Clinical Final 👩🔬 - Addiction, Psychotic Disorders, and Ethics
1/111
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
112 Terms
What did statistics Canada find in their 2018 study on hospital discharge data?
First Nations People living on and off reserves have acute hospital care for substance-related disorders 4 to 7 times more than non-Indigenous Canadians
alcohol was not an issue for indigenous people before the French brought brandy and the English brought rum
Define Impulse-control disorders
Disorders in which a person acts on an irresistible, but potentially harmful impulse (Kleptomania or Pyromania)
What is the term for those using multiple mind-altering and behaviour-altering substances?
Polysubstance use
What is a substance?
A substance is any natural or synthesized product that alters perceptions, thoughts, behaviours, and emotions—- PSYCHOACTIVE EFFECTS
What are the levels of involvement with substances?
Substance Use
Substance Intoxication
Substance-related disorders: substance-use disorder + substance-induced disorder
What counts as substance use?
Substance use is the consumption of psychoactive substances
in MODERATE amounts
NOT AFFECTING LIFE socially, occupationally, or educationally
It is NOT a disorder in the DSM-5
What constitutes substance intoxication? What are 3 elements dictating intoxication?
The physiological effects following substance ingestion
impaired decision making
impaired motor control (speech and walking)
mood changes
Intoxication depends on type of substance ingested, the quantity of substances ingested, as well as individual biological reaction to substance(s)
What constitutes substance-use disorder?
Defined by the DSM 5 as:
how significantly substance use effects life socially, educationally, occupationally
puts you in physically dangerous situations (while driving)
continued use despite harms
CRITERIA:
at least 2 symptoms in the last year interfering with life
4 to 5 for MILD and 6 + for SEVERE
P. I. S. R. symptom criteria → direct or indirect activation of reward system in brain
What criteria does the P for Substance Use Disorder in the DSM?
PHARMACOLOGICAL CRITERIA also called PHYSIOLOGICAL DEPENDENCE:
TOLERANCE, increasing or decreasing dosage to experience the same effects of the drug
WITHDRAWAL, unpleasant physiological symptoms when substance is no longer being ingested
Vomiting, diarrhea, chills, fever, etc.
What criteria does the I in Substance-use disorders represent?
IMPAIRED CONTROL, also known as PSYCHOLOGICAL SYMPTOMS
use longer tor more than intended
multiple unsuccessful attempts to stop or reduce
time devoted to a substance
cravings + drug-seeking behaviours
What does the S in the criteria for Substance Use Disorder represent?
SOCIAL IMPAIRMENT
failure to fulfill major role obligations
use despite persistent problems
important activities given up
What does the R stand for in criteria for Substance Use Disorder?
RISKY USE
physically dangerous use
exacerbation of physical or psychological problems
Can yo use drugs and not become addicted to them
Yes, contrary to popular belief, some people can use heroin, cocaine, and crack several times a year without any impact on their lives
what we don’t know is who will become addicted and who won’t
DEPENDENCE can be present without MISUSE
cancer patients take morphine and go through withdrawal without misuse
How can the severity of Substance Use Disorder vary?
Route of Administration
Duration of effects
Polysubstance use
What were alcoholism and drug misuse labeled as in the early editions of the DSM?
Both alcoholism and drug abuse were labelled under SOCIOPATHIC PERSONALITY DISTURBANCES (forerunner of antisocial personality disorder)
seen as a sign of moral weakness
Why are rates of mood disorder and substance use disorder commonly co-morbid with one another?
SUBSTANCE USE AND MOOD DISORDERS may cooccur by chance, simply because they are both very common
DRUG WITHDRAWAL CAN CAUSE SYMPTOMS OF DEPRESSION, ANXIETY + INCREASED RISK TAKING
alcohol ingestion led to increased risk taking in gambling vs gamblers with no alcohol ingested
DISORDERS CAN LEAD TO SUBSTANCE ABUSE
self medication with substances is common
When is a symptom a result of substance use and when is it not?
If a symptom seen in ______ appears within 6 weeks of withdrawal from a substance
not considered a part of the disorder, rather an effect of withdrawal
Symptoms occurring after 6 weeks of a withdrawal may be considered for a seperate diagnosis.
What are 7 complications of substance use disorder according to slides?
