Pelvic Girdle Arthropathies and Groin Pain Pathologies
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
What are spondyloarthropathies?
Inflammatory arthritic conditions characterized by pain and stiffness, often asymmetric and involving lower extremities.
What is the most common form of spondyloarthropathy?
Ankylosing Spondylitis, a chronic rheumatoid disorder that is usually progressive.
How does ankylosing spondylitis differ in prevalence between genders?
It is more common in men for spinal involvement, while women are more affected in peripheral joints.
What is a common symptom associated with pelvic girdle issues?
Groin pain, which can be difficult to evaluate and presents similarly across various pathologies.
List some conditions that can cause groin pain.
Adductor muscle strain, prostatitis, orchitis, inguinal hernia, urolithiasis, ankylosing spondylitis, Reiter Syndrome, hyperparathyroidism, metastasis, osteitis pubis, stress fracture, conjoint tendon strains, inguinal ligament enthesopathy, entrapment of the lateral cutaneous nerve of the thigh.
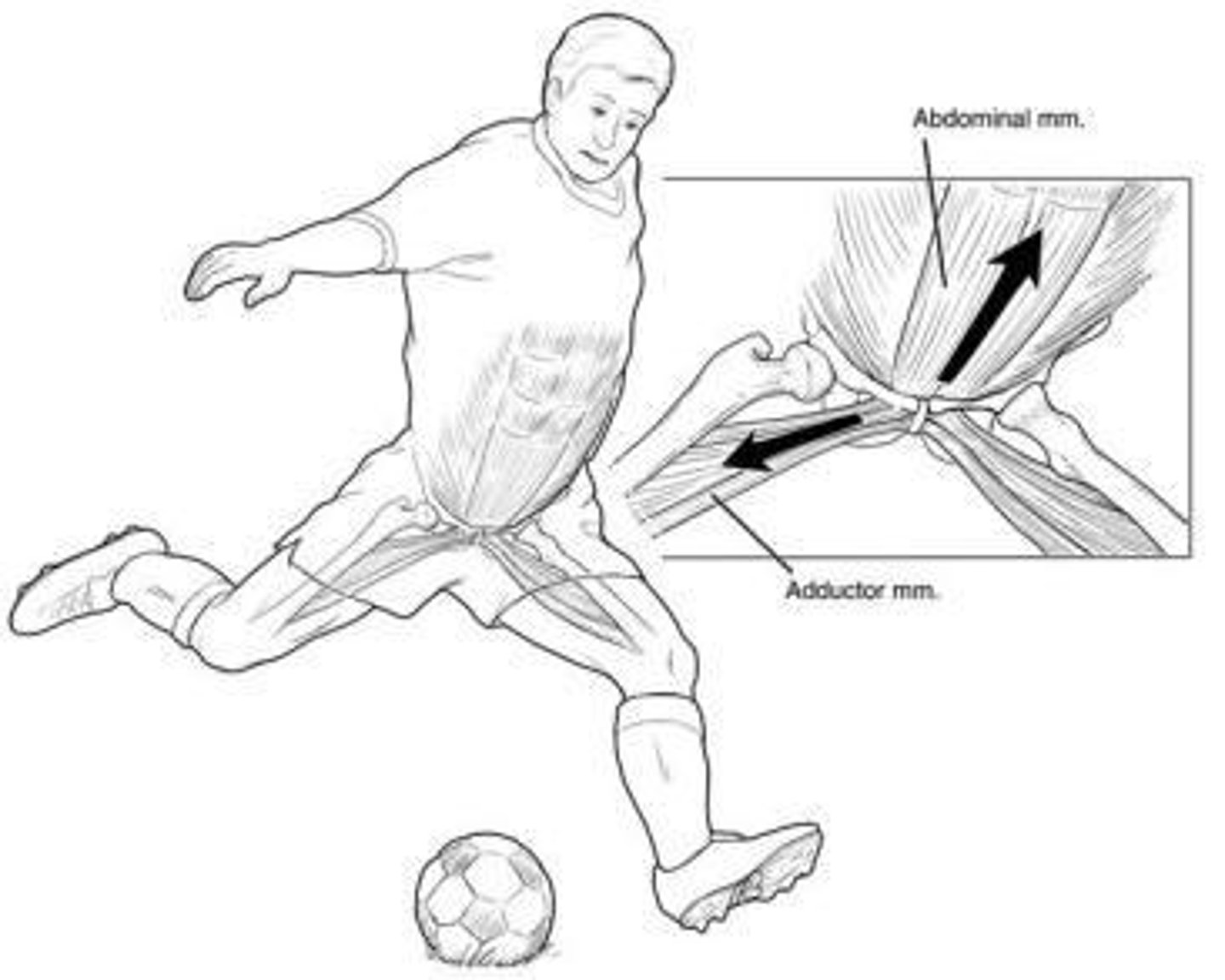
What is the most common form of groin pain pathology?
