Regional anatomy 4 -- the thorax 1
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
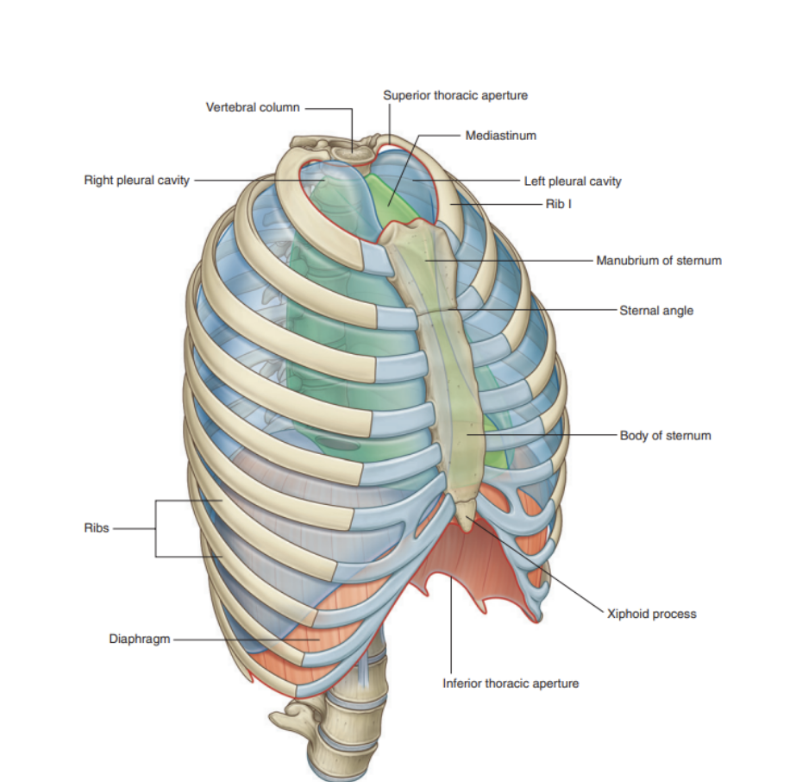
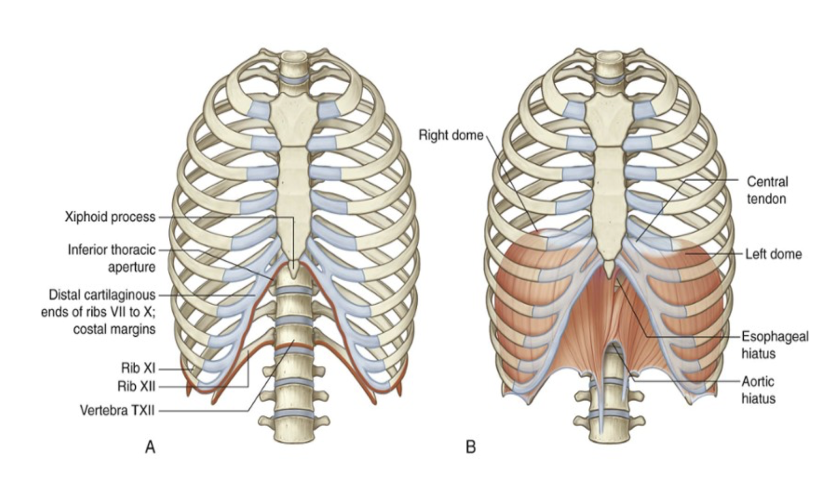
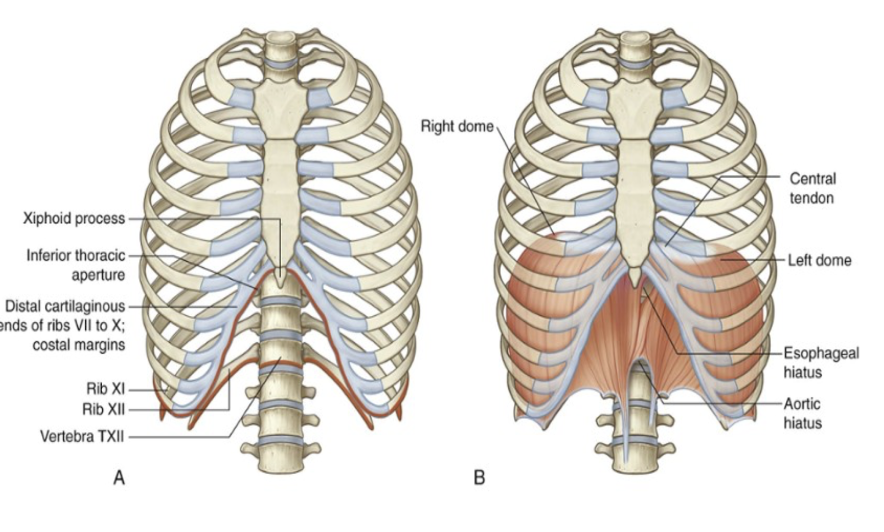
The thorax — overall
An irregularly shaped cylinder with —
A narrow opening superiorly — the superior thoracic aperture
Open, allowing continuity with the neck
A relatively large opening inferiorly — inferior thoracic aperture
Closed by the diaphragm
The muscoskeletal wall at the level of the thorax is composed of segmentally arranged vertebrae, ribs, multiple muscles, and the sternum
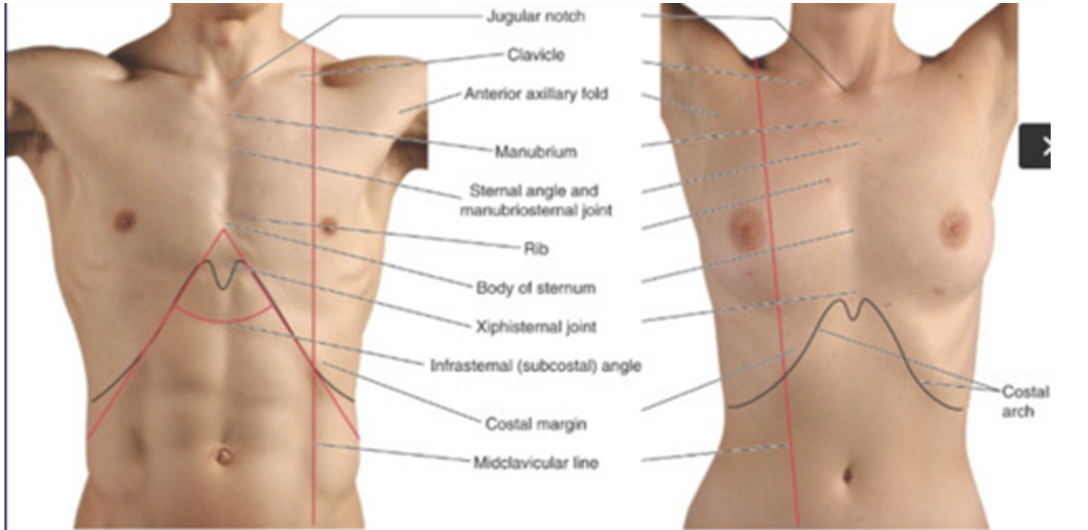
Superficial & deep limits of the thorax
Superficial limits —
Superior limit —
Starts from the depression manubrium of sternum, continues with clavicle & ends at level of T1
Inferior limit —
Originates from xyphoid process (most distal process of sternum), continues at the inferior part of the ribcage and ends at the level of spinous process T12
Deep limits —
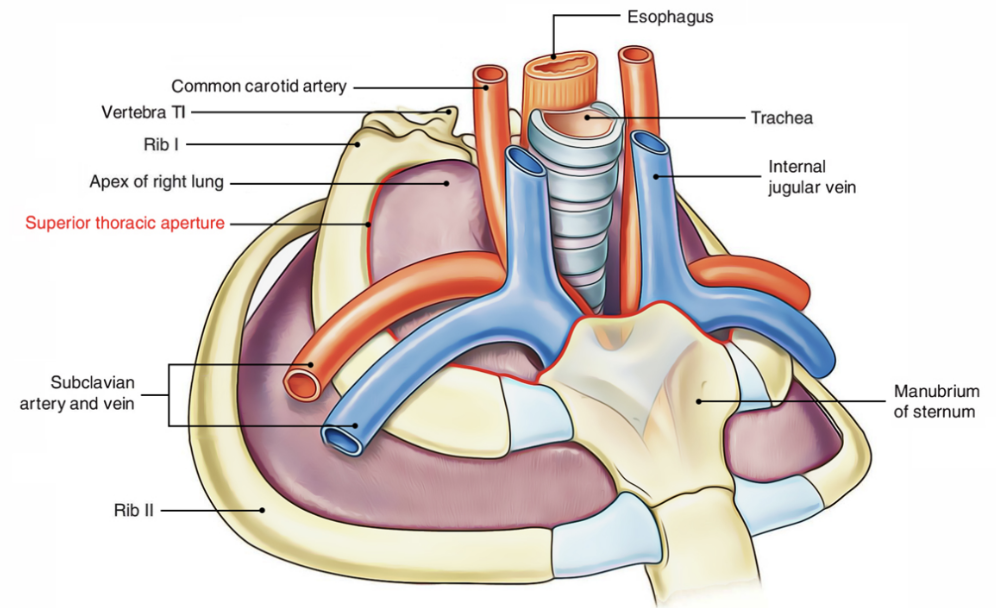
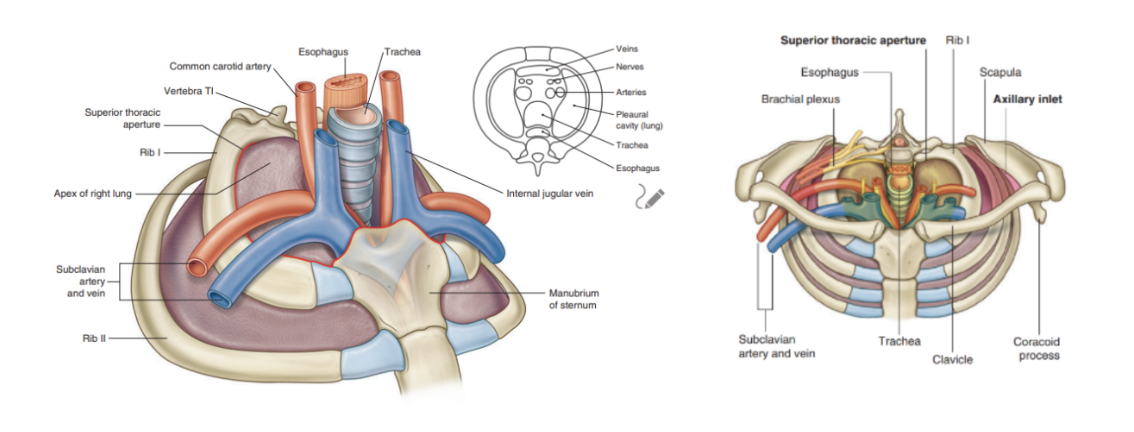
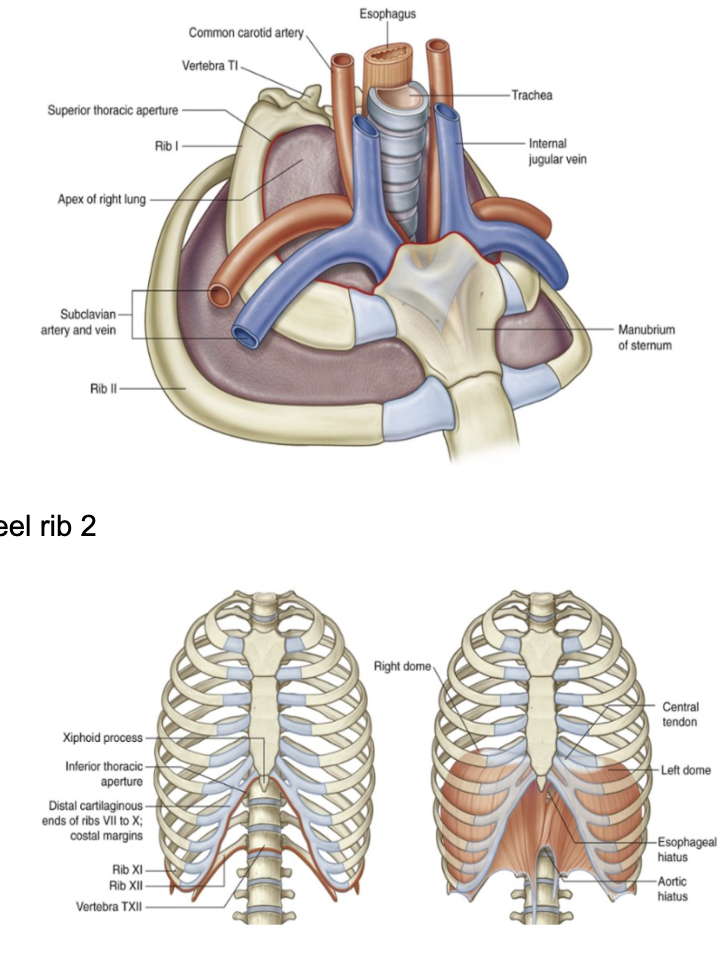
Superior thoracic aperture —
Bordered by Vertebrae T1, Rib 1, and manubrium of sternum
Inferior thoracic aperture —
Bordered by Vertebrae TXII, Rib XII, End of rib XI, Costal margin & xiphoid process of the sternum
Superior thoracic aperture & middle mediastinum
Middle mediastinum —
Centrally located in the thoracic cavity —
Contains — pericardium, heart, origins of great vessels, various nerves, & smaller vessels
Completely surrounded by skeletal elements & consists of —
Posteriorly — body of vertebra T1
On each side — Medial margin of Rib I
Anteriorly — manubrium
The first ribs slope inferiorly from their posterior articulation with T1 to their anterior attachment to he manubrium —
Thus, the plane of the superior thoracic aperture is at an oblique angle, facing anteriorly
Structures that pass between the upper limb & thorax pass over Rib I and the superior part of the pleural cavity as they enter & leave the mediastinum
Ex. subclavian arteries & veins
Structures that pass between the neck & head & thorax pass more vertically through the superior thoracic aperture
