(25.7) Regulation of Urine Concentration & Volume
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
19 Terms
Name main function(s) of the Kidneys
Make any adjustment needed to maintain body fluid osmotic concentration at around 300 mOsm
Produce only small amounts of urine if the body is dehydrated or diluted urine if over-hydrated
Accomplished by using countercurrent mechanism
Define Osmolality
Number of solutes particles in 1 kg of H2O
1 osmol = 1 mole of particle per kg H2O
Body fluids have much smaller amounts → so expressed in milliosmols (mOsm) = 0.001 osmol
Define Countercurrent mechanism
Fluid flows in opposite directions in two adjacent segments of same tube with hairpin turn
Distinguish between Countercurrent multipler & Countercurrent exchanger
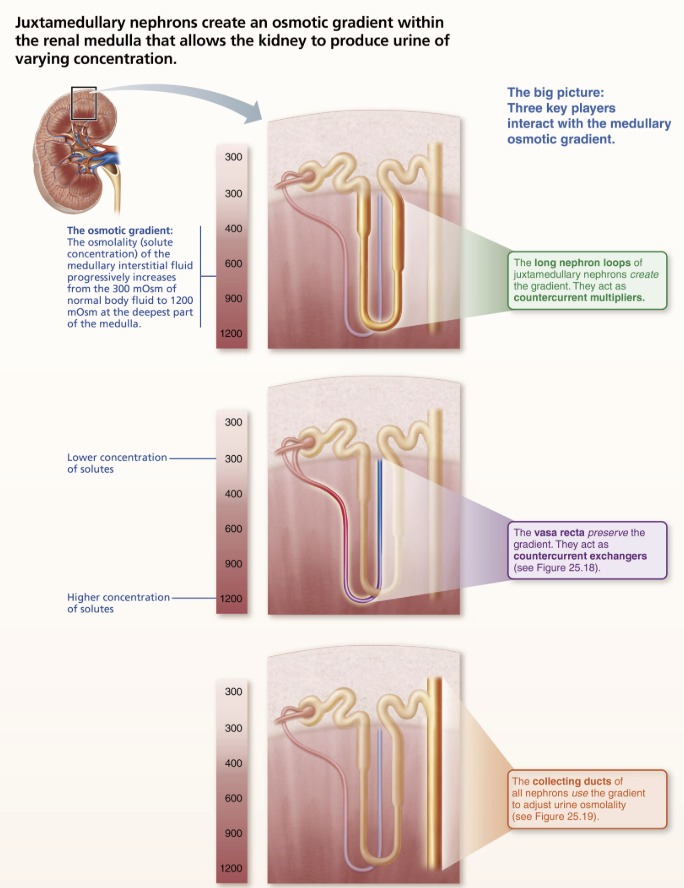
These countercurrent mechanisms work together to: Establish and maintain medullary osmotic gradient from renal cortex through medulla
Gradient runs from 300 mOsm in cortex to 1200 mOsm at bottom of medulla
Countercurrent multiplier forms gradient
