Sexually Transmitted Infections
0.0(0)
0.0(0)
Card Sorting
1/119
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
1
New cards
What host factors influence the risk of contracting STIs?
Complement deficiency (C5-C8)
HIV status
HIV status
2
New cards
Syphilis
Spirochete *Treponema pallidum*
Transmission requires close contact (horizontal spread through sexual contact; vertical spread – transplacental infection)
Organism sensitive to drying
Transmission requires close contact (horizontal spread through sexual contact; vertical spread – transplacental infection)
Organism sensitive to drying
3
New cards
*Treponema pallidum*
Limited ability to grow organism in labs
Replicates __**VERY**__ slowly → Incubation\~ 3 weeks
DO NOT HAVE A TCA CYCLE (rely on host cells for purines, pyrimidines, & a.a.)
Microaerophilic/anaerobic (extremely sensitive to O2)
Replicates __**VERY**__ slowly → Incubation\~ 3 weeks
DO NOT HAVE A TCA CYCLE (rely on host cells for purines, pyrimidines, & a.a.)
Microaerophilic/anaerobic (extremely sensitive to O2)
4
New cards
How is *T. pallidum* transmitted?
MSM are at greatest risk (anyone who has sex w/ barrier protection)
Exclusive to humans (can **NOT** spread through inanimate objects)
Transferred during early stages of disease
Contact with cutaneous/mucosal lesions
Exclusive to humans (can **NOT** spread through inanimate objects)
Transferred during early stages of disease
Contact with cutaneous/mucosal lesions
5
New cards
How is someone infected with *T. pallidum?*
Enters the body through small abrasions on skin/mucous membranes → Local multiplication → Infiltration of plasma cells, PMNs, & macrophages → Immune response reduces bacterial burden → Resolution of lesion
DOES NOT RELIABLY ELIMINATE INFECTION
DOES NOT RELIABLY ELIMINATE INFECTION
6
New cards
Endarteritis
inflammation of the inner lining of an artery
7
New cards
Primary Syphilis
2-10 weeks after initial contact: bacteria multiply at site of infection
Primary chancre appears at site of infection – usually painless
Enlarged inguinal nodes (proliferation of bacteria in regional lymph nodes)
Spontaneous healing may/can occur
Patient still highly infectious
Primary chancre appears at site of infection – usually painless
Enlarged inguinal nodes (proliferation of bacteria in regional lymph nodes)
Spontaneous healing may/can occur
Patient still highly infectious
8
New cards
Secondary Syphilis
1-3 months after primary syphilis symptoms
Flu-like illness (myalgia, fever, headache, mucocutaneous rash)
Symptoms can spontaneously resolve
Multiplication of bacteria and production of lesions in: lymph nodes, liver, joints, muscles, skin, mucous membranes
Flu-like illness (myalgia, fever, headache, mucocutaneous rash)
Symptoms can spontaneously resolve
Multiplication of bacteria and production of lesions in: lymph nodes, liver, joints, muscles, skin, mucous membranes
9
New cards
Latent Syphilis
\~2-6 weeks after 2º syphilis resolves
Treponemas are dormant in liver and spleen (bacterial hepatitis)
Reactivation of treponemas → multiplication
Can last anywhere between 3-30 years
Treponemas are dormant in liver and spleen (bacterial hepatitis)
Reactivation of treponemas → multiplication
Can last anywhere between 3-30 years
10
New cards
Tertiary Syphilis
Progressive destructive disease (dissemination & invasion; cell mediated HS)
Neurosyphilis (“General paralysis of the insane”; Tabes dorsalis)
Cardiovascular syphilis (Aortic lesions; heart failure)
Gummas in skin, bones, testes
Neurosyphilis (“General paralysis of the insane”; Tabes dorsalis)
Cardiovascular syphilis (Aortic lesions; heart failure)
Gummas in skin, bones, testes
11
New cards
Tabes dorsalis
loss of coordination of movement, especially as a result of syphilitic infection of the spinal cord
12
New cards
Congenital Syphilis
Infected mother transmits *T. pallidum* to baby in utero
Acquired after first 3 months of pregnancy (serious infection results in intrauterine death; congenital abnormalities)
Silent infection (not apparent until \~2 years of age; facial & tooth deformities)
Acquired after first 3 months of pregnancy (serious infection results in intrauterine death; congenital abnormalities)
Silent infection (not apparent until \~2 years of age; facial & tooth deformities)
13
New cards
How can we diagnose syphilis?
