The Skin Immune System Pt. 1
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
What regions of the skin are potentially portals of entry for pathogens?
• Epidermis
• Adnexa (Hair follicles and supporting glands)
• Dermis and panniculus/subcutis
• Extension from underlying tissues
In what ways can substances enter into the epidermis of the skin?
• Absorption
e.g. Lipophilic drugs
• Direct contact
e.g. Caustic chemicals
• Colonisation
e.g. Dermatophytes (ringworm)
• Penetration
e.g. Hookworm larvae; trauma inc. UV radiation
• Impaired barrier
Micro-organisms
Allergens
In what ways can substances enter into the adnexa of the skin?
• Entry via follicle ostium
Ostium = tiny surface openings are part of the skin structure that allows microparticles to pass through the epidermis
• Rupture of follicle or adnexal glands (Called Furunculosis)
If immune system exposed to hair follicles → causes nasty reaction and inflammation
In what ways can substances enter into the dermis/panniculus of the skin?
By tracking along “something”, such as:
• Blood vessels
Drugs, toxins, emboli, leukocyte trafficking
• Nerves (rare)
e.g. Feline herpesvirus 1
Axonal flow along sensory nerves causes dermatitis
In what ways can substances enter into the underlying tissues of the skin?
• Penetration by damaged bone
Fracture trauma
• Extension from adjacent tissues
Tumour or infection from lymph node, gland, muscle or bone
How does the skin (in general) respond to inflammation and injury?
• Most conditions provoke an inflammatory reaction
• The skin is limited in how it can respond
• And there are a number of typical primary and secondary lesion patterns
Primary → caused directly by insult
Secondary → caused by animal responding to insult, like raw skin resulting from itching
• Also, several overlapping processes may occur together
How can we characterize patterns of skin disease?
Epidemiology
• Breed, sex, location, season
Clinical Presentation
• Macroscopic lesions, distribution, configuration
Histopathology
• Pattern analysis
• Postgraduate!
When considering epidemiology, what should you consider regarding skin conditions in the following:
• Breed
Skin fold dermatitis (intertrigo) in Sharpei, Bulldog, Pekinese, pug
• Sex
• Symmetrical alopecia with oestrogen production by Sertoli cell tumour in male dogs
• Location
• Cutaneous haemangiosarcoma following sun exposure in dogs in Grenada, West Indies
• Season
• Flea allergy dermatitis
• More common in temperate climates but seasonal in colder climates
Describe the factors used to describe the clinical presentation of skin diseases.
• Clinical signs = macroscopic pathology (What is seen in practice is also seen by pathologists)
• Distribution:
Where are the lesions on the body?
• Description:
Size, shape, colour, consistency
Gives clues as to the lesion type
Red: inflammatory
Thickened: hyperplastic
Bald: alopecic / hypotrichoic
Nodular: Inflammatory / neoplastic
How are histopathology patterns named?
A pattern consists of two parts: a component of the skin (e.g. epidermis) and a histologic reaction of that component to injury (e.g. hyperkeratosis) = pattern (e.g. epidermal hyperkeratosis)
How do primary skin lesions develop?
List some of the main examples.
• Develop spontaneously as a result of underlying disease
Useful in trying to determine aetiology and pathogenesis of disease
• Examples
Macule or (>1cm) Patch
Papule or (>1cm) Plaque
Vesicle or (>1cm) Bulla
Pustule (or Abscess)
Wheal (or Hive)
Cyst
Nodule
What is a “macule”?
primary skin lesion
• A circumscribed, non-palpable spot characterised by a change in the colour of the skin.
• A larger lesion >1.0 cm is a patch.
e.g. haemorrhage, lentigo
Describe the passive defenses present in the skin.
Creates a physical barrier.
• Hair, hooves and claws
Thermal insulation AND dissipation
Mechanical protection
Sensory function
• Melanocytes
Cap of pigment = photoprotection
• Epidermal barrier — more later!
