10-11. electrolyte transport, hindgut function, mechanisms of diarrhea
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
what is the main driver of intestinal fluid and electrolyte absorption?
sodium
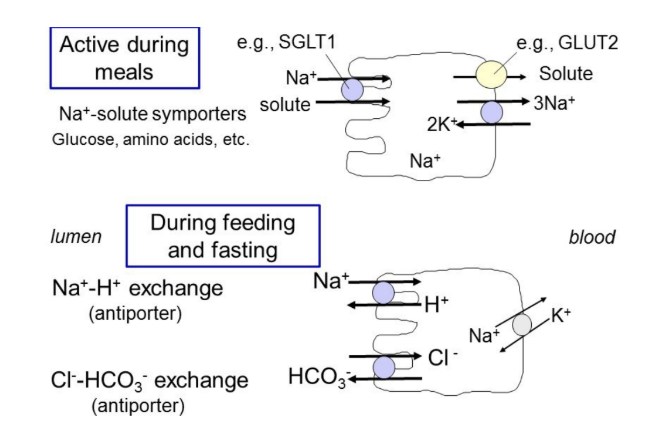
what are the two main mechanisms for Na+ absorption in the small intestine?
nutrient-coupled Na+ absorption → Na+-solute symporters
active during meals → transports products of digestion (glucose, amino acids, etc.) into cell with Na+
Na+-H+ antiporter
active between meals/during fasting
how does water get absorbed?
water flows osmotically (follows solutes) across the epithelium secondary to nutrient and electrolyte absorption, primarily through paracellular spaces → capillaries
how is K+ absorbed?
absorbed via solvent drag
K+ dissolved in H2O → goes with H2O, also through paracellular spaces between epithelial cells
why is it important to maintain appropriate fluidity of the intestinal lumen?
crucial for efficient digestion
needed for mucus protective layer
mucin + H2O → mucus
how does the mucus barrier differ between the small and large intestine?
small intestine: single layer of mucus
colon: 2 layers of mucus → more bacteria, high protection
what is the main driver for intestinal fluid and electrolyte secretion?
chloride
active Cl- secretion then drives movement of Na+ (and other electrolytes) and H2O in the lumen, primarily through the paracellular pathway
what are two types of Cl- channels found in the small intestine/colon?
CFTR → opens in response to increases in intracellular signaling molecules cAMP or cGMP
can also secrete HCO3-
calcium-activated Cl- channels → sensitive to intracellular calcium levels
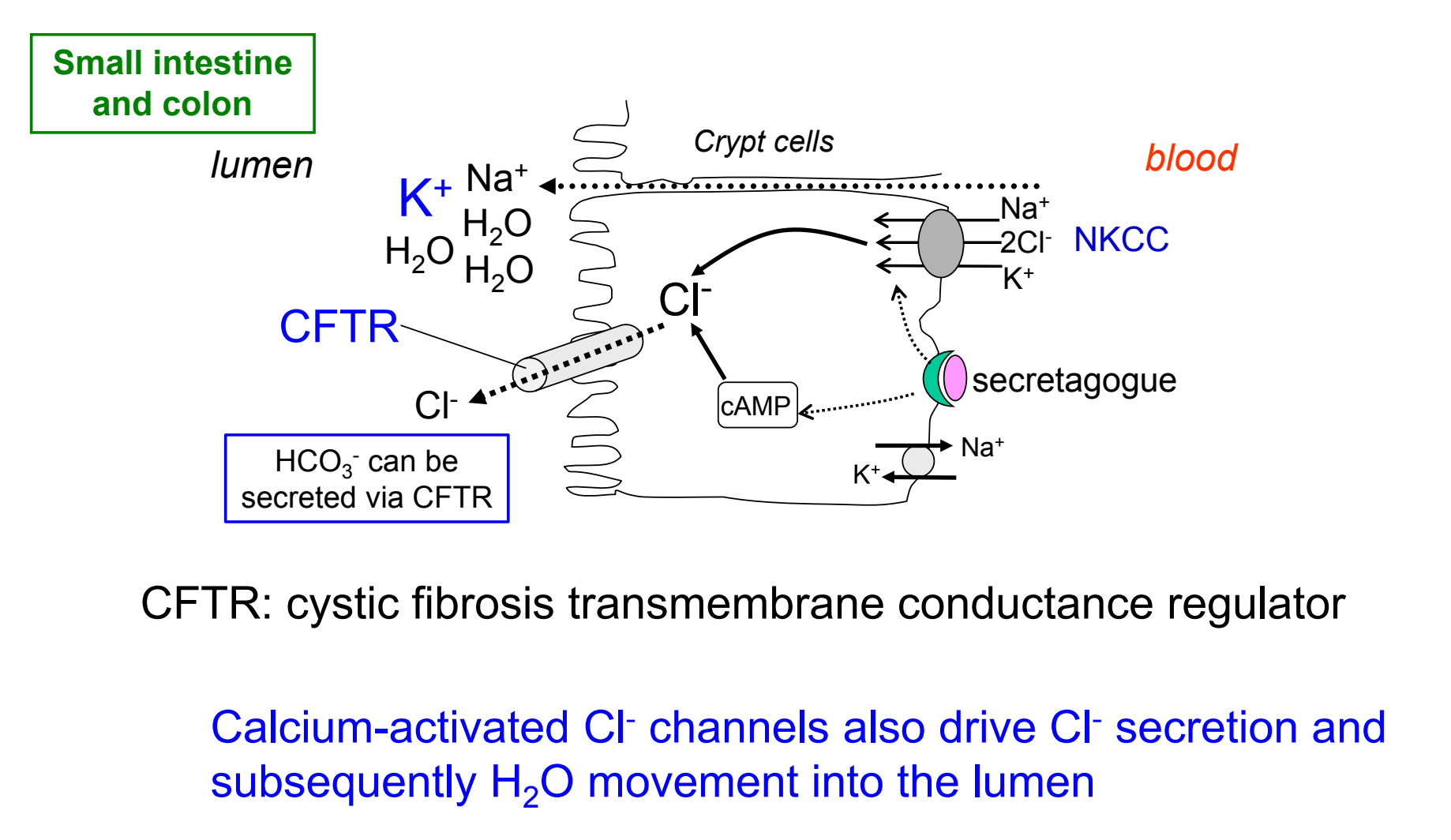
how is chloride secretion regulated?
a variety of chloride secretagogues (neurotransmitters, hormones, paracrine agents, etc.) stimulate chloride secretion
functions of the hindgut
digest & absorb components that cannot be processed more proximally (fiber)
reabsorb much of the fluid that was used during movement of material through GI tract
engage in motility reflexes; store waste products until elimination from body
support unique ecosystem of resident symbiotic bacteria
what are the 3 mechanisms of Na+ absorption in the hindgut?
Na+-H+ antiporter
Na+- short chain fatty acid coupled transport by SMCT1 (aka SCFA transporter)
