Midterm Exam
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
106 Terms
Rete Pegs
Provide strength to our skin so its harder to have wounds form
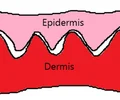
Between the epidermis and the dermis
Where are rete pegs found?
They flatten out as we age causing less skin integrity
How does aging effect the rete pegs?
Causes of Pressure Injuries
-Shear (friction with pressure)
-Moisture alters resiliency of skin
-Decreased blood flow
-Decreased blood pressure
-Psychiatric status (Can’t change positions on their own)
-Smoking (Constricts blood vessels)
-Decreased O2 perfusion
Effects of Aging that Promote Pressure Injuries
-Flattening of rete pegs
-Decreased dermal thickness
-Decreased epidermal turnover
-Decreased surface barrier function
-Decreased subcutaneous fat
Pressure Injury Stage 1
-Intact skin with non-blanchable redness of a localized area. (Usually over a bony prominence
->Dark pigmented skin individuals might not demonstrate blanching
Non-blanchable
Skin doesn’t go white when pressure is applied
Pressure Injury Stage 2
-Partial thickness loss of dermis presenting as a shallow open ulcer with a red/pink wound bed without slough
-May also present as an intact or open/ruptured serum-filled or serosanguinous filled blister
-Presents as a shiny or dry shallow ulcer without slough or bruising
-Does not have necrotic tissue at this stage
Pressure Injury Stage 3
-Full thickness tissue loss
-Subcutaneous fat may be visible but bone, tendon, or muscle are not
-Bone/tendon are not directly palpable
-Can have undermining or tunneling
-Can have necrotic tissue
Pressure Injury Stage 4
-Full thickness tissue loss with exposed bone, tendon, or muscle
-Exposed bone/muscle is visible OR directly palpable
-Can have undermining or tunneling
-Can have necrotic tissue
Common Locations for Pressure Injuries
-Scapula
-Iliac crest
-Greater trochanter
-Sacrum
-Ischium
-Lateral malleolus
-Heel
-Lateral edge of foot
Deep Tissue Pressure Injury
-Deep or prolonged pressure or shear injuring muscle and deep tissues
-Non-blanching deep red, maroon, or purple discoloration
-Can demonstrate blood filled blister
Kennedy Terminal Ulcer
-Sudden onset
-Coccygeal area or gluteal fold
-Mirror image, either pear or butterfly shape
-Red, yellow, or black skin progresses quickly to eschar
-It is a precursor to multi-organ failure and death within 2-3 weeks
Diabetic/Neuropathic Wounds
-Tend to be located on the plantar foot or places of abnormal shoe wear/weight bearing surface
-Etiology can arise from foreign objects
Venous Wounds
-Large amount of edema and exudate
-Often minimal pain (Pain is reduced with elevation)
-Poorly defined wound border
-Pulses are present
-Insidious onset
-Need compression to heal
-Hemosiderin staining present
Lower leg proximal to the medial malleolus (Gaiter Area)
Where are venous wounds usually found?
Hemosiderin Staining
Red blood cells leak into the interstitial space and release iron
Arterial Wounds
-Tend to be distal/anterior/lateral toes/feet but can be more proximal starting by a mild injury
-Painful (Pain worse with elevation)
-Often a well defined border/Punched out look
-Pale
-Minimal drainage
-Faint or absent pulses
-Surrounding skin rubor
Superficial Thickness Wound
Only the epidermis is damaged
Partial Thickness Wound
Goes into the dermis but not all the way through
Full Thickness Wound
Goes through the dermis and into the subcutaneous tissue
Inflammatory Stage Clinical Presentation
-Erythema
-Edema
-Heat
-Pain
-Necrotic tissue
-Exudate
Puss looking
Thick with extra materials
Not necessarily a foul/infection odor
Proliferative Stage Clinical Presentation
-Granulation tissue (Beefy red colored angiogenesis)
-Wound contraction
-Epithelialization (Keratinocyte migration)
-Minimal transudate (Serous/serosanguinous fluid)
Complete epithelialization of the wound
When does the proliferative stage end?
Maturation Stage Clinical Presentation
-Scar size decreases
-Red color fades
When red color is all gone
When does the maturation stage end?
Sensory Neuropathy
Decreased or absent pain/sensation
Motor Neuropathy
Weakened intrinsic foot muscles, imbalance between toe flexors and extensors
Autonomic Neuropathy
-Reduced sweating causing dryness of feet
-Reduced control over vasoconstriction causing increased rate of blood flow which overwhelms the circulatory system resulting in extra connections between large arterial and venous vessels
Matrix Metalloproteases
-Break down surrounding tissue
-Cleans debris out of wounds
During inflammatory phase
When are matrix metalloproteases beneficial?
