Week 4 - Local Anesthetics, Monitoring
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
Local/regional anesthesia is used more commonly in large animal medicine than small animal medicine. Is this because it is ineffective or less useful in small animal medicine?
- No; It is simply taught and used less in small animal medicine historically, but should be used more.
Local and regional anesthesia is typically performed under...
- Heavy sedation or general anesthesia
How are local and regional blocks used?
- They can be used for complete anesthesia (large animal "field" surgical procedures)
- Most often are used as adjuncts to general anesthesia (decrease dose requirements of general anesthesia, prevent/reduce central sensitization to pain)
What about Lidocaine causes it to sting upon injection?
- It's pH
Describe the onset and duration of Lidocaine.
- Rapid onset (5-10 mins)
- Moderate duration (60-90 mins)
Describe the relative toxicity of Lidocaine.
- Relatively lesser; Can lead to neurotoxic seizures
What type of blockade does Lidocaine provide?
- Motor and sensory
Describe the onset and duration of Bupivicaine.
- Slower onset (15-20 mins)
- Long duration (4-6 hours +)
Describe the relative toxicity of Bupivicaine.
- Relatively greater toxicity (cardiotoxic)
What type of blockade does Bupivicaine provide?
- Primarily sensory selective
Bupivicaine cannot be administered ___________.
- IV
Relative to Lidocaine, Bupivicaine causes ____________ tissue irritation.
- Less
Describe the onset and duration of Ropivicaine.
- Slower onset (15-20 mins)
- Long duration (4-6 hours +)
Ropivicaine is _____________ (more or less) lipid soluble than bupivicaine and ___________ (more or less) toxic than bupivicaine.
- Less
- Less
What type of blockade does Ropivicaine provide?
- Primarily sensory selective (greater sensory selectivity than Bupivicaine)
What is the mechanism of action of Lidocaine?
- They move intracellularly within an axon and bind to a receptor within the sodium channel (channel must be open for this to occur). They then block the sodium channels and inhibit/prevent propagation of action potentials within an axon, blocking transmission of information.
Which lasts longer when Lidocaine is administered, the sensory or motor blockade?
- Sensory blockade lasts longer than motor blockade (patient can walk but can't feel its feet sometimes)
- Note: Not everything is blocked the same (i.e., sensory is lost first followed by motor but then the sensory blockade lasts longer)
