Protozoans
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
What is protozoa? + some features (cell structure, how they eat)
The most diverse kingdom
Eukaryotic organisms
Unicellular (occasionally forming colonies/aggregate multi-nucleated cells)
Developed subcellular features like membranes and organelles instead of specialised cells like in multicellular organisms
Many have animal-like cell membranes, plant-like cell walls & can be covered in pellicle (skin)
Can be heterotophs and ingest food by phagocytosis (eat bacteria), or are photoautotrophs & store energy through photosynthesis
How to diagnose?
Nuclear structure
Size (1-150um or <50um for parasitic)
Cytoplasmic inclusions - Coalesced RNA, RBC, Food vacuoles w/bacteria, yeast
Appearance of cytoplasm - smooth/clean or vacuolated
Type of motility - directional/non-directional, sluggish/fast
Nuclear structure
Chromatin (Nuclea rDNA)
Karyosome (Small mass of chromatin)
Peripheral Chromatin (adheres to nuclear membrane)
Nuclear Membrane (Surrounds all nuclear material)
Chromatoid body/bar with coalesced RNA in cytoplasm of the cyst stage.
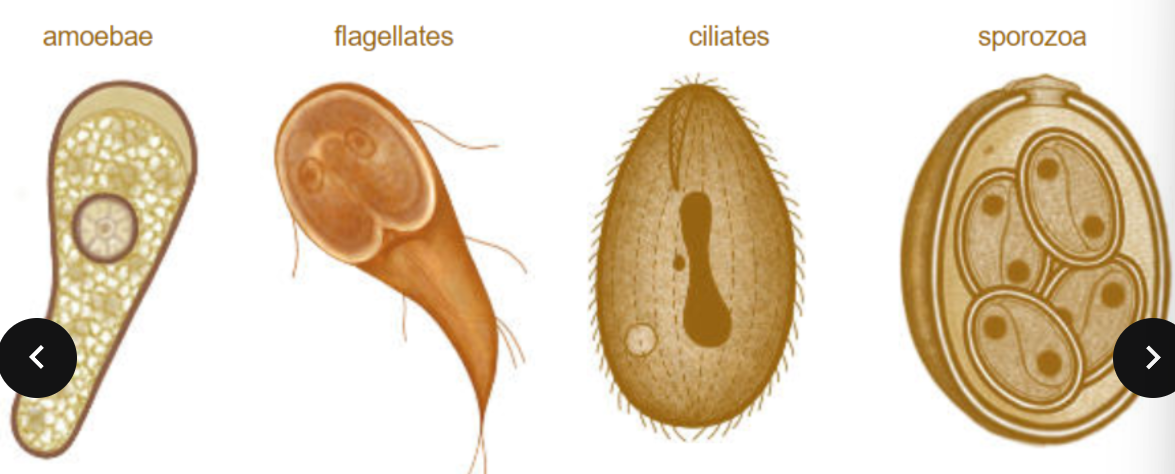
Types of Protozoa
Four subdivisions according to methods of locomotion
Amoebae (creep/crawl over solid substrates)
Flagellates (use elongated flagella which undulate to propel the cell through liquid)
Ciliates (Use numerous cilia to undulate in synchronised waves— swimming thru fluids)
Sporozoans (form non-motile spores as transmission stages) - parasites.
Life cycles of protozoa + Reproduction
Protozoa have short generation times, rapid, development and reproduce in large numbers by asexual or sexual processes.
Asexual division - fission/splitting or internal/endogenous budding.
Sexual reproduction - formation of gametes and fertilization to form zygote, or unique process conjugation where ciliates exchange micronuclei.
Protozoan developmental stages within hosts
Trophozoites - the motile feeding stage (intracellular/extracellular) Not resitant to external environmental conditions and don’t survive very long outside their hosts.
Cyst - Inactive and non-motile infective stages, survives in the environment w/ a cyst wall. Do not multiply but organisms can divide within the cyst wall.
How to transmit protozoans?
Transmission - mostly person-to-person, via faecal-oral route, faecally contaminated food or water, insect bites/faeces or sexual transmission
Does disease happen with infection. + Hosts
Protozoan infections are parasitic disease.
