Exam 3: Tissue Integrity — Pressure injury
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
Tissue integrity
The state of structurally intact and physiologically functioning
epithelial tissues, such as the integument (including skin and
subcutaneous tissue) and mucous membranes
What does impaired tissue integrity reflect?
reflects varying levels of damage to one or more groups of epithelial cells
What do epithelial cells form?
form a continuous, tightly packed layer on surfaces in and out of the body
Skin function
Critical barrier
1st line of defense
Regulates water loss and temperature
Secretion + excretion
Provides sensory input
Nerves allow for sense of touch, temperature, and pain
Vit D produced by body from sun
Wound healing
What does the dermis consist of?
Epidermis
Dermis
Subcutaneous tissue
Subjective assessment of skin
Lifestyle and Personal Habits
Allergies (skin, food, medications, chemicals)
Previous skin conditions
Personal and family history of skin cancer
Specific symptoms to determine a specific disease: OLDCART
Use and types of cosmetics, soaps, shampoos, laundry detergent, etc
Objective inspection of skin
color
Lesions
Open areas/wounds
Pigmentation changes
Surgical incisions
Scars (note scar formation)
Objective palpations of skin
temperature (back of hand)
Moisture
Skin turgor
Color return
Tented skin turgor
indicates dehydration (not a specific assessment)
Color return
assessing capillary refill
How do you assess for the patients risk for skin breakdown?
Braden scale
Diagnositic testing assessment
skin biopsy
Patch testing
Skin scraping
Tzanck smear
Wood light
Culture + sensitivity
Skin biopsy
sample of a nodule, plaque, blister or other lesion
Patch testing
applying suspected allergens x 48 hours to determine sensitivity
Skin scrapings
◦microscopic examination tissue samples from fungal lesion(s)
Tzanck smear
microscopic examination of blister secretions
wood light
lamp using long-wave UV rays to examine for tinea (Assess for infection)
