin D (calcitriol)
steroid hormone. cofactor for normal response to PTH, critical for maintaining adequate Ca2+ & phosphate levels for proper mineralization of bone. important in neuromuscular/immune systems. from diet & synthesis (needs light). raises blood Ca2+
how does vitamin D raise blood Ca2+?
acts on small intestine directly to inc Ca2+ & phosphate absorption, bone (in concert w/ PTH) to release Ca2+ & phosphate from bone, kidney to assist PTH reabsorbing Ca2+ & phosphate, thyroid gland to inhibit release of calcitonin
vitamin D synthesis
humans can make it w/ sufficient sun exposure. involves skin, liver, kidneys. UV light transforms 7DC to vit D in skin. vit D hydroxylated to 25-OH vit D (calcifediol) in liver. serum 25-OH can monitor stored vit D. vit D hydroxylated to active form 1,25-(OH)2 vit D (calcitriol). when blood Ca low, PTH released & stimulates kidneys to inc vit D formation
calcitonin
produced in medulla of thyroid glands. reduces serum Ca2+ by affecting bone (blocking bone resorption) & kidney (inhibits renal reabsorption of Ca2+ & P). levels do not greatly influence serum Ca2+. mainly used to Dx medullary thyroid cancer (very high levels in serum).
how is calcitonin production regulated?
by plasma Ca2+ levels. high when Ca2+ is high, low when Ca2+ is low. ‹
hypocalcemia
total [Ca2+] & iCa2+ low. critical (panic): total [Ca2+] < 6mg/dL. mild to life-threatening. arrhythmias & cardiac arrest. neuromuscular irritability (major): neurologic excitability, tetany. impaired intellectual functioning, psychoses, convulsions if severe. osteoporosis & pathologic fractures if chronic
![<p>total [Ca<sup>2+</sup>] & iCa<sup>2+</sup> low. critical (panic): total [Ca<sup>2+</sup>] < 6mg/dL. mild to life-threatening. arrhythmias & cardiac arrest. neuromuscular irritability (major): neurologic excitability, tetany. impaired intellectual functioning, psychoses, convulsions if severe. osteoporosis & pathologic fractures if chronic</p>](https://knowt-user-attachments.s3.amazonaws.com/9a5473b5-dc5f-4b89-977d-3830c1c589de.png)
hypercalcemia
total [Ca2+] & iCa2+ high. critical (panic): total [Ca2+] > 15mg/dL. often asymptomatic. arrhythmias & cardiac arrest. neuromuscular irritability (major): weakness, lethargy. groans (confusion, depression), bone (demineralization/fracture from high resorption), moans (constipation → abdominal pain, N/V), & kidney stones
![<p>total [Ca<sup>2+</sup>] & iCa<sup>2+ </sup>high. critical (panic): total [Ca<sup>2+</sup>] > 15mg/dL. often asymptomatic. arrhythmias & cardiac arrest. neuromuscular irritability (major): weakness, lethargy. groans (confusion, depression), bone (demineralization/fracture from high resorption), moans (constipation → abdominal pain, N/V), & kidney stones </p>](https://knowt-user-attachments.s3.amazonaws.com/a154f6f7-d960-4544-8187-f0da8b537ecc.png)
primary cause of hypocalcemia
problems w/ parathyroid gland: low serum PTH, primarily hypoparathyroidism (thyroidectomy, autoimmune destruction, mutations, etc). low serum PTH → low Ca2+& vit D, high P
secondary causes of hypocalcemia
problems independent of parathyroid gland: high serum PTH (secondary hyperparathyroidism). pseudohypoparathyroidism, severe vit D deficiency, chronic kidney dz/failure (most common)
hypocalcemia due to pseudohypoparathyroidism
hereditary lack of response to PTH. low Ca2+ & vit D, high P → high serum PTH.
hypocalcemia due to severe vitamin D deficiency
renders PTH ineffective. low vit D → low Ca2+ & low P → high serum PTH.
hypocalcemia due to chronic kidney disease (failure)
most common. low vit D activation, high Ca2+ renal loss, low P renal excretion. low vit D & Ca2+ → high serum PTH. GFR low. high BUN, Cr, urine Ca2+. soft tissue calcification (Ca2+-P precipitate), Ca2+ kidney stones
primary cause of hypercalcemia
problem w/ parathyroid gland: high serum PTH. primary (parathyroid adenoma/hyperplasia, most common) or tertiary hyperparathyroidism. high serum PTH → high Ca2+, vit D, urine Ca, urine P, low serum P. kidney Ca2+ stone
secondary cause of hypercalcemia
problem independent of parathyroid gland: low serum PTH. malignancy & vitamin D intoxication
hypercalcemia due to malignancy
rapidly progressive. direct invasion of bone, secretion of PTH related peptide (PTHrP) by various tumors (MM). high serum PTHrP → high Ca2+, low P, serum PTH, vit D. PTHrP has PTH-like activity, but can be high b/c production not regulated by blood Ca2+
hypercalcemia due to vitamin D intoxication
high vit D → high Ca2+, P, low serum PTH. Ca2+-P precipitated in soft tissues. kidney Ca2+ stone
soft tissue calcification
tissue becomes hardened by deposition of calcium salts, which normally occurs in bone/teeth. from abnormal serum Ca or P levels in trophic tissues. conditions a/w these: chronic kidney failure, hyperparathyroidism, selected neoplasms, hypervitaminosis D