Place the following sensations in the order with which they are lost upon administration of Lidocaine.
- Pain
- Deep pressure
- Heat
- Cold
- Touch
- Pain -> Cold -> Warmth -> Touch -> Deep pressure
- Return of sensation occurs in reverse
Absorption of Lidocaine may be slowed by addition of what drugs? Why?
- Epinephrine or alpha-2 adrenergic agonists (Dexmedetomidine)
- These lead to vasoconstriction and prolong the action of the Lidocaine
What is a rough rule of thumb for the maximum quantity of local anesthetic to administer?
- <0.5 ml/kg (Err on the lower side with cats)
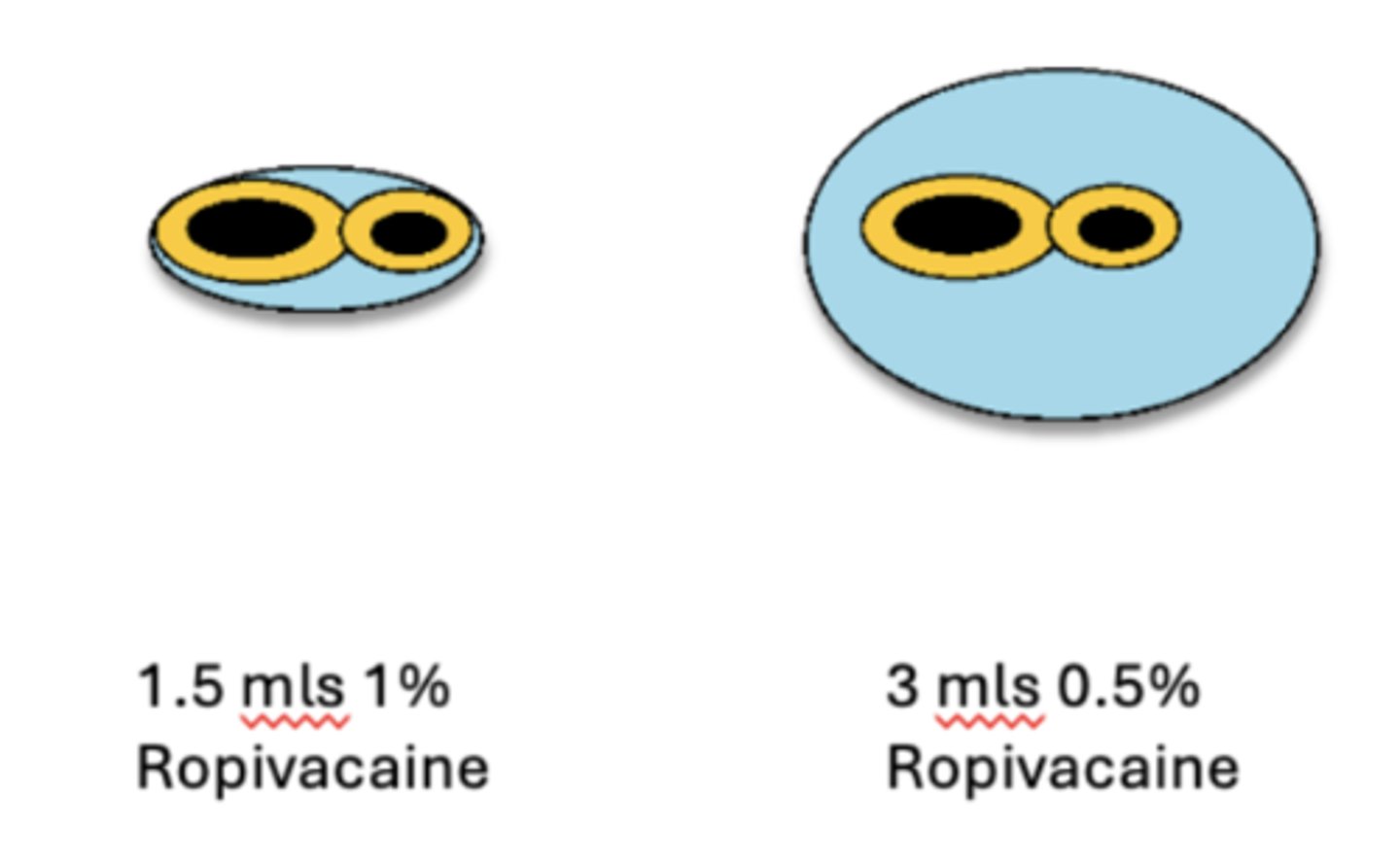
Which is more important for local anesthetics: Sufficient volume or sufficient concentration/dose?
- Sufficient volume (need to get good coverage of nerves)
Toxicity of local anesthetics can lead to what CNS effects?
- CNS depression and coma
- CNS excitation and seizures
Toxicity of local anesthetics can lead to what peripheral nervous system effects?
- Muscle fasciculations
Toxicity of local anesthetics can lead to what cardiovascular effects?
- Hypotension
- Bradycardia
- Disrhythmias
What are some treatment options for Lidocaine/local anesthetic toxicities?
- Benzodiazepines for seizure activity
- Amiodarone for ventricular arrhythmias
- 20% lipid emulsion (e.g., Intralipid 20%)
- Time
What is nocita? In what animals has its use been approved?
- A Bupivicaine liposome injectable suspension which has a 73 hour duration of action (slow release)
- Approved in dogs and cats
What is EMLA cream?
- Lidocaine and Prilocaine
What is a regional block?
- Application of local anesthetic to a nerve or group of nerves
What are some tools which can aid in performing regional blocks?
- Peripheral nerve stimulators and teflon insulated needles (requires the targeted nerve to have motor function)
- Ultrasound (nearly always do US guided blocks now -> New gold standard)
How is an epidural block performed? What region does it block?
- Injection into the epidural space
- Blocks both back legs
What is the most effective and necessary form of patient monitoring during general anesthesia?
- A qualified person to monitor the patient
What are the 5 important rules of good anesthesia?
1) Blood goes round and round
2) Air goes in and out
3) All bleeding stops eventually
4) Fluids are almost always a good idea
5) Oxygen is always indicated (unless your patient is on fire)
Almost all anesthesia-related drugs are potentially _______________.
- Fatal
What is the objective associated with each of the following during anesthesia?