Skin surface lipids
Stratum corneum
Basement membrane
Dermis and superficial dermal fat
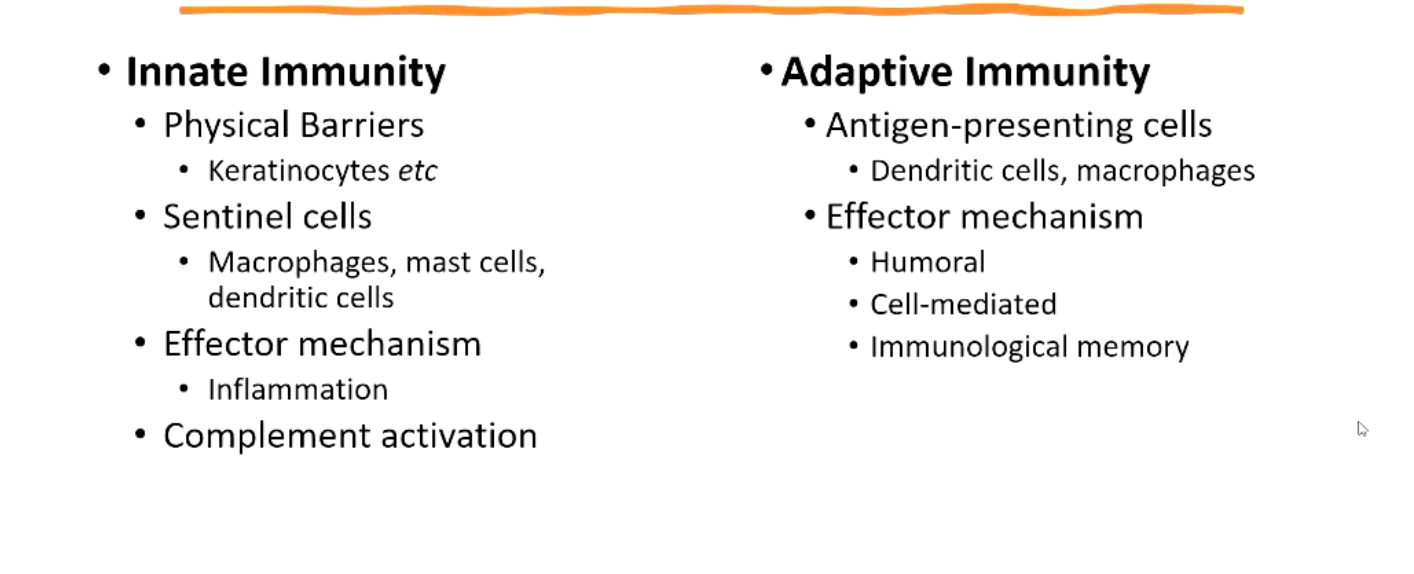
Describe the active host defense in the skin.
• Skin immune system
• Innate immunity
Immediate, non-specific
• Adaptive immunity
Delayed but targeted
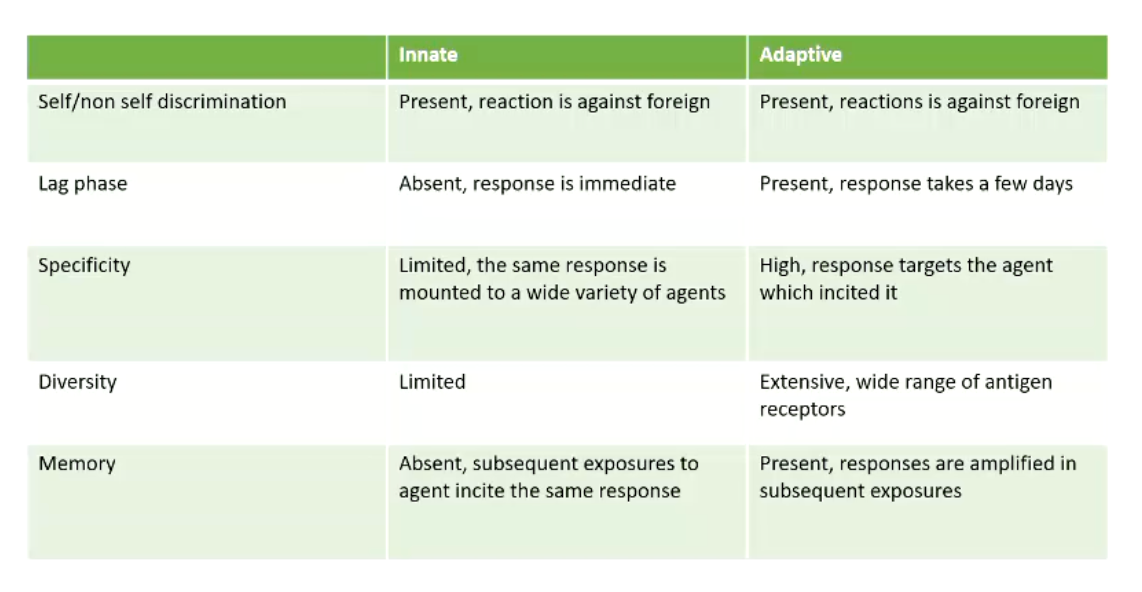
Reminder** what is the difference between innate and adaptive immunity?