tests for calcium disorders
Ca2+ & PTH levels. Ca2+ (total or i): establish Ca D/O. iCa2+: best screening test for Ca D/O. avoid oxalate, citrate, or EDTA (anticoagulant) due to chelating effect (falsely low). albumin, vit D, PTHrP, urea/creatine, alkaline phosphatase, phosphorus & magnesium
PTH measurement
use to determine cause of Ca D/O. specimen type: serum or plasma (green). immunoassay, best method uses Abs that detect both active amino end & intact PTH
low PTH in hypocalcemia
indicative of primary hypoparathyroidism
high PTH in hypocalcemia
indicative of secondary hyperparathyroidism (pseudo-hypoparathyroidism, vit D deficiency, or renal failure)
high PTH in hypercalcemia
indicative of primary hyperparathyroidism
low PTH in hypercalcemia
indicative of secondary hypoparathyroidism (malignancy or vit D intoxication)
albumin test for Ca D/Os
to distinguish true hypo-/hypercalcemia
vitamin D test for Ca D/O
to evaluate hypo-/hypercalcemia & renal failure. serum or plasma (EDTA). method: LC-MS/MS or immunoassay
PTHrP test for Ca D/O
to evaluate hypercalcemia a/w malignancy. method: immunoassay
urea/creatine test for Ca D/O
to assess renal function
alkaline phosphatase test for Ca D/O
to detect high bone turn-over
phosphate
79% in bone, 20% in ICF, <1% in plasma. exists in 3 forms: free form (80%) is active form. bone formation, energy, DNA/RNA synthesis, coenzymes, Hgb function, structure, buffering. plasma concentration controlled by 2 hormones: vit D & PTH
how does vit D affect plasma [PO4]?
increases it by increasing its GI absorption & bone resorption.
how does PTH affect plasma [PO4]?
decreases it by increasing renal phosphate excretion (while increasing reabsorption of Ca2+). plasma [PO4] tends to be inversely proportional to [Ca2+] (PTH action in kidney & tendency to precipitate)
hypophosphatemia
less common but more damaging. 30% mortality w/ severe (PO4 < 1mg/dL). affects neuromuscular, muscular, immune system, bone, & CNS.

causes of hypophosphatemia
low GI intake: vit D deficiency (rickets), oral phsophate binders (Ca- antacids), malabsorption (celiac). high renal loss: primary hyperparathyroidism, Fanconi’s (renal tube D/O). high cellular uptake: redistribution w/ insulin or glucose therapy, re-feeding after starvation. multiple causes: chronic alcoholism
hyperphosphatemia
typically asymptomatic. soft tissue calcification: Ca-phosphate precipitation, result in hypocalcemia & high PTH (secondary hyperparahyroidism). tetany: tonic spasm of muscles, from hypocalcemia b/c of calcification

causes of hyperphosphatemia
vitamin D intoxication. low renal excretion (high retention): renal insufficiency/renal failure (common in dialysis), hypoparathyroidism or pseduohypoparathyroidism. cellular release: diseases w/ high cell turnover (ALL). artifactual: hemolysis (phosphate is main intracellular anion)
tests for phosphate disorders
phosphate: serum/plasma (heparin), avoid hemolysis, separate serum/plasma from cells ASAP, urine, spectrophotometry method. Ca2+, urea/creatine (kidney function), Mg2+, PTH, vit D
magnesium
exists in 3 forms in plasma: free ionized (55%) is active form. major cofactor/activator for many enzymes. required for neuromuscular function, controlling heart rhythm. regulates ATPase ion pumps. component of bone. required for synthesis & secretion of PTH
how is magnesium regulated?
renal control (main). Ca2+ & P: hypercalcemia & hypophosphatemia dec renal Mg2+ reabsorption, promotes urinary loss. PTH: inc renal Mg2+ reabsorption in deficiency states, prevents urinary loss (major). GI absorption in small intestine, PTH enhances
hypomagnesemia
more common. common in critically ill patients, poor prognosis. caused by low intake (malnutrition, seen in alcoholics), redistribution of extracellular Mg to intracellular, high renal loss (primarily drugs, many include diuretics).
signs & symptoms of hypomagnesemia
like those seen in hypocalcemia (largely due to the role Mg plays in neuromuscular function). neuromuscular: tetany (Ca2+ normal). cardiovascular: cardiac arrhythmia. muscle: weakness. bone: osteoporosis
hypermagnesemia
depression of neuromuscular system: respiratory paralysis. cardiac arrest when > 10meg/L. caused by low excretion (renal failure, most common), high intake of Mg2+ (medications like excess antacid or laxative intake)
tests for magnesium disorders
Mg2+: serum/heparin plasma, fasting preferred, avoid hemolysis (oxalate, citrate, ETDA), separate ASAP, urine. Ca2+, urea/creatine
metabolic bone diseases
abnormal bone mineralization caused by mineral or vitamin deficiencies (Ca2+, PO4, or vit D) that result in abnormal bone mass or structure. disorders a/w vit D deficiency. disorders related to bone Ca loss. paget
disorders associated with vitamin D deficiency
low Ca & PO4 → high PTH. rickets (children): deformed bones. osteomalacia (adults): soft bones
disorders related to bone Ca loss
normal Ca & PO4. osteoporosis
paget
may have genetic component. imbalance bone remodeling → abnormally large, dense, weak bones
osteoporosis
normal Ca & PO4. causes: hereditary tendency (white, asian women), lifestyle (lack of exercise, poor diet, lack of sun), medications (steroids, etc), diseases (Cushing’s, hyperthyroidism, etc). treated with Ca & vit D supplements, drugs to inhibit bone resorption