Sedating drugs can lead to depressive disorders
Stimulants can lead to substance-induced psychotic disorders and anxiety disorders
Health (needle administration) can be jeaprodized severely
Aggressive or violent behaviour
Accident-related injuries (Liam Payne)
Suicide
Fetal Problems
What are the 5 clusters of drugs as defined in the textbook?
DEPRESSANTS, substances inducing sedation and relaxation (alcohol, benzodiazepines, and barbiturates)
most likely to cause tolerance and withdrawal
STIMULANTS, substances elating mood and increasing activity and alertness (amphetamines, cocaine, nicotine, and caffeine)
OPIOIDS, substances leading to temporary analgesia (pain reduction) and euphoria (heroin, opium, codeine, morphine)
HALLUCINOGENS, substances altering sensory perception and producing hallucinations, delusions, and paranoia (cannabis and LSD)
OTHER, inhalants (airplane glue), anabolic steroids, and other over-the-counter medications (nitrous oxide)
What consists of Alcohol Use Disorder?
Alcohol (sedative, relaxing, depressant) is the most frequently abused substance
DSM REQUIREMENTS:
Clinically significant impairment or distress caused by alcohol misuse of at least 2 of 11 symptoms, for a year:
TOLERANCE + WITHDRAWAL
psychological effects-drug-seeking, impaired control, use despite social problems, risky use, all of it!
MILD - 2 symptoms, MODERATE - 4 to 5 symptoms, SEVERE - 6 or more symptoms
What is the historical perspective of alcohol use disorder?
Alcohol Use Disorder has been recognized throughout history.
1800s-1900s: moral defect
1930s: prohibition in the United States
1940s-1960s: psychodynamic model
1950s: disease model
1960s=1970s: behavioural model
2000s: integrative model
M. P. D. B. I.
What are 5 things to remember about alcohol consumption from the slides?
66% consume alcohol with an 11% increase in the past decade
22% of men exceed low risk and 19% of women
18% drink heavily
9% have alcohol disorder
3% have significant problems
What are 4 ways alcohol consumption patterns vary?
AGE - alcohol use disorder has a early onset of 11-14 years old, and those who drink earlier seem to be at higher risk for chronic and severe alcohol use disorder later
CULTURE
RELIGION
GENDER - affects onset, course, remission
What did Conrod (2013) find about alcohol consumption patterns?
Conrod and colleagues (2013) found 4 personality traits that put adolescents at greater risk of alcohol use disorder:
anxiety sensitivity: fear of anxiety-related sensations
sensation seeking: tendency to seek novel experiences
impulsivity: predisposition to act upon urges without consideration
hopelessness: tendency towards negative thinking
Brief personality coping skill interventions reduced binge drinking and other alcohol related harms
Describe the route of alcohol, once consumed in the body
ESOPHAGUS
STOMACH - small amounts are absorbed
SMALL INTESTINE - easy absorption into the bloodstream
CIRCULATORY SYSTEM + ORGANS/HEART - system distributes alcohol to every major organ in the body including heart and lungs (vaporized and exhaled)
LIVER - enzymes break down and metabolize alcohol into carbon dioxide and water
What are the neurotransmitter effects of alcohol?
GABA (primary inhibitory NT)
Alcohol is a GABA agonist, downregulating the effects of regular GABA
potentially responsible for “anti-anxiety” effects a it becomes difficult for neurons to communicate with each other
GLUTAMATE (primary excitatory NT)
Alcohol downregulates GLUTAMATE, potentially responsible for blackouts
SEROTONIN (mood, sleep, eating)
potentially responsible for alcohol cravings
DOPAMINE (reward system)
possibly responsible for the pleasurable feelings of alcohol consumption
What can be produced in the body from certain doses of alcohol?
Endogenous opioids, the body’s naturally occurring analgesics (pain-killers)
What are components of alcohol withdrawal symptoms?
WITHDRAWAL DILIRIUM or DILIRIUM TREMENS
frightening body tremors and hallucinations resulting from alchol withdrawal
Does alcohol permanently kill brain cells?