Osteitis Pubis/Athletic Pubalgia.
What is the etiology of osteitis pubis?
The exact cause remains unclear, but there is an association with ROM limiting hip disorders and overuse injuries.
What activities are associated with osteitis pubis?
Activities that create continual shearing forces at the pubic symphysis, such as running, race-walking, gymnastics, soccer, basketball, rugby, and tennis.
What age group is most commonly affected by osteitis pubis?
Individuals in their third and fourth decades of life, more commonly in men.
What are common symptoms of osteitis pubis?
Gradually increasing activity-related lower abdominal and proximal adductor-related pain, described as 'groin burning,' with discomfort while climbing stairs, coughing, or sneezing.
What physical examination findings are associated with osteitis pubis?
Pain at the pubic tubercle and pubic symphysis, elicited pain with resisted adductor contraction, and potential decreased ROM in one or both hips.
What are the four stages of osteitis pubis according to Rodriquez et al.?
I. Unilateral kicking leg pain worsening after training; II. Bilateral inguinal pain worsening after training; III. Bilateral inguinal and lower abdominal muscle pain worsening with kicking, sprinting, changing direction, long walks, and transitioning from sit to stand.
What is a common diagnostic test for osteitis pubis?
The FABER test, which may show limited abduction and adductor muscle spasm.
What can Valsalva maneuvers indicate in osteitis pubis?
They can occasionally reproduce symptoms, indicating pelvic girdle pathology.
What is the role of hip joint evaluation in osteitis pubis?
To rule out intra- or extra-articular hip pathology that may contribute to symptoms.
What is the significance of early diagnosis and management of osteitis pubis?
It is important to prevent a high degree of disability associated with the condition.
What is the relationship between osteitis pubis and biomechanical abnormalities?
Overuse is likely the etiology of inflammation, which may be associated with several biomechanical abnormalities.
What is the typical presentation of osteitis pubis in athletes?
Athletes typically complain of gradually increasing activity-related lower abdominal and proximal adductor-related pain.
What might be detected during daily activities in someone with osteitis pubis?
A soft-tissue mass with calcification and an audible or palpable click over the symphysis.
What is the common presentation of groin pain in pelvic girdle pathologies?
It presents similarly across various conditions, often just as a complaint of groin pain.
What is the importance of palpating the pubic tubercle and symphysis during examination?
These areas may be painful in up to 22% of patients with osteitis pubis.
What are common symptoms of bilateral inguinal pain associated with pubic symphysis dysfunction?
Pain worsens with defecation, sneezing, walking, and prevents activities of daily living (ADL) performance.
What positions can the pubic symphysis be found in?
Anteroinferior, posterosuperior, anterosuperior, and posteroinferior.
What indicates a significant altered positional relationship within the pelvic girdle?
A mobility restriction of the sacroiliac joint (SIJ) or pubic symphysis.
What is typically tender to palpation on the side of impairment in pubic symphysis dysfunction?
The inguinal ligament.
What is the primary treatment approach for dysfunction of the pubic symphysis?
Manual techniques are used to treat these articular dysfunctions.
What is the conservative intervention for osteitis pubis?
Rest from weight-bearing activities, nonsteroidal anti-inflammatory medication, and physical therapy.