Host types:
Definitive Host — supports the adult or sexually reproductive form of a parasite
Intermediate host — supports the immature or non-reproductive forms of a parasite.
The amoebae (intestinal protozoa) general life cycle
The definitive host ingests the infective cyst stage from fecal contamination in environment
The cyst passes into the small intestine and excystation occurs with transformation to the trophozite stage
Trophozites colonise the host, multiplying asexually via binary fission. They can remain near the lumen (non-pathogens) or invade the wall of the intestine and multiple (pathogens)
Cysts and trophozites are passed in the feces of the infected host.
Intestinal protozoa - the amoebae E. Histolytica (epidemiology, pathology & clinical, infection, distribution)
Epidemiology - Occurs worldwide (especially in areas with poor sanitation or tropical/sub-tropical areas)
Pathology & Clinical Manifestation - The most pathogenic of all (causes amoebic dysentery) can become extra-intestinal or be fatal. Hepatic abscess (pus filled mass in liver) is the most common & dangerous complication)
Chronic infections can last for years
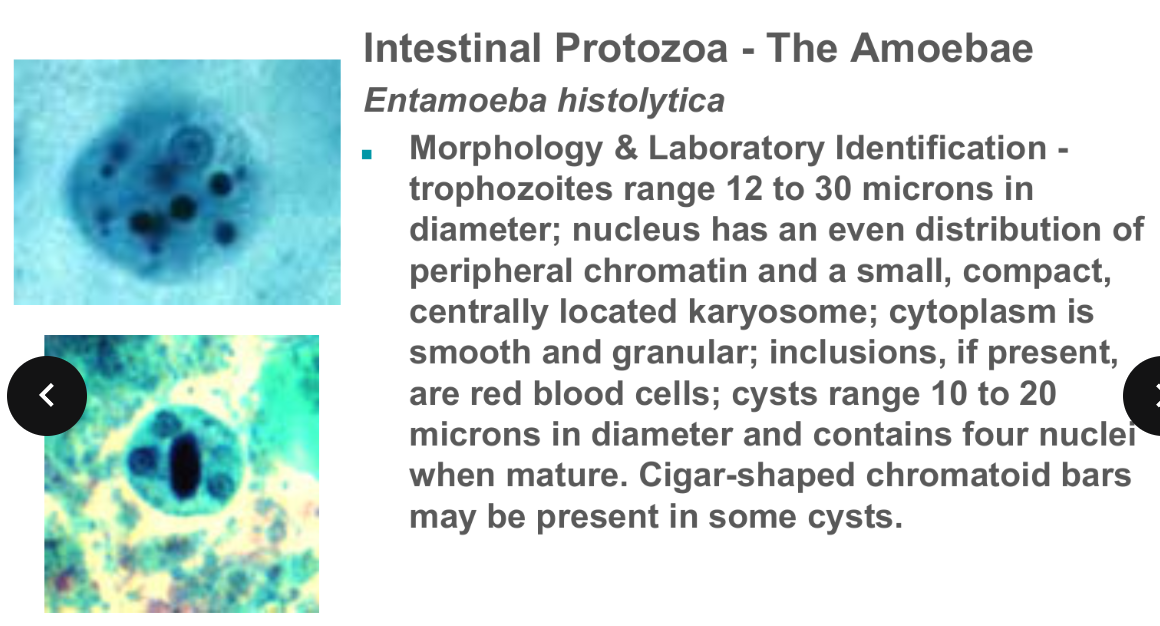
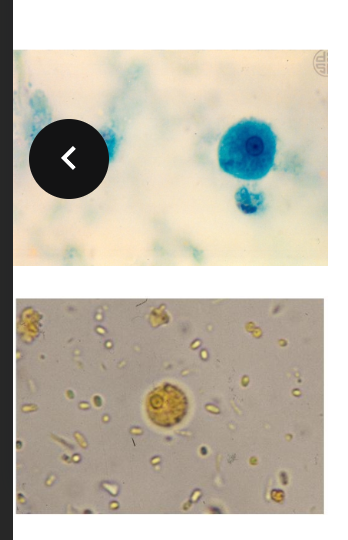
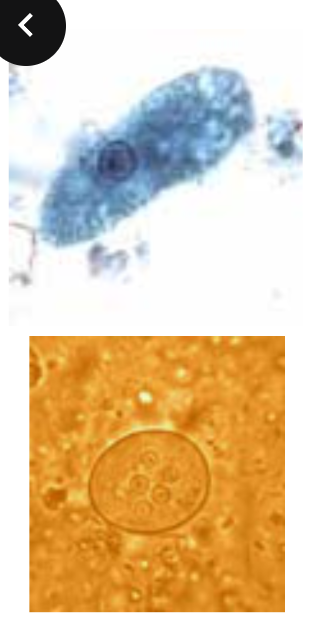
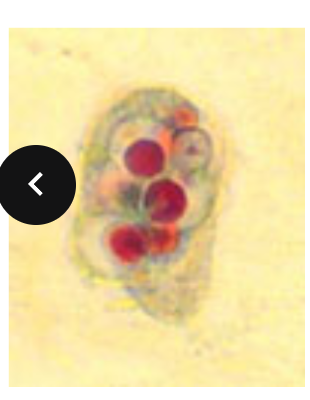
Amoebae morphology/labratory identification E. Histolytica
Amoebae epidemiology of E. Hartmanni & Morphology/Lab identification
Epidemiology - similar to E. histolytica.