A. Circulation
B. Oxygenation
C. Ventilation
D. Temperature
E. Recovery
A. Circulation - To ensure adequate circulatory function
B. Oxygenation - To ensure adequate oxygenation of the patient's arterial blood
C. Ventilation - To ensure the patient's ventilation is adequately maintained
D. Temperature - To ensure that patients do not encounter serious deviations from normal body temperature
E. Recovery - To ensure a safe and comfortable recovery from anesthesia
What are methods to assess circulation during anesthesia?
- Palpation of peripheral pulse to determine rate, rhythm and quality
- Evaluation of mucous membrane (MM) color and capillary refill time (CRT).
- Auscultation of heartbeat
- Continuous (audible heart or pulse monitor) or intermittent monitoring of heart rate and rhythm
- Pulse oximetry to determine % hemoglobin saturation
- ECG continuous display for arrhythmia detection
- Bloop pressure (indirect vs. direct)
What are the two ways to assess blood pressure?
- Non-invasive/indirect: Oscillometric method using Doppler ultrasonic flow detector
- Invasive/direct: Arterial catheter connected to an aneroid manometer or to a transducer and oscilloscope
Is palpation of a pulse sufficient to assess blood pressure?
- No
What are methods to assess oxygenation during anesthesia?
- Pulse oximetry (non-invasive estimation of hemoglobin saturation).
- Arterial blood gas analysis for oxygen partial pressure (PaO2).
Is ventilation the same thing as oxygenation?
- No
What are methods to assess ventilation during anesthesia?
- Primary way is capnography (End-expired CO2 measurement)
- Observation of thoracic wall movement or observation of breathing bag movement when thoracic wall movement cannot be assessed.
- Auscultation of breath sounds with an external stethoscope, an esophageal stethoscope, or an audible respiratory monitor.
- Arterial blood gas analysis for CO2 partial pressure
- Respirometry (tidal volume measurement)
What is the #1 anesthesia-related problem?
- Changes in temperature
What are methods to assess temperature during anesthesia?
- Rectal thermometer for intermittent measurement.
- Rectal or esophageal temperature probe for continuous measurement.
What should be recorded during anesthetic record keeping?
- Literally everything (examples include when drugs were administered including dose, route, adverse reactions, when the patient is moved, when the surgery starts, changes in vitals, when mistakes occur, and any untoward/unusual events/circumstances)
Monitoring a patient in anesthetic recovery should include at the minimum...
- Evaluation of pulse rate and quality, mucous membrane color, respiratory pattern, signs of pain, and temperature.
When during veterinary anesthesia procedures do the highest incidents adversities occur? Why?
- Recovery
- Lack of monitoring during this time
What are current AVMA recommendations regarding personnel and monitoring of general anesthesia?
- Ideally, a veterinarian, technician, or other responsible person should remain with the patient continuously and be dedicated to that patient only
- If this is not possible, a reliable and knowledgeable person should check the patient's status on a regular basis (at least every 5 minutes) during anesthesia and recovery
- A responsible person may be present in the same room, although not necessarily solely occupied with the anesthetized patient (for instance, the surgeon may also be responsible for overseeing anesthesia)
- In either of (2) or (3) above, audible heart and respiratory monitors must be available.
What are methods to assess anesthetic depth related to the CNS?
- Ocular reflexes (palpebral, corneal, eye position, lacrimation, nystagmus)
- Muscle relaxation (jaw tone)
- Response to nociception (pedal reflex with drawl reflex)
- Laryngeal reflexes (swallowing)
- Other stimulation (ear flick, whicker reflex)
What are the 4 stages of anesthesia?
1) Heavy sedation
2) Going into general anesthesia (pt can get stuck in a point with uncontrolled flailing muscle movement)
3) Surgical stage (when we want them)
4) Too deep of anesthesia (loss of sympathetic tone)
Describe what is commonly observed during "stage 2 anesthesia".
- The patient can develop uncontrolled flailing muscle spasms/movements. All patients go through this stage, but we use things like Propofol, Ketamine and Alfaxalone to move them through this stage rapidly.
- When masking down patients, this stage may be more readily observed
Describe the typical eye position of dogs/cats under general anesthesia.
- Ventromedially initially and may roll central (can indicate too light/deep)
Describe the typical eye position of cows under general anesthesia.
- Should be rotated ventromedially (if center - either too deep or too light)
Describe the typical eye position of horses under general anesthesia.