NERDS (Superficial Critical Colonization)
-Non-healing
-Exudate increases
-Red and bleeding
-Debris
-Smell
STONEES (Deep Critical Colonization)
-Size is bigger
-Temperature increases
-Os (Probe to bone or exposed bone)
-New breakdown
-Exudate increases
-Erythema, Edema
-Smell
S/S of Infection
-Induration
-Fever/heat
-Erythema
-Edema
Pseudomonas
-Blue-green exudate and appearance to wound
-”Sweet” smell
-Commonly treated with topical antimicrobial, Sulfamylon
Maceration
-Softening or dissolution of tissue after lengthy exposure to fluid
-Pruney, wrinkly appearence
-Caused by wound being too wet
Compression for venous wounds
-Reduces risk of DVTs
-ACE wrap not a good candidate for venous wounds since it is a “long stretch” wrap
-Short stretch bandages are inelastic for 30-40 mmHg pressure and are great for venous wounds
-Multilayer wraps
Ankle Brachial Index (ABI)
-Systolic BP at ankle/Systolic BP at brachial artery
-Need a venous doppler
-Value >1 is normal or venous disease
-0.8-1 some arterial involvement
-<0.8 = arterial involvement, do not compress
-<0.5 = urgent referral to vascular surgeon
Charcot Joint
-9% of diabetics
-Remodeling
-Rocker-Bottom foot
Inflammation
-Erythema
-Edema
-Pain
Deformity
-Subluxation of midfoot bones
UVC Indications
Infected or highly colonized wounds where traditional interventions are not working
UVC Contraindications
-Light sensitive disease such as SLE
-Current or PMH of melanoma or squamous cell carcinomas
-HIV
-Fever
-Radiation or deep XR therapy
UVC Application
-Skin sensitivity test to uninvolved skin for 15 secs. and observed for 24 hrs.
-Drape/protect periwound skin
-Therapist must wear protective eye wear and have patient cover eyes
-Protocols vary from 30 secs. to 2.5 minutes
-Flush wound to wash
Effectiveness of UVC
-Combating a developing surface infection,
-Infected wounds where poor circulation reduces the effectiveness of systemic antibiotics
-Replacing topical antibiotics
-Treating antibiotic resistant species such as MRSA
-5 daily treatments should begin to show infection improvement
Extended Spectrum Beta-Lactamase
-Causes hydrolysis of many antibiotics
-Can produce carbapenemase
Levine Technique
-Cleanse the wound first
-Hold the culturette tube in one hand and remove the cap and applicator with other hand
-Apply gentle pressure and swab wound gently to obtain a sample of drainage on applicatory
-Do not culture purulent or necrotic debris or drainage over hard eschar
-Roll the tip of the applicator completely over in a one centimeter square area for 5 seconds
-Return applicator to culture tube without contaminating the applicator or outside of container
-Apply cap
-Break the liquid capsule at the bottom of the culture tube if present
-Make sure the culture medium surrounds the swab
Ultrasound Treatment Settings
-20% duty cycle
-3 MHz frequency
-<0.5 watts per square cm for intensity
-Treatment time is 1-2 minutes 2-3 times per day 3 times a week
Gauze Dressings
-Thick with significant absorption ability
-Tends to dry out wound (No moisture retention)
-Used for maximal exudate where frequent dressing changes are required and maceration is not a problem
Transparent Films
-No ability to add or absorb moisture
-Use as a primary dressing over negligible or non-draining wounds to hold in moisture
-Impermeable to liquids and bacteria but permeable to gases
-Can help maintain moisture in superficial wounds or as a secondary dressing on deeper wounds
Hydrocolloid
-Maintain tissue moisture but have a moderate absorption ability
-Slow rate of moisture absorption
-Use with minimal to moderate draining wounds changing towards minimal drainage
-Often used as a secondary dressing
-Allow 2-3 days between dressing changes depending on exudate levels
Foam
-Moderate to max moisture absorption but must be over a relatively shallow wound
-Cannot be easily packed in undermining or tunneling due to the “memory” of it that does not conform to the shape of the new wound space
-Some are designed to conform to undermining and tunneling, however, some spread moisture out to the edges of the foam and macerate surrounding tissues if not cut to the specific wound dimensions
Calcium Alginate
-Used with maximally exudating/maximally draining wounds
-Used as sheets for more shallow wounds or rope for wound filling/packing
-Can dry a wound out that does not have significant drainage
Hydrogel/Hydrogel Infused Dressing
-Provide moisture to a dry wound
