Infectious disease principle (EXAM 2)
1/164
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
165 Terms
What are infectious diseases
diseases caused by pathogens (bacteria, viruses, fungi, parasites, and prions)
**prions are the worst theres no defense against them
how are infections spread
person to person, insects/animals (vector), contaminated food/water, fomites (furniture)
what are the first symptoms of infectious diseases
fever and fatigue
who are most vulnerable to infectious diseases
very young, elderly, immunocompromised, poor socioeconomic status
how is an infection established
microorganism enters host and multiples which results in tissue injury (directly though cytotoxins and indirectly through inflammatory response)
first line of defense against establishment of infection
physical and chemical barriers
inflammation
Physical barriers to infection
squamous epithelium (first line)
mucous membranes containing lysozymes
chemical barriers to infection
innate immunity activated by foreign proteins
Vascular response to inflammation
vasodilation and increased capillary blood flow (causing heat and redness)
increased vascular permeability; accumulation of fluid in tissues (swelling, pain, and Impaired function)
infiltration of leukocytes
when are plasma derived mediators activated
during inflammatory response
the kinin system
plasma derived mediator
activated by coagulation factor XII
increases vascular permeability (MC bradykinin) leading to vasodilation
bradykinin results in pain and itching
the clotting system
plasma derived mediators
converts plasma protein to fribrinogen then fibrin (component of exudate, crusting, discharge)
Fibrinolytic system
plasma derived mediator
forms plasmin which breaks down fibrin (gets rid of scab)
the complement system
plasma derived mediators
helps our immune system
protein, chemotactic for neutrophils, increase vascular permeability, stimulate release of histamine from mast cells and adhere to surface of bacteria
C3a, c5A, C4a
in the complement system
activate mast cells to release histamine
C3b
in complement system
opsonin (opsonization)
tags making more susceptible for phagocytosis
C5a
in complement system
vasodilation, inc vascular permeability, neutrophil activation
MAC (membrane attack complex) (C5b-C9)
lipid dissolving agent (cell lysis)
help break down cells
part of complement system
histamine
cell derived mediators
mast cells and basophils (when injured)
triggers vasodilation and vascular permeability
serotonin
cell derived mediators
from platelets
increase vascular permeability and vasodilation
prostaglandins
vascular permeability
pain and fever
cell derived mediator
Leukotrienes
vascular permeability
migrate neutrophils
cell derived mediator
Lysosomal compounds
from neutrophils
increase vascular permeability
cell derived mediator
platelet activating factor
platelet aggregation and vasodilation
cell derived mediator
cytokines
secreted from immune cells
inflammation mainly produced by T helper cells and macrophages
cell derived mediator
nitric oxide and oxygen
pro inflammatory mediator
produced by macrophages
toxic to bacteria
cell derived mediator
what is the goal of the inflammatory response
to remove foreign protein and limit the extent of tissue damage
first line and nonspecific
doesn't require prior contact
can be triggered bu infections and non-infections (trauma)
steps in the inflammatory response
acute phase: cells release histamine; vascular permeability and vasodilation and vasodilation
Subacute proliferative phase: inflammation phase; clotting factors and enzymes contrast and plug injuries blood vessels to prevent blood from entering injuries site; signs of inflammation begin
Proliferative phase: blood platelets send chemical signals to move cells in for healing; cells produce collagen to form scar tissue
Remodeling phase: decreased inflammation, complete healing
acute inflammation
first symptoms is redness and heat due to vasodilation
pain and swelling follow
chronic inflammation
response of macrophages and lymphocytes instead of neutrophils
fibroblast proliferation rather than exudates
granuloma formation (associated with fb)
subclinical carrier
asymptomatic carrier
no clinical findings
subacute patient presentation
mild symptoms (not as acute as acute)
acute patient presentation
clinical disease with specific signs and symptoms
anything from self limiting to severe disease
chronic patient presentation
continuous, long term with exacerbations and remission
colonization
presence of microorganisms in or on a host with growth and multiplication but without tissue invasion or damage
commensalism
A relationship between two organisms in which one organism benefits and the other is unaffected
mutualism
A relationship between two species in which both species benefit
(ex: e.coli)
Parasitic
A relationship between two organisms of different species where one benefits and the other is harmed
saprophytes
organisms that live on dead organic matter
virulence
ability to infect and cause a disease
capsule increases virulence
pathogen
very virulent
normal flora
bacteria that colonize skin and mucous membranes w/o causing infection
prevent pathogen colonization
synthesize vitamins
potentially harmful (endogenous disease)
opportunistic pathogen
endogenous organism that is normally commensal that can cause disease and become a pathogen when the hosts resistance is altered
eukaryotes
chromosomes contained in distinct nucleus
prokaryotes
single celled organism without a distinct nucleus with a membrane nor other specialized organelles
virus
cannot replicate on their own
not eukaryotes or prokaryotes
most common infections
respiratory infections (flu, adenovirus, RSV)
meningitis/encephalitis
life cycle of viruses
Attachment via a specific protein on the capsid, to a receptor on the host cell
Viral entry via fusion, endocytosis and release of contents into host cell
Once inside the cell the viral genome is copied, viral proteins produced. The mRNA encoding viral genes are translated into viral proteins using host ribosomes. The viral proteins produced vary from virus to virus and include capsid proteins, envelope proteins, proteins that can block host defenses or assist with viral replication
Viral particles are assembled from the viral proteins and copies of the viral genome.
Complete viral particles are released from the cell and infect other cells.
retrovirus
▪ After entry into host cell viral RNA translated into DNA by viral enzyme reverse transcriptase. Viral DNA is integrated into host chromosome and exists latently
▪ Reactivation requires reversal of this process.
