ihs 340 exam 1 content
1/164
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
165 Terms
the problem this course addresses. . .
allergy prevalence has greatly increased over the past century or so
deadliest pandemics in history
measles, black death, HIV/AIDS, smallpox, spanish flu, cholera, typhus, COVID, tuberculosis, etc.
why is tuberculosis the biggest killer?
not only can it cause death, but if infected individuals don’t die, it has a great effect on the immune system after infection
hidden story in list of leading causes of death in the US
diseases like cancer, heart disease, stroke, etc. all have microbial components
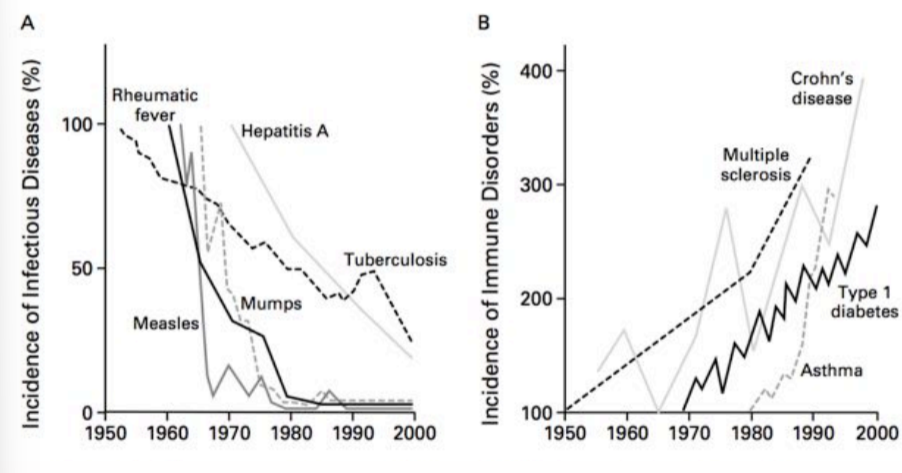
what is the relationship between incidence of infectious diseases and the incidence of immune hypersensitivity diseases?
inverse
infection
the invasion of an organism’s body tissues by a disease-causing agent
the multiplication or metabolically-active persistence of those agents
reaction of host tissues to the infectious agents and any toxic compounds they produce
has always existed
infectious disease
disease that can result from infection by a transmissible agent (passed from host to host)
hasn’t always existed
ex. measles is an infectious disease that will die out in small populations, because it needs a sufficient number of hosts
endemic level of disease
baseline, the amount of a particular disease that is usually present in a community over a sustained period of time
ex. the cold, the flu, COVID
endemic
the constant presence and/or usual prevalence of a disease or infectious agent in a population within a geographic area
sporadic
a disease that occurs infrequently and irregularly
hyperendemic
persistent, high levels of disease occurrence
epidemic
often sudden increase in the number of cases of a disease above what is normally expected in that population in that area
outbreak
same definition as epidemic, but often used for a more limited geographic area
cluster
aggregation of cases grouped in place and time that are suspected to be greater than the number expected, even though the expected number may not be known
pandemic
an epidemic that has spread across the globe, usually affecting a large number of people
allergen
an environmental antigen that typically elicits allergic responses (“a hyper-sensitive immune response”) in susceptible individuals, non-infectious
antigen
a substance that induces an immune response in the body
is specifically bound by antibodies or T lymphocyte antigen receptors
what largely mediates the allergic response?
mast cells
mast cells location and action
prominent in mucosal and epithelial tissues, high numbers found in mucosal surfaces of respiratory and GI tract
also located in subendothelial connective tissue
can have limited local response or life-threatening systemic response (anaphylaxis)
key structure of mast cells
they have granules full of mediators released when the cell gets activated
the activation and effect of mast cells is very quick because they’re pre-formed and loaded with these mediators
atopy
the propensity for developing allergy diseases (asthma, food allergies, seasonal allergies, etc.)
defined operationally by elevated serum levels of allergen-binding IgE or by skin test reactivity to allergens
asthma
a heterogenous disease usually characterized by chronic airway inflammation, involving history of wheezing, SOB, chest tightness, etc. varying over time and intensity
is asthma an allergic disease?