Countercurrent exchanger preserves gradient
Collecting ducts can then use gradient to vary urine concentration
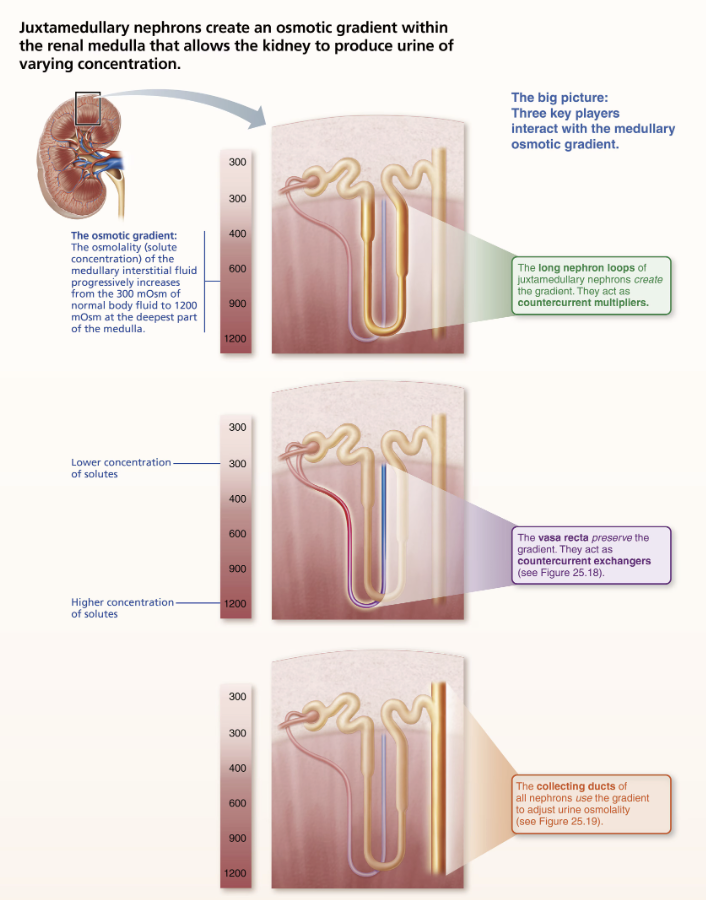
Describe the Location and Function of Countercurrent Multipler
Nephron loops of the juxtamedullary nephrons create gradient
T/F: Limbs of nephron loop are not in direct contact but close enough to influence each other’s exchanges with surrounding interstitial fluid
→ TRUE
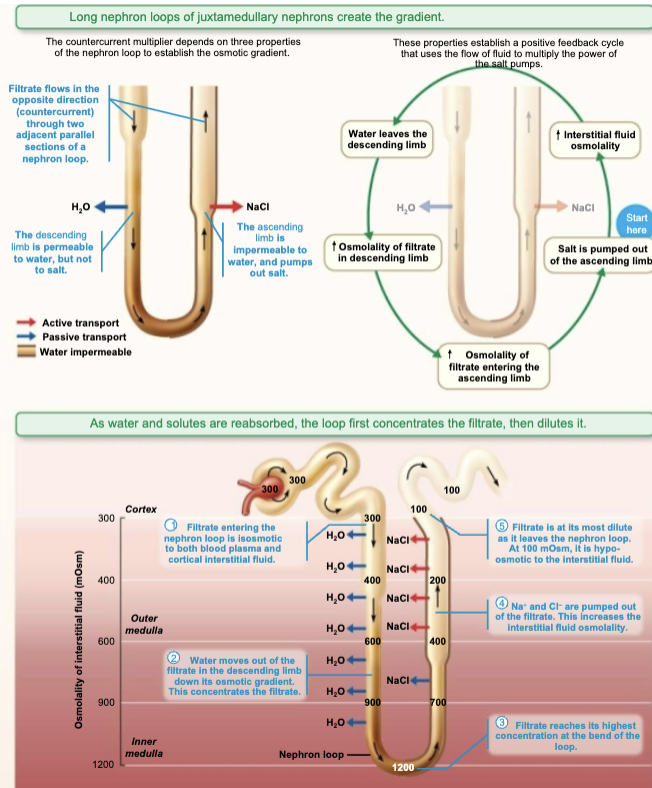
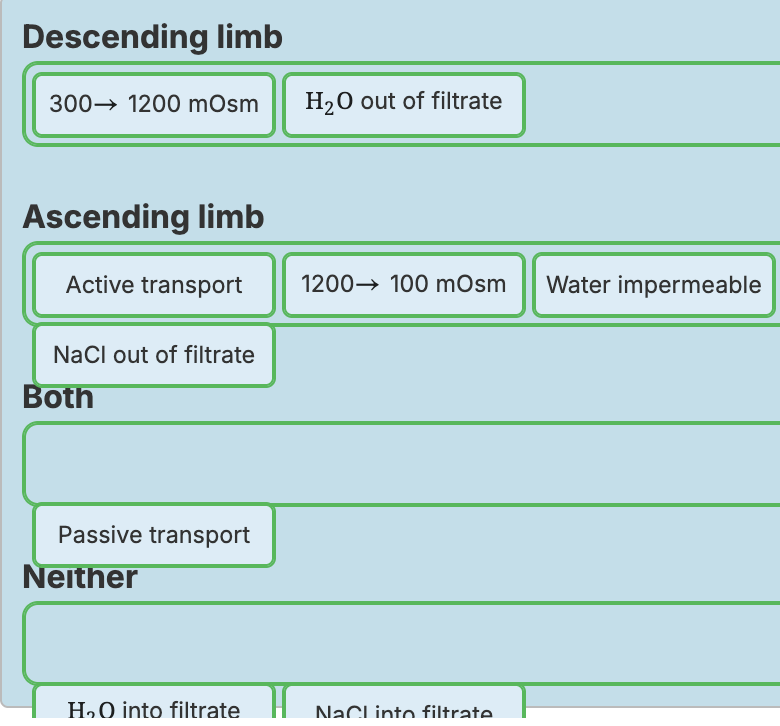
Describe how Changes in the Permeability of the Nephron Loop to Water and Salt create Osmotic Gradients
Countercurrent Multipler
Descending limb of nephron loop is freely permeable to H2O, impermeable for solutes
H2O passes out of filtrate into hyperosmotic medullary interstitial fluid
Causes remaining filtrate osmolality to increase to ~1200 mOsm
Ascending limb of nephron loop is impermeable to H2O and selectively permeable to for solutes
Na+ and Cl- are actively reabsorbed in thick segments
Some passively reabsorbed in thin segment
