CH24: Health Education and Promotion Theories
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Learning objectives
Explain the steps in a preventive program, identify the need to conduct preventive counseling, and describe the proper setting.
Describe the importance of partnering with the patient to come up with a plan for change.
Describe and explain the methods of motivational interviewing.
Describe how to recognize and explore the patient’s ambivalence and describe techniques to elicit and recognize change talk.
Understand and explain various plans to strengthen the patient’s commitment for change.
Models of health education
“Old” Model: Expert to Patient:
▪ Provider prescribed treatment
▪ Patient were expected to listen and absorb knowledge
▪ Paternalism/Prescriptive/Passive Model
Current Model: Provider and Patient as partners:
▪ Patient autonomy is important
▪ Active participant in decision making process
▪ Right and capability to control health outcomes
▪ Collaborative effort focused on empowerment
▪ Provider is an equal
▪ Teach the tools for success
Steps in a preventive program
ASSESS THE PATIENT’S NEEDS-dental biofilm index, discussion of risk factors, assess oral aids
PLAN FOR INTERVENTIONS
IMPLEMENT THE PLAN
PERFORM CLINICAL PREVENTIVE SERVICES-patient education before biofilm removal btw
EVALUATIVE PROGRESSIVE CHANGES-show and let them show you; can they do it efficiently?
PLAN SHORT & LONG-TERM CONTINUING CARE
Health literacy
▪ What the patient knows about maintaining health and/or improving-ask open ended questions and you will talk differently to a child, adult, and adult with special needs. What do you know about cavities?
▪ Health education meeting minimal standards for all school grade levels
▪ Need to understand information that maintains good health
▪ Need for health systems to reduce their complexity (“lay-terms
Principals of health
▪ Health is not defined as merely death or life but as a continuum.
▪ State of complete physical, mental, and social well-being that involves more than just the absence of disease
▪ Wellness scale-Continuum of health
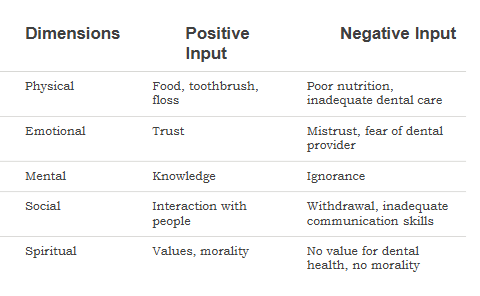
Five dimensional health model
interconnected
one change in one can affect the other
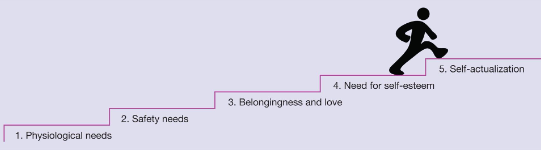
Maslow’s hierarchy of needs
if lower level basic needs aren’t met first, then higher needs cannot be fulfilled
know where the patient is when we start to motivate and counsel
Healthy behavior
an action that helps prevent disease and promotes health
Health education
the teaching of health behaviors that bring an individual to a state of health awareness
Health promotion
informing and motivating individuals to adopt healthy behaviors
Health education and promotion theories basics
▪ Health Belief Model
▪ Transtheoretical Model-Stages of Change
▪ Theory of Reasoned Action
▪ Social Learning Theory-Social Cognitive Theory
▪ Locus of Control
▪ Salutogenesis-Sense of Coherence
help define and categorize behavior (to predict behavior=predict outcomes of behavior)
meet the patients where they are
Health belief model basic info
▪ Developed in the 1950’s
▪ Implies people with better information make better choices
▪ Places high value on attitudes of the learner
▪ Recognizes the importance of the learner’s readiness to enact meaningful behavior
Framework for health behavior interventions
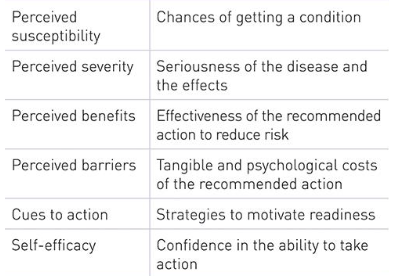
Health belief model (staged theory)
▪ 1. Must believe susceptible to the disease/condition
▪ 2. Must believe the condition is serious
▪ 3. Must believe the intervention/treatment options are successful
▪ 4. Must believe they can overcome all barriers to use the intervention
Patient must understand their susceptibility to disease and the seriousness behind the disease, they must believe the intervention options are successful, and that they can overcome behaviors
Health Belief model strengths and weaknesses
Strengths:
▪ Acknowledges patient values and attitudes towards health behaviors
▪ Involves patient in the process
Weaknesses:
▪ The predictive value of behavior is not constant
▪ Poor evidence due to research design
▪ Change in belief may not be powerful enough to change 9behavior/lifestyle
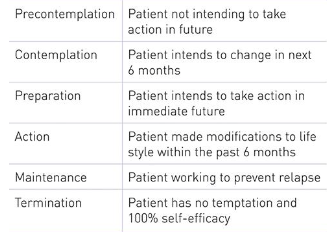
Transtheoretical theory (stages of changes)
▪ Based on a person/group’s readiness to adopt a new health behavior
▪ Stages represent distinct beliefs and levels of readiness
▪ Foundations for Motivational Interviewing
▪ Custom design an intervention to the stage based on the person
Included in the method:
▪ Assessment of learner behavior and attitude
▪ Methods to assess stages
▪ Method of helping learner progress through steps
People may skip, lapse, or stagnate in stages
▪ Goal: assist patient in identifying benefits of behavior change and overcome obstacles to achieve optimal health
Six stages of changes in the transtheoretical model
Implementation of health education models
Population specific techniques:
-kids, teens, adults, community, groups
Setting of the intervention dictates the implementation technique
Adult health education
Strongly influenced by experience and established habits:
•Autonomous in decisions making
•Self-directed in implementing a behavior