E. Hartmanni is non-pathogenic unlike E. Histolytica
Difference lies in the sizes of the respective organisms. Trophozoites measure less than 12 microns, while cysts will measure less than 10 microns.
Amoebae E.coli significance and morphology
Harmless commensal (symbiotic), must be differentiated from pathogens. Morphology - Trophozoites are 10-35 microns, Cysts 10-30 (w/ 8-16 nuclei). Nucleus exhibits and eccentric karyosome with irregular coarse chromatin. Cytoplasm is vacuolated, w/ yeast, bacteria and debris.
Amoebae E. Gingivalis (Infective site, transmission, morphology)
Infective site - mouth (thrives in diseased gums) - destroyed in stomach when swallowed
Transmission - contact with fomites (drinking glasses, utensils, kissing)
Morphology - resembles E. histolytica (but has no cyst stage) ingests leucocytes (blood cell)
Amoebae E. Nana (Occurence, Pathogenicity, Morphology)
Occurence - occurs in 21% of worldwide population
Non pathogenic.
Morphology - Trophozoites 5-10 microns. Nucleus has a large & blot like karyosome. Little to no peripheral chromatin. Cysts are sub-oval with 4-6 by 6-10 microns.
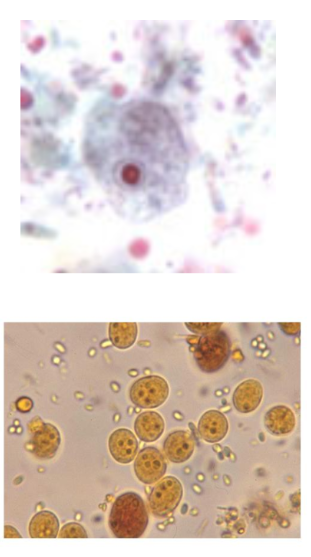
Amoebae I. Butschlii (Pathogenicity & Morphology)
Pathogenicity - None
Morphology - Iodine cyst (large glycogen vacuole which stains dark brown with iodine)
Tissue dwelling amoebae N. Fowleri (Classification, Symptoms, Diagnosis & Life cycle)
Classification - an ameboflagellate (free-living organism alternating between amoeboid and flagellated forms; only the amoeboid form is found in tissues)
Life cycle - the amoebae gains entry via the nasal mucosa, usually during swimming. (moves along the olfactory nerve and gains access to the brain) Cases are invariably fatal- do not spread from person-to-person.
Symptoms - Dramatic and rapidly progressive. Headache, fever, nausea & vomiting 1-2 days. Meningoencephalitis, irrational behaviour, coma & death occur within 9 days of exposure.
Diagnosis - made at autopsy.
Tissue Dwelling Amoebae Acanthamoeba spp. (Life cycle, Symptoms, Common infections)
Life cycle - Free-living amoeba which reaches the brain hematogenously after entering wound/lesion on skin. COmmonly associated with getting into eyes via contaminated/homemade cleaning solutions.