*T. pallidum* can __**NOT**__ be grown (easily) in (most) laboratory
Exudate from 1º chancre can be examined w/ dark-field microscopy
UV microscopy after staining w/ fluorescein antibodies
Silver staining
Exudate from 1º chancre can be examined w/ dark-field microscopy
UV microscopy after staining w/ fluorescein antibodies
Silver staining
14
New cards
Cardiolipin
non-specific syphilis test that allows for detection of anti-lipid IgG and IgM; Lipoidal material released from damaged cells → lipids in the surface of *T. pallidum*
15
New cards
ELISA use in syphilis can be used to detect what?
IgM or IGG
16
New cards
FTA-ABS (Fluorescent treponemal antibody absorption) test
specific syphilis test where a patient’s serum is absorbed w/ nonpathogenic treponemes → removes cross reacting Ab → detection of reaction w/ *T. pallidum* antigens
17
New cards
How can we treat syphilis?
Penicillin (drug of choice; reliably tx fetus when given to mother)
•Doxycycline if allergy to penicillin
Prevention of 2º & 3º disease depends on early dx & appropriate tx
•Doxycycline if allergy to penicillin
Prevention of 2º & 3º disease depends on early dx & appropriate tx
18
New cards
How is congenital syphilis treated?
treatable w/ early screening of mother'; Treatment w/ penicillin
19
New cards
Gonorrhea
*Neisseria gonorrhoeae (*Gram - coccus; Gonococcus – diplococci)
Gonococcus does __**not**__ survive well outside humans
Asymptomatically infected people are major reservoir (women > men)
2nd most reported STI in USA
Gonococcus does __**not**__ survive well outside humans
Asymptomatically infected people are major reservoir (women > men)
2nd most reported STI in USA
20
New cards
What are the gonococcal virulence factors?
**Pili –** mediate attachment; responsible for antigenic variation
**PorB** – must be functionally active for gonococcus to survive
**LOS –** increases TNFα activity
**PorB** – must be functionally active for gonococcus to survive
**LOS –** increases TNFα activity
21
New cards
What is the site of entry of *N. gonorrhoeae*?
Vagina or urethral mucosa of penis are sites of entry
Can enter through throat or rectal mucosa
Infection is **USUALLY** localized – can disseminate
Can enter through throat or rectal mucosa
Infection is **USUALLY** localized – can disseminate
22
New cards
How does *N. gonorrhoeae* evade host antibodies?
Produce IgA protease
23
New cards
What is the pathogenesis of gonorrhoeae?
Gonococci invade non-ciliated epithelial cells → Multiplication in intracellular vacuoles (protected from phagocytes & antibodies) →
Vacuoles move down & fuse w/ basement membrane of the cell → Release bacterial contents into subepithelial connective tissues → Damage is result of host inflammatory response (untreated can cause chronic inflammation & fibrosis)
Vacuoles move down & fuse w/ basement membrane of the cell → Release bacterial contents into subepithelial connective tissues → Damage is result of host inflammatory response (untreated can cause chronic inflammation & fibrosis)
24
New cards
How is gonorrhea transmitted?
Direct transmission, person to person (sexual contact)
Vertical transmission from mother to baby (childbirth)
Women have a 50% chance of becoming infected after contact, men have 20% chance
Vertical transmission from mother to baby (childbirth)
Women have a 50% chance of becoming infected after contact, men have 20% chance
25
New cards
What are the symptoms of gonorrhea in women?
Initially asymptomatic
Vaginal discharge
Untreated can lead to: PID, chronic pelvic pain, infertility
More likely to develop invasive disease
Sore throat
Rectal purulent discharge
Vaginal discharge
Untreated can lead to: PID, chronic pelvic pain, infertility
More likely to develop invasive disease
Sore throat
Rectal purulent discharge
26
New cards
What are the symptoms of gonorrhea in men?
Urethral discharge, dysuria
Sore throat
Rectal purulent discharge
Sore throat
Rectal purulent discharge
27
New cards
How can we diagnose gonorrhea?
Microscopy & culture (urethral & vaginal discharges(
Cultures are needed for women/asymptomatic men
Cultures also aid in antibiotic susceptibility tests
Cultured on selective (Thayer Martin) & non-selective medium (chocolate)
Blood cultures for suspected disseminated disease
Joint aspirates
Cultures are needed for women/asymptomatic men
Cultures also aid in antibiotic susceptibility tests
Cultured on selective (Thayer Martin) & non-selective medium (chocolate)
Blood cultures for suspected disseminated disease
Joint aspirates
28
New cards
How do we treat gonorrhea?