about half of the people with asthma have allergic asthma, other half have non-allergic asthma
contributing factors in pathogenesis of asthma
occupation exposures, exposure to microbial organisms, infections, diet, pollution, stress, poverty, etc.
anaphylaxis
immune system releases flood of chemicals that causes the body to go into shock, BP drops suddenly, airways can become blocked, nausea, vomiting, skin rash, fast and weak pulses also common
conditions mistakenly associated with food allergies
ADD/ADHD, celiac disease, food intolerances, etc.
mucosa
soft tissue that lines the body’s canals and organs in the digestive, respiratory and reproductive systems
inside the body but exposed to the outside world
environment-gene interactions underlying allergic diseases
environmental factors like level of development in a country, family size, home location, antibiotic use, sanitation levels are driving factors for developing allergic disorders or not
genes are modifying factors for developing allergic disorders or not
robert hooke
built the first compound microscope, observed mold and lice
published Micrographia
coined the term cell
antonie van leeuwenhoek
built single-lens magnifiers
first to observe single-celled microbes, called them animalcules
credited with advancing the field of microbiology
microbe
single-celled organism
why are sizes of microorganisms relevant?
it determines how the immune system deals with the microorganism and how it spreads
gram-positive bacteria
stains purple
has peptidoglycan cell call
gram-negative bacteria
stains pink
has an inner and outer membrane with a thin peptidoglycan wall in between
fungi
eukaryotic microbes
more than 100,000 species
unicellular and multicellular forms exist (yeast, molds)
parasitic disease
majority occur in the tropic and sub-tropical regions
parasites include protozoa and helminths
usually 2 hosts to complete life cycle
florence nightingale
English social reformer, statistician, and founder of modern nursing
john snow
traced the source of the london cholera outbreak of 1854, although his work was mostly ignored because it was before germ theory was accepted
louis pasteur
started as organic chemist
discovered the microbial basis of fermentation
disproved that microbes arise by spontaneous generation
francesco redi
experimented to disprove spontaneous generation of flies on meat
pasteur’s experiments disproving spontaneous generation of microbes
microbes come from dust particles in the air, not coming from the air or from the broth used in the experiment
pasteurization
process of heating a liquid to below the boiling point to destroy microorganisms but retain flavors of the liquid, first developed for wine
mary catherine evans
showed that drinking unpasteurized milk could transmit brucellosis-causing bacterium from domestic farm animals to humans
ignaz semmelweis
discovered infectious nature of puerperal fever and developed antisepsis technique (washing with chlorinated lime water) to prevent the condition
joseph lister
developed carbolic acid to treat wounds and clean surgical instruments
aseptic
environment is microbe-free
puerperal fever
aka childbed fever, infection of some part of the female reproductive organs following childbirth or abortion
phenol usage and history
aka carbolic acid, the oldest surgical antiseptic but no longer used even as disinfectant because of corrosive effect on tissues and instruments and carcinogenic effects
disinfectants
strong chemical agents that inhibit or kill microorganisms, strong enough to cause tissue damage
antiseptics
disinfecting agents with low toxicity to host cells, can be used on skin, wounds, or mucous membranes, subclass of disinfectants
sterilants
kill both vegetative bacterial cells and bacterial spores when applied to materials for appropriate times and temperatures
classifications of antiseptics and disinfectants
those that denature proteins
those that cause osmotic disruption of the cell
first two kill microorganisms
those that interfere with specific metabolic processes
third one affects cell growth and reproduction without killing the cell
phenol, iodine, alcohols, aldehydes and metallic compound mechanism of action
denature proteins and DNA bases
cationic detergents mechanism of action
interfere with plasma membrane’s permeability and cause leaking of enzyme, coenzyme and metabolites
oxidizing compounds mechanism of action
oxidize functional molecules in the microorganisms
history of listerine
named listerine because dr. lawrence was a fan of joseph lister
was promoted to dentists as mouthwash but wasn’t very popular until ads started running about halitosis (bad breath)
essentially the disease was created with the cure at the ready
robert koch
discovered that using solid media provided simple way to get pure cultures
observed that masses of cells (colonies) had different morphologies
why was growing a pure culture of microorganisms needed?