How does the innate immune system respond to insult in the skin?
• Exposure to antigen, recognized by langerhans’ cells and the keratinocytes
Release of primary cytokines
Promote inflammation
• Upregulation of endothelial expression of adhesion molecules
• Recruitment of additional innate effector cells
Activation of skin cells & resident innate immune cells
Endothelial cells become activated, expressing attachment sites for immune system
Neutrophils, macrophages, NK cells
• Langerhans' and dermal dendritic cells carry antigen to draining lymph node
Dendritic cells carry the antigens to the T-cells, making the bridge between the innate and adaptive response
How does the adaptive immune response become activated?
• Memory T cells carry T cell receptors (TCRs) specific for antigen previously encountered in skin
• Interaction of antigen specific T cells with APCS results in T cell activation
• Cytokines also stimulate expression of T cell specific chemokine ligands on endothelium
• T cells recruited by antigen non-specific mechanism
Summarize the difference in the important cells and effector mechanisms between innate and adaptive immunity.
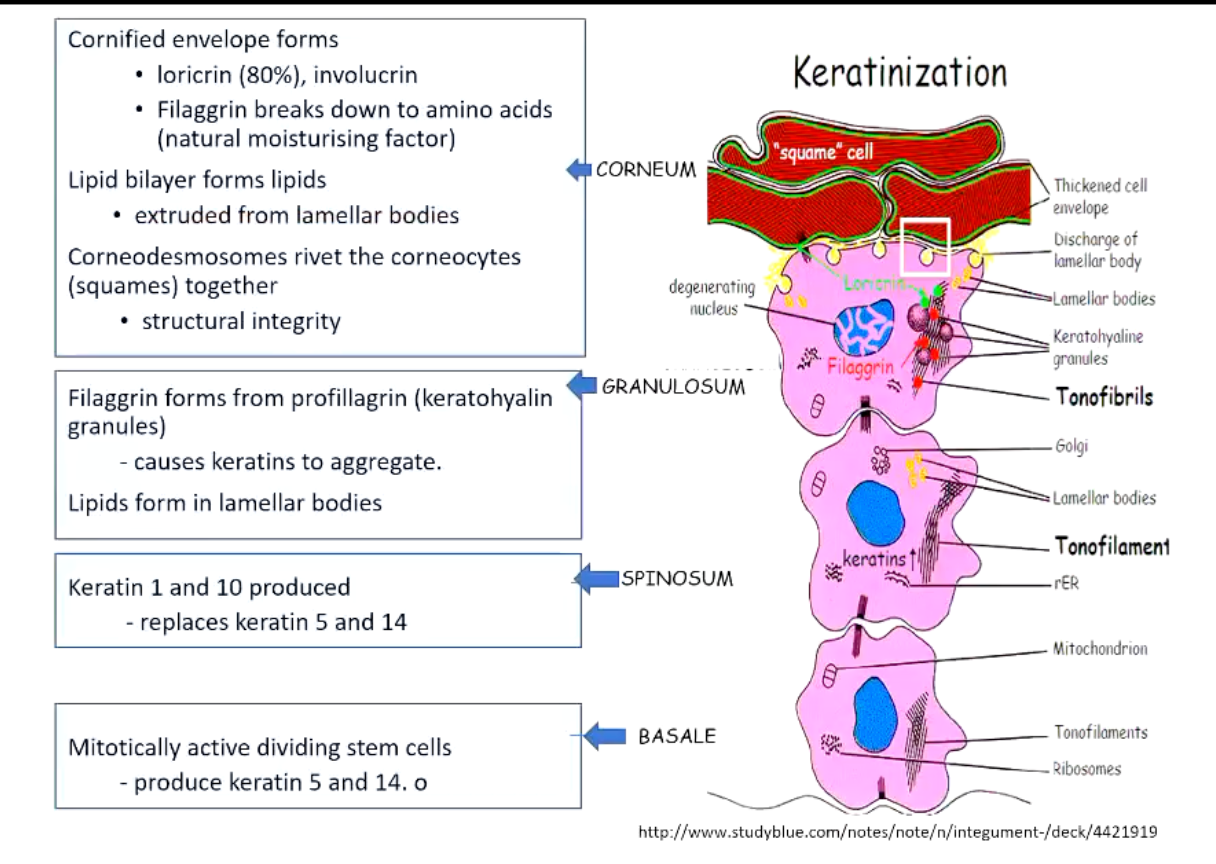
What makes up the skin barrier?