Cefixime or ceftriaxone (+ azithromycin)
Antibiotic eyedrops for affected babies
Antibiotic eyedrops for affected babies
29
New cards
How can we prevent Gonorrhea?
Follow-up & contact tracing are vital to control spread
Condoms for prevention
Condoms for prevention
30
New cards
What can compromise the treatment of gonorrhea?
penicillinase producing strains (resistance to fluroquinolones also observed)
31
New cards
Chlamydia
*Chlamydia trachomatis* (very small, intracellular bacteria)
Exists in different forms: Elementary body (EB) & Reticulate body (RB) – adapted for intracellular multiplication
Exists in different forms: Elementary body (EB) & Reticulate body (RB) – adapted for intracellular multiplication
32
New cards
What form of chlamydia is adapted for extracellular survival and initiation of infection?
\
A. Elementary body (EB)
B. Reticulate body (RB)
\
A. Elementary body (EB)
B. Reticulate body (RB)
A. Elementary body (EB)
33
New cards
What form of chlamydia is adapted for intracellular multiplication?
\
A. Elementary body (EB)
B. Reticulate body (RB)
\
A. Elementary body (EB)
B. Reticulate body (RB)
B. Reticulate body (RB)
34
New cards
What serotypes of Chlamydia cause trachoma?
\
A. A, B, C
B. D-K
C. L1, L2, L3
\
A. A, B, C
B. D-K
C. L1, L2, L3
A. A, B, C
35
New cards
What serotypes of Chlamydia cause cervicitis, urethritis, proctitis, conjunctivitis, pneumonia (in neonates)?
\
A. A, B, C
B. D-K
C. L1, L2, L3
\
A. A, B, C
B. D-K
C. L1, L2, L3
B. D-K
36
New cards
What serotypes of Chlamydia cause lymphogranuloma venereum?
\
A. A, B, C
B. D-K
C. L1, L2, L3
\
A. A, B, C
B. D-K
C. L1, L2, L3
C. L1, L2, L3
37
New cards
Trachoma
serious eye infection
38
New cards
Cervicitis
infection/inflammation of cervix
39
New cards
Urethritis
infection/inflammation of urethra
40
New cards
Proctitis
infection/inflammation of prostate
41
New cards
Conjunctivitis
infection/inflammation of conjunctiva; eye infection
42
New cards
Pneumonia
infection in the lungs
43
New cards
Lymphogranuloma venereum
chronic infection of the lymphatic system
44
New cards
What is the most common bacterial STI?
*Chlamydia trachomatis*
45
New cards
What type of cells are infected with *Chlamydia trachomatis?*
Nonciliated columnar, cuboidal, and transitional epithelial cells
46
New cards
What form of *Chlamydia trachomatis* is a metabolically inactive infectious form?
Elementary body (EB)
47
New cards
What form of *Chlamydia trachomatis* accumulates in the phagosome and are called inclusions?
Reticulate body (RB)
48
New cards
How is *C. trachomatis* transmitted?
Most infections are genital, acquired through sexual contact
Neonates develop ocular infections from passage through birth canal
Adult ocular infections can also occur
Neonates develop ocular infections from passage through birth canal
Adult ocular infections can also occur
49
New cards
What is the pathogenesis of chlamydia?
Chlamydiae enter host through small abrasions in mucosal surfaces → Bind to specific receptors on host cell → “parasite induced” endocytosis → Inside the cell lysosomal fusion is inhibited → EB begins its developmental cycle → EB differentiate into metabolically active RBs → RBs divide and produce fresh EB progeny → Released into extracellular environment
50
New cards
What serotypes of Chlamydia are restricted to columnar and transitional epithelial cells?
\
A. A, B, C
B. D-K
C. L1, L2, L3
\
A. A, B, C
B. D-K
C. L1, L2, L3
B. D-K
51
New cards
What serotypes of Chlamydia can cause systemic disease?
\
A. A, B, C
B. D-K
C. L1, L2, L3
\
A. A, B, C
B. D-K
C. L1, L2, L3
C. L1, L2, L3
52
New cards
What are the symptoms of *C. trachomatis?*
Most genital tract infections are asymptomatic (can result in PID in women)
Clinical manifestations can include cervicitis & endometritis
Bartholinitis, perihepatitis, salpingitis, urethritis
Mucopurulent discharge is seen in symptomatic infections
Clinical manifestations can include cervicitis & endometritis
Bartholinitis, perihepatitis, salpingitis, urethritis
Mucopurulent discharge is seen in symptomatic infections
53
New cards
How can we diagnose chlamydia?