to prove a particular bacterium caused a specific disease
angelina and walther hesse
developed solid medium using agar as improvement over gelatin (bacteria ate the gelatin)
julius richard petri
developed double-dish container to culture bacteria
koch’s postulates
criteria used to establish causative link between an infectious agent and disease
microbe is found in all cases of the disease but is absent from healthy individuals
the microbe is isolated from the diseased host and grown in pure culture
when the microbe is introduced into a healthy, susceptible host, the same disease occurs
the same strain of microbe is obtained from the newly diseased host
rabies vaccine
created by louis pasteur, he attenuated the disease from rabbit to rabbit, eventually causing mild disease but protecting against the real disease
how did we learn that viruses are different from bacteria?
iwanowski and beijerinck separately proved that virus from diseased tobacco plants wasn’t diluted with filtration even fine enough to retain smallest bacteria, and it was replicating because it wasn’t diluted between newly infected plants
sterilization by filtration
filtration avoids use of heat on sensitive liquids and gases to sterilize
virus
metabolically inert sub-cellular agent that can infect specific types of living cells and replicate while inside the cell
does not exhibit “free-living” or “independent” growth
RNA viruses need RNA replicases
retroviruses carry reverse transcriptase
virion
virus particle, consists of nucleocapsid (capsid/protein coat and nucleic acid)
two categories - naked and enveloped in lipid envelope
capsomeres
repeating protein subunits that make up capsid
virus morphology
typically smaller than bacteria, highly symmetric
enveloped viruses
have envelop/lipid bilayer surrounding nucleocapsid with embedded proteins
envelop makes initial contact with host cell
much of the membrane is picked up from the host cell during exit
most infect animal cells
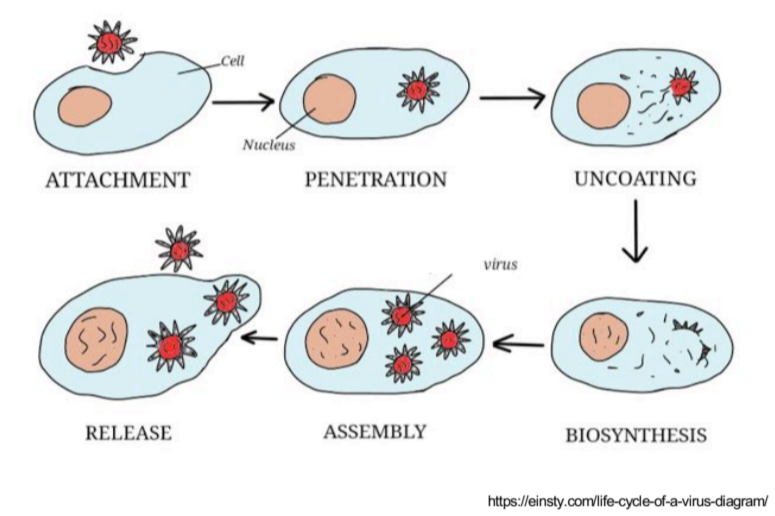
phases of virus life cycle
attachment of virus to susceptible host cell
entry of virion or its nucleic acid
synthesis of virus nucleic acid and protein by cell metabolism as redirect by virus
assembly of capsids and packaging of viral genomes into new virions (maturation)