▪ Ex/ Human retroviruses: HIV-1 and HIV-2
oncogenic viruses (oncoviruses)
▪ transform host cells into malignant cells on replication. Ex/ retroviruses and DNA viruses such as herpesviruses ex/HPV (human papillomaviruses) and cervical cancer , EBV and lymphoma
RNA viruses
▪ the common cold, influenza, hepatitis C, West Nile fever, polio and measles, rotavirus
viral diseases
▪ Stop synthesis of normal cell proteins: RNA and DNA
▪ Some weaken cell membranes and lysosomal membranes
▪ Some viral proteins are toxic to cells, immune defenses also may kill virus-infected cells.
parasite advantage
▪ Parasite has advantage (nutrients); presence is usually detrimental to the host. Transmission usually fecal-oral
protozoa
▪ microscopic, unicellular eukaryotes, motile
malaria
Plasmodium Protozoa; transmitted by mosquitos. Reside within RBC; reoccurring cycles of fevers, chills, and other non-specific symptoms
Babesiosis
▪ spread by Ixodes scapularis tick. Infects RBCs. Fever, chills, sweating, headache, body aches, loss of appetite, nausea, fatigue, hemolytic anemia.
Toxoplasmosis (Toxoplasma Gondii)
▪ can lead to brain abscesses in HIV patients with a CD4 T Cell count <200. Transmission: undercooked pork, exposure to cat feces. MRI or CT scan show ring enhancing lesions
Trypanosoma cruzi
trypanosomiasis (Chagas disease, African Sleeping Sickness)
Tape worms (cestodes)
flat bodies with hooks or mouths for attachment
Flukes (trematodes)
▪ Flat bodies with mouth or hooks for attachment: intestinal and urinary: Burrow in skin, travel to lungs, liver, bladder, GI tract
Ascaris lumbricoides (nematode)
type of round worm