• The physical and permeability barrier is regenerated by the process of keratinisation
Proliferation, differentiation, cell death
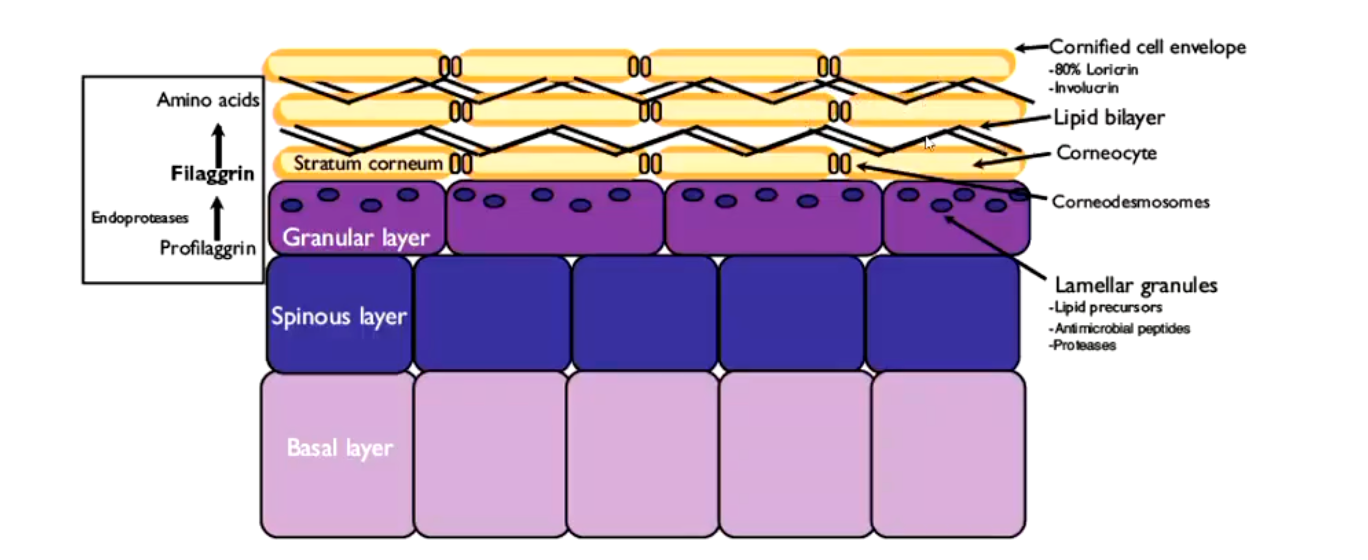
What are key features of the stratum corneum?
• Lipid bilayer of cell membranes = cornified envelope, each keratinocyte is joined together by corneodesmosomes
Loricrin and involucrin
Filaggrin
• Control of desquamation
By the balance of stratum corneum protease inhibitors & proteases (Healthy smooth normal skin, or you could have flaky skin or ulceration, both abnormal balance)
Skin pH
Dog normal 5.5-7.5
Reminder** Summarize each layer of the skin and the primary processes happening in each of those layers.