Culture and sensitivity
suspected bacterial infection
Age related changes
fragility and thinning
↓ elasticity and turgor
↓ thickness (tissue and fat)
↓ sebum (of sebaceous glands)
Considerations for examination/diagnosis
meds can lead to photosensitivity
Loss of subcutaneous tissue
Vascular changes can impact fragility of skin and would healing
Increased susceptibility to trauma (skin tears, bruising)
Pressure injury
Localized injury to skin and underlying soft tissue due to intense and/or prolonged pressure with or without shear or friction
can also be caused by pressure that doesnt include shear and friction
Pressure injuries tend to occur over…
Bony prominences
not much subcutaneous tissue
What can pressure injury can be precipitated by? Examples?
Any hard surface in contact with the patient
Examples: bed, wheelchair, armrest
Never events
Serious and preventable patient safety incidents that should never occur in healthcare settings
How to ensure never events do not occur
Reposition patients often
Skin monitoring
Redistribution of pressure
never events are _____-_____ problems
nursing sensitive
First sign of pressure injury
Erythema
Erythema
Redness of skin due to dilation of capillaries
first sign of a pressure injury
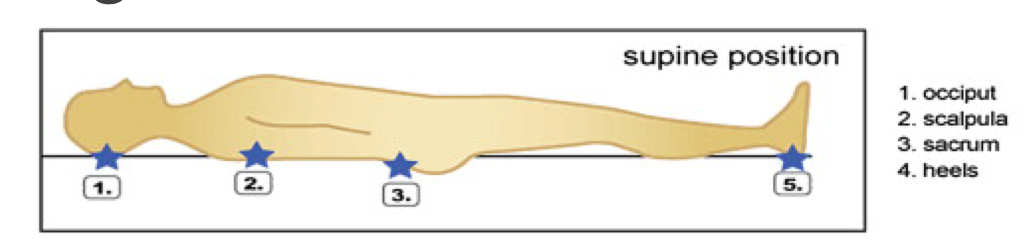
High risk areas for pressure injuries in supine position
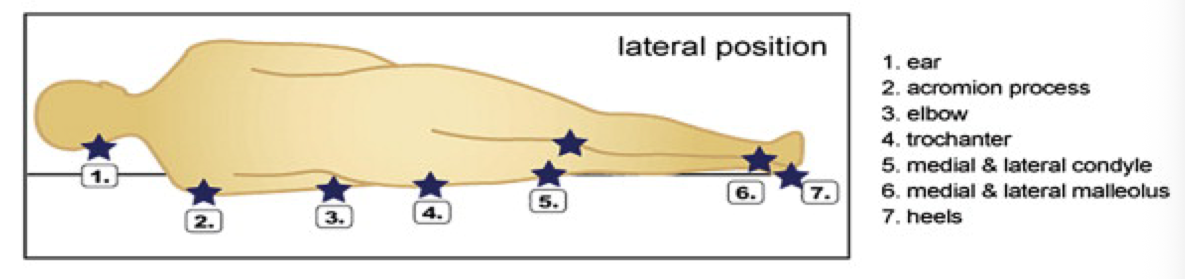
High risk areas for pressure injuries in lateral position
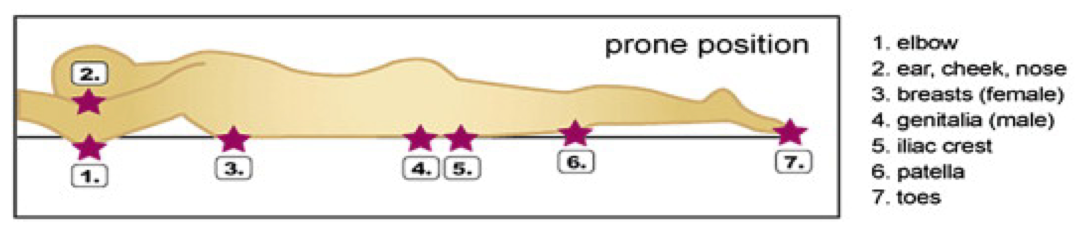
High risk areas for pressure injuries in Prone position
How to prevent pressure injury when lateral
make sure that the extremities are not rubbing on eachother and cause pressure
Friction and location
force of rubbing two surfaces against each other
outside of skin
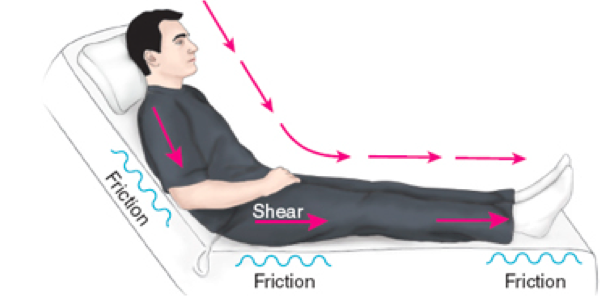
Shearing and location
exerting a parallel force on patient’s body
deeper tissue (e.g., muscles)
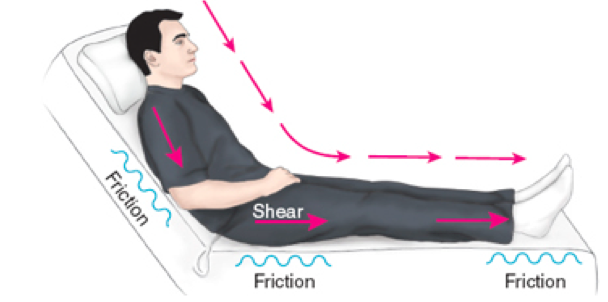
Why do we need a lifting device to move patients?