fecal oral, common worldwide: Swallow food/water contaminated with eggs, larvae hatch, go to liver, then lungs and alveoli, crawl to trachea, swallowed, travel to small intestine, develop into worms and release eggs, colonic obstruction, biliary obstruction, intestinal perforation
Helminths
parasitic worms
▪ Multicellular: three main life-cycle stages: eggs, larvae, adults
▪ Drugs that kill helminths are frequently very toxic to human cells
arthropods
Presence of an exoskeleton, jointed appendages, and a body composed of specialized regional segments
(ex: ticks, mosquitos)
Ectoparasites
▪ infest body surface, localized tissue damage and inflammation due to bite or burrowing of arthropod
▪ Present with erythematous, edematous eruptions with papules and urticaria common with bites and stings.
▪ Toxic venom can result in systemic autonomic instability, neurotoxicity, organ failure
bacteria
contain circular double stranded DNA and cell walls (except mycoplasma)
have plasmid to increase virulence and resistance
Cocci divide in chains called streptococci, divide in pairs (diplococci), clusters (staphylococci)
Community of bacteria=biofilm; make antibitocs to work harder
growth parameters for fastidious, anaerobes, aerobes, and facultative anaerobe
Fastidious: strict growth; cannot live outside human body (ex: neisseria gonorrhea)
Anaerobes: cannot survive in oxygen rich environment
Aerobes: require oxygen to survive
Facultative anaerobe: adapt metabolism to aerobic or anaerobic conditions: Fermentation , aerobic cellular respiration
how are bacteria identified
gram stain (purple-gram positive)
acid fast stain (membrane resists decolorization of primary stain when treated with acid alcohol.) (ex: TB mycobacteria)
gram positive vs gram negative
Gram +: thick peptidoglycan layer that holds the crystal violet stain