- Do not show a consistent eye position
Horses can develop what ocular abnormality when recovery from anesthesia or when anesthesia is light?
- Nystagmus
Describe what occurs with lacrimination/tearing during anesthesia.
- In horses, lacrimation can indicate a light plane of anesthesia
- In SA anesthesia, this is uncommon and often the eyes become dry, requiring artificial tears
What is an objective method to assess jaw tone?
- Scale of 0-4 with 0 indicating now jaw tone (too deep) and 4 indicating full jaw tone (too light)
- Goal: 1-2
How should you interpret a positive pedal reflex (withdrawal reflex) during general anesthesia?
- If present spinal reflex; analgesia problem
How should you interpret a positive ear flick/whisker reflex during general anesthesia?
- If see response, indicates light anesthesia (or it's time to extubate your patient)
What is a normal canine HR?
- 60 to 180 BPM
HR in dogs _______________ with increasing size
- Decreases
What is a normal feline HR?
- 100 to 220 BPM
What is a normal equine adult HR? Juvenile?
- Adult: 30 to 50 BPM
- Juvenile: 50 to 70 BPM
What is a normal ruminant adult HR? Juvenile?
- Adult: 70 to 100 BPM
- Juvenile: 80 to 120 BPM
What is a normal camelid adult HR? Juvenile?
- Adult: 60 to 90 BPM (with anticholinergic) or 28-40 BPM (with xylazine)
- Juvenile: 90 to 125 BPM
What is a normal swine adult HR? Juvenile?
- Adults: 60 to 90 BPM
- Juveniles: 90 to 125 BPM
What can be assessed when palpating a pulse?
- Strength
- Rate
- Rhythm
What is pulse pressure?
- Difference between systolic and diastolic pressure (i.e. 120/90 feels the same as 90/60)