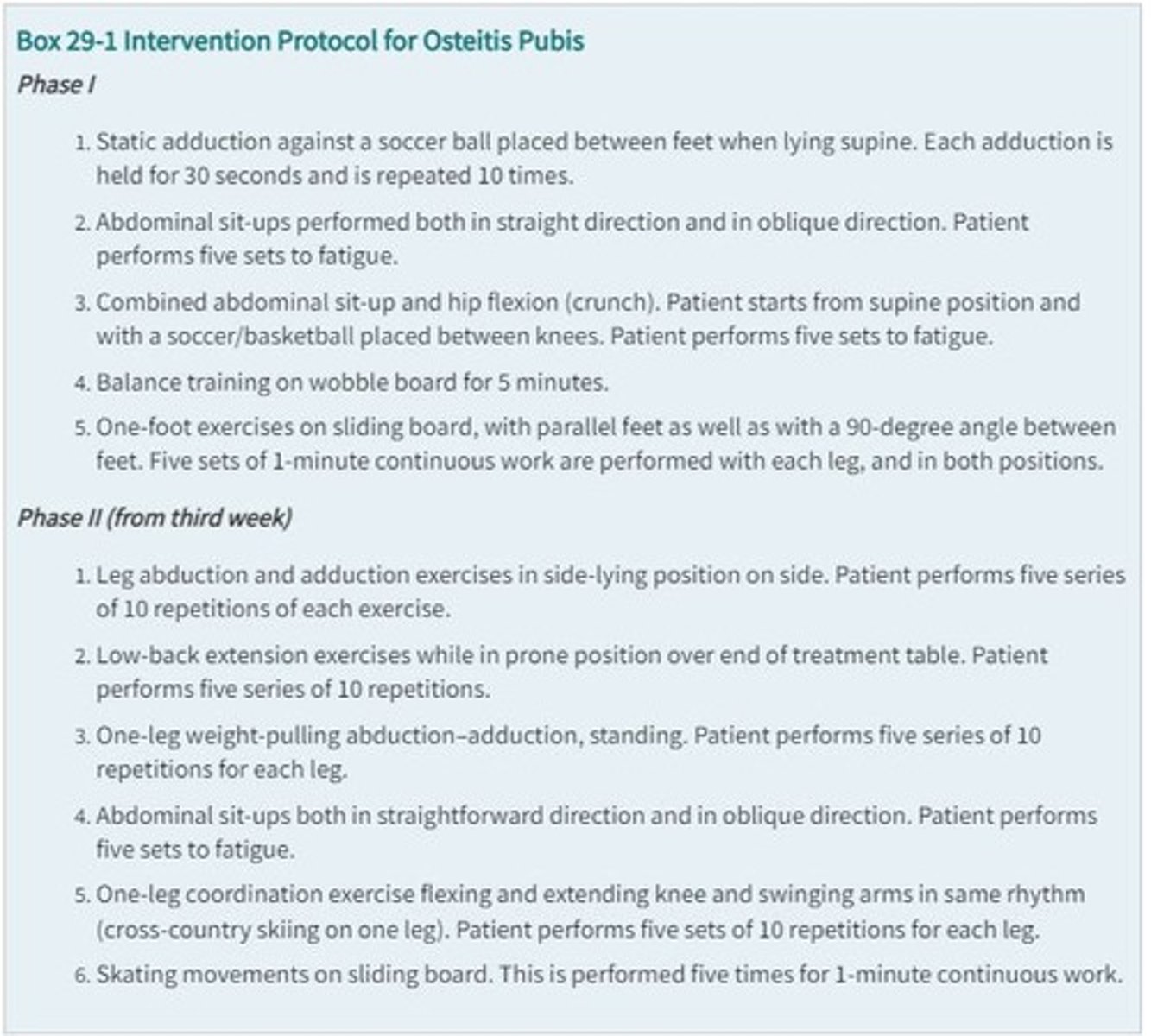
What should rehabilitation for osteitis pubis focus on?
Core stabilization, postural retraining, and normalization of the dynamic relationship of hip and pelvis muscles.
What activities should be avoided during recovery from osteitis pubis?
Deep hip flexion and low repetition, heavy weight strength training.
What is diastasis symphysis pubis (DSP)?
An increase in the gap between the pubic symphysis that can increase as much as 9 mm.
