Hematology II Bone Marrow and Anemia
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
110 Terms
How many times of bone marrow are there
Two-Red and Yellow
What is the yellow marrow primarily composed of and is it active
Fat, and it is inactive
What is the function of red marrow
It is active in hematopoiesis (blood cell production)
How many total marrow space does an adult have
About 4 liters
How much of an adult’s marrow is acitve
About half
How much total marrow space does a child have
About 1.6 liters
How much of a child’s marrow is active
Nearly 100%
Which bone has the highest percentage of total marrow
The pelvis 40%
What are the preferred sites for bone marrow sampling
Posterior superior iliac crest
Anterior iliac crest in adults
Sternum at second intercostal space
What is bone marrow composed of
A jelly like material dispersed among bony trabeculae and supported by a fine reticulin network
How is the bone marrow supplied with blood
By a main nutrient artery with small terminal arterioles
What is special about about the central blood vessel or the central sinusoid in bone marrow
It has a permeable basement membrane similar to the glomerular filtration barrier in the kidney
What does the bone marrow provide for stem cells
A suitable micro-environment for growth and development
What type of stromal cells are found in bone marrow
Macrophages or Histocytes
Fibroblast or Reticulin cells
Fat cells
Endothelial cells
Osteoblasts
Osteoclasts
What does the bone marrow provide for developing cells
A wet, sticky surface for adherence, a normal population of red marrow cells for interaction, and supportive substances like cytokines, growth factors, and extracellular matrix molecules
What is the normal composition of adult bone marrow
50% hematopoietic tissue and 50% fat
What are the 3 developmental periods in hematopoiesis
Mesoblastic
Hepatic
Myeloid
What happens during the mesoblastic period
Blood islands of the yolk sac form, primarily producing RBC’s, and embryonic hemoglobin is produced
What happens during the Hepatic period
At 5-6 weeks, cell production occurs in the liver, fetal HGB is produced, and the spleen, thymus, and lymph nodes also contribute to production
What happens during the Myeloid phase
At the 5th month, the bone marrow becomes the main site of production, and the liver and spleen engage in extramedullary hematopoiesis
What are the indications for bone marrow examination
Evaluation of Pancytopenia
Leucoerythroblastic anemia
Diagnosis and staging of tumors
Suspected cases of myelofibrosis
Evaluation of myeloproliferative syndrome
Dry tap
What is leukoerythroblastic anemia?
A condition where the bone marrow is infiltrated with metastatic anemia, lymphoma, or granuloma
How is the marrow sample typically collected?
By needle biopsy of the iliac crest under local anesthesia.
What is the first step in collecting a marrow sample?
A needle core biopsy is first obtained.
What happens after the core biopsy?
Some jelly-like marrow substance is aspirated and smeared onto a glass slide.
What is the size of the modified Illinois sternal iliac bone marrow aspiration needle for adults?
Size 15
What is the size of the modified Illinois sternal iliac bone marrow aspiration needle for children?
Size 18
What is the size of the Jamshidi bone marrow biopsy needle for adults?
Size 11 or Size 13
What does a trephine biopsy obtain
A solid core of bone and marrow tissue
What type of needle is used for a trephine biopsy?
A specialized needle with a curved edge
Why is a biopsy more accurate than aspiration?
It is better for determining cellularity and detecting bone-involving processes.
What is obtained during bone marrow aspiration?
A jelly-like marrow substance.
How is the aspirated marrow sample prepared?
It is smeared onto a glass slide for examination
What is a bone marrow aspiration used for
A differential
What stain is commonly used for bone marrow aspiration smears?
Wright-Giemsa stain, along with iron and other necessary stains.
What is the normal % of myeloid cells in the bone marrow
60-70%
What % of erythroid cells is considered normal in the bone marrow
20%
What is the normal % of lymphocytes in the bone marrow
15%
What is the normal % of plasma cells in the bone marrow
2%
What is the normal % of Megas, Monos, Fibroblasts, Osteoclasts, and Osteoblasts in the bone marrow
1%
What is the normal M:E ratio
2.5-4.1
What is the M:E ration typically seen in infection
5-6.1
What M:E ratio is associated with anemia
2:1
What is erythroid hyperplasia
An abnormal increase in the number of red blood cell precursors (erythroid cells) in the bone marrow
What does hypercellular bone marrow mean?