What are two ways to auscultate the heart during anesthesia?
- Stethoscope (if thorax is accessible)
- Esophageal stethoscope (for patient's who are under drapes)
On a blood pressure wave form, there is a notch between systole and diastole know as what?
- Dicrotic notch (when the aortic valve closes)
What is the equation for MAP?
- MAP = PP/3 + DAP
What is capillary refill time? What is a normal CRT?
- Crude indicator of adequacy of the cardiovascular system (may be normal in a dead patient - hence, crude)
- Refill should occur within 2 seconds
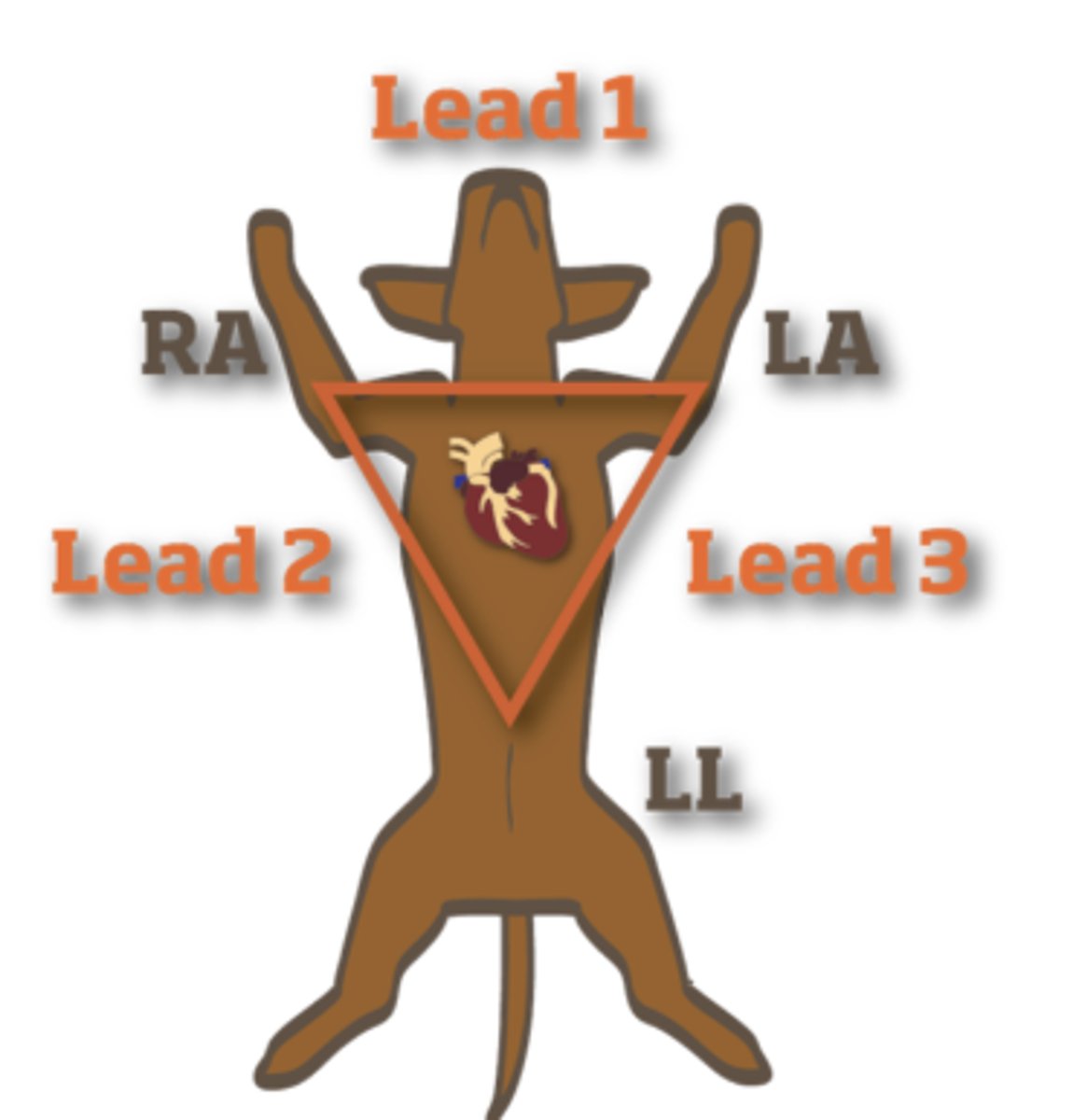
When using an ECG, the metal pieces which touch the patient are the leads or the electrodes?
- Electrodes
Indicate where the leads are in a canine ECG relative to the patient's limbs.
- Lead 1 is between the right and left arm
- Lead 2 is between the right arm and left leg
- Lead 3 is between the left arm and left leg
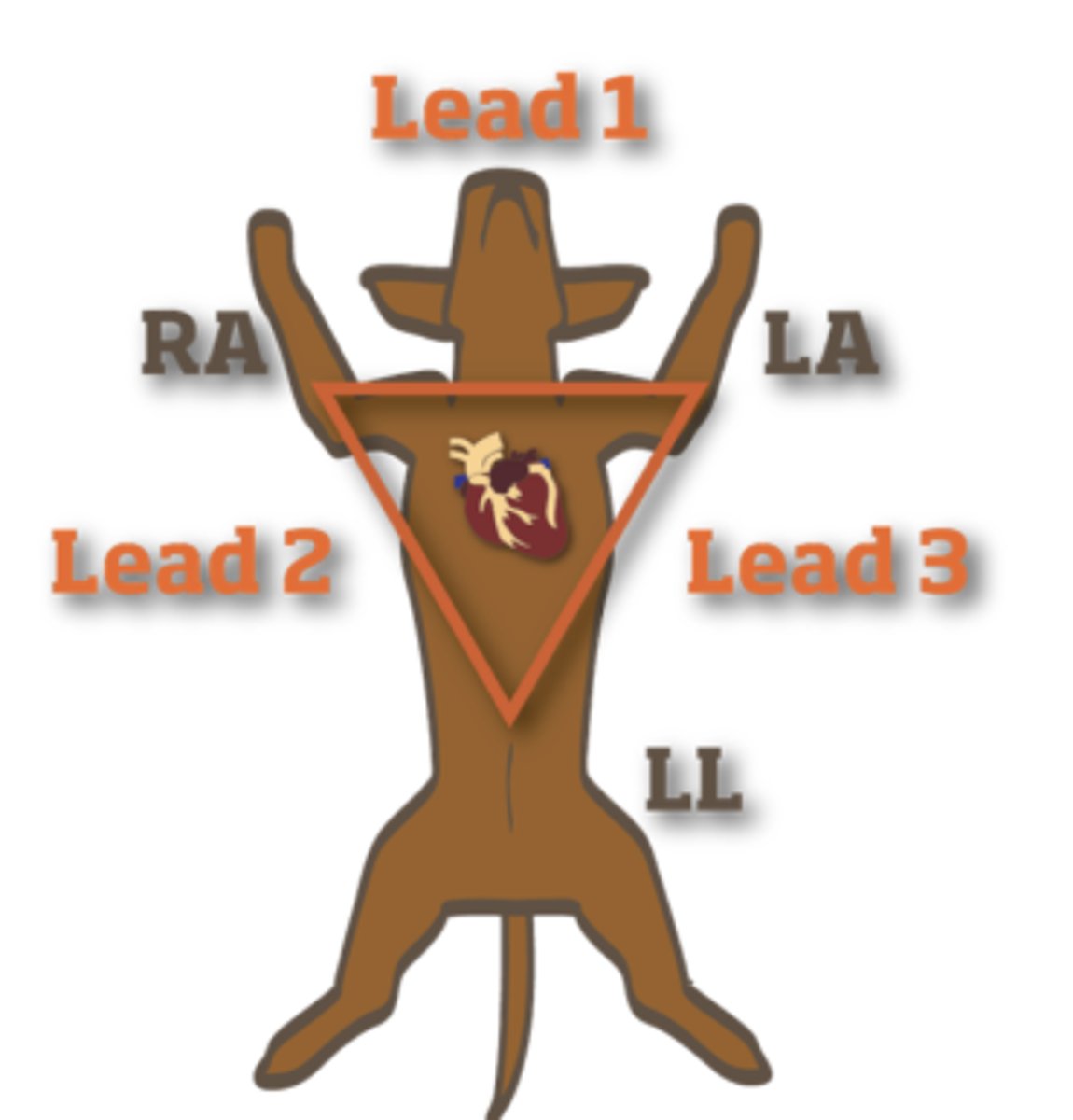
Why is lead 2 commonly used in canine ECGs?
- Because in a dog, electrical activity tends to go from SA node to apex of the heart (left side), so lead 2 follows that vector best
What is one of the most common cardiovascular anesthetic complications?
- Hypotension
What is hypotension defined as?
- Systolic < 90 mm Hg
- MAP < 70 mm Hg
What are the equations for BP and CO?
- BP = CO + Systemic vascular resistance
- CO = HR * SV
What are treatment/management options for patients with hypotension under anesthesia?
- Normalize the HR/rhythm
- Assess anesthetic depth (reduce inhalant dose if possible)
- Fluid bolus
- Inotropes/vasopressors
Anesthetic bradycardia is most commonly ______________ bradycardia.
- Sinus