we need to have a lifting device to move patients so there is no friction/shearing when the bed is moving against their body we need to have a lifting device to move patients so there is no friction/shearing
Risk assessment for pressure injuries
Skin: inspect each pressure site
Mobility: get patients moving in some way)
Neurologic status: ↓ LOC, ↓ sensory perception bc decreases mobility
Vascular status: poor circulation
Nutrition: malnourishment
Incontinence or increased moisture (pay attention to skin folds — especially in larger ppl)
Shear and friction
Braden Risk scale assessment scale
Sensory perception
Moisture
Activity
Mobility
Nutrition
Friction and shear
Risk levels for pressure injury based on Braden assessment
Low risk = 15-16
Moderate risk = 13-14
12 or less = high risk
Stage 1 pressure injury and signs
intact skin
Non-blanching erythema
Skin may be warm to touch and painful
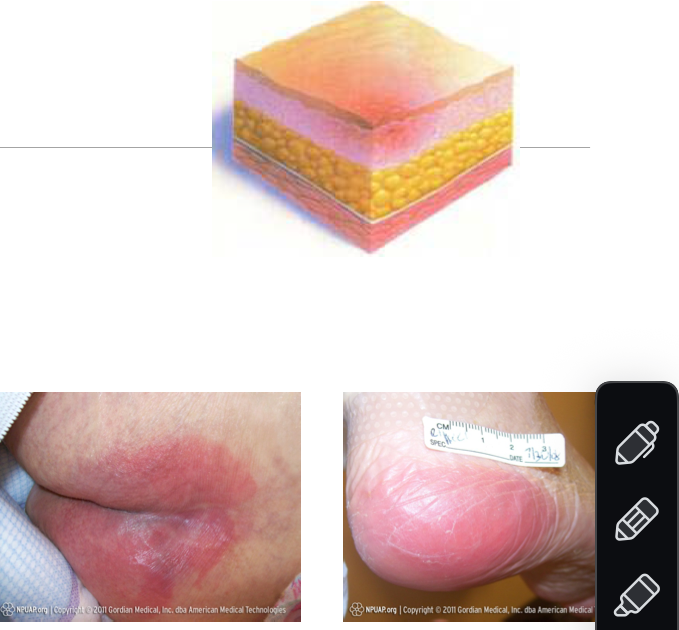
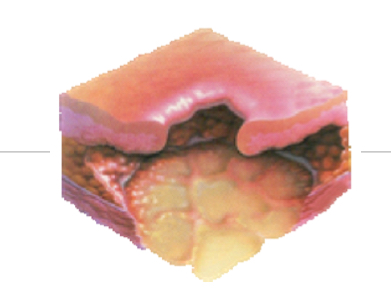
Stage 2 pressure injury and signs
Partial-thickness tissue loss involving dermis and epidermis
Shallow open ulcer, blister, or abrasion with a red-pink and moist wound bed
No slough or bruising
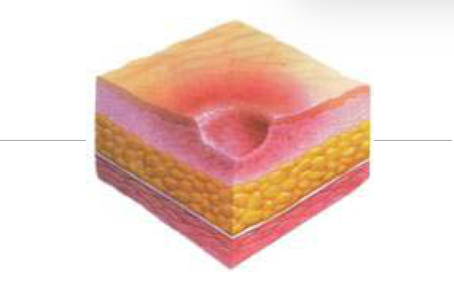
Stage 3 pressure injury and signs
Full-thickness tissue loss
Subcutaneous tissue may be visible
Slough may be present but able to visualize wound bed
May include undermining and/or tunneling
Sloughing
the process where the outer layer of skin (epidermis) detaches and is shed
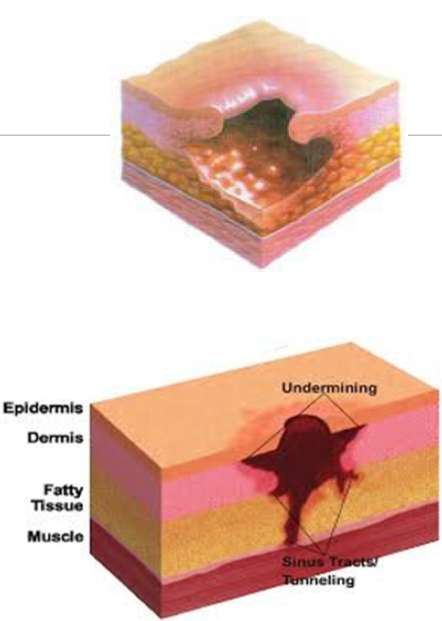
Stage 4 pressure injury and signs
Full-thickness tissue loss with exposed bone, tendon, and/or muscle
Slough or eschar may be present
What is the MAJOR risk of stage 4?