-Can help hydrate necrotic tissue to facilitate autolytic debridement
-Can cause wound maceration if too much moisture
-Use for dry wounds or to hydrate dry necrotic tissue
Collagen Dressing
-Absorbs exudate
-Acts primarily as a matrix on which granulation tissue can grow
-Can distract excess MMPs to attack the dressing instead of the growing granulation tissue
Collagen-Oxidized Regenerated Cellulose
-Binds MMPs and renders them inactive bringing MMP levels back down to normal levels in chronic wounds to allow granulation tissue to grow and epithelialization
-It is believed this destroys the 3-dimensional shape of the MMPs so they can not bind to any other cells or chemicals
-Use in chronic wounds where high levels of MMPs are suspected of slowing or stagnating wound healing
Copper Oxide Impregnated Dressing
-Increases angiogenesis by increasing vascular endothelial growth factor
-Increased expression of integrins
Stimulates:
Extracellular matrix
Basement membrane
Cell adhesions
Growth factors
-Increased activity of copper dependent enzymes for matrix remodeling, cell proliferation, and re-epithelialization
-Can eliminate Gram positive and Gram negative bacteria, viruses and fungi
Composite Dressing
-Contact layer of primary dressing with a secondary dressing component
EX: Collagen with a hydrocolloid
-Some additions for odor such as activated charcoal or additions for pain such as silicone contact layers covering absorptive foams
Honey Dressing
-Promoted to decreased pH and increase osmotic flow of fluids to help autolytic debridement
-Draws water out of bacterial cells slowing their reproduction
-Transparent films
-Hydrocolloids
What dressings are used for moisture maintenance?
-Foams
-Hydrocolloids
-Alginates
What dressings are used for moisture absorption?
Hydrogels
What dressings are used for moisture addition?
-Silver containing dressings
-Copper oxide dressings
-Iodine containing dressings
What dressings are used to reduce bacterial levels?
-Collagen
-Collagen ORC dressings
What dressings are used to reduce protease levels?
Activated Charcoal
What is used to reduce odor?
Silicone Dressings
What dressings are used to reduce pain?
Barrier Cream
-Protects skin from continued exposure to feces, urine, or both
-Usually contains high level of zinc oxide
-Will not wash away after repeated exposure to urine and feces
-Contains Karaya to absorb moisture and adhere to weepy, macerated skin
-Some are fragrance free (No alcohol, for reduced irritation)
-Those with a higher petrolatum base can be clear so that you can see through the ointment
Good Goals
-Wound area will decrease from _____ cm3 to ______ cm3 in order to… (Promote wound closure OR Decrease risk of future infections)
-Wound tunneling will decrease from _____ cm to _____ cm…
-Wound undermining…
-Pt will independently instruct caregiver how to reposition pt from supine to sidelying
-Pt will demo 2+/5 general bilateral LE strength to promote more independence with bed mobility and self-repositioning
Child Abuse Signs
-Bruise on ear, likely a hit on the head
-Burn older than history given
-Parent story does not match burn
-Parent story does not match child developmental abilities
-Immersion burn gives spared areas
Total Body Surface Area (TBSA)
-Head = 9%
-Trunk = 18% for each side
-Arms = 9% each
-Legs = 18% each
-Genitalia = 1%
Cutaneous Functional Units
-The entire surface of skin recruited for full movement of a joint
-Adjacent joint positions impact the amount of skin recruited
-Normal skin has 50% extensibility
->Burn scar only 15%
->Mature burn scar only 5%
-Always stretch the joint distal to the burned skin
Proper Positioning of Burn Patients
-Use crucified position if possible
-Splints are helpful
-Microstomia devices
-Tongue depressors for stretching vertical mouth
Escharotomy
-Operation where an opening is made into an area of skin that is thickened and tightened after a severe burn
-Used to cut through dead tissue to get to the lungs to assist with breathing or to help with circulation in the extremities
Integra
-A dermis substitute made of bovine collagen and glycosaminoglycan
-Has an outer silicone layer that functions like epidermis until ready for skin graft
Integra Precautions
-Must wait 5-6 days prior to ROM
-Prior to grafting over this the physician will wait until adequate dermal growth is seen by capillary growth
Ectropion
Outward turning of the eyelids due to a facial burn
Excising and grafting the wound early
How do you prevent ectropion?