Maybe: evidence comes from heavy drinkers who experience blackouts, hallucinations, and seizures
ORGANIC BRAIN DISORDERS → dementia and Wernicke Korsakoff Syndrome
DEMENTIA: loss of intellectual abilities that can be associated directly with neurotoxicity from alcohol consumption
WERNICKE-KORSAKOFF SYNDROME: confusion, loss of muscle coordination, and unintelligeble speech due to thiamine deficiency (from alcohol largely)
Blood Alcohol Level + standardized ethanol units
Standardized ethanol unit: 0.5 oz ethanol
is found in 1 oz of hard liquor, 5 oz of wine, 0.5 pint of 5% beer
BAL = 0.06 (2 to 4 drinks) - warmth, euphoria, loss of certain motor control
BAL = 0.09 (4 to 6 drinks) - exxagerated emotion, talkative, noisy, legally drunk
BAL = 0.12 (6 to 8 drinks) - clumsiness, unsteady walking, narrowing visual field
BAL = 0.15 (8 to 10 drinks) - very drunk, lack of coordination, tunnel vision
BAL of 0.35 brings someone to a coma
What is Fetal Alcohol Syndrome?
Fetal Alcohol Syndrome is a pattern of problems relating to the victim’s drinking levels while pregnant
cognitive and learning difficulties
behavioural deficits
small eye openings, short nose, underdeveloped jaw, thin upper lip, small head + flat face
What are the Canadian recommendations for drinking?
LOW RISK: 0 to 2 drinks a week for everyone
HEAVY DRINKING: 4 or more drinks on one occasion for women, 5 or more drinks on one occasion for men, at least once a month over a year
What are the 4 effects of alcohol use disorder?
Acute effects
Chronic effects
Neurological effects
Social effects
What are the 4 acute effects of alcohol use disorder?
Respiratory Suppression - shallow breathing leading to CO2 in the blood
Hemmorhagic pancreatitis - bleeding into or around the pancreas
Asphyxia - oxygen deprivation leading to unconsciousness or death
Withdrawal - GABA receptors become less sensitive, glutamate activity can lead to over-excitation and cell death, in severe cases 5% develop delirium tremens and 1-5% die
treatment: benzodiazepines and acamprosate (GABA agonist that’s less addictive and controls excitotoxicty when ethanol is withdrawn)
What are 2 types of chronic effects of alcohol use disorder?
Gasointestinal
Liver (Fatty liver, hepatitis, cirrhosis - scarred tissue replacing healthy tissue)
What are the 4 neurological effects of alcohol use disorder?
Wernicke-Korsakoff Encephalopathy (thiamine defficiency)
Alcohol-induced dementia (lesions)
Peripheral neuropathy (nerve damage)
Fetal Alcohol Syndrome (growth retardation, cognitive deficits, behaviour problems, learning difficulties)
What are 4 social effects of alcohol use disorder?
Accident-related
Legal - violent crimes, people with poorer executive function are more likely to be aggressive when intoxicated (Robert Phil)
Social
Economic
What are the biological factors of alcoholism?
GENETICS:
family history, adoption, and twin studies suggest that genetics play a substantial role as high as 50%
CENTRAL NERVOUS SYSTEM CIRCUITS:
James Olds found the Pleasure Pathway → DOPAMINERGIC SYSTEM in MID BRAIN through NUCLEUS ACCUMBENS to FRONTAL LOBE
substances that inhibit GABA directly increase dopamine availability in the reward center
66% alcoholics (vs 33% non alcoholics) carry a DRD2 gene regulating dopamine 2 receptor
What are the 3 psychological influences of alcoholism?
Learning - reinforcement (positive or negative), conditioning (stimuli paired with anxiety reduction become conditioned stimuli)
Cognitive - alcohol expectancies (personal beliefs of what will or won’t happen when drinking)
Social Modeling - parents and peers, UBC Pit study
What are the socio-cultural influences of alcoholism?
Some religions ban alcohol or drug use
Some cultures expect heavy drinking on occasion
Media depictions of alcohol
What are opioid-related disorders?
OPIATE is the natural chemicals in the opium poppy that create narcotic effects (reducing pain—analgesic—-and inducing sleep), OPIOIDS include opium, morphine, heroin, codeine, methadone, and oxycoton.
DSM:
again, at least 2 symptoms for 1 year of pharmacological symptoms (withdrawal and tolerance), psychological effects (seeking behaviours + impaired control), affecting social life, risky use
What are included in the clinical picture of opioids?