Gram - cannot hold crystal violet stain, counterstained by safranin (red). Have antibiotic-inactivating enzymes. Endotoxins are in outer cell wall especially worry in sepsis (usually gram negative)
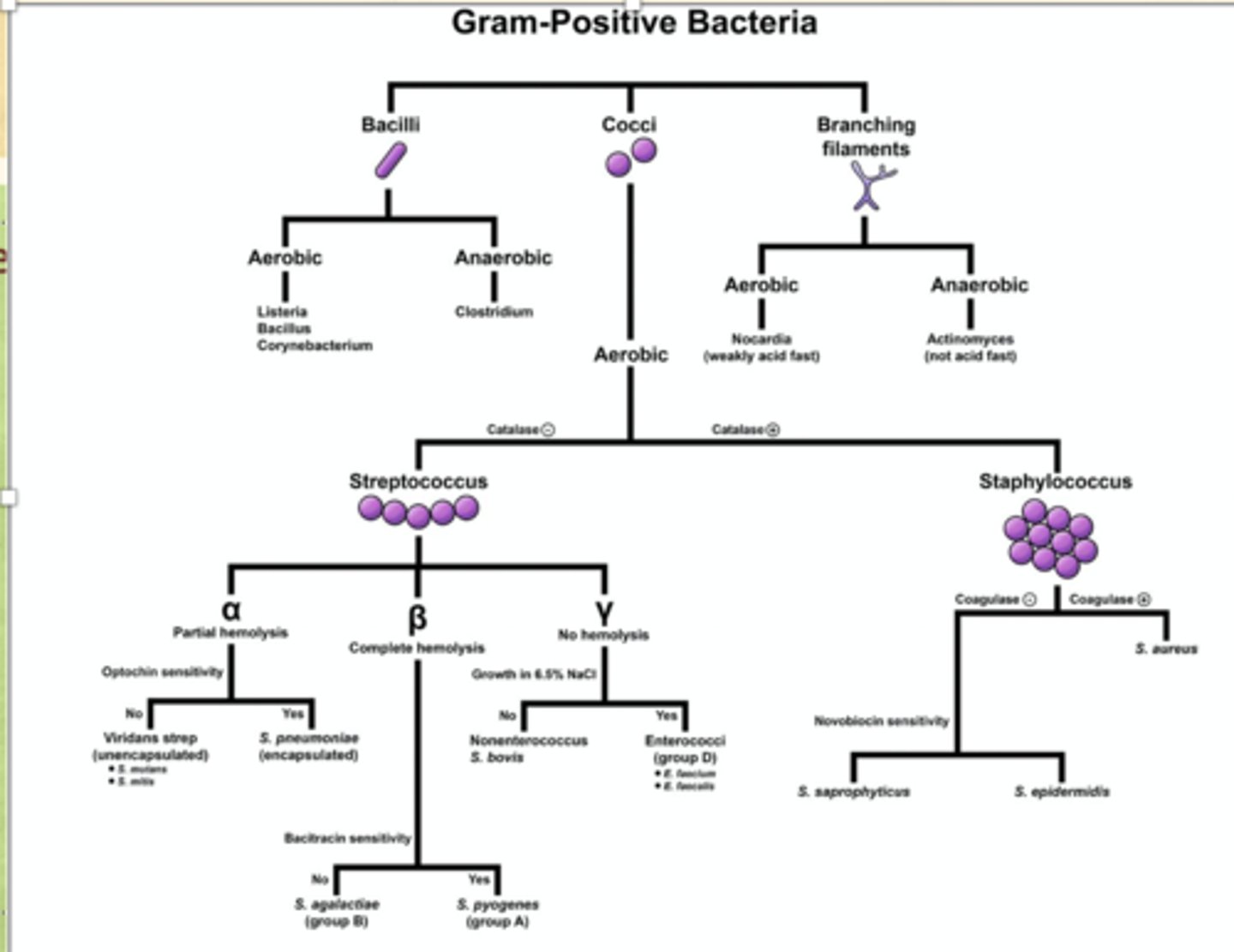
How bacteria are identified (review chart)
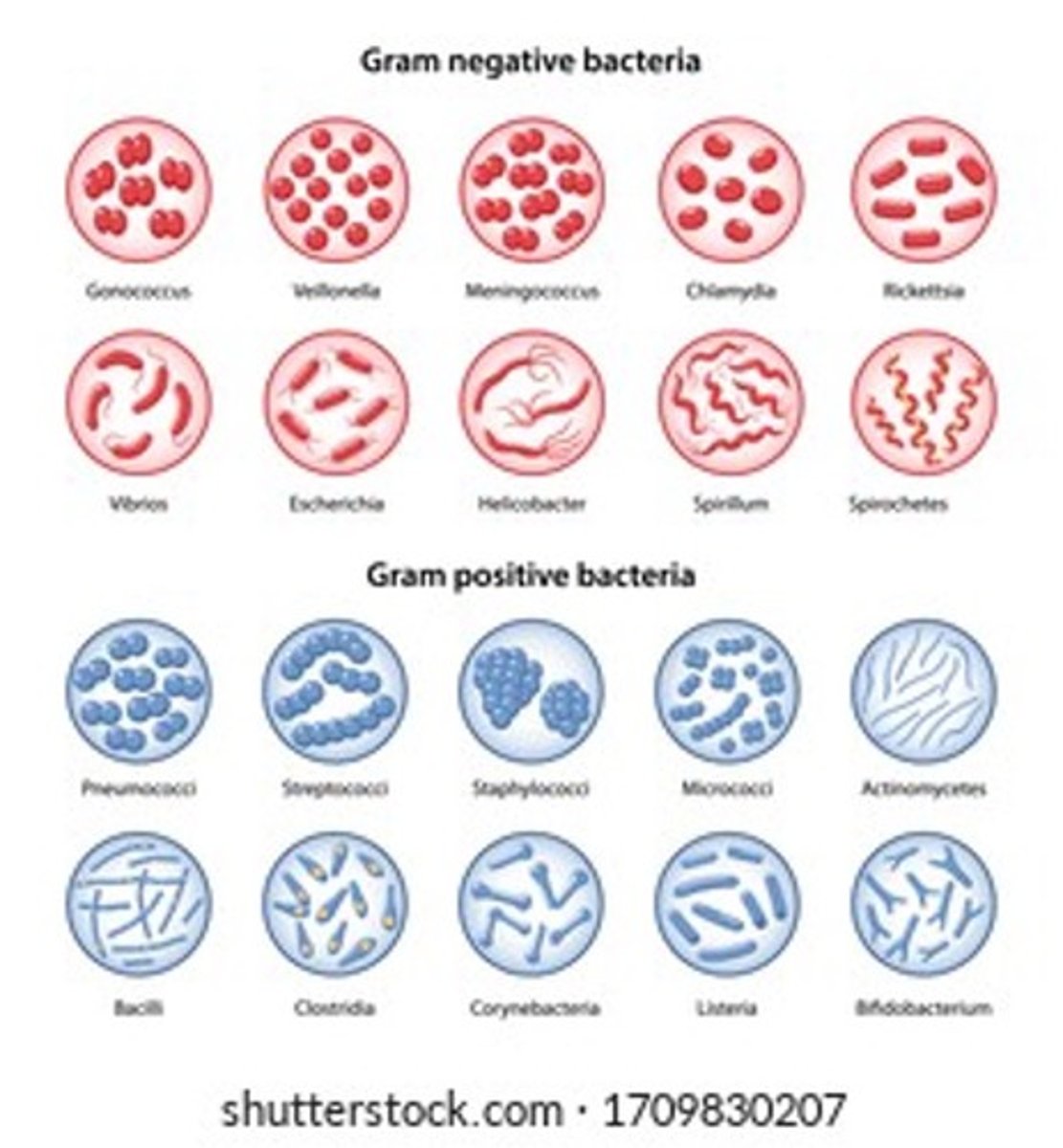
types of gram stains
giemsa stain; usually stains fungus but also bacteria; stain blood cells and bone marrow samples, can stain chromosomes, parasites; stains nuclei dark blue/pink by binding to DNA; is perfered for malaria
india ink; stain is not taken up by polysaccharide capsule ; transparent halo; good for any encapsulated species
silver stain; used for fungi and bacteria and psuedomonis; turns black
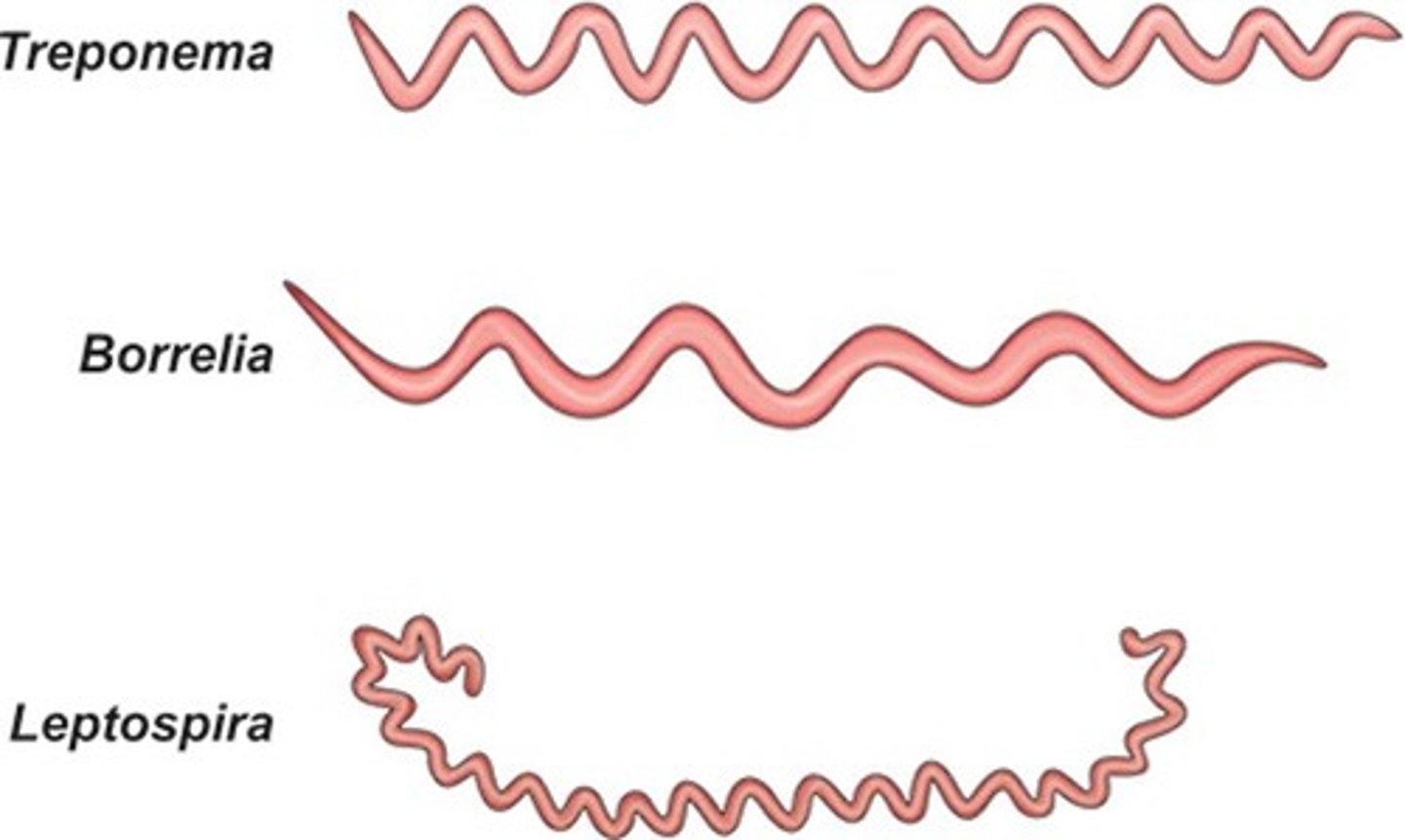
Bacteria: Spirochetes
gram negative coiled rods
anaerobic
Leptospira: Transmitted from infected urine to humans through mucus membranes and can produce fatal Weil syndrome (jaundice, renal, hemorrhage).
Treponema : transmission is direct contact with Treponema pallidum (syphilis)
Borrelia: transmission is animal to human through bite of vector (lice/ticks). (relapsing fever (Borrelia recurrentis), Lyme disease (Borrelia Burgdorferi)
Bacteria - Mycoplasma
Prokaryote, absence of cell wall, flexible cell membrane containing cholesterol
Not visible on gram stain, resistant to beta lactam antibiotics, glycopeptide antibiotics (penicillin and cephalosporins)
Limited metabolic activity, not culturable on standard culture media, requires specialized media with sterols
Can grow under aerobic, anaerobic conditions (facultative)
Primarily affects the respiratory tract by attaching to respiratory epithelium, atypical pneumonia.