Symptoms - slow onset (10 or more days). Presents as chronic granulomatous lesions in brain. In eye lesions, the infection resembles a herpes virus infection.
Acanthamoeba Keratitis (infection associated with extended-wear contact lenses)
Flagellates (where do they inhabit, morphological characteristics)
Inhabit the mouth, bloodstream, gastrointestinal or urogenital tracts.
Morphological Characteristics
Flagellum(ae) - organelles of locomotion; an extension of ectoplasm; moves with a whip-like motion.
Axostyle - a supporting mechanism, a rod-shaped structure; not all flagellates have these.
Undulating membrane - a protoplasmic membrane with a flagellar rim extending out like a fin along the outer edge of the body of some flagellates.
Costa - a thin, firm rod-like structure running along the base of the undulating membrane.
Cytosome - a rudimentary mouth; also referred to as a gullet.
What do you identify glagellates based on?
Size
Shape
Motility
Number & morphology of nuclei
Number & location of flagellae
Location in the body of the host.
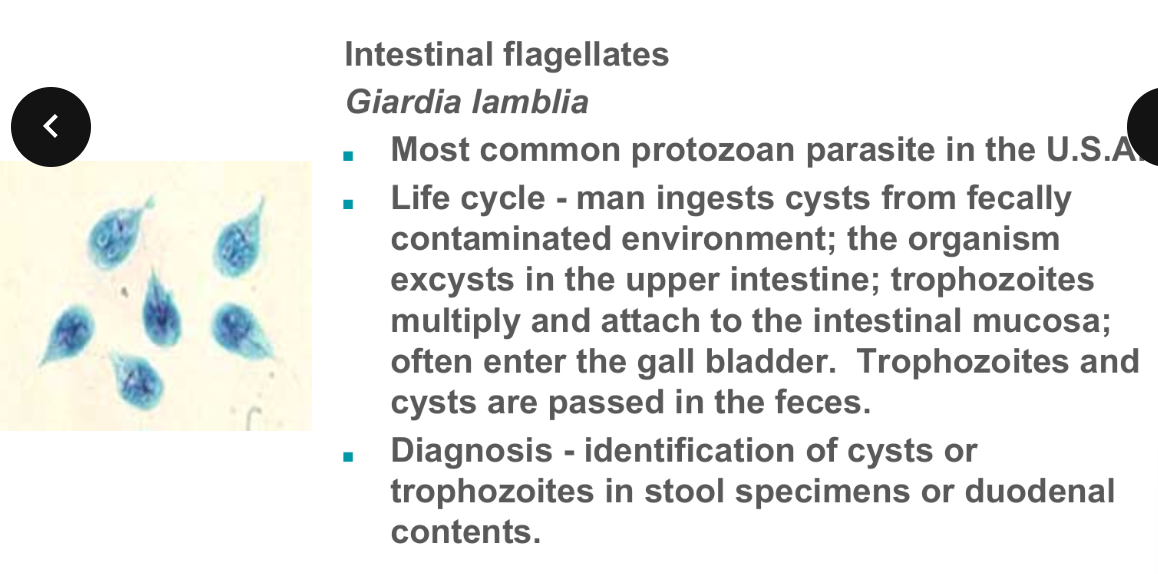
Intestinal flagellated G. Lamblia (Life cycle, Diagnosis, Morphology, Trophozite characteristics, Epidemiology, Pathology & Clinical Manifestations)
Morphology - very distinctive. Dorsal-ventrally flattened, and Bi-laterally
symmetrical.
Cyst - 9 x 12 micrometers and contain 2 to 4 nuclei; parabasal bodies are present.
Trophozoite - Four pairs of flagella - one pair located anterior, two pair located ventrally, and one pair located posteriorly. An axostyle and parabasal bodies are present.
Epidemiology - prevalence 1 to 30%, common in children’s day care centers; can be transmitted in water. Sexual transmission has been well documented.
Pathology and Clinical Manifestations - symptoms can be severe; diarrhea, foul-smelling, greasy, mucus-laden stools, flatulence, nausea, cramps. Most infections are asymptomatic; chronic cases experience weight loss, malabsorption of fat, protein, folic acid, and fat-soluble vitamins.