What is the purpose of cutaneous lipids?
How much is found within the skin?
• Healthy stratum corneum is up to 85% lipid
Sphingolipids (ceramide)
Cholesterol
Free fatty acids
• Sphingolipids and fatty acids important for...
Physical barrier
Permeability barrier and
Immunologic barrier
• Some molecules have ANTIMICROBIAL properties
e. g. Sphingoid bases derived from epithelial sphingolipids
Mechanisms are not fully understood
What cells produce antimicrobial peptides and what do they do?
Produced by neutrophils, macrophages, epithelial cells (etc)
Activate and recruit inflammatory cells & alarm and arm keratinocytes
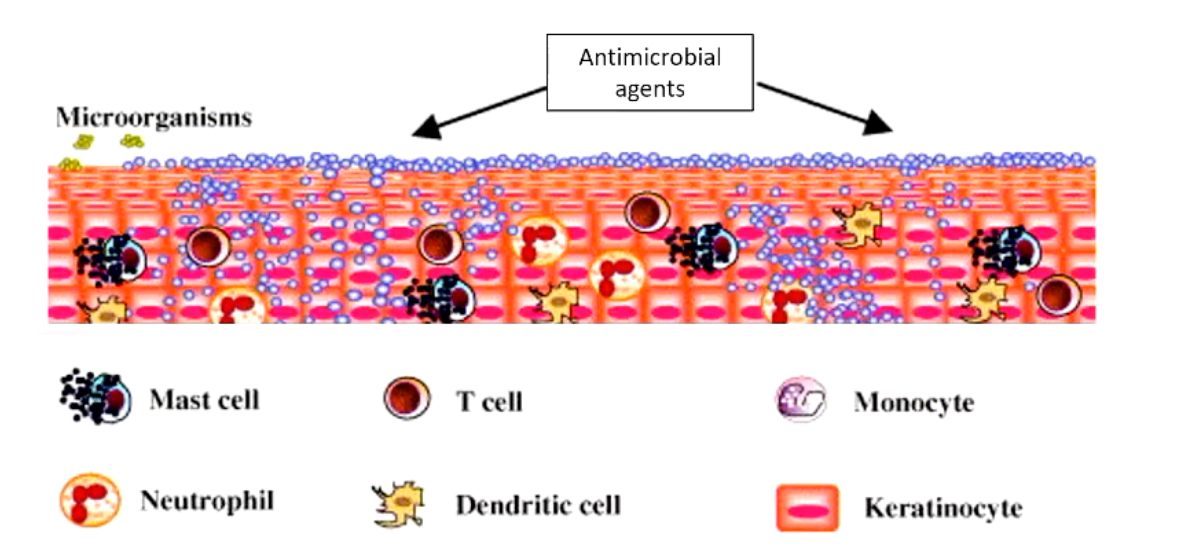
How does AMP expression look like in normal skin?
What does it look like in injured skin?
Normally skin has a normal low level of AMP production
Injured keratinocytes increase AMP production
Neutrophil and mast cell recruitment
Inflammatory cells also produce AMPs (Producing a compounding effect)
AMPs stimulates angiogenesis and keratinocyte proliferation leading to thickening of the skin
What is atopic dermatitis?
Describe what causes it and classic lesions for the condition.
Classic lesions: reddening and alopecia
Ulceration due to itching by animal
• Allergens can be absorbed via the skin +/- inhaled
Causes inflammation, oedema and mast cell rich infiltrate
• Abnormal canine skin barrier
Variations in filaggrin expression
Geographic and breed variations
Downregulation (but not gene mutation) of filaggrin reported in WHWTs
• Disorganised lipid lamellae
Altered ratio of cholesterol / ceramides
Altered balance of antimicrobial peptides

Why are dust mites and normal bacteria associated with atopic dermatitis?
Exogenous producers of proteases which create gaps in skin, allowing allergens to enter the skin
What is the importance of the skin’s microbiome?