Inferior thoracic aperture
Closed by the diaphragm, with structures passing between the abdomen and thorax piercing or passing posteriorly to the diaphragm
Skeletal elements —
Body of vertebra TXII posteriorly
Rib XII and distal end of XI posterolaterally
Distal cartilaginous ends of ribs VII to , uniting to form the costal margin anterolaterally
Xiphoid process anteriorly
The joint between the costal margin and sternum lies roughly in the same horizontal plane as the intervertebral disc between vertebrae TIX and TX —
The posterior margin of the inferior thoracic aperture is inferior to the anterior margin — when viewed anteriorly, the inferior thoracic aperture is tilted superiorly.
Subdivisions of the thorax —
The thoracic cavity is enclosed by the thoracic wall & diaphragm & is subdivided into 3 major compartments —
A right & left pleural cavity (for each lung)
Mediastinum —
Heart, esophagus, trachea, major nerves & systematic blood vessels, and thymus
Clinical drop — significance of the medistanium & pleural cavities
Pleural cavities are completely separated from each other by the mediastinum
Thus mediastinum can be entered separately, and an abnormal event in one pleural cavity will not affect the other
Functions of the thorax —
Breathing
Protection of vital organs
Conduit
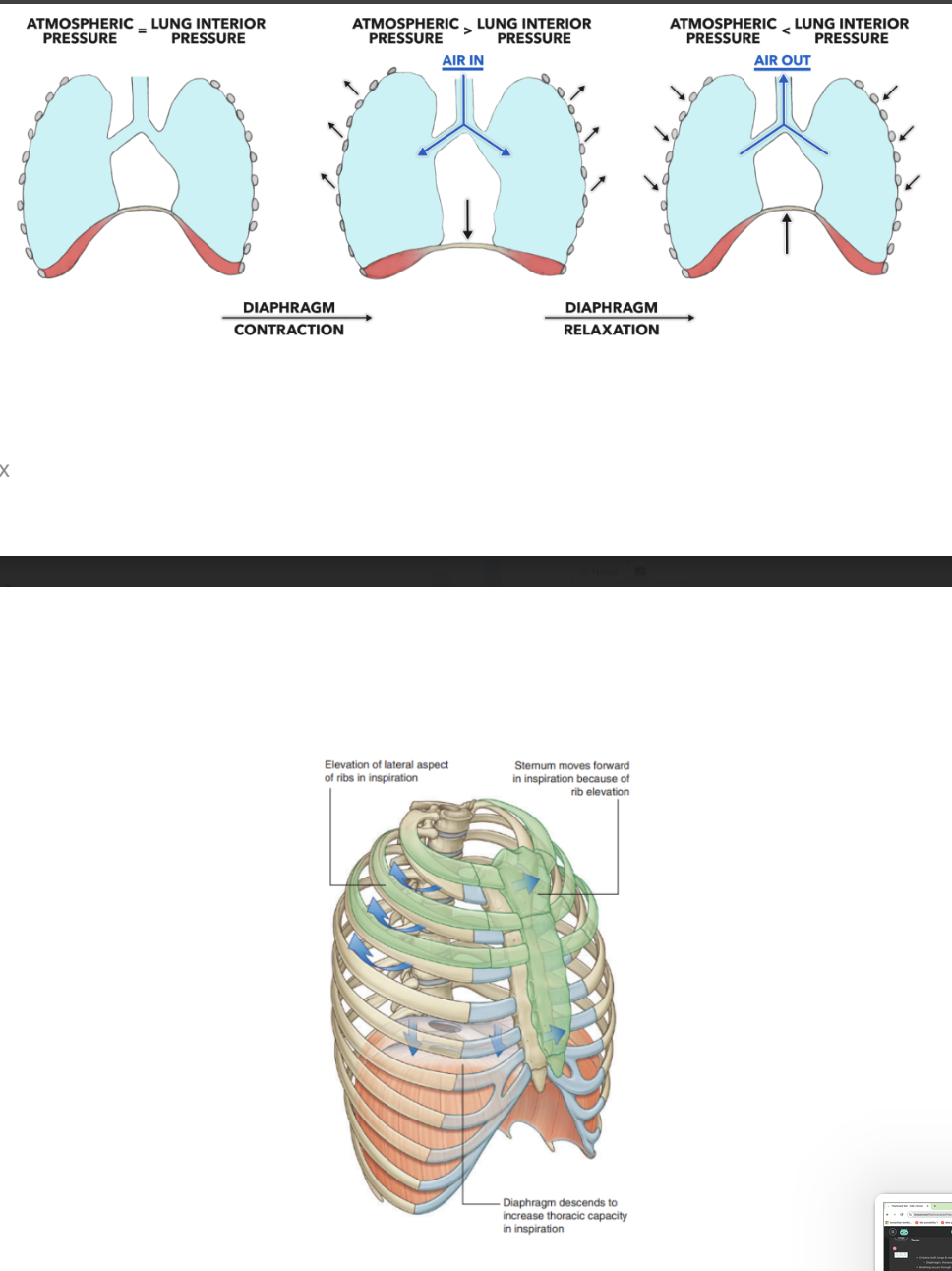
Breathing function of the thorax
Contains both lungs & machinery necessary for breathing —
Diaphragm, thoracic wall, & ribs
Breathing occurs through the establishment of pressure differences, up & down movements of the diaphragm, and lateral & anterior movements of the thoracic wall (via rib movement)
Vital organ protection function of the thorax
Houses & protects the heart, lungs, and great vessels
Due to the diaphragm’s specific shape (upward domed shape), the thoracic wall also offers protection to some of the important abdominal viscera
Ex. liver, stomach, & spleen — all lie under the right dome of the diaphragm
Conduit function of thorax
Many structures pass through allowing communication from one bdy region to another & for structures that connect organs in the thorax to other body regions — ex.