Intestinal flagellated D. Fragilis (Diagnosis, Morphology, Pathology, Distribution & Parasitic associations)
Laboratory diagnosis - detection of bi-nucleated trophozoites; fragmented karyosomes consisting of 4 to 8 granules of chromatin.
Diagnostic stage - the trophozoite in feces. There is no cyst stage.
Morphology - 1 or 2 nuclei, with little or no peripheral chromatin; karyosome is divided into 4 to 8 distinct granules.
May rarely ingest rbc’s.
Pathology - infection is usually asymptomatic; can be associated with diarrhea, anorexia, abdominal pain.
Association with pinworm - the organism may be transmitted from host to host within the egg of Enterobius vermicularis.
Distribution - worldwide, there is a 1% to 20% prevalence.
Intestinal flagellates C. Mesnili (Morphology, Transmission, Pathogenicity)
Non pathogenic
Found in Cecum & Colon
Transmission - by ingestion of mature cysts
Morphology
Trophozoite - 4 flagella (3 anterior, 1 associated with the cytostome; one nucleus, always located anteriorly.
Cyst - lemon shape; 1 nucleus; cytostome may be seen.
Trichomonads Characteristics
Undulating membrane - protoplasmic membrane with flagellar rim extending out like a fin along outer edge of body.
Flagella - several in a tuft, provides locomotion.
Axostyle - functions for support.
Costa - firm rod-like structure running along base of the undulating membrane.
Cytostome - rudimentary mouth.
Name the trichomonads
T. Hominis
T. Vaginalis
T. Hominis (Commensal, Transmission, Morphology)S
T. Vaginalis (Life cycle, Mode of infection, Diagnosis, Pathology, Morphology)
Life cycle - trophozoite lives in the vagina, urethra, epididymis, and
prostate; multiplies via longitudinal fission; no cyst stage.
Mode of infection - sexual intercourse or fomites.
Diagnosis - identification of trophozoites in body fluids (wet
mounts of discharges) or on PAP smears.
Pathology - Females: vaginal discharge; burning, Itching, or chafing. Frequency of urination or dysuria. Males: frequently asymptomatic. If the prostate is involved, the patient may develop discharge, dysuria, and enlargement of prostate with tenderness.
Morphology - has an axostyle and short undulating membrane that extends less than half the body length; 4 flagellae.
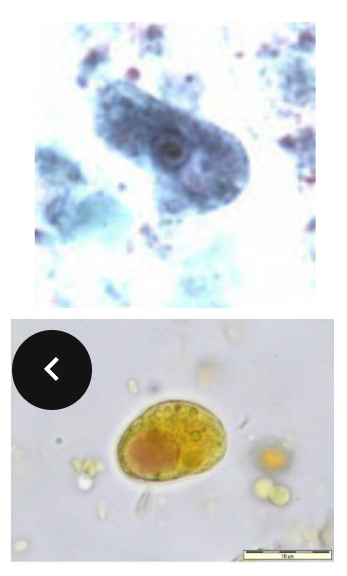
Ciliates B. Coli (Epidemiology, Size, Life cycle, Pathology, Diagnosis & Symptoms, Morphology)
Pathology/Symptoms
Infections are asymptomatic, organism feeding on bacteria at surface of mucosa. Severe infections - with the aid of hyaluronidase, the organism burrows into submucosa, producing ulcers.
Symptoms - dysentery, abdominal pain, nausea & vomiting, fever, headache.
Diagnosis - Diagnosed by observing cysts & trophozoites in fecal samples.
Morphology - Large, oval shape; two nuclei, 1 large kidney shaped
(macronucleus) & 1 small micronucleus (micronucleus not often seen); body surface covered by longitudinal rows of cilia; cytostome present.
Primary animal reservoir - pigs, monkeys.
Sporozoans - Intestinal Coccida General info
General -
Organisms infecting humans include Isospora, Sarcocystis, Cryptosporidium, Cyclospora & Toxoplasma.
Some have 2-host life cycle.
Sexual & asexual reproduction - Schizogony - asexual binary fission; Sporogony - sexual reproduction.
Diagnostic stages are often difficult to locate. Acid fast stains are used to visualize. Oocysts do not stain with iodine or permanent stains like trichrome.