The skin, like the gut, needs microbial signals for proper immune function
Reciprocal: the cutaneous and innate immune responses modulate skin microbiota AND the microbiota modulate the immune system
Diverse and variable population of commensal microbes e.g. Staph. epidermidis
What factors affect the skin microbiome?
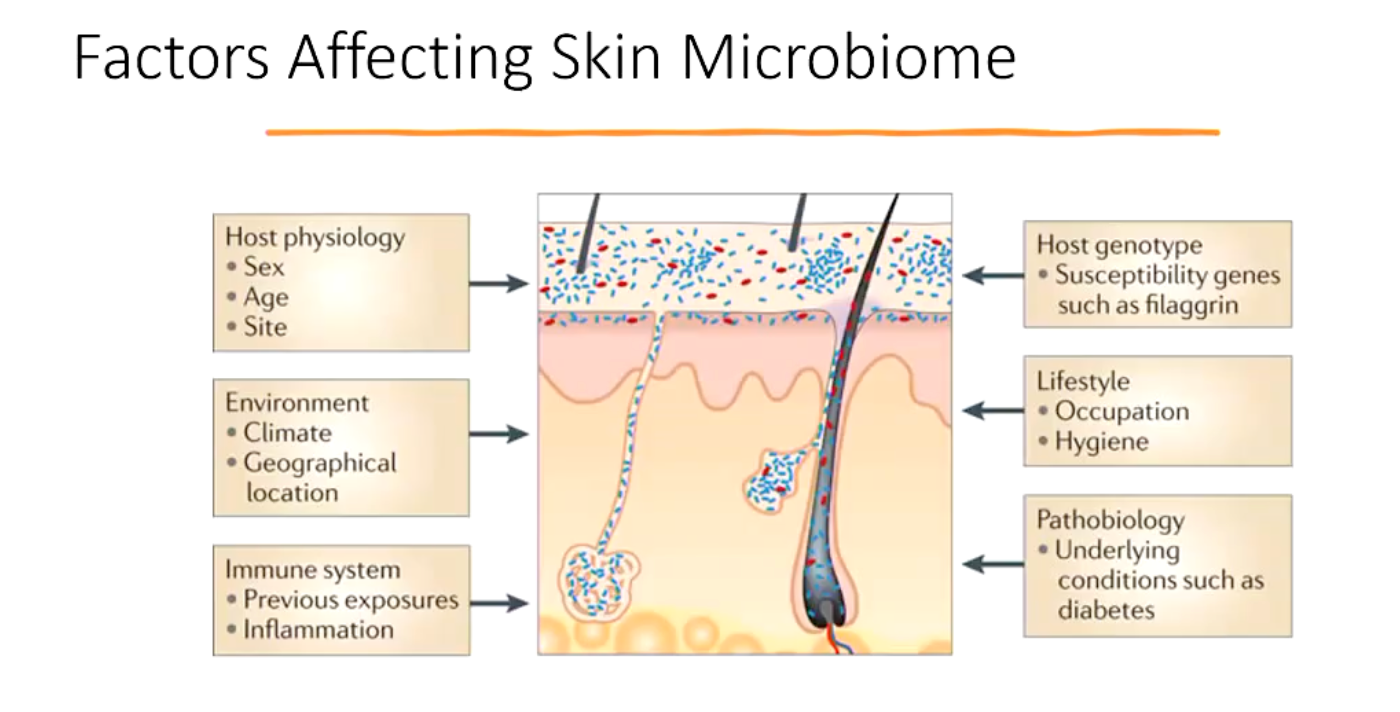
How does the microbiome and innate immune response modulate skin microbiota?
• For example: Staphylococcus epidermidis (commensal) produces
• Antimicrobial peptides
e.g. Modulins: act as barrier to pathogenic colonisation
• Small molecules
Which enhance expression of defensins via Toll-like receptors (TLRs)
What are the main cellular components of the skin?
• Endothelial cells
Express adhesion molecules and bind T lymphocytes
• Keratinocytes
Roles in defence and immune modulation
• Dendritic/Langerhans cells
Major role in antigen presentation
Epidermal (Langerhans cells) and dermal
• Mast cells
Release histamine etc.