Esophagus, Vagus nerves, & thoracic duct — pass through the mediastinum as they go between abdomen & neck
Phrenic nerves — originate in neck & pass through mediastinum to penetrate & supply diaphragm
Trachea, thoracic aorta, & superior vena cava — pass at mediastinum en route to & from major visceral organs in the thorax.
Thoracic wall
Composed of skeletal elements & muscles —
Posteriorly —
Formed by 12 thoracic vertebrae + intervertebral discs between
Laterally —
Formed by ribs + 3 layers of flat muscle
These muscles span between adjacent ribs & function to move the ribs & provide support for the intercostal spaces
Anteriorly —
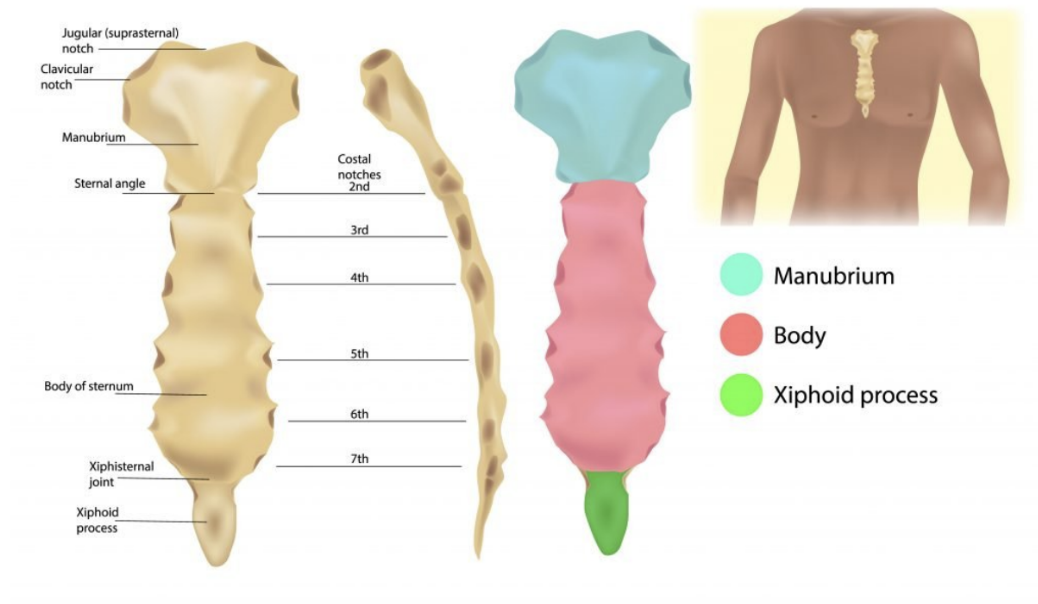
Made of the sternum —
Manubrium of sternum + body of sternum + Xiphoid process
Clinical drop — manubrium of sternum as a landmark
It is angled posteriorly on the body of sternum at the manubriosternal joint — forming the sternal angle
This angle is used by clinicians as an important landmark when performing physical examinations of the thorax
Skeletal framework of the thorax
Skeletal elements of the thoracic wall consist of —
The thoracic vertebrae
Intervertebral discs, ribs, and sternum
Thoracic vertebrae
There are 12 thoracic vertebrae, each of which is characterized by articulaions. with ribs — Typical thoracic vertebrae —
Heart-shaped vertebral body, with roughly equal dimensions in the transverse & anteroposterior directions, and a long spinous process
Vertebral foramen — generally circular
Broad laminae overlapping with those of vertebra below
Superior articular processes are flat, with their articular surfaces facing posteriorly, while inferior articular processes project from the laminae and their articular facets face anteriorly
Transverse proesses are club shaped and project posterolaterally
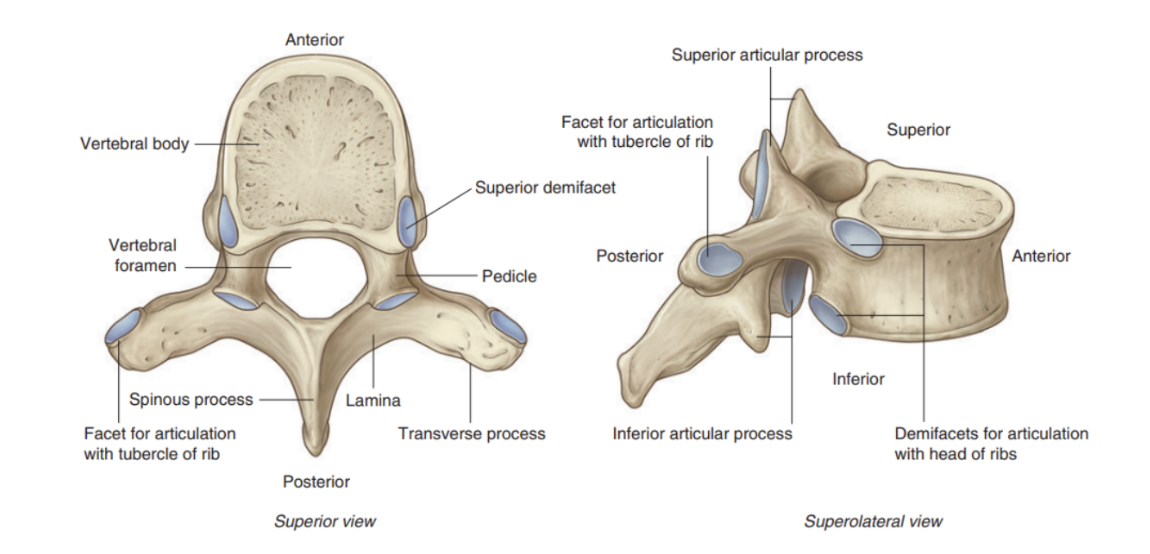
(typical) Vertebral articulations with the ribs
The typical thoracic vertebra has 3 sites on each side for articulation with ribs —
2 demifacets (partial facets) located on the superior & inferior aspects of the body for articulation with corresponding sites on the heads of adjacent ribs —
Superior costal faet articulates with part of the head of its own rib
Inferior costal faet articulates with part of the head of the rib below
Oval facet (transverse costal facet) at the end of the transverse process articulates with the tubercle of its own rib
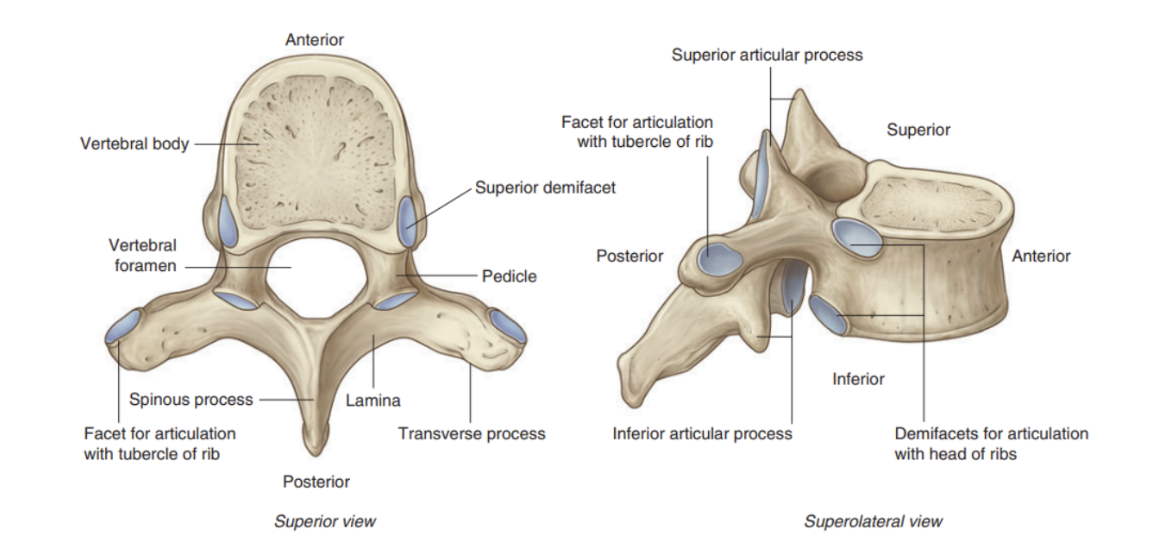
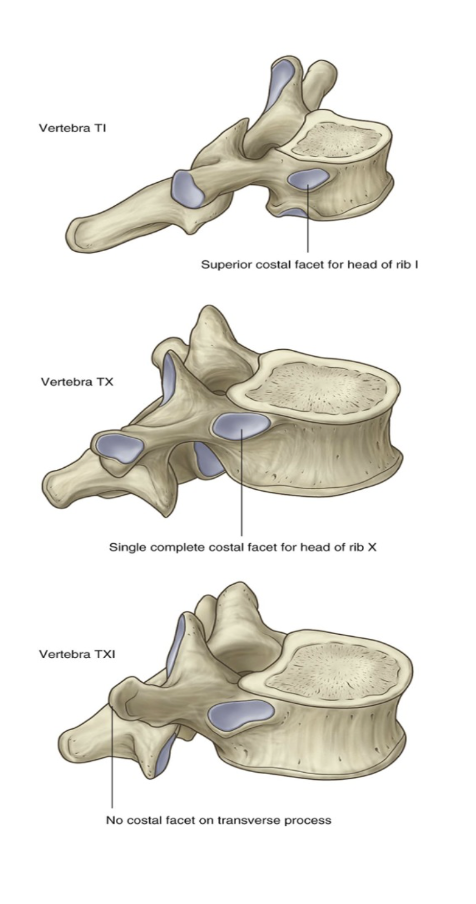
Atypical vertebral articulations with ribs
Superior costal facets on the body of vertebra T1 are complte and articulate with a single facet on the head of its own rib —
the head of rib I does not articulate with vertebra CVII
Vertebra TX (& often TIX) articulates with only its own ribs — thus lacks inferior demifacets on the body
Vertebrae TXI & TXII articulate only with the heads of their own ribs — they lack transverse costal facets and have only a single complete facet on each side of their bodies
(basically rib 1 only attaches via 1 superior costal facet to T1 — no attachment to C7, vertebrae T10,11, & 12 only attach via a superior costal facet — no inferior costal facet (1 rib per vertebrae), and vertebrae T11 & 12 don’t have transverse costal facets)
Ribs (overall)
The anterior end of each rib (distal) —
Composed of costal cartilage — contributes to mobility & elasticity of the wall
All ribs articulate with the vertebral column — however, only the costal cartilages of the upper 7 ribs (true ribs), articulate directioly with the sternum