Risk for osteomyelitis
Bone infection
Serious complication
Unstageable pressure injury and signs
Stage is unclear because we can’t tell the deepness/base of the wound d/t slough and eschar
Full-thickness tissue loss
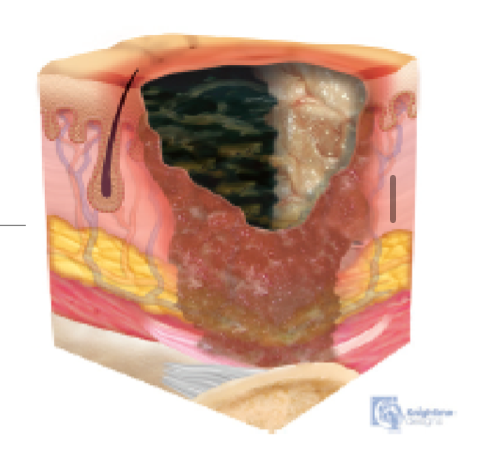
How can we determine the level of damage of unstageable pressure injury?
Remove slough to determine depth/stage
Deep tissue pressure injury
Damage to underlying soft tissue
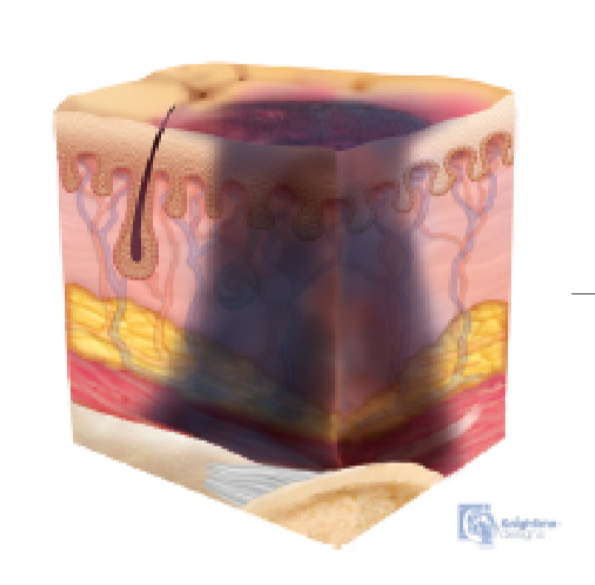
Characteristics of deep tissue injury
Purple or maroon localized area
Skin intact or blood-filled blister
Painful
Boggy or mushy but can be firm
Assessment of pressure injury
• Inspect
Color, blanchable
Document size: measure in centimeters, always length x width x depth
Determine presence of undermining or tunnelling
Describe any drainage including amount and odor
Describe wound bed tissue
Describe wound edges
Observe condition of surrounding tissue
• Palpate
Surface temperature over injury area
Bony prominences & dependent areas for edema and/or bogginess
Types of drainage
Sanguinous
Serous
Serosanguineous
Purulent
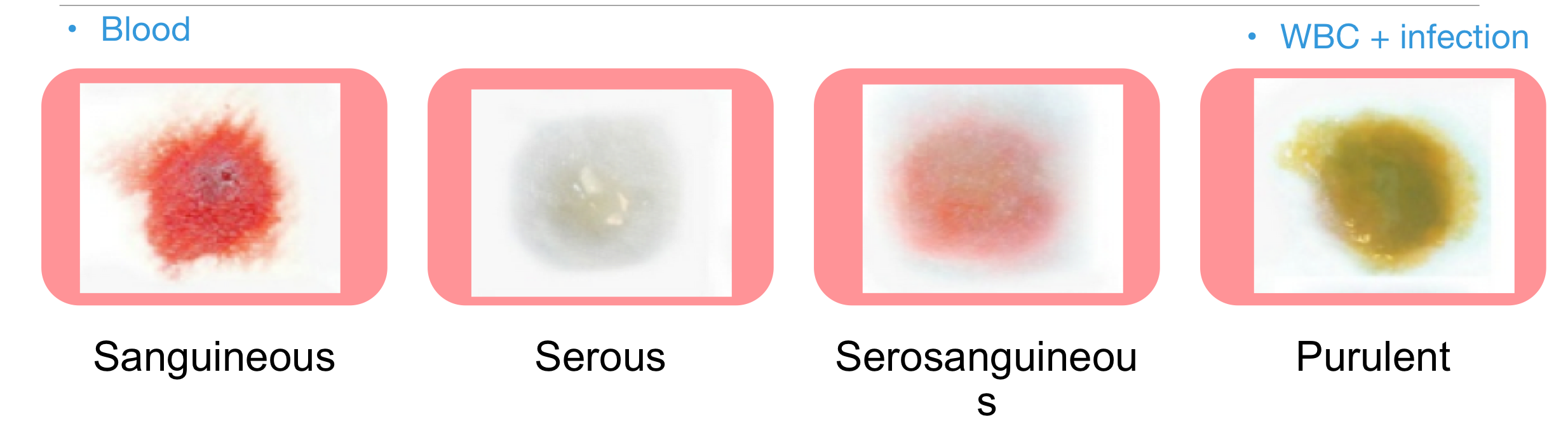
Salguinous drainage
Appearance: Bright red, fresh blood
Indicates: Active bleeding or trauma to blood vessels
Serous drainage
Appearance: Clear or pale yellow, watery fluid
Indicates: Normal healing or mild inflammation
Serosanguinous drainage
Appearance: Pink or light red, mix of clear fluid and blood
Indicates: Mild bleeding with serous fluid, often seen in healing wounds
Purulent drainage
Appearance: Thick, cloudy, yellow, green, or tan pus
Indicates: Infection with bacteria and white blood cells present
To heal a wound, you must _____ the wound
clean
Wound bed tissue types (4)
Granulation
Epithelialization
Necrotic slough
Necrotic eschar

Wound edges types (4)