Smallest free-living organism; doesn’t live in the cell
diagnosed by PCR
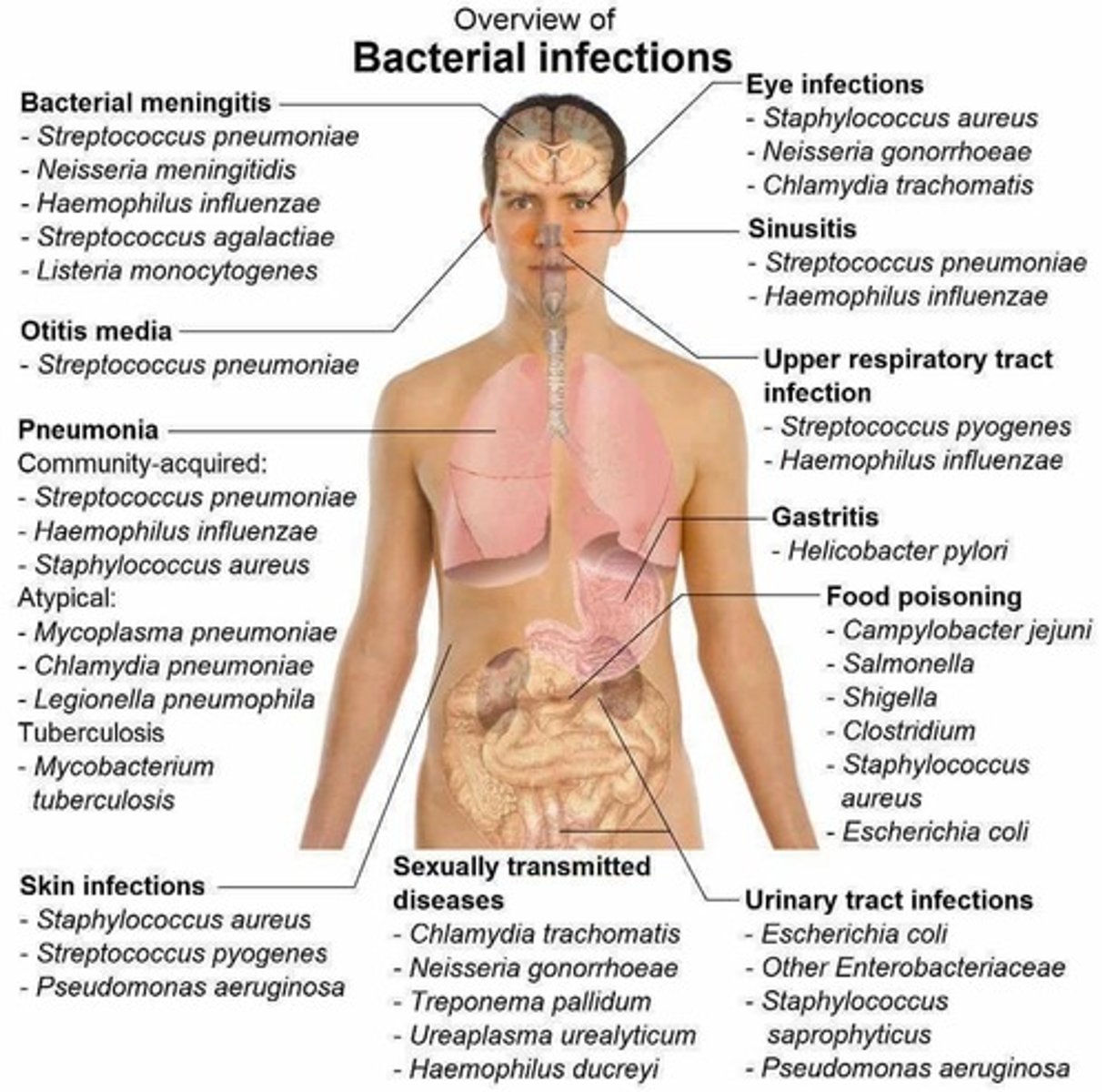
overview of bacterial infections (need to know bacteria and where it causes infection) (image)
gram negative bacteria (chart need to know)
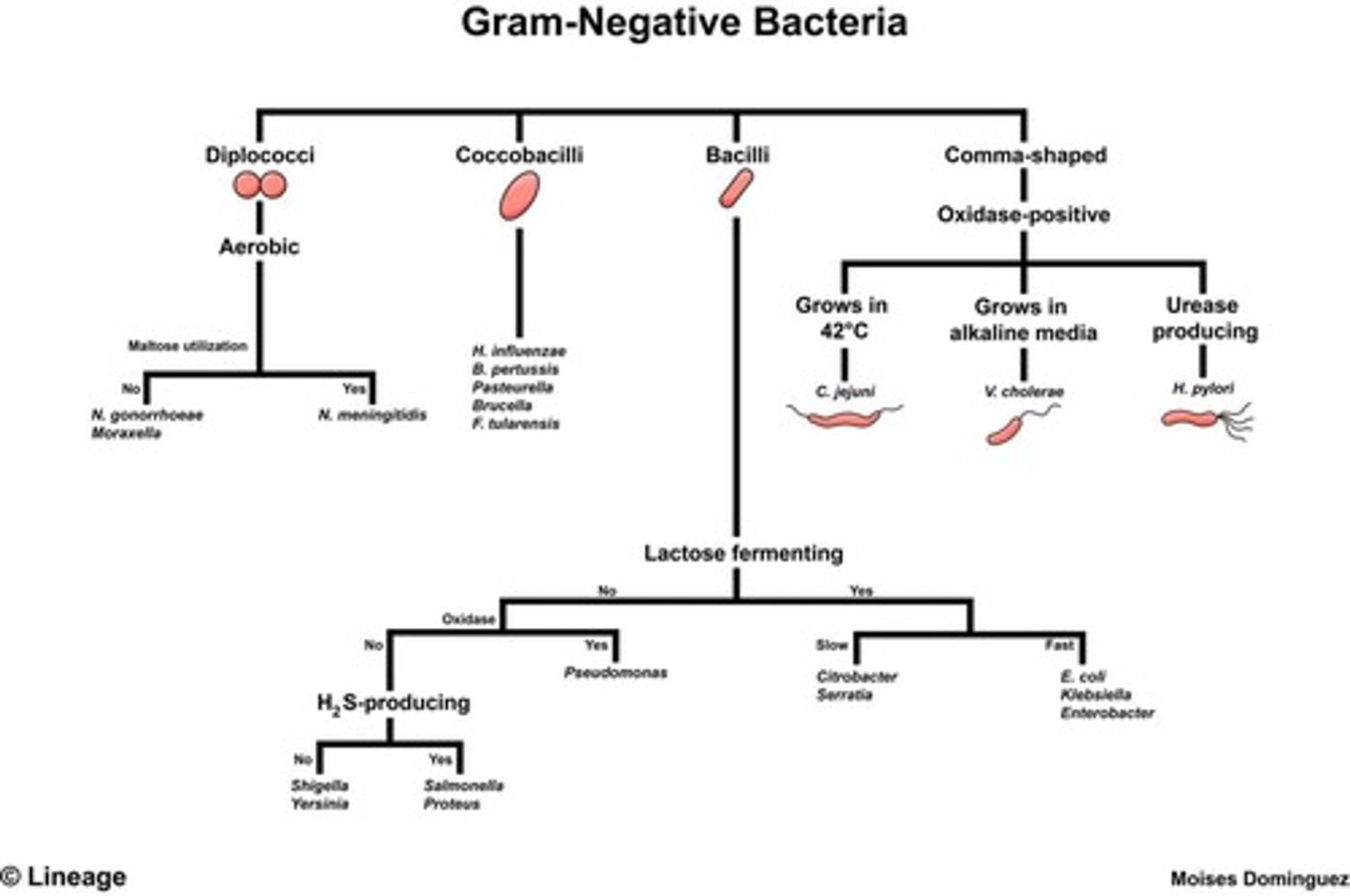
▪ Names by genus followed by species
▪ H2S: hydrogen sulfide producing organism
▪ Oxidase positive: aerobic
▪ Lactose fermenting: produce acidic byproducts
gram positive bacteria (chart need to know)
▪ Catalase positive: enzyme that converts hydrogen peroxide to water and oxygen gas: (sample will bubble)
▪ Coagulase positive: ability to clot blood plasma. Coagulase-positive staphylococci are the most pathogenic species S aureus. (increases virulence)
▪ Acid fast: bacterium have ability to resist decolorization by acids during staining procedures.