Remaining 5 pairs are called false ribs
Groups of ribs —
Last 2 ribs – rib 11 & 12 – called floating ribs
We don’t have a connection with the anterior part of the sternum
3 diff groups of ribs (2 main) –
Vertebrosternal – 1-7
Vertebrochondral – 8-10
False ribs – 11 & 12 (no connection with sternum, but fundamental for insertion of muscles of lumbar region ribcage
(basically — 1-7 attach via costal cartilages to body of sternum, 8-10 attach via costal cartilages to bottom of body of sternum, 11 & 12 don’t attach — floating)
Nomenclature —
The part of the ribs articulating with the thoracic vertebrae (in the spine) is called the proximal end & the part articulating with the costal-cartilage/sternum is called the distal end
Rib structure
Each rib is divided into different parts
Posterior part – connected to vertebrae in thoracic region – called head
Can see 2 articular apexes for the articulation with the vertebrae of the thoracic region
2nd part called the neck
Makes a connection between the head & the body of the rib
Between the neck & the body, there is the tubercul
In the tubercul we have the costal passage for the articulation of the transverse process of the thoracic vertebrae
On the inferior part of each rib, we have a groove
Allows passage of neurovascular bundles
Bundle pattern – most superior structure = intercostal vein, then artery, then nerve
All these structures are protected by the inferior border of the rib
This anatomic structure is fundamental when we want to carry out thoracentesis – insertion of a needle/tube in the chest between the intercostal spaces to take out the abnormal accumulation of fluid – to avoid injury of neurovascular bundle, we have to insert the needle on the superior border of the rib
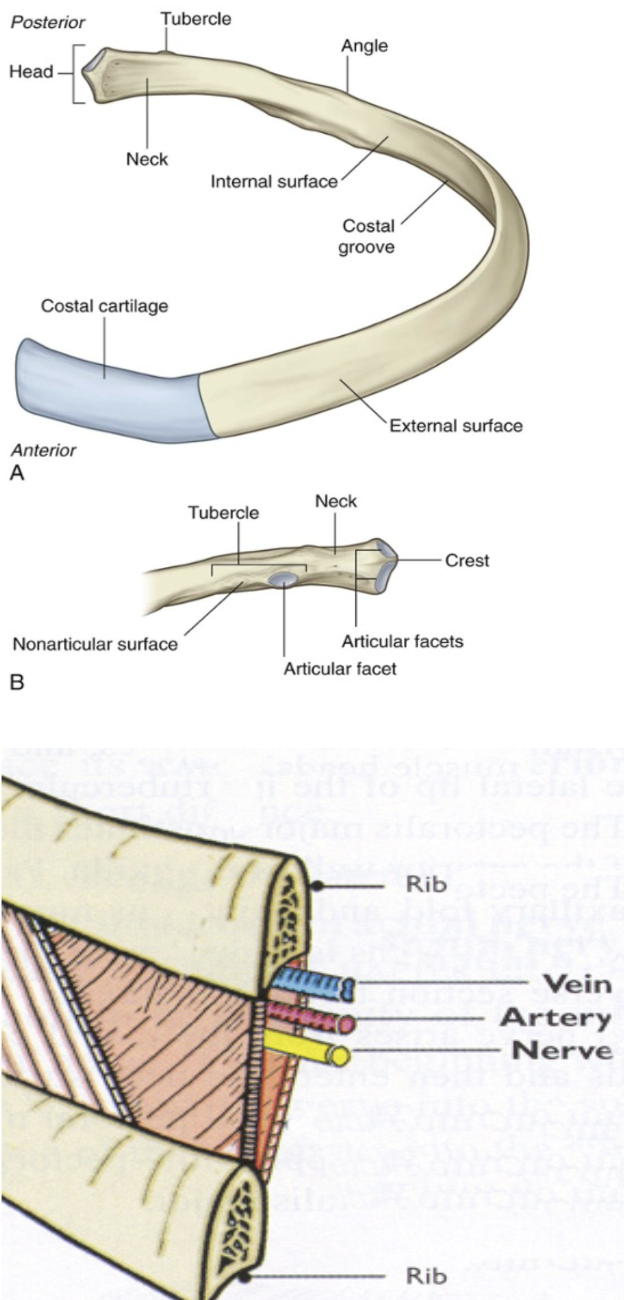
Rib 1, 11, & rib 12 –
Only 1 articular facet on the head for the articulation with the first thoracic vertebrae – in rib 1, 11, & 12, and sometimes also rib 10 – only 1 facet for the articulation with the body of the vertebrae instead of 2
Rib 1 has a horizontal plate with 2 depressions (1 anterior & 1 posterior)
Allow passage of 2 vessels – anteriorly subclavian vein, posteriorly subclavian artery
Palpation of subclavian artery
Impossible to palpate subclavian artery because behind the clavicle
Rib 1 embedded in soft tissues and muscles originating in clavicle & posterior to clavicle, so impossible to palpate
Blood goes along subclavian artery to end (brachial artery) – so first step to check is brachial artery – if ok then we can figure out that there isn’t an injury at greater vessels at base of neck, so necessary to do further exams
Rib 11 & 12 – missing tubercular articular facet
Only an articular facet on the edge of the rib, and another exception to the pattern – there isn’t the articular facet on the tubercle for the articulation for the thoracic vertebrae – only 1 articular facet on the head, the lack of one on the tubercle, and then it ends without the connection to the sternum
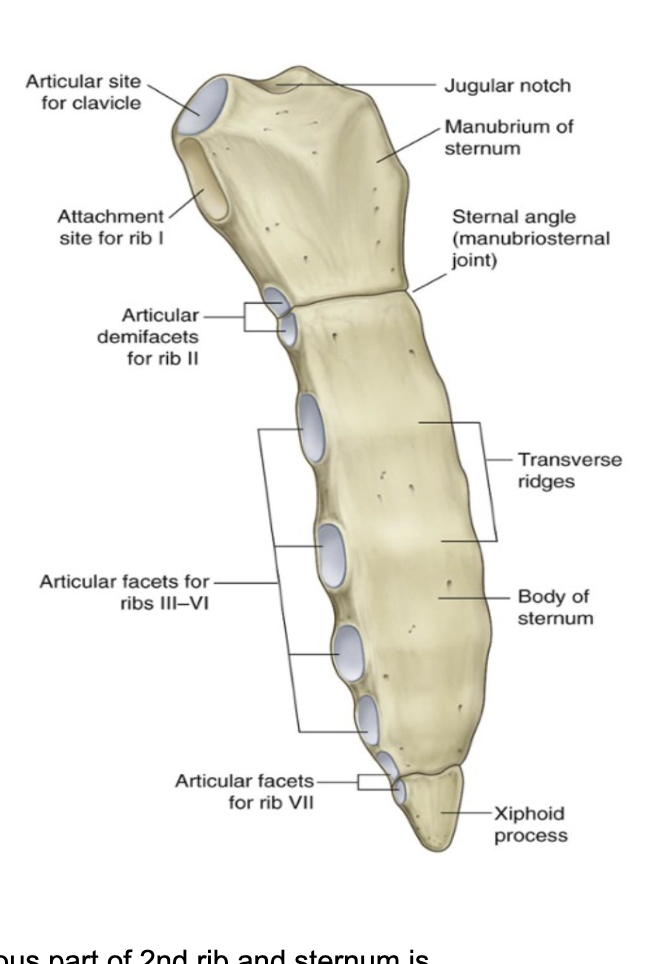
Sternum –
The anterior part of the ribcage, very important for physical examination
Made up of 3 different parts
Superiorly – manubrium of the sternum
Superior notch, at base of neck – called jugular notch of the sternum
On each lateral side, we have 2 further notches – called clavicular notches
Important for the articulation with the clavicle