2 keys to successful education and adaptation of health behaviors:
•Must provide the relevance
•The change must be practical
Key steps in education
1. Determine the patient’s interests, attitudes, and current knowledge
2. Asses what the patient is ready to learn
3. Assess what information can be put to immediate use
Accomplished by:
▪ Observing the patient
▪ Conversations as review health history, dental history, and previous notes
▪ Gather as much information as possible
▪ During patient assessment
▪ History review, intra extra oral exam, periodontal probing,
How to motivate the patient: motivational interviewing
Patient centered counseling
• Resolves conflicts
• Eliminates ambivalence
Encouraging the patient to set personal goals as negotiated with the DH
Combines principles from:
• Adult education
• Readiness to learn
Motivational interviewing PACE
▪ Partnership
▪ Acceptance
▪ Compassion
▪ Evocation
Motivational interviewing: Partnership
Learners and providers are partners in the process
• Identify and prioritize a list of needs for the patient
Shared goal of improving oral health
• Takes multiple encounters
Patient:
• Identifying personal needs and concerns
• Identifying state of readiness
Provider
• Assessing the health condition
• Presenting effective interventions
Motivational interviewing: acceptance
Accepting what the patient brings, but doesn’t mean you have to approve of the patient’s actions
4 patient centered conditions that convey acceptance:
-absolute worth-honor and respect patient
-accurate empathy-be genuine
-autonomy support-support patient has the right to choose
-affirmation-patient can change
Motivational interviewing: compassion
Establishes trust and builds a relationship with the patient
Promoting the welfare and
prioritizing patient needs
Addressing the patient’s best interest and not the clinician’s agenda
Motivational interviewing: evocation
Commitment to elicit patients’ assessment of their own strengths, thoughts, ideas, and resources
Motivational interviewing key points
Motivation to change is initiated by the patient
It is the patient’s responsibility to determine conflict or ambivalence between different courses of action
Direct persuasion is not effective in changing behavior-just because we provide info, doesn’t patient will automatically change their behavior
Counseling style is quiet and encourages patient participation-motivation interviewing in a private environment, have patient seated up to discuss (eye to eye contact)
The provider must assist the patient in examining conflict or ambivalence
Readiness to change is constantly changing-so reassess in every appointment
The counseling relationship is a partnership
What not to do with motivational interviewing
Arguing that the patient has a problem in need of change
Offers direct advice without determining the patient’s interests in change-patient should ask for advice
Adopts a superior attitude to the patient
Provider does most of the talking
Labels the patient-don’t label patient as unwilling, don’t judge
Uses coercion-don’t keep asking when they made their decision
Motivational interviewing guiding principles
Resist Righting Reflex-normal to want to solve problems, but maintain collab approach
Understand the patient’s motivation-why the patient wants to change
Listen to the patient
Empower the patient
Motivational interviewing: implementation
Ask permission-patient asks you for advice, or you ask directly for permission. Can I share my oral cancer findings with you?
Elicit provide Elicit-asking for permission, explore patient’s prior knowledge, determining patient’ interest in the info. What do you know about using smokeless tobacco and the effect it has on your mouth?
Agenda setting-patient is given as much decision making freedom as possible. Provide list of topics and let them decide what topics they want to ask about first
Core skills:
Open-ended questions
Affirmations
Reflective listening
Summary-what you went over with patient
Questions to determine need
What concerns do you have about your mouth?
Tell me about your past experiences with dental treatment.
What methods have you used in the past to clean between your teeth?
What do you know about how to prevent gum (periodontal) disease?
Sustain talk vs. change talk
Sustain: patient is happy about current health-related behaviors
-Clinician can use MI techniques to determine what info the patient is interested in receiving
Change: prepping for changing behavior
-Clinician can move to reflect change talk and elicit a plan for change
Decision balance
▪ Balancing the benefits and cost of a behavior
Benefits:
▪ What can be gained
▪ Health, emotional and social gains
Cost:
▪ Obstacles
▪ Social pressure, addiction, disease, money, time
Allows the patient to see the benefits or risks/costs of their behavior.
What are the benefits of continued smoking? What are the risks? What are the benefits and risks of a change?
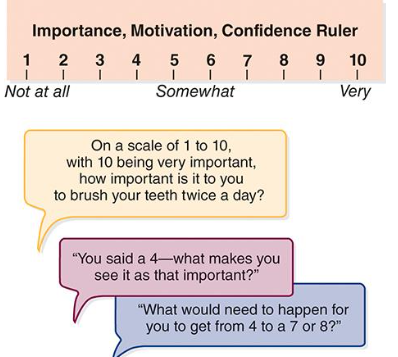
Readiness ruler
▪ Visual aid to allow the clinician to know the patient’s readiness for change
Summary
▪ Health education is complex and challenging
▪ Educational theory
▪ Implementing education strategies
▪ Motivational interviewing