What are causes of bradycardia?
- Drugs (i.e., Dexmedetomidine)
- Hypothermia
- Vagal tone/reflex
What are different types of bradycardia?
- Sinus bradycardia
- AV block
- Sinus arrhythmia (variable P-P interval)
Explain the mechanism behind a sinus arrhythmia.
- As the patient exhales, the heart starts to slow down.
- As the patient inhales, blood if pulled into the heart due to negative pressure in the thoracic cavity, so the heart speeds up due to extra blood
What are treatments for bradycardia under anesthesia?
- Glycopyrrolate
- Atropine
What are causes of tachycardia under anesthesia?
- Too light?
- Pain
- Shock/hypovolemia/hypotension
- Hypercarbia
- Hypoxia
- Hyperthermia
- Drugs
- Cardiac disease
- Generalized disease
What are treatments for tachycardia under anesthesia?
- Correct the underlying cause
- Pharmacology (Fentanyl or Esmolol - beta blocker)
What are the different types of AV blocks?
- 1st degree (prolonged PR interval)
- 2nd degree (Mobitz 1 = Cyclical increased PR interval until dropped QRS; Mobitz 2 = Intermittent or runs of dropped QRS - more common)
- 3rd degree (AV dissociation - sinus rate does not equal ventricular rate)
What are some cause of tachy-arrhythmias?
- Underlying disease
- High sympathetic tone (nociception, disease process)
- Systemic illness
- Trauma (HBC)
- Cardiac disease
What is the first question to consider when evaluating an ECG?
- Do I have a readable ECG tracing? (i.e., minimal artifact)
When there is an ECG abnormality, what questions can you ask yourself when deciding whether to treat it?
- Is it causing hemodynamic instability?
- Does it herald more significant issues?