An increase in one or more of the cell lines.
What is the usual mechanism behind hypercellularity?
It is usually a compensatory response.
What causes granulocytic hyperplasia?
Infection.
What causes erythroid hyperplasia?
Anemia
What causes megakaryocytic hyperplasia?
Hemorrhage
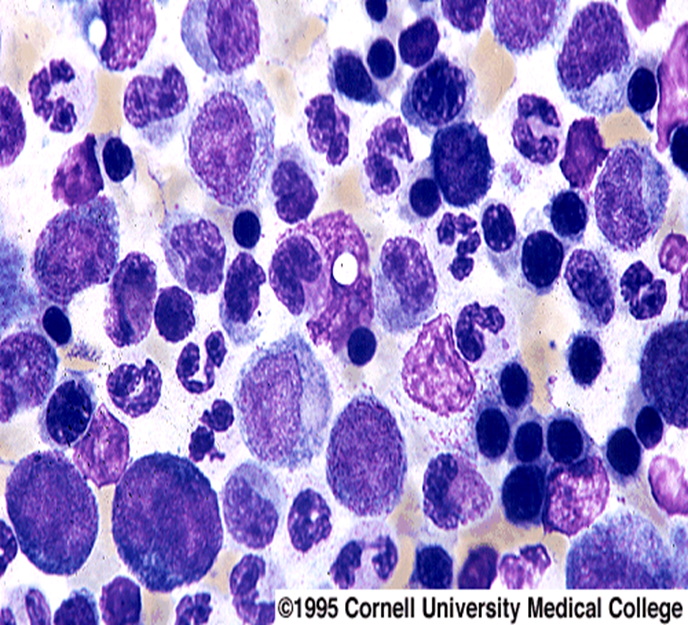
Hypercellular
What does hypocellular bone marrow mean?
A decrease or complete loss of cellularity.
What is aplasia or hypoplasia?
A significant reduction or absence of bone marrow cells.
What are possible causes of hypocellularity?
Idiopathic factors, chemotherapy, radiation, drugs, and viral infections.
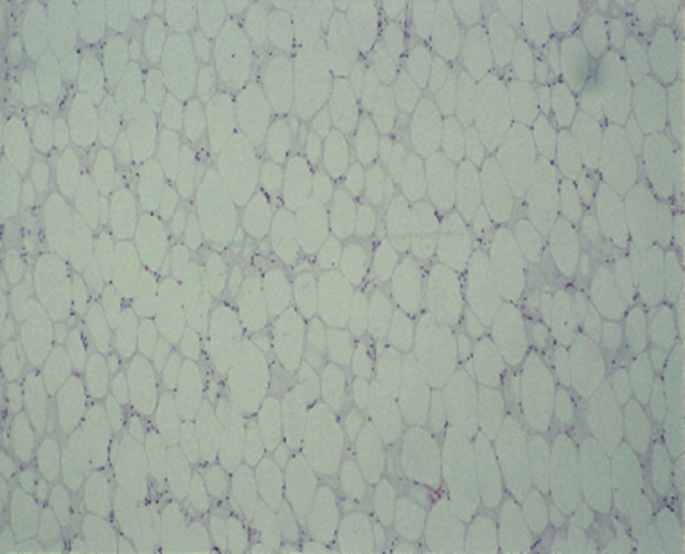
Hypocellular
What anemias are associated with an RPI of < 2 which is ineffective
Hypo proliferative or Maturation
What anemias are associated with an RPI of > 3 which is effective
Hemolytic or Blood loss
What is the goal of a bone marrow transplant?
To rebuild the recipient's blood cells and immune system and hopefully cure the underlying disease.
Where are the donor stem cells obtained from?