Microscopy using direct fluorescent antibody test (EBs stain bright yellow-green)
Nucleic-acid-based tests are capable of directly testing (Nucleic acid probe and amplification tests; Specimen from cervix, urethra, urine, etc. can be used; Commercially available – rapid results)
Nucleic-acid-based tests are capable of directly testing (Nucleic acid probe and amplification tests; Specimen from cervix, urethra, urine, etc. can be used; Commercially available – rapid results)
54
New cards
How can we treat chlamydia?
__**NOT**__ susceptible to β-lactam antibiotics
Azithromycin along w/ β-lactam antibiotics for concurrent infections (Prescribed to partners too)
Erythromycin used in babies
Prevention = condoms
Azithromycin along w/ β-lactam antibiotics for concurrent infections (Prescribed to partners too)
Erythromycin used in babies
Prevention = condoms
55
New cards
Lymphogranuloma venereum
*C. trachomatis* serotypes L1, L2, L3
Systemic infection involving lymphoid tissue
Common in Africa, Asia, and South America
Affects males > females (especially men who have sex w/ men)
Systemic infection involving lymphoid tissue
Common in Africa, Asia, and South America
Affects males > females (especially men who have sex w/ men)
56
New cards
What are the clinical features of Lymphogranuloma venereum?
Primary lesion is an ulcerating papule at site of inoculation (occurs after 1-4 weeks)
Accompanied w/ fever, headache, myalgia
Systemic complication can include fever, hepatitis, pneumonitis, meningoencephalitis
Accompanied w/ fever, headache, myalgia
Systemic complication can include fever, hepatitis, pneumonitis, meningoencephalitis
57
New cards
What is a complication associated with Lymphogranuloma venereum?
Chronic granulomatous reactions in lymphatics & neighboring tissues
Can cause fistula in ano or genital elephantiasis
Can cause fistula in ano or genital elephantiasis
58
New cards
How do we diagnose Lymphogranuloma venereum?
Cell culture, immunofluorescence, nucleic-acid based tests for diagnosis
59
New cards
How can we treat Lymphogranuloma venereum?
Doxycycline or erythromycin
Pregnant women and children < 9 years old should be treated w/ erythromycin
Pregnant women and children < 9 years old should be treated w/ erythromycin
60
New cards
Chancroid
*Haemophilus ducreyi* infection
Characterized by a **painful** non-indurated genital ulcers
Local lymphadenitis
Endemic in some areas of USA (occurs in outbreaks)
Characterized by a **painful** non-indurated genital ulcers
Local lymphadenitis
Endemic in some areas of USA (occurs in outbreaks)
61
New cards
What is the most common cause of genital ulcers in Africa and Asia?
chancroid
62
New cards
*Haemophilus ducreyi*
Gram-negative
Requires specialized media – chocolate agar (Hemin (X factor) & Nicotinamide adenine dinucleotide (V factor))
Causes tender papule 5–7 days after exposure → 2 days later–lesion ulcerates → Inguinal lymphadenopathy
Requires specialized media – chocolate agar (Hemin (X factor) & Nicotinamide adenine dinucleotide (V factor))
Causes tender papule 5–7 days after exposure → 2 days later–lesion ulcerates → Inguinal lymphadenopathy
63
New cards
How do we diagnose chancroid?
Gram stain of aspirates from ulcer (also can use enlarged lymph node aspirates)
*H. ducreyi* is hard to grow in laboratory (use rich media & lower temps (33C))
Slow growth – 2 to 9 days
*H. ducreyi* is hard to grow in laboratory (use rich media & lower temps (33C))
Slow growth – 2 to 9 days
64
New cards
How do we treat chancroid?
erythromycin, azithromycin, or ceftriaxone
65
New cards
Donovanosis
*Klebsiella granulomatis* infection (granuloma inguinale or granuloma venereum)
Common in tropical and subtropical regions (Caribbean, New Guinea, India & central Australia)
Nodules → erode to granulomatous ulcers → ulcers bleed on contact
Bacteria invade and multiply within mononuclear cells → Cause lysis
Common in tropical and subtropical regions (Caribbean, New Guinea, India & central Australia)
Nodules → erode to granulomatous ulcers → ulcers bleed on contact
Bacteria invade and multiply within mononuclear cells → Cause lysis
66
New cards
*Klebsiella granulomatis*
Gram negative
Prolonged incubation (weeks-months)
Transmitted via sexual contact or nonsexual trauma to the genitalia
Causes painless granulomatous lesions (can resemble syphilis)
Prolonged incubation (weeks-months)
Transmitted via sexual contact or nonsexual trauma to the genitalia
Causes painless granulomatous lesions (can resemble syphilis)
67
New cards
How do we diagnose donovanosis?