Na+ channels regulated by neurotransmitters & hormones
aldosterone stimulates Na+ channels when Na+ intake is low
high amplitude propagating contractions
contractions in the colon that are designed to clear the colon of its contents
associated with defecation but does not necessarily result in the defecation reflex
gastrocolic reflex
prepares distal segments for entry of meal
gastric distention triggers a long reflex arc that results in increased colonic motility → evacuation of colonic contents to make room for incoming meal
defecation reflex
rectal volume threshold capacity exceeded
activation of stretch receptors in rectal wall can result in either:
voluntary inhibition of defecation (only up to certain limit) → increasing tone of external anal sphincter; transient increase in internal anal sphincter tone
high amplitude contractions of rectum/distal colon + contraction of abdominal muscles → relaxation of internal & external anal sphincters → defecation
what are the clinical signs of small intestine diarrhea?
large volumes (due to high secretion in the small intestine)
normal urgency
melena (digested blood)
no mucous
weight loss (most nutrient absorption)
what are the clinical signs of large intestine diarrhea?
small volumes
urgency → defecation reflex
frank blood
mucous (2 layers of mucus in large intestine)
weight generally unchanged
mechanism of osmotic diarrhea
reduced digestion/absorption of nutrients
ingestion of large quantities of non-digestible/non-absorbable substances
damaged villi
infection
exocrine pancreatic insufficiency (reduced output of pancreatic enzymes)
water is retained or moves into intestinal lumen
mechanisms of secretory diarrhea
increased secretion of fluid and electrolytes
increased crypt cell secretion results in SI losses
induced by secretagogue/receptor interactions at the apical or basolateral membranes of the intestinal epithelial cells
mechanisms of altered permeability
breakdown of absorptive barrier
infectious/inflammatory
inflammatory/idiopathic protein losing enteropathy
increased GI secretions
cytokine release
altered NaCl absorption in small intestine
mechanisms of motility disorders
reduced segmental contractions → decreases mixing with digestive enzymes and contact with mucosa
decreased residence time (nutrients/water moving too fast to absorb)