Rickettsia and Chlamydia
▪ Vector borne, obligate intracellular pathogen
▪ Have a rigid peptidoglycan cell wall, reproduce by cellular division, contain RNA and DNA like bacteria (don’t gram stain well), depend on host for nutrition
▪ Rickettsiae: transmission to humans via arthropods (fleas/ticks) bites, Ex/ Rickettsia rickettsii: Rocky Mountain spotted fever
▪ Chlamydiae: does not require arthropod vector
Chlamydia trachomatis: genitourinary sexually transmitted disease, ocular infections and pneumonia in newborns. (not usual in eyes and lungs)
Chlamydia pneumoniae: chlamydia pneumonia in those with underlying pulmonary disease (immunocompromised)
prions
▪ Protein without DNA or RNA. No reproductive and metabolic functions (antibiotics don’t work)
▪ Degeneration of neurons; slowly progressive, non-inflammatory results in loss of coordination (ataxia), dementia, death: spongiform encephalopathies (holes in brain) (neurodegenerative disease)
▪ No treatment
▪ Prion associated disease: Creutzfeldt-Jakob disease (CJD): in humans; rapid neurodegeneration causing brain to develop holes
fungi (mycotic)
▪ Primary occur in immunocompetent, and those that occur in immunocompromised. Can be local (skin related; ringworm or vaginal; yeast infection) or systemic (mainly immunocompromised).
▪ Eukaryotic
▪ Yeast
unicellular fungi, reproduce by budding, reproduce slower than bacteria
-Buds that do not separate form long chains of yeast cells called pseudohyphae
-Ex/ Candida albicans forms pseudohyphae
▪ Mold
-multicellular colonies, clumps of intertwined branching hyphae grow by longitudinal extension and produce spores (aspergillosis)
▪ Dimorphic fungi
-Can grow as yeast or mold depending on the environmental conditions: usually grow as a yeast at body temperature and mold at colder temperatures:
-Ex/ Histoplasma, Blastomyces, Coccidioides
Fungi
▪ Inhalation of fungal spores into lungs or direct contact
▪ Dermatophytes: superficial infections in immunocompetent patients; incapable of growing at core body temp, infection limited to cooler cutaneous surfaces. Ringworm, athlete’s foot
▪ Rigid cell wall with non-peptidoglycan layer so PCN does not work
▪ Rarely causes clinical syndromes in immunocompetent hosts. Self-limited infections of skin and subcutaneous tissue(puncture wounds or inhalation): opportunistic infection; found in immunosuppressed patients
Fungi Morphology
▪ Spores: reproductive structure of molds, Coccidioidomycosis and histoplasmosis are transmitted by inhalation of asexual species
▪ Hyphae: long, threadlike, branching, filamentous, tubular structure composed of fungal cells attached end to end, grow by extending from the ends of the tubules
▪ Cell membrane: innermost layer contains ergosterol which is analogous to cholesterol: amphotericin B and nystatin (antifungals) bind to ergosterol, ketoconazole inhibits ergosterol synthesis
▪ Cell wall: surrounds cell membrane, contains complex carbohydrates; explains calcification in chronic infections. can become potent allergen.
▪ Capsule: polysaccharide coating surrounding the cell wall, capsule increases virulence. visualized with India ink stain
Where is Candida, aspergillosis, Tinea, histoplasma/cryptococcus, cryptococcal meningitis found
▪ Candida: found in skin, GI tract (esophagus), lungs
▪ Aspergillosis: found in lungs
▪ Tinea: skin
▪ Histoplasma, Cryptococcus: lungs
▪ Cryptococcal meningitis : meningitis in AIDS patients
Prevalence and incidence
▪ Prevalence: total number of people in a specific group population who have a certain disease, condition; existing cases
▪ Incidence: proportion or rate of persons who develop a condition during a particular time period.
disease occurrence
▪ Endemic: Incidence (new cases) and prevalence (existing cases) are as expected and stable.
▪ Epidemic: abrupt and unexpected increase in the incidence over endemic rates.