On the lateral borders, we have the facets for the articulations with the anterior cartilaginous part of the ribs
First costal notch for first rib – fibrocartilagenous joint
Middle – body of the sternum
Narrow & longitudinally oriented
Inferior – xyphoid process
Small
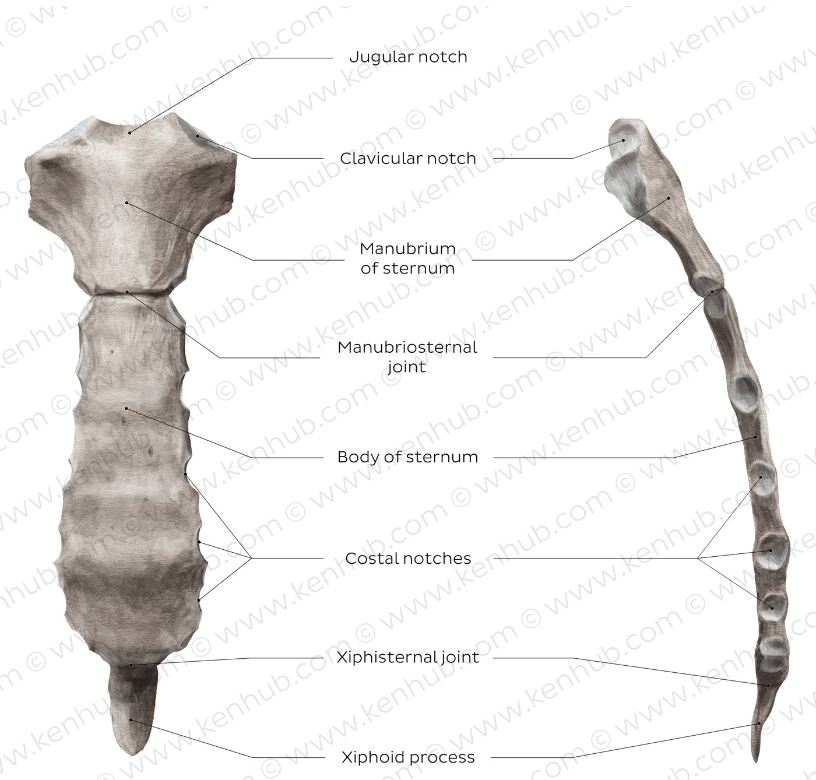
Manubrium of the sternum —
Forms part of the bony framework of the neck & the thorax
Superior surface —
Expanded laterally with jugular notch on the midline
On either side of this notch is a large oval fossa for articulation with the clavicle
Immediately inferior to this fossa on each lateral surface — a facet for the attachment of the first costal cartilage
At the lower end of the lateral border is a demifacet for articulation with the upper half of the anterior end of the second costal cartilage
Body of the sternum
Flat
Marked by transverse risdges on its anterior surface that represent lines of fusion between the segmental elements called sternebrae (from where the body arises embryologically)
Laterally (on the margins) — articular facets for the costal cartilages
Superiorly, each margin has a demifacet for articulation with the inferior aspect of the second costal cartilage
Inferior to this demifacet — 4 facets for articulation with the costal cartilags of ribs II to VI
At the most inferior end we have another demifacet for articulation with the 7th costal cartilage
I think ts saying theres a demifacet between manubrium & body & between body & xiphoid — nvm not at bottom only up there? look at image talking ab sternocostal joints
Inferior end of the sternum body is attached to the xiphoid process
Exceptions to synovial joints between ribs & sternum —
All articulations between the ribs and the sternum are synovial – with only 1 exception (the first rib, articulates with the manubrium of the sternum with a fibrocartilagenous joint)
Further exception – articulation between cartilagenous part of 2nd rib and sternum is between the manubrium & the body of the sternum so is divided into parts –
On the cartilagenous part of rib 2 there are 2 costal facets that articulate with the 2 costal facets present on the inferior border of the manubrium & the superior part of the body
Synovial joints with the other ribs until rib 7
On the anterior part of the sternum, we have bony crests – due to fusion of bony elements of the sternum that in the embryo are called sternobrae – can make a comparison between the sternum & another bone with these crests – sacral vertebrae
Importance of sternum for physical examination
What is the method to count the intercostal spaces (to know where to inset needle/tube) – can consider the sternal angle
The angle between the manubrium of the sternum ‘7 the body of the sternum – have to palpate the jugular notch along the midline at the base of the neck, go down & palpate the manubrium of the sternum, and when going down, can palpate a bony ridge – which is the angle between the manubrium & the body – at level of 2nd rib
If moving laterally, we enter wit the tip of the finger into the first intercostal space – from there go down
Can also palpate the clavicle, go down – the first space is the intercostal space (best way to check)
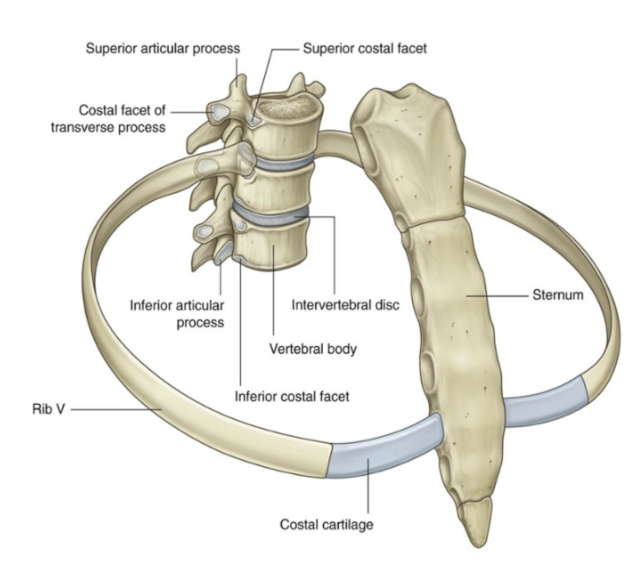
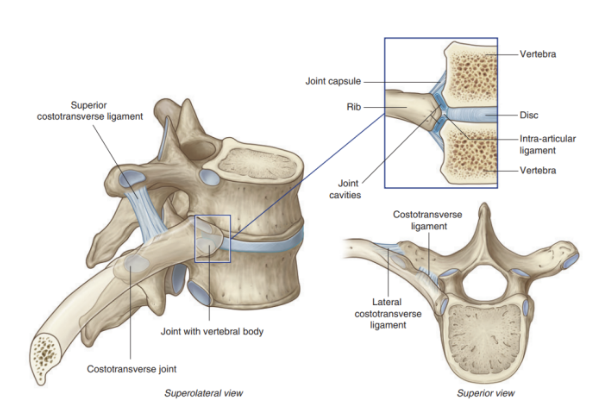
Joints relating to ribs
The typical rib articulates with —
Bodies of adjacent vertebrae, forming a joint with the head of the rib