release of mature virions from host cell
passive barriers to infection
lysozymes, mucus and cilia, blood and lymph proteins, skin, stomach acidity, flushing of urinary tract, epithelial cells
three layers of mucosa
epithelium - single cell wide
lamina propria - loose connective tissue
muscularis mucosa - smooth muscle
layers of the epidermis
stratum corneum, lucidum, granulosum, spinosum, basale
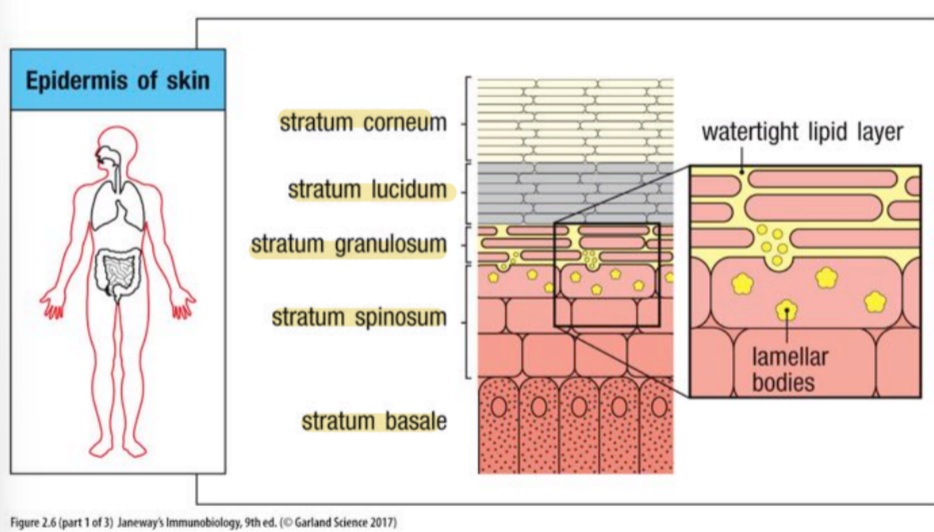
epithelial surfaces. . .
provide first barrier against infection and against dehydration
airway anatomy
anatomically contiguous surface
oral and nasal cavities have a significant resident microbiota
alveoli not mucus-covered, lipid-covered (surfactant) which allows them to open and close
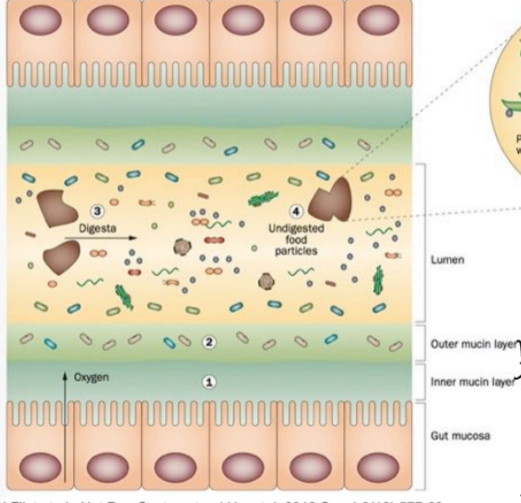
gut microbiome
architecture largely determined by diet and physiochemical gut conditions
pH gets higher when going from stomach to colon
as pH increases, so does load of bacteria
mucosal layer prevents microorganisms from engaging directly with the epithelial surface in healthy individuals
mucous membrane in GI tract composition
mucus and host effector molecules like IgA
MALT
mucosa-associated lymphoid tissue, part of immune system, ex. peyer’s patch in small intestines
epithelium in gut
composed of epithelial cells and secretory cells, there are invaginations called crypts, few bacteria are in the crypt
lamina propria
composed of
non-cellular connective tissue elements like collage and elastin
blood and lymphatic vessels
fibroblasts and myofibroblasts
nerve endings
few leukocytes
intestinal mucus
small intestine - penetrable but bacteria are kept away from epithelium by antibacterial products, mucus not attached to epithelium
large intestine - inner mucus layer is impenetrable to bacteria whereas outer layer is expanded and serves as habitat for bacteria
major building blocks - large glycoproteins called mucins
human microbioime
indigenous microbial communities of the human body
significant positive effects of this symbiotic relationship:
helps make necessary metabolites and vitamins, helps digest carbs, competes with pathogens for “parking space”, promotes well-regulated immune response
microbiome throughout the body
each body site is colonized predominantly by only certain bacterial species, driven by pH, mucus type, etc.