Bone marrow or peripheral blood from a healthy donor.
Why are donor cells transferred to the recipient?
Because the recipient's body cannot produce normal blood cells.
What is an autologous transplant?
A transplant using the patient’s own stem cells.
What is an allogeneic transplant?
A transplant using stem cells from a donor of the same species
What is important for allogeneic transplants?
HLA testing or matching.
What is the reference range for RBC for males
4.20-6.00
What is the reference range for RBC for females
3.80-5.20
What is the reference range for HGB for males
13.5-18
What is the reference range for HGB for females
12-15
What is the reference range for HCT for males
40-54
What is the reference range for HCT for females
35-49
What is the reference range for MCV
80-100
What is the reference range for MCH
24-36
What is the reference range for MCHC
32-36
What is the reference range for RDW
11.5-14.5
What is the reference range for PLT
150-450
What is the reference range for NEUT
50-70
What is the reference range for LYMPH
18-42
What is the reference range for MONO
2-11
What is the reference range for EO
1-3
What is the reference range for EO
0-2
Formula for RETIC %
# of RETIC/ # of RBC * 100
Formula for Absolute Retic count
RETIC % X RBC count / 100
What is the formula for RPI
Corrected RETIC count/ Maturation Correction Factor
What is the formula for corrected RETIC count
RETIC % x PT HCT/ Normal HCT
What is anemia?
A condition with decreased hemoglobin, often accompanied by a reduced number of red blood cells.
What are erythrocytosis and polycythemia?
An increase in red blood cells in circulation above normal levels.
What is relative anemia or erythrocytosis caused by?
a decrease in plasma volume, meaning the concentration of red blood cells appears higher than normal because there is less fluid in the blood, typically due to dehydration from factors like vomiting, diarrhea, excessive sweating, or not drinking enough fluids; essentially, it's a "relative" increase in red blood cells rather than an actual increase in their number.
How does plasma volume affect red cell mass (RCM) in relative anemia?
Fluid shifts from the intravascular to the extravascular compartment, decreasing plasma volume and increasing the relative concentration of red blood cells.
In what conditions is relative anemia commonly seen?
Pregnancy and hyperproteinemia.
What is absolute anemia?
A true decrease in red cell mass
What are the categories of hypoproliferative anemias?
Anemia of bone marrow failure
Anemia of systemic disorders
What are the types of maturation disorders in anemia?
Anemia of abnormal nuclear development
Anemias of abnormal iron metabolism
Anemias of abnormal globin development (e.g., Thalassemias)
What are the types of hemolytic disorders?
Hereditary hemolytic anemias
Hemoglobinopathies
Membrane and enzyme disorders
Acquired hemolytic anemias
Non-Immune
Immune
What are the types of anemias of blood loss?
Acute blood loss
Chronic blood loss
What are the symptoms of mild anemia?
No symptoms
Palpitations and dyspnea
Tachycardia, shortness of breath, headache
Pallor of the skin
Leg cramps, dizziness, fatigue, and insomnia
Tissue hypoxia, coma, and death (in severe cases)
What tests are used for anemia diagnosis?
CBC with cell indices (HB, HCT, RBC, MCV, MCH, MCHC)
Reticulocyte count
Blood smear examination
Bone marrow examination
Other: Urinalysis & Occult blood
What is effective erythropoiesis?
When ≥90% of progenitor cells mature into differentiated RBCs.
What is ineffective erythropoiesis?
When progenitor cells are defective and fail to produce mature RBCs.
What is insufficient erythropoiesis?
When there is a quantitative absence of RBC progenitor cells.
What is the etiology of anemia
The cause or underlying pathophysiologic mechanism that leads to the anemia
How is anemia classified morphologically?
Based on RBC indices and direct examination of RBC morphology, including size and hemoglobin content.
What RBC indices are used for classification?
Mean Corpuscular Volume (MCV)
Mean Corpuscular Hemoglobin (MCH)
Mean Corpuscular Hemoglobin Concentration (MCHC)