Constant difference of 200 mOsm always exists between two limbs of nephron loop and between ascending limb and interstitial fluid
Difference is “multiplied” along length of loop (from 3000 to 1200 mOsm = difference of 900 mOsm)
Which of the following is NOT a property used to establish the medullary osmotic gradient?
A.) the filtrate flow through the ascending and descending limbs of the long nephron loops of juxtamedullary nephrons
B.) the blood flow through the ascending and descending portions of the vasa recta
C.) the descending limb's permeability to water and impermeability to salt
D.) the ascending limb's impermeability to water and permeability to salt
→ B.) the blood flow through the ascending and descending portions of the vasa recta → The vasa recta act as countercurrent exchangers to
preserve the osmotic gradient.
A.) the filtrate flow through the ascending and descending limbs of the long nephron loops of juxtamedullary nephrons
C.) the descending limb's permeability to water and impermeability to salt
D.) the ascending limb's impermeability to water and permeability to salt
Explain the Countercurrent Multipler role in Countercurrent mechanism
The MORE NaCl are ascending limb actively transport out into interstitial fluid, the more water diffuses out of the descending limb
The MORE water that diffuses out of the descending limb, the SALTIER the filtrate becomes
Ascending limb uses salty filtrate to further raise osmolarity of medullary interstitial fluid
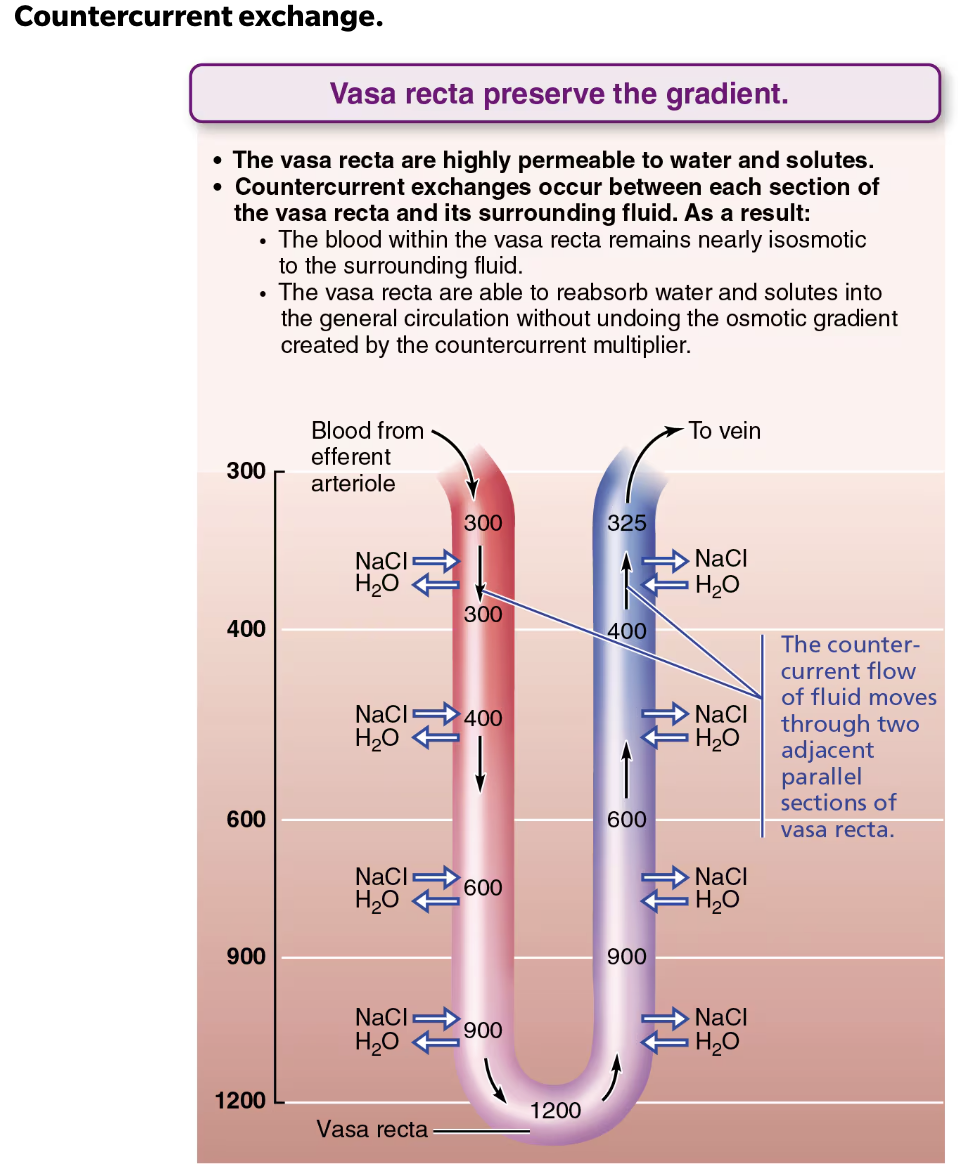
Describe the Location and Function of Countercurrent Exchanger
Countercurrent exchanger utilizes vasa recta → preserve the gradeint
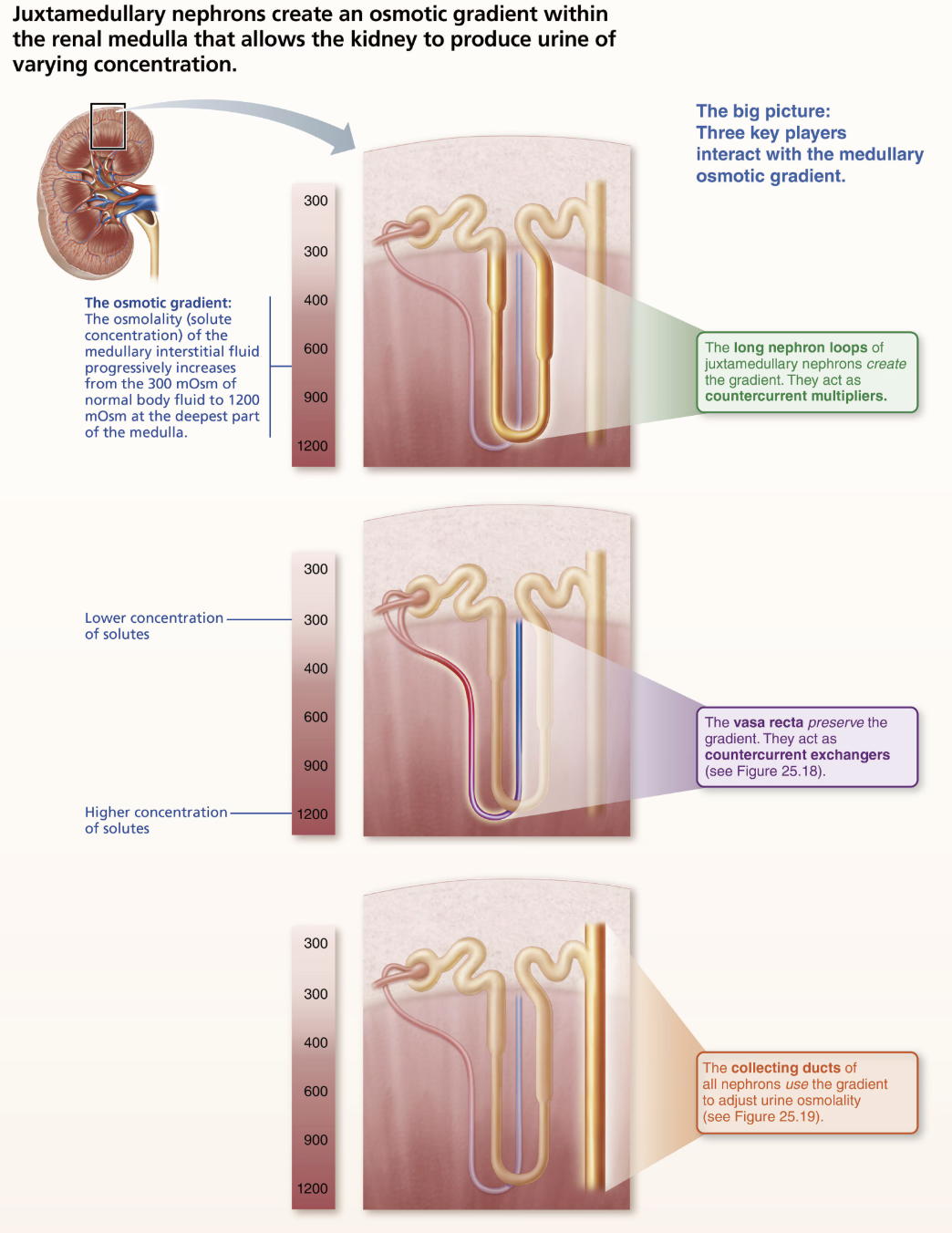
Role of Vasa Recta
Countercurrent exchanger utilizes vasa recta → highly permeable to water and solutes
Flow of blood in vasa recta is also countercurrent (hairpin turn) so blood can exchange NaCl and water with surrounding interstitial fluid as it moves adjacent parallel sections of gradient
Blood inside vasa recta remains isosmotic with surrounding interstitial fluid