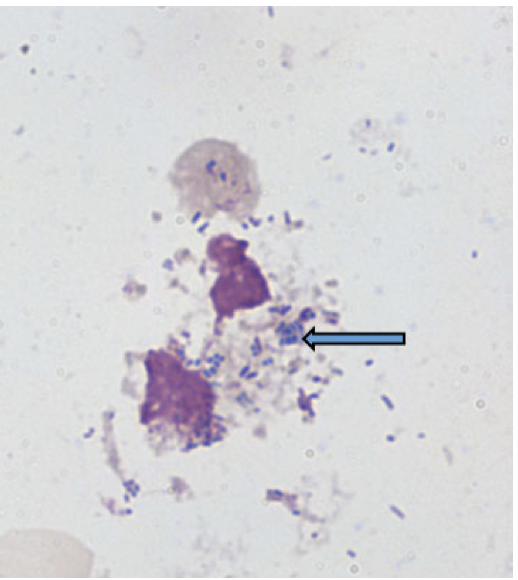
Wright’s or Giemsa stain on smear from lesion
Appearance of Donovan bodies (clusters of blue/black stained organisms in cytoplasm of mononuclear cells)
Appearance of Donovan bodies (clusters of blue/black stained organisms in cytoplasm of mononuclear cells)
68
New cards
How do we treat donovanosis?
doxycycline, azithromycin, or co-trimoxazole
69
New cards
What are potential causes of genital tract infections?
*Mycoplasma hominis*
*Mycoplasma genitalium*
*Ureaplasma urealyticum*
*Mycoplasma genitalium*
*Ureaplasma urealyticum*
70
New cards
What pathogen may cause non-gonococcal urethritis?
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
A. *Mycoplasma genitalium*
71
New cards
What pathogen may cause PID, postabortal and postpartum fevers, pyelonephritis?
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
B. *Mycoplasma hominis*
72
New cards
What pathogen may cause non-gonococcal urethritis and prostatitis?
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
\
A. *Mycoplasma genitalium*
B. *Mycoplasma hominis*
C. *Ureaplasma urealyticum*
C. *Ureaplasma urealyticum*
73
New cards
What are treatment options for genital tract infections?
doxycycline or azithromycin
74
New cards
Candidiasis
*Candida albicans (n*ormal flora of vagina)
Can be transmitted sexually (presence does not imply sexual transmission)
Increase in candida causes an intensely irritant vaginitis
Can be accompanied by urethritis and dysuria
May present as UTI
Balanitis is seen in \~10% of male partners of infected women
Can be transmitted sexually (presence does not imply sexual transmission)
Increase in candida causes an intensely irritant vaginitis
Can be accompanied by urethritis and dysuria
May present as UTI
Balanitis is seen in \~10% of male partners of infected women
75
New cards
Balanitis
Inflammation of glans penis
76
New cards
*Candida albicans*
Exist as an oval yeastlike form that produce buds or blastoconidia
Forms germ tubes
Primary site of colonization is the GI tract (whole tube)
Opportunistic pathogen (can infect many sites)
Forms germ tubes
Primary site of colonization is the GI tract (whole tube)
Opportunistic pathogen (can infect many sites)
77
New cards
What are predisposing factors for Candidiasis?
Oral contraceptives
Pregnancy
Diabetes mellitus
Systemic corticosteroids
HIV
Antibiotic use
Pregnancy
Diabetes mellitus
Systemic corticosteroids
HIV
Antibiotic use
78
New cards
How can we diagnose candidiasis?
microscopy or culture of discharge
79
New cards
How can we treat candidiasis?