▪ Pandemic: epidemic that has spread over several countries or continents, usually affecting a large number of people Morbidity
reasons for an epidemic
▪ Increased virulence of the agent
▪ Introduction of agent into a new setting where it has not been before
▪ Enhanced mode of transmission
▪ Change in susceptibility of the host response to the agent
▪ Increased host exposure
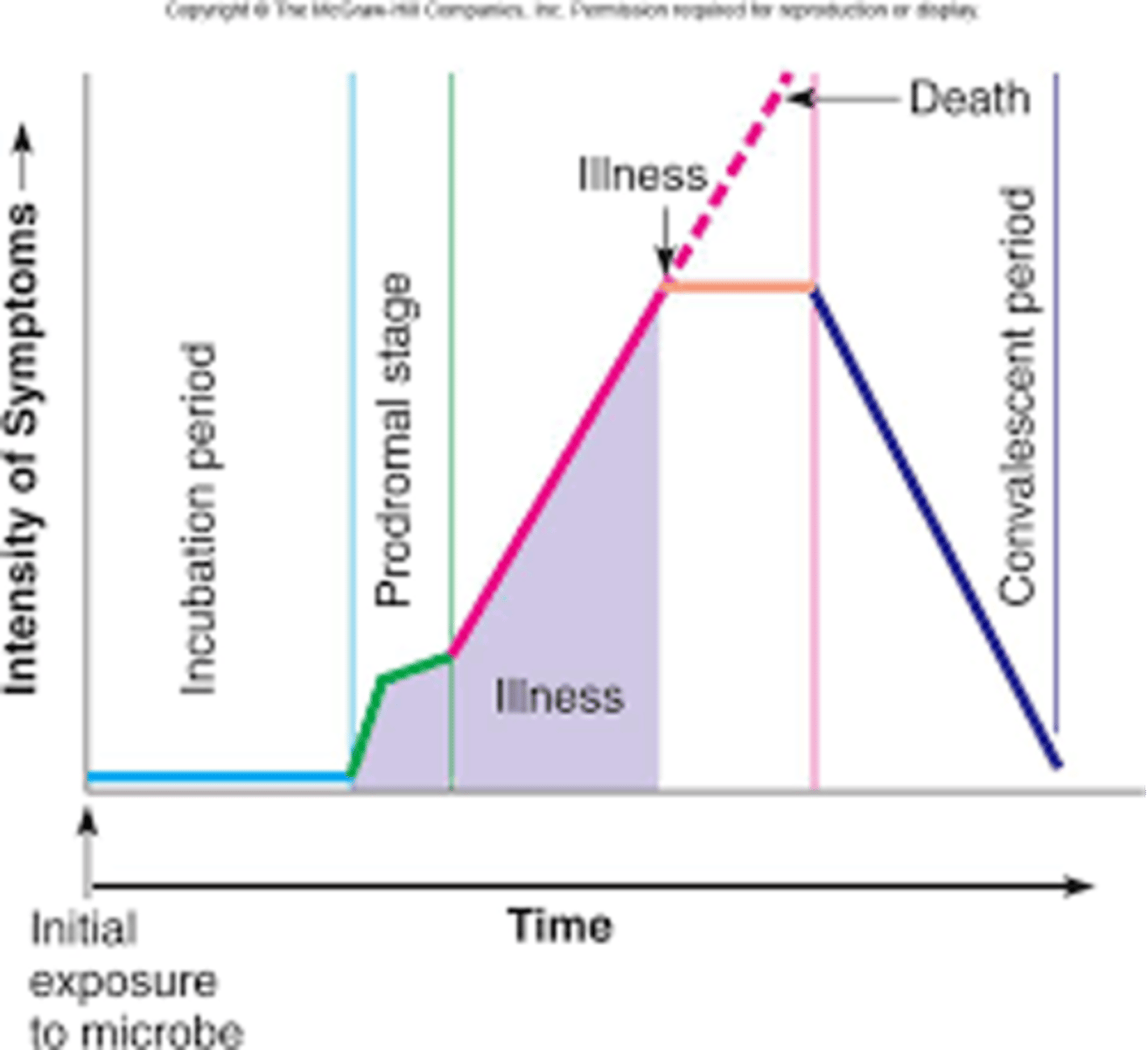
stages of infectious disease
Incubation: Pathogen begins active replication, asymptomatic. Timing can be short (Salmonella food poisoning 6-24 hours vs HIV can be years); dependent on host immune system, dose, and method of infection
Prodrome: Initial appearance of non-specific symptoms in host. Constitutional symptoms (infectious disease): mild fever, myalgia, headache, fatigue (inflammatory response)
Acute stage: Rapid proliferation of pathogen. Immune response results in tissue damage and inflammation. (max impact; specific symptoms)
Convalescent stage: progressive elimination and tissue repair.
Resolution: complete elimination fo the pathogen; no residual symptoms
barriers to resolution (abscess and Biomedical implants)
▪ Abscess: host can contain the infection however unable to eradicate. Usually require surgical drainage.
▪ Biomedical implants: catheters, artificial heart valves, prosthetic bone implants. Infectious agent colonizes surface of implant and creates a biofilm. Usually needs to be removed because antibiotics don’t work against biofilm.