13% of Canadians use opioid pain relievers (2% for non-medical reasons)
34% increase in ER emissions
OPIOID DEPENDENCE: 12 month prevalence in adults of .37% and up to 1% in young adults
onset: late teens/early adulthood + 37% from earlier prescriptions
course: chronic, 20-30% long term abstinence
gender: twice as high in men than in women (where prescription opioids are more common)
culture: higher in the indigenous community
What are 3 complications related to opioid related disorders?
DEPRESSION
LEGAL PROBLEMS
HEALTH (HIV/AIDS - B.C. has the highest rates in the developed world, HEPATITIS - 90% of intravenous users, SKIN ABCESSES/SCARRING
What are the mortality rates of opioid related disorders?
MORTALITY is 94% accidental with fentanyl as a large cause
22% mortality vs 12% for the rest of population
average age of death 40, 33% overdose and 50% are homicide, suicide, or accident
Weed 101
THC tetrahydrocannabinol is high inducing
CBD cannabidol is anti-inflammatory and analgesic
K2/SPICE are dangerous synthetic versions of THC
Anandamide, brain’s own THC
15-20% of Canadians use cannabis with 26% being young adults (more common in those with mental disorders)
400 chemical compounds with limited research (case studies with open designs, single dose lab setup, using synthetic > actual plant)
Response varies by strain, means of administration, and THC dose
What is part of the clinical description of Cannabis Use Disorder?
At least 2 symptoms for a year
9% develop a dependence(versus 32% for nicotine and 10-12% for alcohol)
4% men and 1% women are heavy users + youth are at risk
moderate heritability from twin studies
What are the 4 repercussions of cannabis use disorder and heavy use, plus tolerance and withdrawal effects
TOLERANCE - some say they experience “reverse tolerance” feels better after repeated use
WITHDRAWAL (33% of regular users) tiredness, irritability, appetite loss, IMPAIRED CONTROL + OCCUPATIONAL AND EDUCATIONAL DISTURBANCES
and
Decreased reactivity to dopamine + reward circuitry
amotivational syndrome
lung cancer, bronchitis, esophagus
motor vehicle accidents and er visits from panic
What is the relationship between schizophrenia and marijuana use?
SCHIZOPHRENIA is found in vulnerable adolescents
a family history of psychosis brings you to 10% risk
marijuana doubles this risk to 20%
mechanisms are unclear, but disrupts normal neurological development
What are the biological treatments for Substance Use Disorders?
ANTAGONISTS
naloxene
used for overdose, acting within 2 minutes and lasting 30-60 minutes - many need multiple doses and causes opioid withdrawal
naltrexone
used for opioid abuse, blocking opioid receptors for pleasure and also used to decrease craving for alcohol
acomprasate
upregulates GABA to protect from withdrawal symptoms
AGONIST SUBSTITUTIONS (providing safer drugs)
methadone
opioid agonist
buprenorphine
partial agonist/antagonist that is more effective than methadone + less withdrawal, can be combined with naloxene
nicotine patches
AVERSIVE TREATMENTS
disulifram (antabuse) for alcohol, preventing acetaldehyde breakdown and making it hell
anti anxiety and depression medication
What are the psychosocial treatments for substance use disorder?
ALCOHOL ANONYMOUS/NARCANON
effective if continued, but 75-85% dropout rate
RESIDENTIAL TREATMENT CENTERS
expensive, not more effective than outpatient treatment
beneficial for managing withdrawal symptoms and stabilization
BEHAVIOURAL + COGNITIVE TREATMENT
learning self-control strategies and learning situation managemnet
HARM REDUCTION
controversially controlled drinking
safe injection sites
relapse prevention
Explain Behavioural Addiction
BEHAVIOURAL ADDICTION is a compulsion to repeatedly engage in non-drug related behaviour despite negative consequences
beyond substance definition of tolerance + withdrawal, as well as dopamine circuitry alteration
gambling, sex, and provisional internet gaming
What is the clinical picture of gambling addiction?