S. Suihominis, Bovihominis & Lindemanni (Patholofy, Definitive hosts, Infective stage)
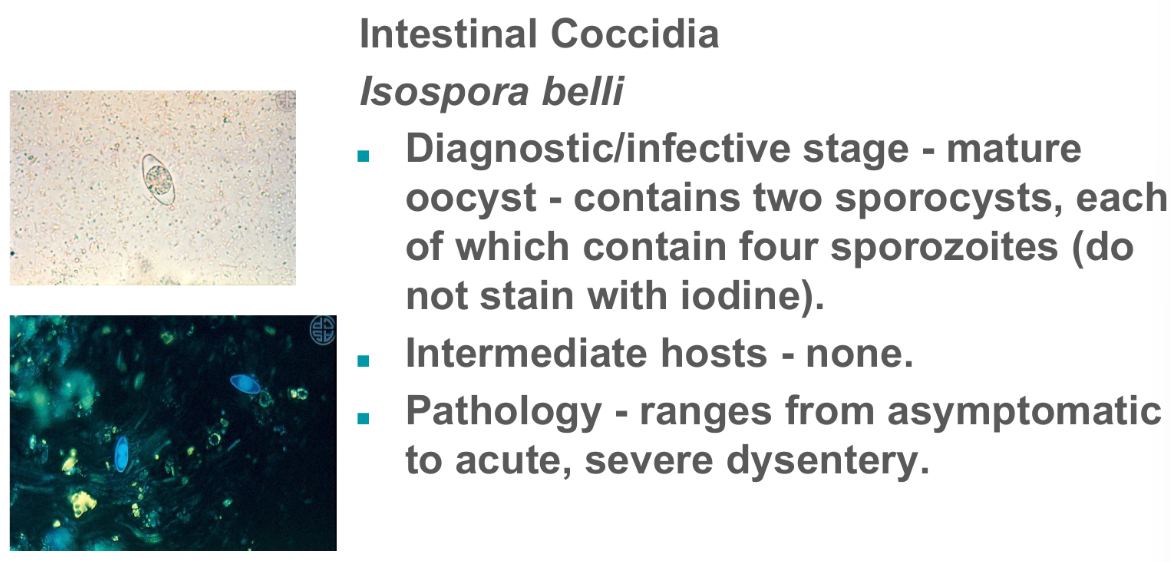
I. Belli (Definitive host, Schizogony, Sporogony, Diagnostic/infective stage, Intermediate hosts, Pathology)
Definitive host - humans.
Schizogony - takes place upon initial infection when sporozoites invade the intestinal epithelium and multiply.
Sporogony - progeny of asexual reproduction initiate development into gametes (male & female); fertilized gametes develop into oocysts which are passed as the infectious stage in the feces.
C. Parvum (Infection, Origins, Identification, Transmission, Pathology)
Cryptosporidium parvum
Site of infection - primarily an intestinal infection, can become systemic in AIDS patients.
Originally considered an animal parasite (rodents, cattle and sheep). Organisms from some (fish, fowl and reptiles) do not infect humans.
Infections in immunocompromised people can be serious, even fatal.
Identification - oocysts are 2 - 5 microns in diameter; do not stain with iodine; and are acid-fast.
Transmission - the endemic cycle is maintained via person-to-person, fecal-oral route transmission; a relatively common finding in “day-care” diarrhea; can be sexually transmitted; big potential for being waterborne due to significant resistance to disinfectants.
Pathology - most infections cause severe diarrhea. In the immunosuppressed patient, the condition is protracted and life threatening. There is no drug effective against this parasite.
C. Cayentanensis (General, Transmission, Pathology, Identification)
General - The first outbreak in the USA occurred in medical residents in 1980; a large multi-state outbreak occurred the summer of 1996. During this outbreak, Texas had more than 100 cases over a period of about six weeks, while no more than one case had been reported during any previous year.
Transmission - fecally contaminated food or water. The 1996 outbreak was associated with contaminated raspberries.
Pathology - diarrhea similar to that experienced with Cryptosporidium
infections.
Identification - Oocysts are 10 microns in diameter, and are variably acid-fast.