Transverse process of its related vertebra, forming a costotransverse joint
Joints with the vertebral bodies are divided into 2 synovial compartments by an intra-articular ligament (image), which attaches to the intervertebral disc
The 2 synovial compartments & the ligament are surrounded by the same joint capsule
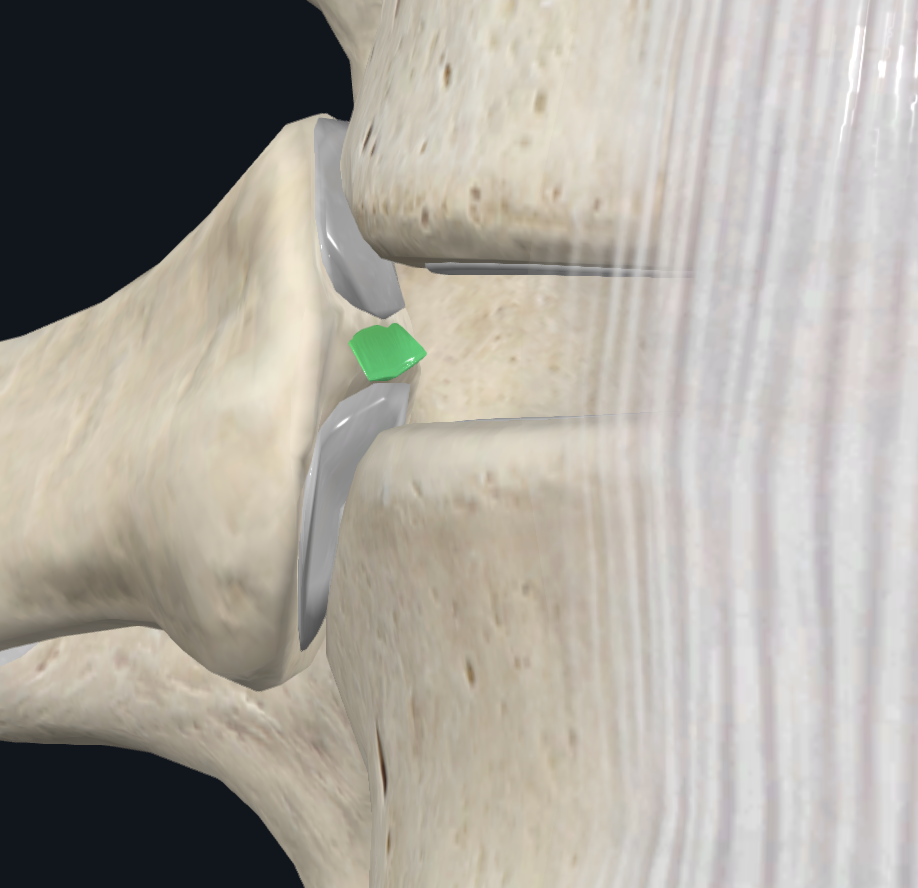
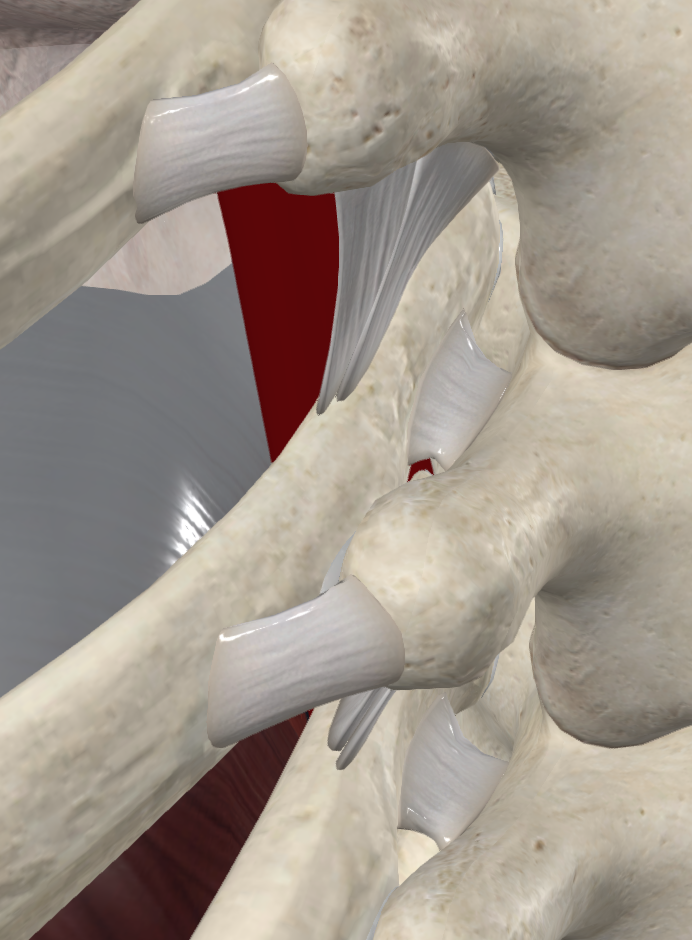
Costotransverse joint
A synovial joint stabilized by ligaments that is formed between the tubercle of the rib & the transverse process of the vertebra
Ligaments —
Costotransverse ligament —
Attaches medial to the joint on the vertebrae & neck of rib
Costo – the first to the rib
Transverse – referred to the vertebrae – transverse process
Thus, ligament that fills the gap between the rib & the transverse process of the vertebrae
Lateral costotransverse ligaments —
Lateral to the joint, attaches the tip of the transverse process to the non-articular part of the rib tubercle
Lateral – because between the tip of the transverse process of the vertebrae & the rough part of the tubercle
Tubercle of each rib is divided into 2 different parts — 1 smooth, with the facet for the articulation with the rib, and 1 rough, for the articulation with the lateral costotransverse ligament
Superior costotransvere ligament —
Attaches the superior surface of the neck of the rib to the transverse process of the vertebra above
Fills gap between superior border of the neck of the rib & the inferior border of the transverse process of the vertebrae above
Overall —
Costotransverse ligament — before the costotransverse joint, lateral — directly after, superior — from rib above where costotransverse ligament attaches to bottom of transverse process of vertebra above
Functions —
Along with the ligaments permit a level of mobility of the rib cage essential for thoracic cavity volume alteration during breathing
The middle part of each rib is inferior to its 2 ends — thus, when this region is elevated, it expands the thoracic wall laterally with the posterior attachment higher than the anterior one.
Essentially, when one rib is elevated is moved the anterior thoracic wall forward (relative to posterior wall)
Sternocostal joints
Joints between the upper 7 costal cartilages & the sternum
Joint between Rib I & manubrium —
Not synovial — fibro-cartilaginous
Joint between Rib II-VII & manubrium —
Synovial joints with thin capsules reinforced by sternocostal ligaments
The joint between the second costal cartilage & the sternum is divided into 2 compartments by an intraarticular ligament —
Attaches the 2nd costal cartilage to the junction of the manubrium & body of the sternum
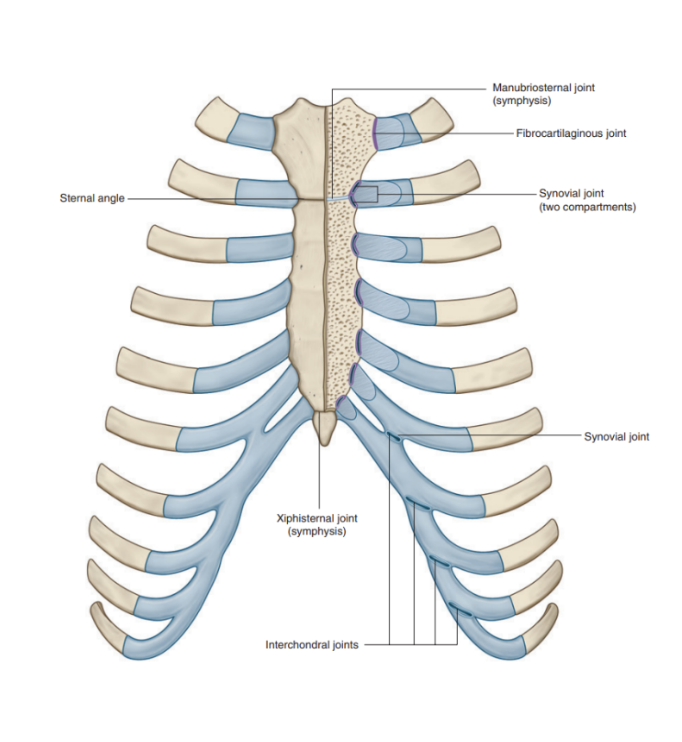
Interchondral joints —
Provide an indirect anchorage to the sternum & contribute to the formation of a smooth inferior costal margin — usually occurs between the costal cartilages of adjacent ribs
Mainly occurs between —
Costal cartilages of ribs VII to X, but may also involve those of ribs V & VI
Manubriosternal and xiphisternal joints
Manubriosternal joint —
Joints between the manubrium and the body of the sternum
Xiphisternal joint —
Between the body of the sternum and the xiphoid process
These joints are usually symphyses. They serve as important landmarks
Structures behind the sternum and first two ribs (detail more for vessels) —
Heart
Lungs (pleural cavities)
Nerves
Arteries —
Left & right subclavian arteries —