Able to reabsorb water and solutes without undoing osmotic gradient created by countercurrent multipler
Main function(s) of Countercurrent Exchanger
Preserves medullary gradient by:
Preventing rapid removal of slat from interstitial space
Removing reabsorbed water
T/F: Volume of blood at end of vasa recta is lesser than at beginning
→ FALSE
Water is ascending vasa recta comes from descending vasa recta or is reabsorbed from nephron loop and collecting duct
RESULT → volume of blood at end of vasa recta is GREATER than at beginning
SUMMARY of Creation of the Medullary Osmotic Gradient
Describe how the Osmotic Gradients are used to create Dilute and Concentrated Urine
Established medullary osmotic gradeint can now be used to form dilute or concentrated urine
WITHOUT GRADIENT would not be able to raise urine concentration >300 mOsm to conserve water
Explain Effect of Overhydration vs Dehydration in relation to Urine
Overhydration
Produces LARGE volume of dilute urine
ADH production decreases; urine ~100 mOsm
IF aldosterone present, additional ions can be removed, causing water to dilute to ~50 mOsm
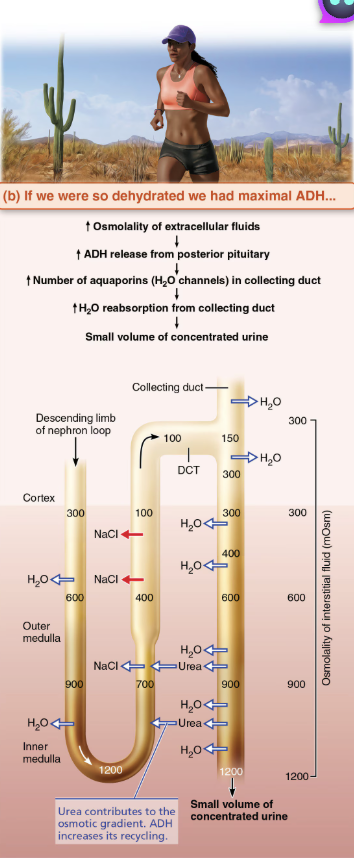
Dehydration
Produces SMALL volume of concentrated urine
Maximal ADH is released; urine ~1200 mOsm
Severe dehydration: 99% water reabsorbed
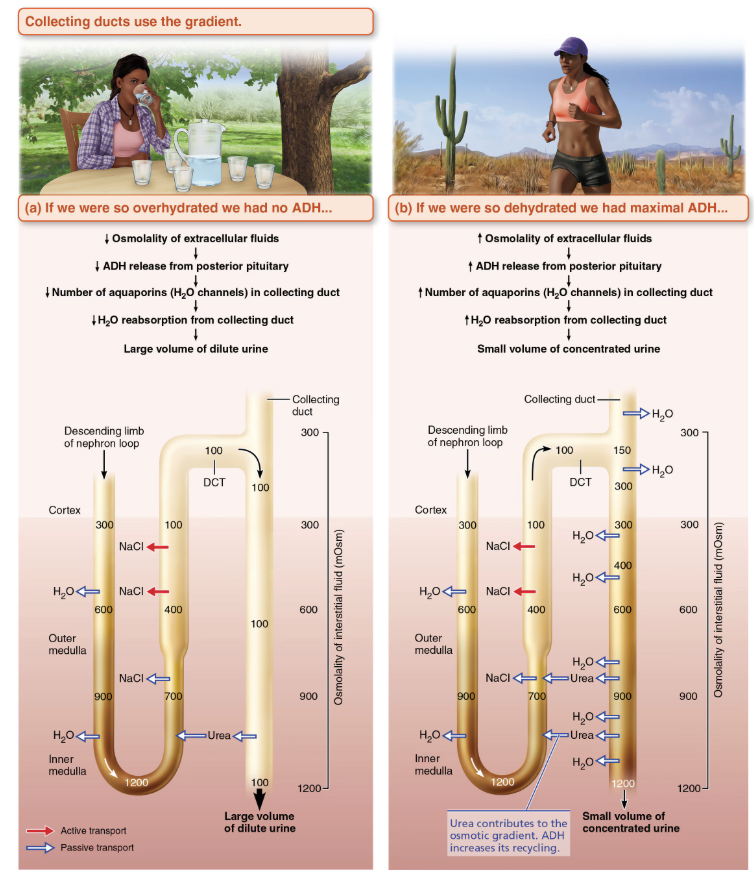
Role of Urea
Urea helps form medullary gradient
Enters filtrate in ascending thin limb of nephron loop by facilitated diffusion
Cortical collecting duct reabsorbs water, leaving urea behind
In deep medullary region, now highly concentrated urea leaves collecting duct and enters interstitial fluid of medulla
Urea then moves back into ascending thin limb
Contributes to HIGH osmolality in medulla
Define Diuretics
Chemicals that enhance urinary output
List three diuretics we learned function to increase urine production
Caffeine (drugs for hypertension or edema)
Na+ reabsorption inhibitors (and resultant H2O reabsorption)
Alcohol
ADH inhibitors
Osmotic diuretics
Substance not reabsorbed, so water remains in urine
EX: in diabetic patient, high glucose concentration pulls water from body