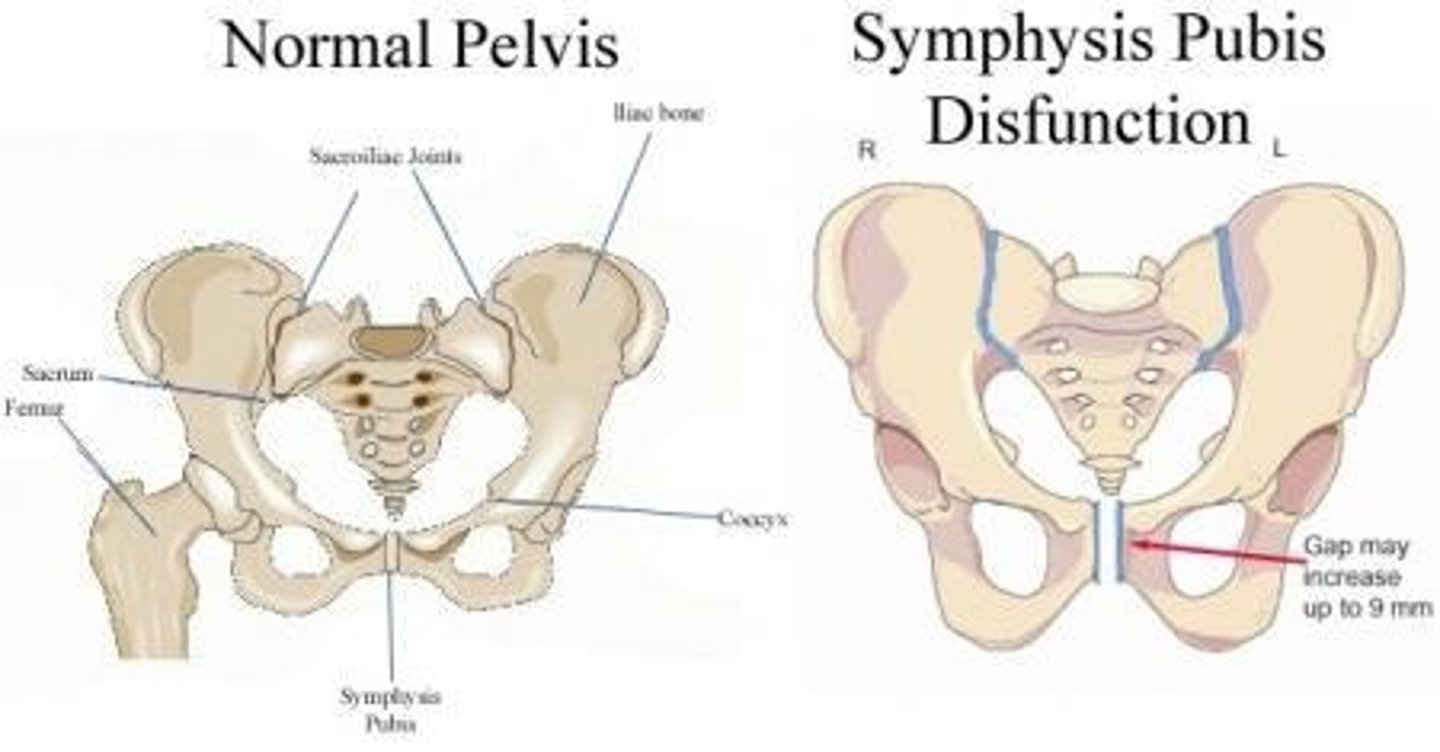
What causes symphysis pubic dysfunction (SPD) during pregnancy?
Ligamentous laxity in response to the hormones progesterone and relaxin.
What are common symptoms of SPD?
Pain with activities involving lifting one leg or parting the legs, and an antalgic waddling gait.
What objective findings are typically present in a patient with SPD?
Tenderness over the anterior pubic symphyseal area, limited hip movements due to pain, and inability to perform unilateral standing.
What can be felt or heard during palpation of the pubic symphysis in SPD?
Occasional clicking.
What findings on physical examination indicate SPD?
Positive sacroiliac joint (SIJ) stress tests and tenderness over the anterior pubic symphyseal area.