GAMBLING ADDICTION was the first behavioural addiction to be recognized, may activate the same brain systems as pharmaceuticals
blunted VMPFC activation, limiting risk-reward assessment
up to 3% of the population with 1% severe cases
chronic disorder - only 1.3% in B.C. seek treatment
What are the dysfunctional cognitive beliefs of gambling addiction?
GAMBLER”S FALLACY believing result of an independent event is influenced by previous events
HOT HAND FALLACY believing success in an independent event will predict future successes for other events
“NEAR"“ WINS results appearing as almost a win to motivate further gambling
ANTHROMORPHOTISM assuming control
What is internet gaming disorder?
INTERNET GAMING DISORDER is a provisional behavioural addiction
tolerance and withdrawal
preoccupation or excessive use
impairment in education or occupation + social functioning
What is hypersexual disorder and what are its nuances?
HYPERSEXUAL DISORDER is a sexual promiscuity and behaviours in response to distress
1-2 hours a day of excessive masturbation, pornography dependence, or cyber sex
at risk for STDs, unwanted pregnancy, and relationship disturbances
Definition does not signify how much is too much, and there is no information about heritability and developmental causes - what is “normal” and what is excessive
What is Schizophrenia?
SCHIZOPHRENIA is a cluster of symptoms on a large spectrum, involving disturbances in:
thought (delusions)
perceptions (hallucinations)
speech, emotion, and behaviours
full recovery is rare, though present in 1 of 100 people
Is it one disorder or many? There is heterogeneity of a spectrum!
What is psychosis? What 4 disorders is it involved with?
PSYCHOSIS is a term to characterize many symptoms of unusual, realty-distorting behaviour, but mostly:
HALLUCINATIONS sensory phenomena without external input
DELUSIONS disorder of thought and belief content
PSYCHOTIC SYMPTOMS are in
BIPOLAR DISORDER
SCHIZOPHRENIC SPECTRUM DISORDER
SEVERE MAJOR DEPRESSIVE DISORDER
SOME PERSONALITY DISORDERS
What is schizosphrenia spectrum disorder in DSM? What are the 7 things to remember?
SCHIZOPHRENIA SPECTRUM DISORDER is a collection of disorders, all commonly marked by distorted reality, falling under:
SEVERITY of symptoms
DURATION of symptoms
PROGNOSIS
Constitutes of:
Attenuated psychosis syndrome
Schizotypal Personality disorder
Delusional disorder
Brief Psychotic episode
Schizophreniform disorder
Schizophrenia (most common)
Schizoaffective disorder
What are the misconceptions of schizophrenia?
People that are previously violent are more likely to be violent + dangerous than those with schizophrenia
Bleuler thought of Schizophrenia to be due to a split personality, confused with DID
What did Kraeplin and Bleuler contribute to the discussion of schizophrenia?
What is the criterion for Schizophrenia diagnosis?
CLUSTER A (2)
Postive and/or negative symptoms
Florid symptoms present at least 1 month and persisting for 6 months (in the absence of medication)
at least one must be hallucinations, dellusions, or disorganized speech
CLUSTER B
social and occupational impairment
CLUSTER C
continous signs of disturbance for over 6 months
What are the positive symptoms of schizophrenia?
POSITIVE SYMPTOMS refer to symptoms grounded in distorted reality:
hallucinations, sensory events without external stimuli: auditory (most common), visual, olfactory, gustatory
delusions, disordered thoughts and beliefs not shared by others, commonly: prosecution, reference, influence, Cotard’s syndrome, Capgras Syndrome, Grandiose
What are Cotard's and Capgras syndrome?
COTARD’S SYNDROME is a postiive symptom of schizophrennia as part of delusions
belief that one is dead, dying, or non-existent
CAPGRAS SYNDROME is a postiive symptom of schizophrenia as part of delusions
belief that a familiar has been replaced by an identical imposter
What are the disorganized symptoms of Schizophrenia?
THE DISORGANIZED SYMPTOMS of schizophrenia include:
DISORGANIZED SPEECH
derailment, loose associations
tangential thinking - going off topic
incoherence - “word salad”
neologisms
clang associations
GROSSLY DISORGANIZED/CATATONIC BEHAVIOUR
impaired grooming
inapropriate sexual behaviour
unpredictable agitation or aggression
odd mannerisms
catatonic motor behaviours
What are the negative symptoms of Schizophrenia?