Treated w/ topical antifungal – clotrimazole (oral antifungal – fluconazole)
80
New cards
*Trichomonas vaginalis*
Protozoan parasite
Inhabits vagina (women) and urethra/prostate (men)
Causes vaginitis w/ copious amounts of discharge
One of the most prevalent non-viral STIs in USA (higher incidence in HIV+ population)
Associated w/ PID in HIV+ women
Inhabits vagina (women) and urethra/prostate (men)
Causes vaginitis w/ copious amounts of discharge
One of the most prevalent non-viral STIs in USA (higher incidence in HIV+ population)
Associated w/ PID in HIV+ women
81
New cards
How is *Trichomonas vaginalis* transmitted?
transmitted as fomite
82
New cards
*T. vaginalis* infection is associated with what?
associated with preterm delivery
83
New cards
Heavy infection with what pathogen leads to copious foul-smelling vaginal discharge?
*T. vaginalis* infection
84
New cards
How do we diagnose *T. vaginalis?*
Detected by wet preparation microscopy of secretions or swab
Rapid immunochromatographic tests & nucleic acid detection test
Rapid immunochromatographic tests & nucleic acid detection test
85
New cards
How do we treat *T. vaginalis?*
nitroimidazoles, metronidazole, or tinidazole
Sexual partners should __**BOTH**__ be treated
Sexual partners should __**BOTH**__ be treated
86
New cards
Bacterial Vaginosis
Associated w/ *Gardnerella vaginalis*
Causes a fishy smelling discharge
Can be associated w/ an anaerobic infection
Can be sexually transmitted
Disruption of the normal acidity of vagina & of equilibrium between constituents of normal flora
Causes a fishy smelling discharge
Can be associated w/ an anaerobic infection
Can be sexually transmitted
Disruption of the normal acidity of vagina & of equilibrium between constituents of normal flora
87
New cards
Bacterial vaginosis is characterized by what?
Excessive malodorous vaginal discharge
Vaginal pH > 4.5
Presence of clue cells (vaginal epithelial cells coated with bacteria)
A fishy/amine-like odor
Vaginal pH > 4.5
Presence of clue cells (vaginal epithelial cells coated with bacteria)
A fishy/amine-like odor
88
New cards
*G. vaginalis* is consistently found in what?
found in vaginosis
89
New cards
How can we diagnose bacterial vaginosis?
Can be cultured on human blood agar plates from swab (Urethra & Vaginal)
90
New cards
How can we treat bacterial vaginosis?
metronidazole
91
New cards
Genital Herpes
Most commonly caused by Herpes simplex virus 2 (HSV2) (HSV1 can also be cause)
HSV2 is transmitted sexually (most common STI, \~500 million infected worldwide)
HSV2 is transmitted sexually (most common STI, \~500 million infected worldwide)
92
New cards
Herpes Simplex Virus - 2
Large, enveloped virus (dsDNA)
Encodes crucial enzymes (DNA-dependent DNA polymerase, deoxyribonuclease, thymidine kinase, ribonucleotide reductase, protease)
Very little cross immunity w/ HSV1 (infect mucoepithelial cells)
Can cause lytic or latent infection
Infection can result in 2-fold increased risk of developing HIV (breach in mucosal barrier due to ulcers)
Encodes crucial enzymes (DNA-dependent DNA polymerase, deoxyribonuclease, thymidine kinase, ribonucleotide reductase, protease)
Very little cross immunity w/ HSV1 (infect mucoepithelial cells)
Can cause lytic or latent infection
Infection can result in 2-fold increased risk of developing HIV (breach in mucosal barrier due to ulcers)
93
New cards
Ribonucleotide reductase
converts ribonucleotides to deoxyribonucleotides
94
New cards
Thymidine kinase
phosphorylates the deoxyribonucleosides to provide substrates for replication of the viral genome
95
New cards
How does HSV infect cells?
Binds to cell surface receptor → Penetration through fusion of envelope & cell surface membrane → Interaction w/ nectin-1 → Virion releases capsid into cytoplasm → enters nucleus → transcription → replication → assembly → capsid buds into trans-golgi network → released by exocytosis or cell lysis
96
New cards
Infection of what can establish HSV2 latency?
infection of neurons
97
New cards
What enzyme is necessary for HSV2 latency?
thymidine kinase
98
New cards
What are the only regions to be transcribed on HSV2 virus?
Latency-associated transcripts (LATs)
99
New cards
Reoccurrence of HSV2 can be activated by which type of stimuli?
Stress, trauma, fever, sunlight
100
New cards
What is the process of latency in HSV2?
Lesion → Virus travels up sensory nerve endings → Establishes latent infection in dorsal root ganglion neurons → Reactivation (sunburn, stress, trauma) → Travels down nerves to same area → Recurrent lesions