Role of PT in Hospital
-Get patient to the next step in recovery process (We determine where the patient goes next)
-Communicate with other healthcare staff, families of patients, and patients themselves
-Mobilizing patient ASAP (Function, function, function)
Donning PPE
Put on gown
Put on mask
Put on goggles/face shield
Put on gloves
Doffing PPE
Take off gloves
Take off gown
Wash hands!!
Take off goggles/face shield
Take off mask
Wash hands!!!!
Standard Precautions
-Clean hands
-Clean equipment
-PPE when in contact with body fluids
-Practice cough etiquette
Contact Precautions
-Clean hands
-Gown
-Gloves
Droplet Precautions
-Includes standard precautions
-Mask
-Face shield OR goggles
Novel Respiratory Precautions
-Includes standard precautions
-Gown
-Gloves
-N95 and Face shield OR PAPR
Airborne Precautions
-Includes standard precautions
-Keep door shut
-N95 or higher level respiratory
Prehab for TKA
-Strengthening quads for quicker recovery
-Focus is strengthening, ROM, and expectations following surgery
-Same exercises as post-surgery (Heel slides, quad sets, TKEs, SLRs, knee extension, knee ROM in sitting)
-Patient education on postoperative expectations
-Discussing and instructing in use of planned postoperative ADs (Walker or crutches)
-Addressing home environmental barriers that may impede independent mobility post-discharge
Prehab for THA
-AROM exercises to involved hip as tolerated
-Strengthening exercises focusing on hip and knee extensors and hip abductors such as:
Quads sets
Glute sets
Heel slides
Hip abduction
Ankle pumps
-Patient education on postoperative epectations
-Discussing and instructing in use of planned postoperative ADs (Walker or crutches)
-Addressing home environmental barriers that may impede independent mobility post-discharge
Mental Function Outcome Measures
-Orientation
-DeJonghe’s 5 orders
-RASS
-GCS
-CAM-ICU/pCAM-ICU
-MMSE
-MoCA
Integumentary Integrity Outcome Measures
-Edema Grading Scale
-Braden Scale
-Pressure ulcer scale for healing (PUSH)
Mobility Outcome Measures
-6 Clicks
-Acute care index of function (ACIF)
-Barthel index
-10 MWT
-FIM
-AlphaFIM
Aerobic Capacity/Endurance Outcome Measures
-6 MWT
-2 MWT
-2 MST
Muscle Performance Outcome Measures
-Hand held dynamometry
-5x STS
-MMT/MRC
-30 sec. Chair stand
Balance Outcome Measures
-Function in sitting test (FIST)
-Functional reach/Modified functional reach test
-Berg balance scale (BBS)
-Dynamic gait index (DGI)
-Timed up and go (TUG)
Interventions for TKA
-Weight bearing with an AD
-Surgeon protocol/preferences
-Minimize swelling and pain as a healthcare team
-Early mobility
Functional training (Transfers, gait with AD, stairs)
AROM (Initiate exercises)
Safety with ADs
-Breathing exercises with all post surgery patients
-Patient education
Interventions for TSA
-Physician protocol
-Sling
-Immobility
-PROM exercises of shoulder (Forward flexion and ER)
-Bed mobility and transfers
-Ice
Interventions for Spinal Fusion
Supine
-Heel slides
-TKEs
-Abduction/Adduction
-Ankle pumps
-UE flexion
-UE abduction/adduction
-UE IR/ER
-Diaphragmatic breathing
Goals for Acute Care
-Improve mobility (Functional activities required for daily living)
-Address equipment needs
-Patient education
-Caregiver training
-Discharge needs
Anterior Approach Hip Precautions
-No hip hyperextension
-No hip ER past neutral
Posterior Approach Hip Precautions
-No flexion past 90 degrees
-No adduction past neutral
-No IR past neutral
Global Approach Hip Precautions
-No Hip hyperextension
-No hip ER or IR past neutral
-No hip flexion past 90 degrees
-No adduction past neutral
Trochanteric Osteotomy Hip Precautions
-No active hip abduction
-Limited WB status (TDWB-PWB)
Discharge Home Independently or with Family Parameters
-Patient has returned to PLOF
-Patient is safe with transfers and mobility
-Patient has support from family or friends, OR patient can complete IADLs and ADLs independently
-May need some coordination with case manager for meals, transportation, other needs