What is the relationship between the severity of symptoms and treatment for SPD?
Intervention is based on the severity of symptoms rather than the degree of separation measured by imaging.
What activities may evoke characteristic pain in SPD?
Bilateral pressure on the trochanters or hip flexion with legs in extension.
What is the typical gait pattern observed in patients with SPD?
An antalgic, waddling gait.
What is the significance of palpating the position of the pubic tubercles?
It helps determine the impairment pattern by correlating findings with the side of the positive kinetic test.
What is the role of physical therapy in the treatment of osteitis pubis?
To gently mobilize, stretch, and strengthen the muscles of the groin.
What is a common outcome for athletes recovering from osteitis pubis?
Most athletes return to their respective sports within a few days to weeks.
What type of pain is associated with SPD when performing certain activities?
Severe pain or muscle spasm may occur during certain maneuvers.
What is the importance of considering SPD in postpartum patients?
It should always be considered when examining patients experiencing suprapubic, sacroiliac, or thigh pain.
What are the three types of diastasis symphysis pubis?
Type I: Minor anterior damage and mild (<2.5 cm) pubic symphysis diastasis; Type II: Wide diastasis with disruption of the anterior SI ligament complex; Type III: Total disruption of the SIJ with diastasis greater than 2.5 cm.
What is a recommended sleeping position for managing symphysis pubic dysfunction?
Use a pillow between the legs and keep the legs and hips parallel and symmetrical when moving or turning in bed.
What should patients avoid when managing symphysis pubic dysfunction?
Avoid sudden movements and sit down when putting on pants or socks.
What conservative management strategies are suggested for symphysis pubic dysfunction?
Bed rest in lateral decubitus position, pelvic support with a brace, ambulation with assistive devices, and graded exercise progression.
How long do symptoms of symphysis pubic dysfunction typically last?
Symptoms usually resolve in approximately 6-8 weeks with no lasting sequela.
What activities may help relieve pressure on the joint in symphysis pubic dysfunction?
Swimming (except breaststroke) and deep-water aerobics using flotation devices.
What surgical interventions may be considered for severe cases of symphysis pubic dysfunction?
Surgical intervention may be utilized in cases of inadequate reduction, recurrent diastasis, or persistent symptoms.
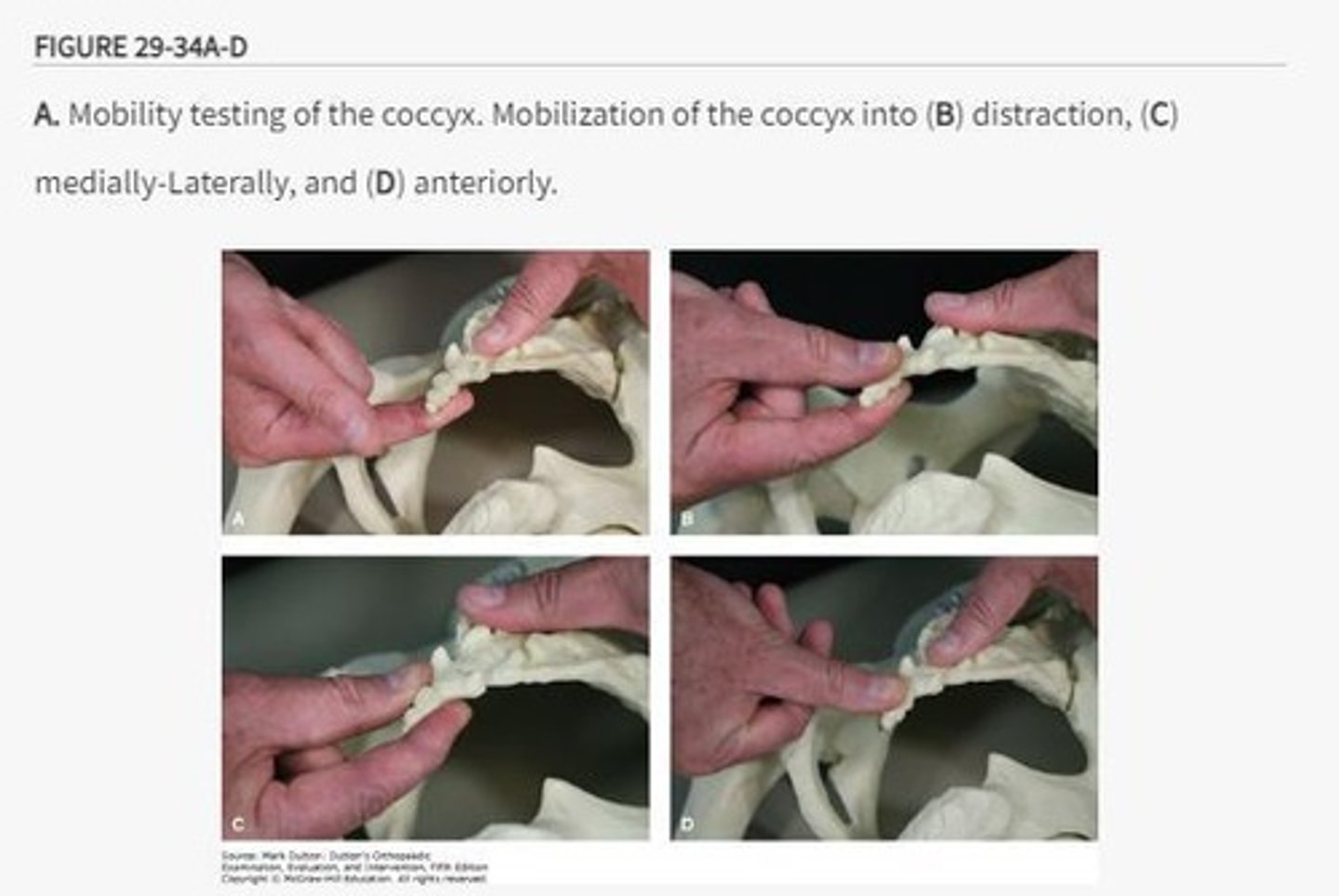