- What is the likely cause and can I treat the cause?
- Can I treat the arrhythmia?
What is the large square method of assessing HR? What about the pen method?
- Divide 300 by the number of large squares between R and R
- Take the number of R waves in the length of the avg. pen and multiply it by 10
When looking at a continuous ECG monitor, what is one way to determine if something on the ECG is artifact or real?
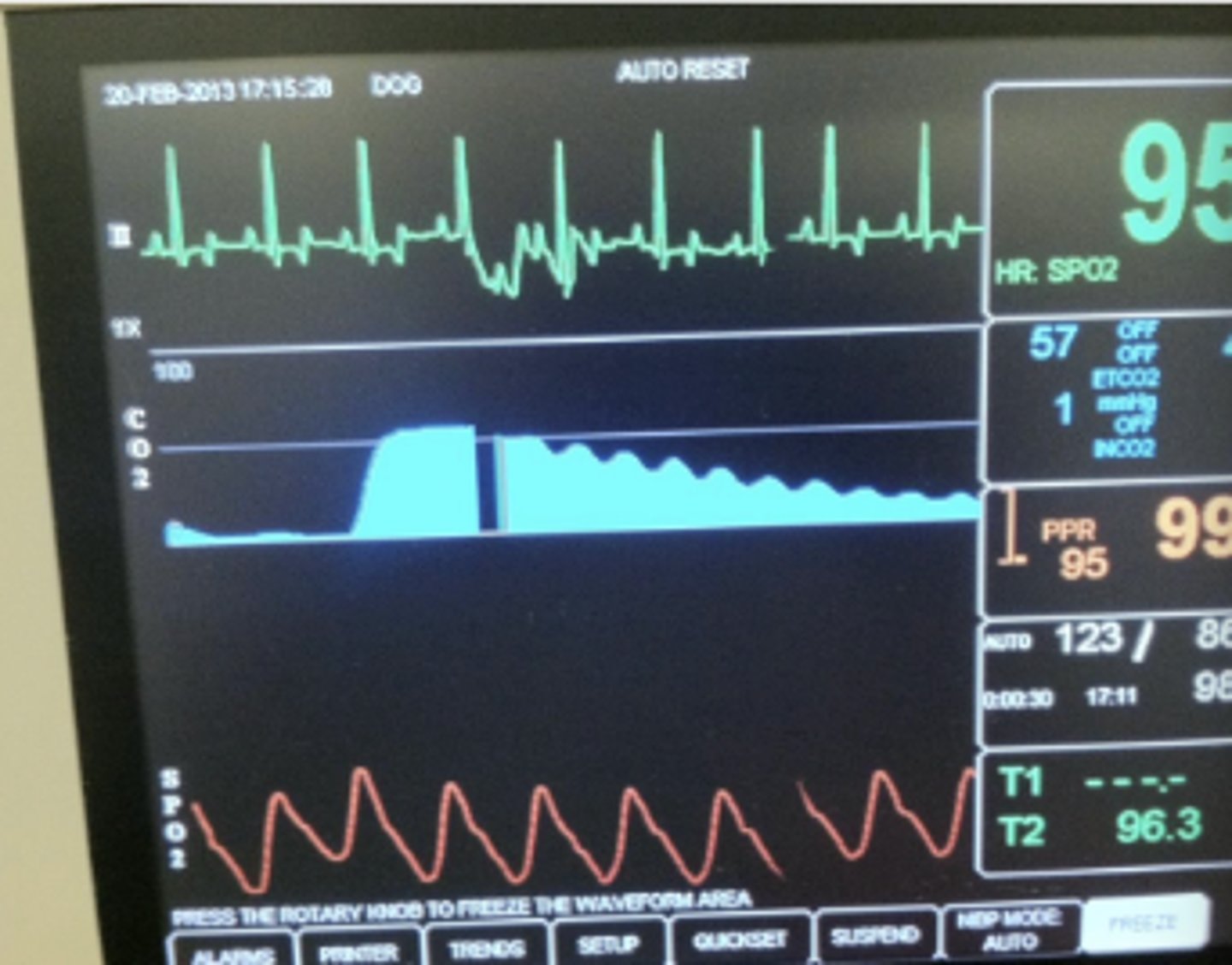
- Look at the pulse waves at the same time and see if they are also abnormal (note that the change in the ECG image is artifact because the pulse wave is normal)