Branching of the vertebral artery (within cervical area — passes through foramen magnum & in upper limb)
Supplies the trunk, spinal cord, head, brain, meninges, & upper limb
Brachiocephalic trunk
Left & right common carotid arteries
Fundamental to supply the head & brain
Veins —
Left & right brachiocephalic veins —
Origin of internal jugular veins that drain the skull, brain, face, & neck
Left & right subclavian veins —
Origin of the external jugular veins that drain the face, scalp, and neck
Posteriorly to the veins & arteries, we find the esophagus & trachea
Clinical drop — fracture of the sternum
Most commonly caused by blunt, anterior chest-wall trauma & deceleration injuries
3-6.8% in motor vehicle collisions
Athletic injuries, fals, and assaults — frequent causes on remaining cases
Effect on different demographics —
Within adults & elderly —
Life threatening condition, caused by a lack of elasticity that occurs with aging
Within children —
Due to elasticity, all mechanical forces are transferred in the organs contained in the mediastinum —
Thus, rare to find a fracture of sternum/ribs in children but much more likely to have internal organ injuries
Superior & inferior thoracic aperture
Rib superior margin – superior thoracic aperture – starts anteriorly from the jugular notch, then following the medial margin/border of the clavicle, reaches the anterior border/spinous process of the first thoracic vertebrae
Here the angle between the manubrium & body of the sternum is seen marking the beginning of rib 2 – when palpated and move laterally, can feel rib 2
Inferiorly, the thoracic aperture follows the inferior margin of the ribcage & is closed by the diaphragm
In the diaphragm, there are some passages to allow the passage of the organs that from the thorax go to the abdomen
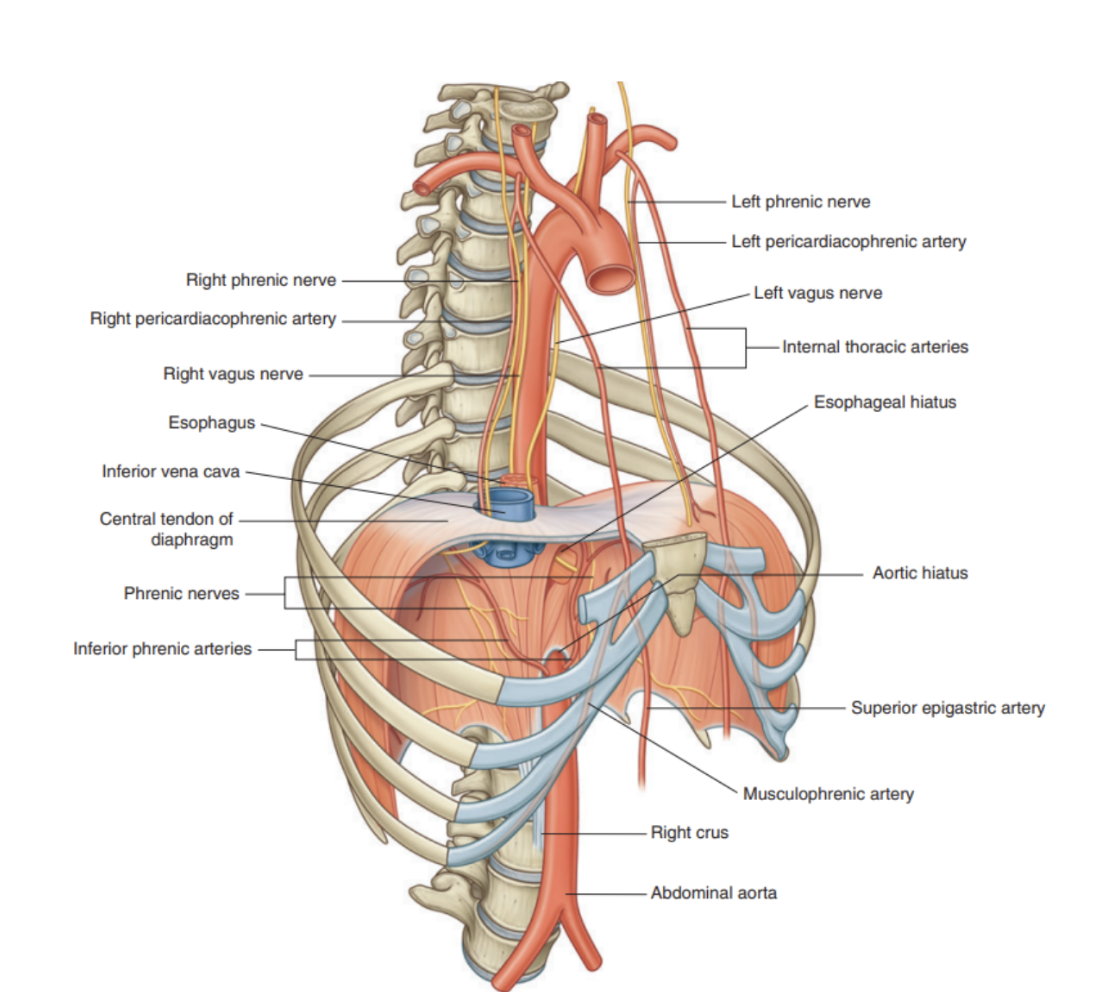
Diaphragm (ligaments) --
Dome shaped, origin is on the vertebral column in the lumbar region
Starts with 2 ligaments called right & left crus
Right crus is attached to LIII vertebrae
Left crus is attached to anterior side of body to LII, anterior disc, and L1
Both ligaments join together along the midline with a ligament called median arcuate ligament
Starts from LII and follows inferior part of vertebrae L1, with its final insertion on the transverse process of L1
When moving to lateral side, there is another ligament – lateral arcuate ligament
On the left and on the right – starts from transverse process of L1 and ends on the tip of the false rib 12
Also the superior part of the anterior layer of the thoracolumbar fascia that goes down to cover the quadratus lumborum muscle (latissisim dorsi muscle) muscle
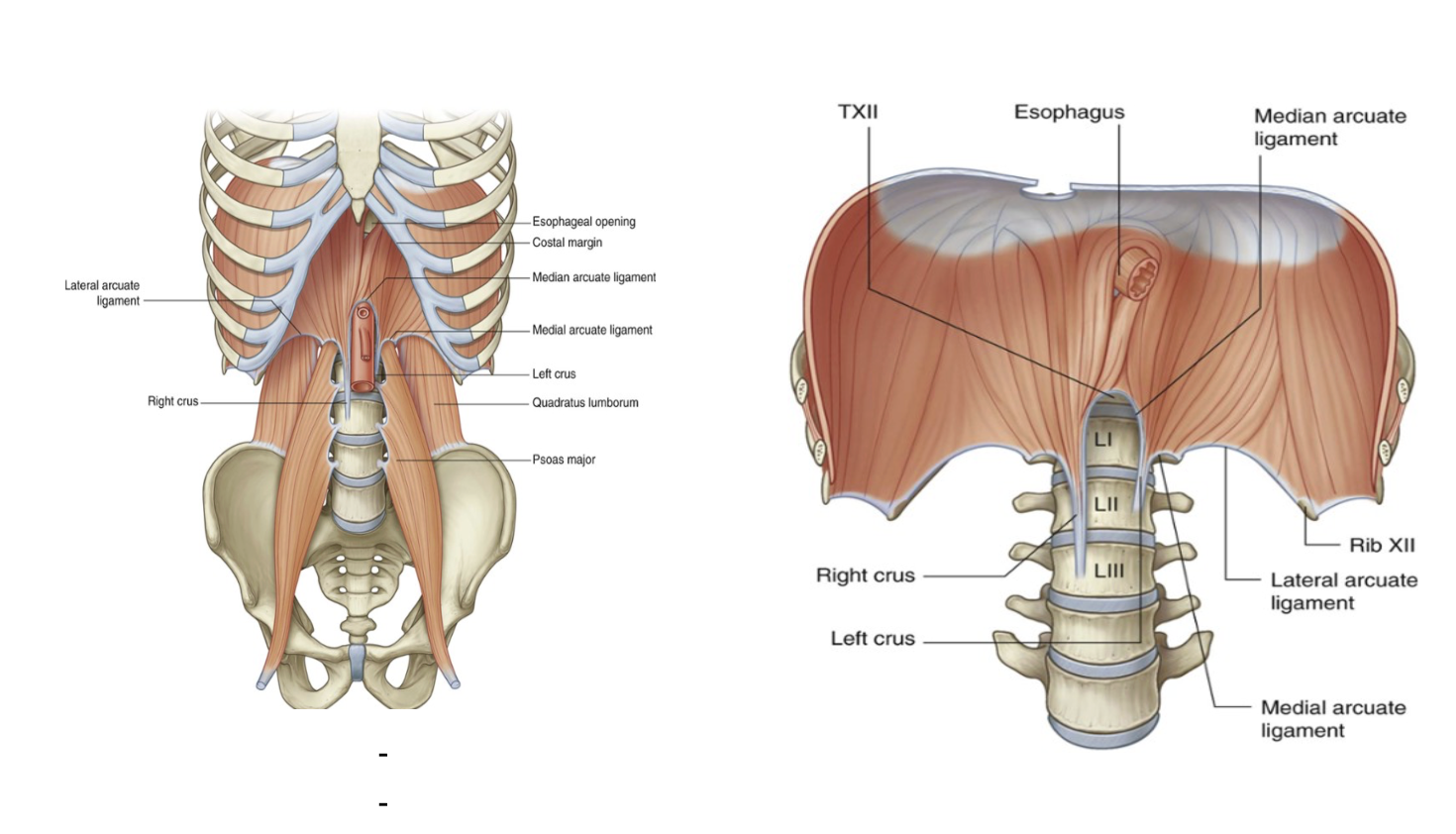
Origin of diaphragm –
Between transverse process of L1 & tip of rib 12, there is a thickening of these fascial layers, that at that point goes up with the muscle fibers to give the origin of the diaphragm
What passes through the diaphragm? –
The inferior vena cava passes through the central tendon at approximately vertebral level TVIII
The esophagus passes through the muscular part of the diaphragm, just to the left of midline, approximately at vertebral level TX.
The vagus nerves pass through the diaphragm with the esophagus.
The aorta passes behind the posterior attachment of the diaphragm at vertebral level TXII.
The thoracic duct passes behind the diaphragm with the aorta.
The azygos and hemiazygos veins may also pass through the aortic hiatus or through the crura of the diaphragm.