acquisition of the microbiome in early life from mother-to-child microbial transmission
passed on via oral, mammary, cutaneous, and vaginal methods
healthy of babies delivered via C-section vs. vaginal birth showed difference between bottle-fed and breast-fed, but with bifidobacteria added to formula, no difference in microbiome
microorganisms in large intestine
microbes like to live around undigested particles in the lumen, little to none in the inner mucin later in the healthy state
microbiome role in fiber metabolism
microbiome breaks down fiber into SCFAs like acetate and butyrate, increases epithelium health/function, and decreases inflammation systemically
anti-microbial peptides (AMPs)
AMPs directly destroy microbial cell walls and membranes
produced by various cells in body, stored in granules, and released when cell activated
AMPs that are excreted require transcription and translation after cell activation
defensins
small antimicrobial cationic peptides that can form a pore in bacteria membranes
activation of anti-microbial peptides
activated by proteolysis to release an amphipathic anti-microbial peptide
AMP research
AMPs are our own form of antibiotics, and no AMP resistance found in nature! failed in clinical trials though
mechanisms of infection
gain access to the body and attain a unique niche (colonize)
acquire necessary nutrients in vivo
multiply or persist
avoid, subvert, or circumvent innate host defenses
cause tissue damage or disease
mechanisms of infectious disease
same as infection AND exit and transmit infection to new hosts
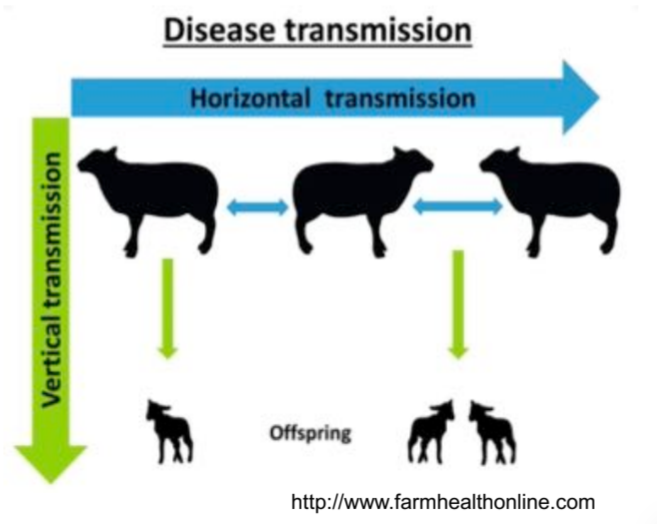
horizontal transmission
individual-to-individual
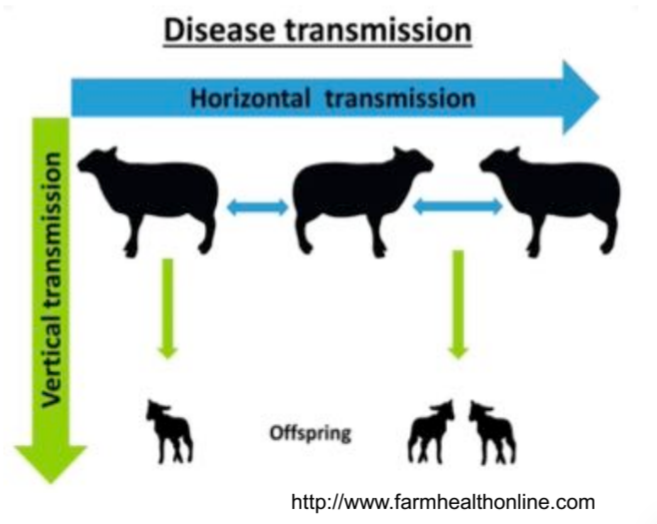
vertical transmission
maternal-to-neonatal, infectious agent may cross placenta from the mother to fetus
direct contact transmission
person-to-person spread of microorganisms through actual physical contact
ex. handshakes, sneezing
indirect contact transmission
occurs when a susceptible person comes in contact with a contaminated object or material
fomite
an inanimate object or substance, like clothing, bedding, furniture, soap, etc. that is capable of transmitting infectious organisms from one individual to another
transmission via ingestion
fecal-oral transmission, via the gastrointestinal tract
f-diagram:
feces —> fluids, fingers, flies, fields/floors —> food —> future victim
handwashing
one of the most important means of preventing transmission of infectious agents from person to person
giardiasis
caused by infection with giardia lamblia
can parasitize intestinal tract of wide range of vertebrates
transmission of disease is primarily by injection of water/food contaminated with cysts
disease spreads very easily, can occur in daycares