Epibole
Macerated
Fibrotic
Callused
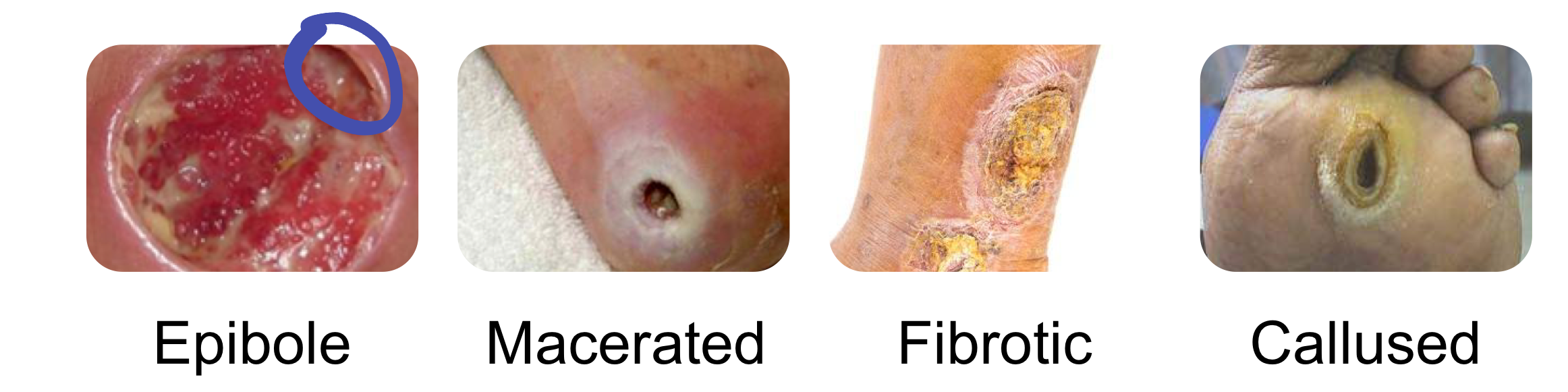
Epibole wound edge
Rolled-under wound edges where epithelial cells have curled down instead of migrating across; stalls healing because the wound “thinks” it’s closed
Macerated wound edge
Soft, mushy, white or pale edges caused by excess moisture breaking down skin (often from prolonged drainage or over-moist dressings)
Fibrotic wound edge
Thick, dense, and tough edges made mostly of scar-like connective tissue; usually from chronic inflammation or long-standing wounds
Callused wound edge
Hard, thickened skin around the edges from repeated friction or pressure; common in diabetic foot ulcers and can block epithelial migration
Lab tests for wounds
CBC
Wound culture and sensitivity
Serum protein
Albumin
Prealbumin
CBC
Measures WBC (infection concern) and hemoglobin (anemia concern)
Wound culture + sensitivity
Done when there is an infection to determine what the bacteria is and what antibiotics work on it
Serum protein, albumin, and prealbumin
All 3 are used to determine nutrition status
Protein: measures overall protein in blood
Albumin: measures long-term nutritional status
Prealbumin: measures short-term nutritional status
Purpose of nutrition for wound healing
provides the body with the necessary building blocks to repair damaged tissue, fight infection, and maintain overall health
Prevention of pressure injuries (7)
Reduce pressure over bony prominences
Smooth surfaces
Frequent weight shifts (repositioning)
Exercise and ambulation
Lifting devices (particularly helpful to prevent injury from shearing or friction)
HOB < 30 degrees
Early nutritional consultation
Prevention devices
Mattresses that are air filled and can blow up in ways that are best for the patient’s body
Pillow