This means, that during contraction, the diaphragm can affect the venous drainage – not aorta (because posterior), but yes inferior vena cava, because goes through — opening can widen during inspiration – increase of the venous drainage that goes to the right chambers of the heart
During expiration – this foramen narrows, thus reducing the blood flow to the heart
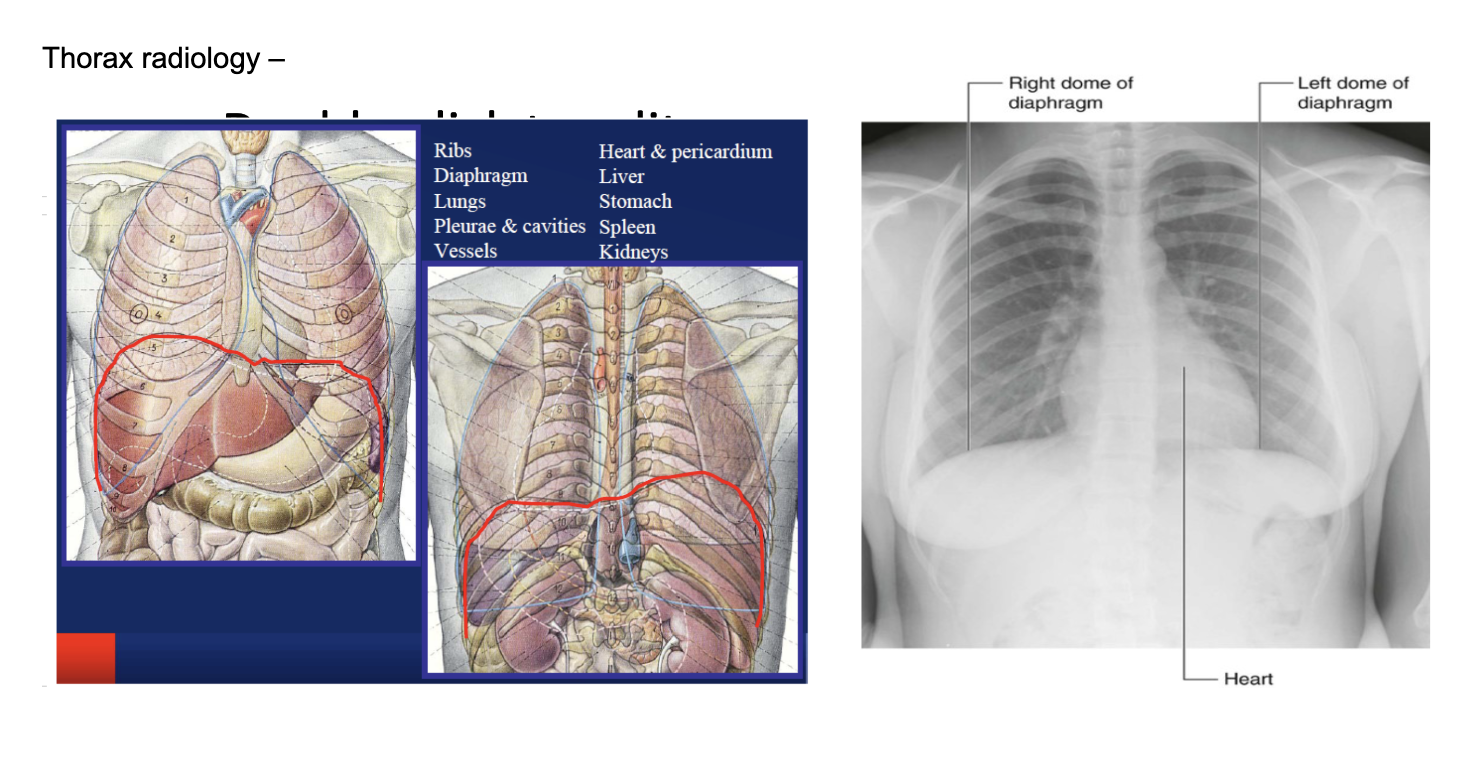
Thorax radiology – (images)
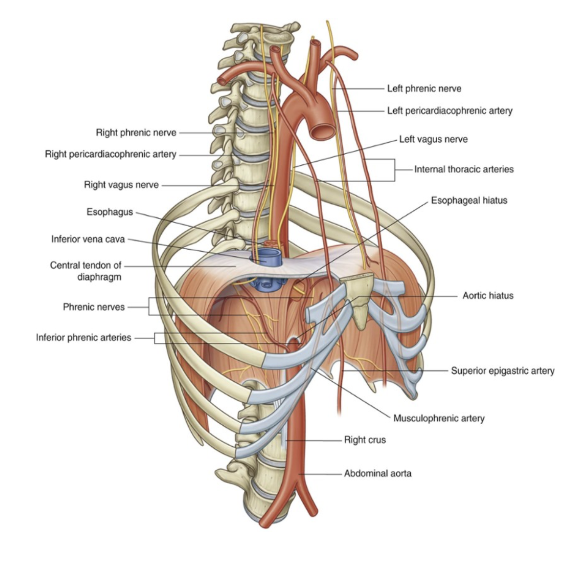
Arterial supply of the diaphragm
The arterial supply originates from vessels that arise superiorly & inferiorly to it from above —
Pericardiiacophrenic & musculophrenic arteries
Branches of the internal thoracic arteries
Superior phrenic arteries
Originate directly from lower parts of the thoracic aorta
Small branches from intercostal arteries
Inferior phrenic arteries
Branch directly from the abdominal aorta, arising below the diaphragm & are the largest arteries that supply the diaphragm
Venous drainage of the diaphgram
Occurs by veins that generally parallel the arteries — draining into —
Brachicephalic veins in the neck
Azygos system of veins
Abdominal veins (left suprarenal vein & inferior vena cava)
Basically — pericardiacophrenic vein same course as artery, but coming from brachicephalic vein, musculophrenic vein coming in same way from internal thoracic vein (attaches to brachiocephalic), superior phrenic coming from hemiazygos before going through diaphragm, inferior phrenic coming from inferior vena cava
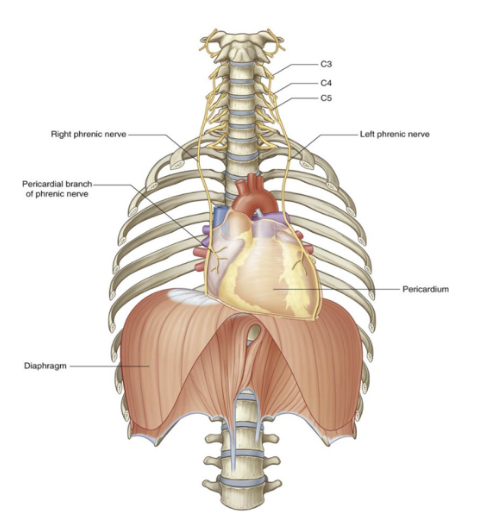
Innervation of the diaphragm
Motor innervation
2 phrenic nerves that originate as branches of the cervical plexus in the neck
Arise from the anterior rami of cervical nerves C3, C4, and C5 (most important = C4)
They descent vertically through the neck, superior thoracic aperture, & mediastinum
such high origin of nerves is due to embryological development
Any injury below the interested segments will not affect the diaphragm
Sensory innervation —
Pain & proprioception at the central tendinous part is innervated by the phrenic nerves while the periphery muscular portions are innervated by 6th to 11th intercostal nerves
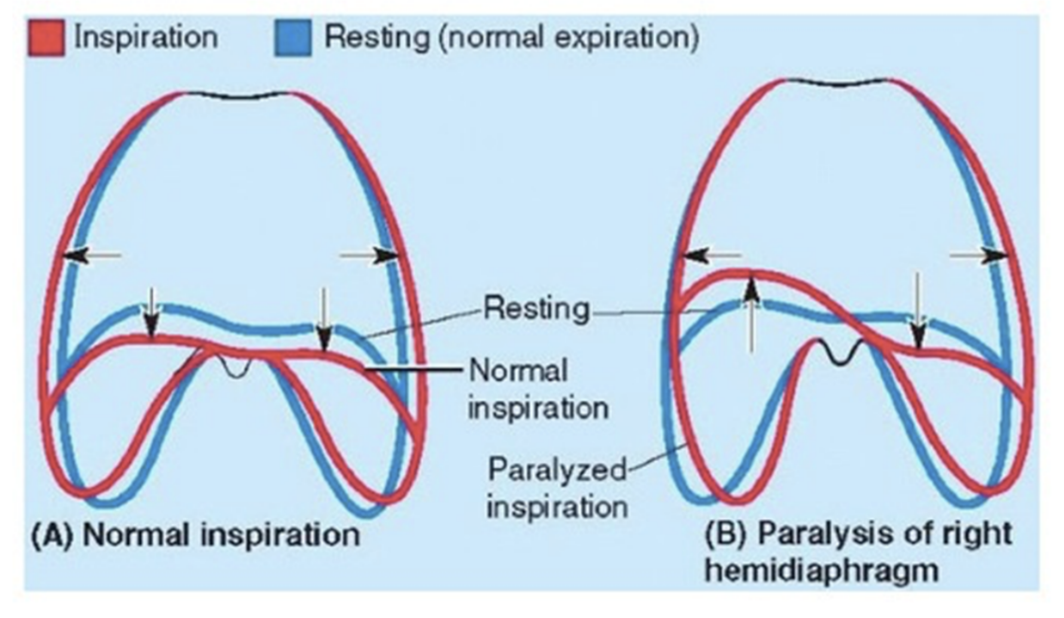
Clinical drop — paralysis of diaphragm
Paralysis of half of the diaphragm (one dome) due to injury to its motor supply from the phrenic nerve does not affect the other half because each dome has a separate nerve supply
We can detect paralysis radiographically by noting its paradoxical movement —
Instead of descending as it normally does during inspiration (contraction), the paralyzed dome ascends as it is pushed superiorly by the abdominal viscera that are being compressed by the active contralateral dome —
Instead of ascending during expiration, the paralysed dome descends in response to the positive pressure in the lungs