What is coccydynia?
A painful condition related to the coccyx that may be caused by trauma, pregnancy, obesity, or other unidentified causes.
Which demographic is more likely to experience coccydynia?
Women are four times more likely to have symptoms, and individuals with a higher body mass index are three times more likely to develop it.
What are the ligaments that can be injured in coccydynia?
Anterior (ventral), lateral sacrococcygeal, anterior ligament of the coccyx, posterior (dorsal), superficial and deep posterior sacrococcygeal, and intercornual ligament.
What is the dominant muscle associated with coccydynia?
The levator ani.
How is coccydynia diagnosed?
Diagnosis is based on clinical presentation and may involve static-view radiological imaging to identify coccyx displacement.
What conservative management strategies are typically used for coccydynia?
Nonsteroidal anti-inflammatory drugs, manual therapy, and local cortisone injections.
What is the procedure for manual therapy in coccydynia?
The clinician grasps the coccyx with one hand while stabilizing the pelvis with the other, assessing movement in the anterior-to-posterior direction.
What is the significance of imaging in diagnosing coccydynia?
Dynamic imaging may assess abnormal mobility by comparing the coccyx position in standing versus seated positions.
What is the role of patient education in managing symphysis pubic dysfunction?
Providing advice on how to avoid stress to the area is crucial for effective management.
What is the expected outcome for patients with coccydynia?
Symptoms may resolve with conservative management, but some cases may require further intervention.
What is the importance of verbal consent in the examination of coccydynia?
Given the intrarectal nature of the examination, it is critical to explain the procedure and obtain consent.
What are the potential causes of coccydynia?
Trauma, pregnancy, obesity, or other unidentifiable causes.
What is the typical intervention for restricted mobility in coccydynia?
The coccyx can be distracted or mobilized in various directions to improve mobility.
What is the role of pelvic support in managing symphysis pubic dysfunction?
Pelvic support with a brace or girdle helps stabilize the area and alleviate symptoms.
What is the significance of the anterior SI ligament complex in symphysis pubic dysfunction?
Disruption of this complex is associated with Type II diastasis of the symphysis pubis.
What is the relationship between coccydynia and body mass index?
Individuals with a higher body mass index are more likely to develop coccydynia.