Heal boots (for ppl that are immobile to prevent friction from the bed)
Treating pressure injuries
Remove direct pressure
Do not massage reddened areas
Provide devices to reduce/diffuse pressure
Increased repositioning
Provide ROM exercises
Consult Certified Wound and Ostomy Nurse (CWON)
Clean and dress the wound as prescribed
Obtain culture & sensitivity (C&S) if indicated
Collaborate with wound care/skin service providers
Teaching for patient and family
Autolytic wound debridement
uses body’s own enzymes to break down tissue
Enzymatic wound debridement
enzyme containing ointment, speeds rate of necrosis removal
Mechanical wound debridement
wet-to-damp dressings, wound irrigations
Biologic wound debridement
enhance wound healing through contact
Surgical wound debridement
removal of tissue to promote wound healing
Considerations when selecting a dressing
Keep wound bed continuously moist
Keep surrounding skin healthy & dry
Control exudate (wound drainage) without drying out wound bed
Consider time & costs
Types of dressings
Passive
Interactive
Active
Passive dressings
protective only
transparent film
Gauze
Interactive dressings
Protect wound and absorb wound damage
Create a moist environment
hydrocolloid dressings
Manage exudate to aid in healing
Active Dressing
skin grafts and substitutes that actively participate in the healing process
create a moist wound environment
promote autolytic debridement (gently remove dead skin cells)
incorporate bioactive agents or mechanically stimulate wound contraction
Wound vac wound healing
Negative pressure develops to help pull exudate out of the wound

Hyperbaric oxygen therapy
Patient put in chamber that’s has increased pressure and 100% has O2, which increases the O2 levels in the blood and tissues to promote healing and fight infections