NEGATIVE SYMPTOMS of schizophrenia include:
AVOLITION inability to initiate and persist in activities, associated with poor outcomes
ALOGIA impoverished or absence of speech
ANHEDONIA indifference to pleasant activities
ASOCIALITY lack of interest in social interactions
AFFECT FLATTENING diminished emotional expression
What is the clinical picture (onset, prevalence, and course) of schizophrenia?
ONSET
normally preceded by a prodromal period (1-2 years), but can occur abruptly
residual period occurs with only negative symptoms or attenuated positive symptoms
PREVALENCE
around 1%
men (onset earlier) > women (onset later, with more favourable outcomes)
more common in developed countries (more common in indigenous and african-canadians)
COURSE
1 episode (-22%) has favourable outcomes
35% have exacerbations or remission
8-12% have chronic course
35% have progressive worsening
Overall a reduced life expectancy is present for those with schizophrenia (10-15 years) because of suicide, cardiovascular disease, substance abuse, diabetes, etc.
What is SCHIZOTYPAL PERSONALITY DISORDER?
SCHIZOTYPAL personality disorder is a relatively stable condition marked by pervasive social and interpersonal deficits (5 of the following):
ideas of reference
odd beliefs or magical thinking
unusual perceptual experiences
suspiscousness or paranoid ideation
odd thinking or speech
inappropriate affect
excessive social anxiety that does not diminish with familiarity
odd, ecentric, or peculiar behaviour
lack of close friends other than relatives
9 total deficits
What is Delusional Disorder?
DELUSIONAL DISORDER is the presence of one or more delusions, more circumscribed than other spectrum disorders:
EROTOMANIC
GRANDIOSE
JEALOUSY
PERSECUTORY
SOMATIC
very rare (.2%)
What is Brief Psychotic Disorder?
BRIEF PSYCHOTIC DISORDER are the postive symptoms of psychosis: delusions, hallucinations, disorganized speech, grossly disorganized behaviour
for less than 1 month with a tendency to remit on its own (good outcomes)
prevalence of .9% of psychotic disorders
What is Schizophreniform Disorder?
SCHIZOPHRENIFORM DISORDER are positive and negative symptoms of psychosis for a duration of 1 to 6 months
if presumed with good lifestlye, may resume with normal life
In 0.2% of population
What is Schizoaffective Disorder?
SCHIZOAFFECTIVE DISORDER is a mood disorder as well as schizophrenia
prevalent in 0.3%
What are the genetic contributions (family, twin, and adoption studies) to Schizophrenia disorder?
Genes are responsible for making some individuals vulnerable to schizophrenia
FAMILY STUDIES
48% identical twin with schizophrenia
46% for two parents with schizophrenia
9% sibling with schizophrenia
6% one parent with schizophrenia
5% one grandparent with schizophrenia
1% of the general population
TWIN STUDIES (Gottessman et al.)
48% concordance rate for MZ twins (100% genes and environment)
17% concordance rate for DZ twins (50% genes and 100% environment)
How heritable, 40% 60% 80%? Higher rates includes “probable psychosis”
ADOPTION STUDIES
22% for a child with a schizophrenic mother
1% for a child of a non-schizophrenic mother
What is a genetic trait associated with schizophrenia?
A genetic marker for schizophrenia is smooth-pursuit eye movement
What are the 2 theorized biochemical contributions to schizophrenia?
1. DOPAMINE CIRCUIT DYSFUNCTION
a two factor theory, that dopamine is deficient in the D1 receptor sites of the FRONTAL AREAS and dopamine is excessive in the D2 receptor sites of the striatal areas
2. GLUTAMATE DYSFUNCTION
due to GABA dysfunction or excessive dopamine, an underactivity at NMDA receptors, too much NMDA results in too little glutamate, operates through NMDA receptors
PCP and “special K” createa schizophrenic-like symptoms
What is the 2 Factor theory of Dopamine dysfunction in relation to schizophrenia?