site specific symptoms (-itis in tissue and -emia in the blood)
tissue
▪ Nose: rhinitis
▪ Pharynx: pharyngitis
▪ bronchioles: bronchitis
▪ Intestine: gastroenteritis,
▪colon: colitis
▪ bladder/urethra: cystitis/urethritis
▪ Meninges: meningitis (headache)
▪Brain: Encephalitis
▪ Heart: Carditis
blood
▪ Bacteremia, Viremia, Fungemia, Sepsis or septicemia: microbial toxins in the blood
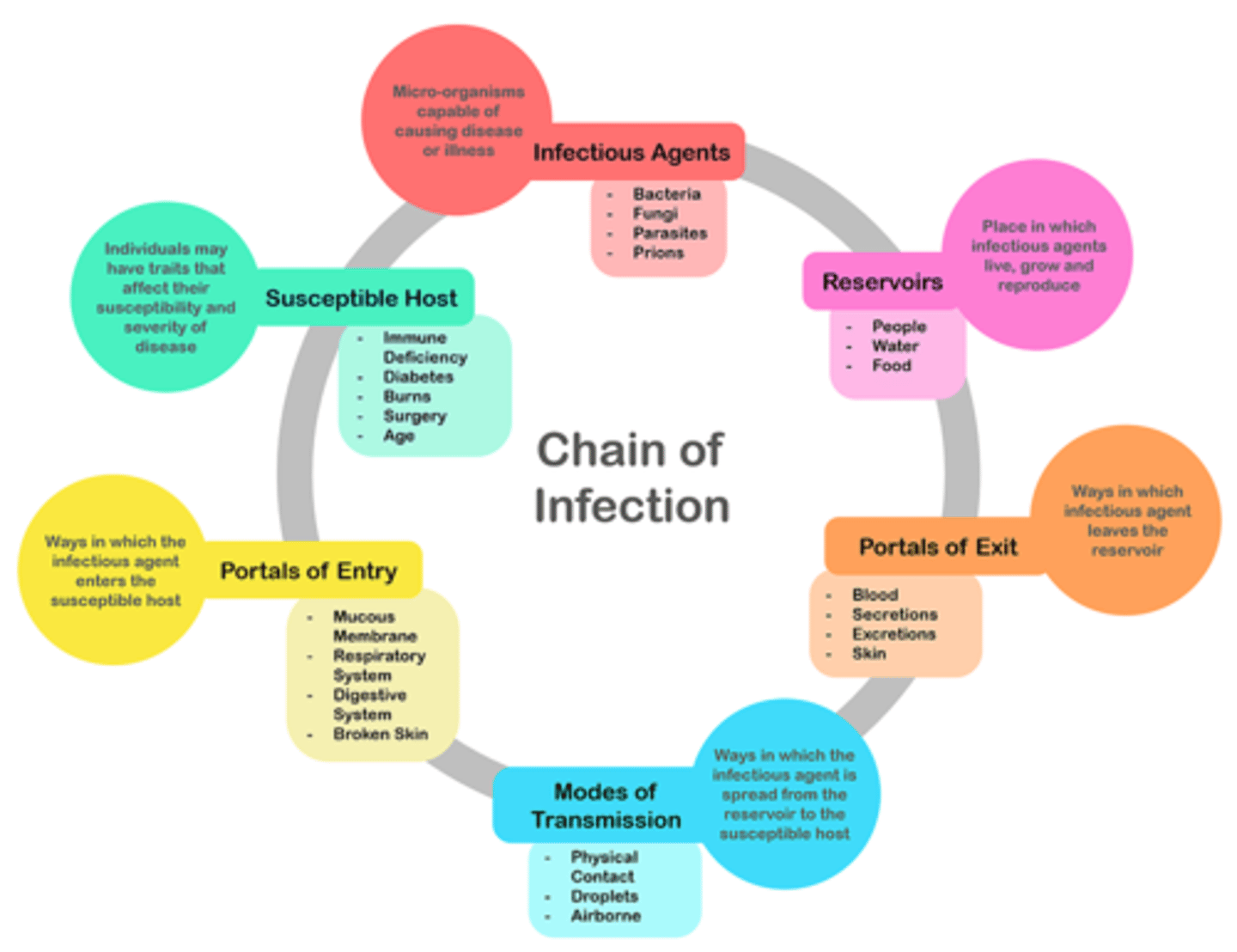
chain of infection (picture)
How we spread infection
In order for infection to spread we need an infectious agent; next reservoir to transmit pathogen (food, water, people, etc.); next portal of exit (sneeze, cough, etc.); mode of transmission (airborne, contact, etc.); portal of entry (breathing it in, wounds, etc.); susceptible host (immunocompromised, age, etc.)
goal: infectious control; breaking the chain
sources of infection (exogenous, endogenous, zoonoses, other)
▪ Exogenous: acquired from external environment: water, food, soil, air, human
▪ Endogenous: acquired from hosts own microbial flora: opportunistic infections
▪ Other: direct contact: person to person, congenital (placenta), inanimate objects (fomites: toys, door), vector (animals, insects)
▪ Zoonoses: from animals to human (ex/white foot mouse is an animal reservoir for the bacteria Borrelia burgdorferi (Lyme disease). Ixodes ticks is an insect vector; tick larva feed on an infected mouse, become infected and transmit to human blood stream through saliva
Healthcare associated infections
▪ “healthcare-associated infections”: both hospitalized patients and community patients
▪ Often resistant to multiple antibiotics
▪ Colonization progresses to infection (symptomatic). Ex/ long term hospitalization often colonized with gram-negative bacteria: risk for pseudomonas pneumonia and sepsis.
direct vs indirect mode of transmission
▪ Direct: transferred from a reservoir to a susceptible host
▪ Direct contact: occurs through skin-to-skin contact, kissing, and sexual intercourse.
▪ Droplet: spray with large, short-range aerosols produced by sneezing, coughing, or talking
▪ Indirect: refers to the transfer of an infectious agent from a reservoir to a host by suspended air particles,
▪ Vehicle: food, water, biologic products (blood), and fomites
▪ Vector: mosquitoes, fleas, and ticks
Susceptible host (chain of infection)
▪ Depends on genetic factors, specific immunity, and factors that affect an individual’s ability to resist infection (ex: sickle cell pts protected from malaria).
▪ Specific immunity: protective antibodies directed against a specific agent in response to infection, vaccine, toxoid (toxin that has been deactivated and retains its capacity to produce antibodies), acquired by transplacental transfer, injection of antitoxin or immune globulin
▪ Nonspecific factors: intact skin, mucus membranes, gastric acidity, cilia in respiratory tract, cough reflex
▪ Factors that may increase susceptibility: steroids, comorbidities, malnutrition, immunocompromised
what can we do to break the chains of infection? (standard precautions and for patient's infected with pathogens)
▪ Standard Precautions: everyone follows
▪ Respiratory hygiene/cough etiquette, handwashing
▪ Safe injection techniques
▪ Use of masks during sterile procedures
▪ For patients infected with pathogens to control transmission:
▪ Early identification, Early isolation, Early treatment
▪ Appropriate isolation of patients infected with communicable disease: contact, airborne, or droplet
do we sterilize our hands
no we disinfect hands
subclinical
▪ symptoms are either very mild or asymptomatic
clinical disease
▪ same as acute stage; specific signs and symptoms
carrier/ chronic carrier
▪ can pass disease on to others. No clinical response to presence of pathogen
latent infection
▪ infected but not symptomatic (dormant)
chronic infectious disease
continuous long term with exacerbations and remissions (HIV, herpes)