• Lymphocytes
T cells
B cells
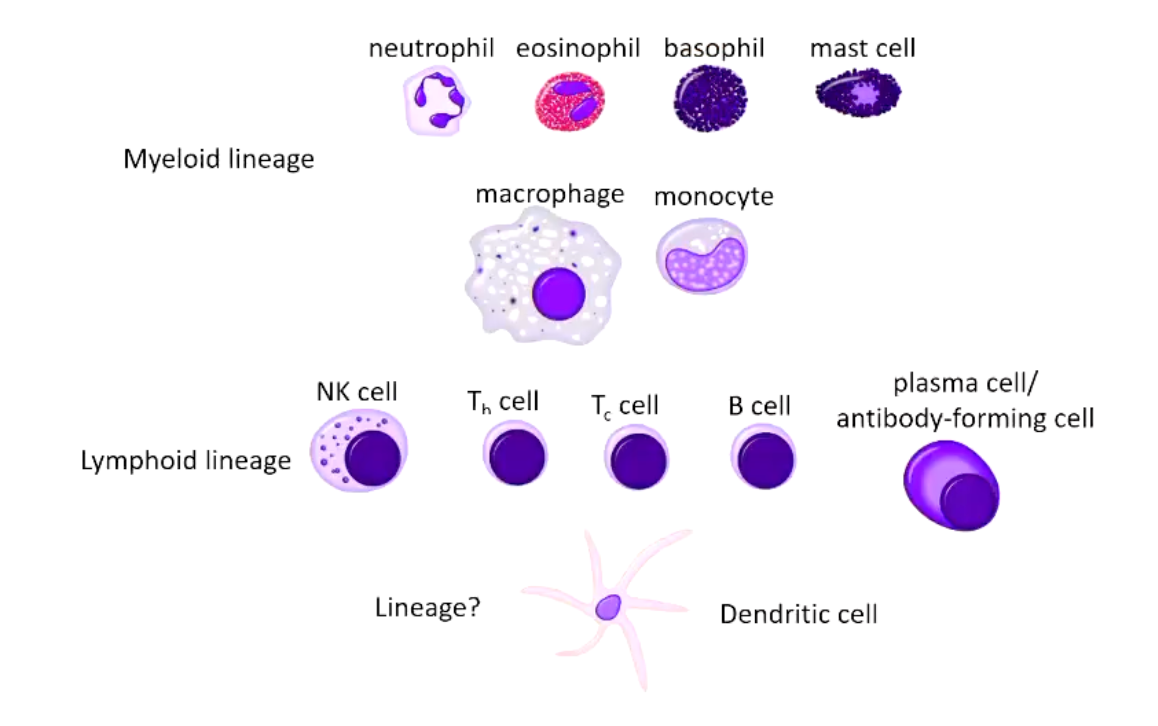
Reminder** Cells of the immune system.
Myeloid Lineage
Lymphoid Lineage
How are keratinocytes involved in the immune response?
• Act as sentinel cells
Express Pattern Recognition Receptors (PRRs)
Respond to DAMPs (e.g. generated by UV light) and PAMPs (associated with microbial invasion)
Induce innate immune response
• Effect is po-inflammatory
Produce a complex mixture of AMPs, pro-inflammatory cytokines and chemokines
• Non-professional antigen-presenting cell
Expresses MHC class Il molecules
Can interact with antigen-experienced T cells
• Mechanism through which the skin discriminates between commensal and harmful bacteria is unclear - tolerance?
What are DAMPs and PAMPs?
DAMP: damage associated molecular pattern
PAMP: pathogen associated molecular pattern
How to keratinocytes in the innate immune system protect the body?
Provide a physical barrier
Make antimicrobial peptides which activate mast cells and help kill pathogens
Also recruit inflammatory cells
Can present pathogens to memory T-cells
What are the main roles of the Langerhans cells?
• Aka Epidermal Dendritic Cells
• Dendritic cells link the innate and adaptive immune responses
• Langerhans cells interact with skin resident memory T cells
Help maintain a balance between immune reactions and tolerance
If too tolerant of “self” - pathogen becomes overgrown
If launching an immune response to something that is self → hypersensitivty