1. DOPAMINE CIRCUIT DYSFUNCTION
a two factor theory, that dopamine is deficient in the D1 receptor sites of the FRONTAL AREAS and dopamine is excessive in the D2 receptor sites of the striatal areas
treatment is dopamine antagonists (which already are antipsychotic drugs)
drugs produce negative side effects similar to parkinson’s disease
L-DOPA (dopamine agonist) can produce psychotic symptoms in some people
amphetamine activates dopamine and makes psychotic symptoms worse
CONTRASTING EVIDENCE:
dopamine agonists are not universally effective
CLOZAPINE, a weak dopamine antagoist is still effective
there is discontinuity between dopamine blockage and symptom change
less helpful in reducing negative symptoms
What are the structural and functional brain abnormalties realted to schizophrenia?
PET and fMRI: hypofrontality (reduced blood flow to FC)
MRI studies: enlarged ventricles
Reduction in grey matter
Low synaptic density in schizophrenic brains
there are cause and effect issues, but changes can be seen after first psychotic episode
changes are not specific to schizophrenia, also seen in major depression
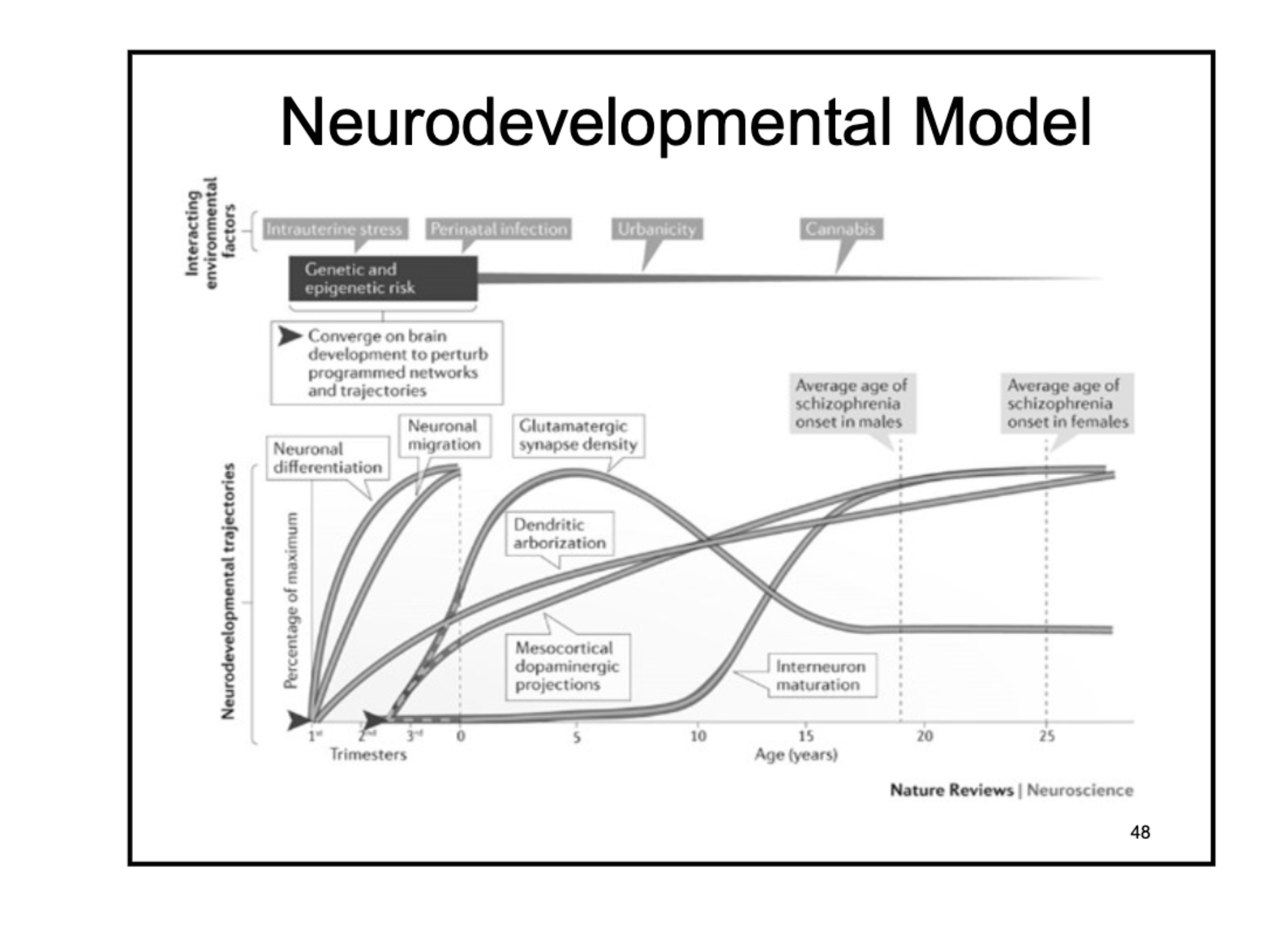
What is the contemporary model of schizophrenia? What 4 elements support this model?
NEURODEVELOPMENTAL MODEL suggests that early deficits in cortical development manifests as schizophrenia in later life during stressful late adolescent periods
smaller head circumference at birth
slower to reach developmental milestones
higher rates of left-handedness
congenital minor physical and craniofacial abnormalities
Evidence comes from high-risk studies looking at birth complications (obstetric complications, premature births, hypoxia)
What did Kallman discover for schizophrenia?
Kallman showed that the severity of the parent’s disorder influenced the likelihood of the child having schizophrenia as well.
you inherit a general schizophrenia vulnerability, which then can manifest either as the same one your parent has or a different one
What are theories attributing to the neurodevelopmental model?
PHYSICAL STRESS
1st semester maternal starvation (Dutch Hunger winter of 1945)
Prenatal viral exposure during second trimester (Helsinki Influenza 1957)
MICRO-GLIA + IMMUNE CELLS
function to remove damaged cells + promote cell death
increase activation in regions important for executive functions
regulated by dopamine and GABA
There may be excessive neuronal pruning in key areas at critical adolescent periods, stressed during adolescence
Explain how neurodevelopmental factors lead to schizophrenia in men and women
What is the Multiple Hit Model of schizophrenia?
There may be a MULTIPLE HIT MODEL of genes, nutrition, virus + toxins, birth injury, and stressors that make up schizophrenia development
brain development from conception to early adulthood (neuron formation, migration, and synaptic pruning)
anatomical and functional disruption in neural connectivity and communication → COGNITIVE DYSMETRIA
difficulties in processing high-level cognitive processes (attention, memory, language, emotion)
All contributing to HALLUCINATIONS, DELUSIONS, DISORGANIZED SPEECH + GROSSLY DISORGANIZED BEHAVIOUR
What are the 3 theories of recurrence for schizophrenia?
Stressful life events
Family processes
Brown (1959) found higher risk of relapse for those living in a high-criticism family dynamic
Expressed Emotion
Hooley (1985) found that emotional climate of a family is a significant indicator for relapse
but not across cultures!!!!!!!!!!!!!!!!!!!
What was the first generation of antipsychotics for biological schizophrenia treatment?
FIRST GENERATION OF ANTIPSYCHOTIC MEDICATION focused on positive symptoms with multiple side-effects
AKINESIA - impaired movement
TARDIVE DYSKINESIA
It was more so about managment, not cure with a 30-50% non respondance rate
What was the second generation of antipsychotics for biological schizophrenia treatment?
SECOND GENERATION OF ANTIPSYCHOTIC MEDICATION reduced negative symptoms more than first generation
fewer bad side effects, though still possible - diabetes, weight gain, immune dysfunction (1%), and seizures
fewer suicides and reduced relapse rates
CLOZAPINE, OLANZAPINE, RESPERIDONE
What are the current medications for those with schizophrenia?
CHOLINERGIC SYSTEM AGONISTS
increasing acetylcholine (memory, attention, arousal), aiding neural transmission
little research
What are the 3 psycho-social treatments for schizophrenia?
Token economy programs (rewarding tokens for desired behaviours)
Skill training
Behavioural family treatment to reduce expressed emotion
PSYCHOLOGICAL TREATMENTS can reduce relapse rates but not always - drugs with support or education is the best, skill training + family treatment are about equal (slightly over half as productive as drugs + education/support)
What is included in the cognitive therapy for schizophrenia?
COGNITIVE THERAPY acts to reframe positive symptoms
identify possible triggers
identify anxiety-provoking beliefs (delusions)
gently provide alternative explanations
.5 to 1% of those with SD have a reduction in symptoms
Relationship with patient is critical and treatment effect sizes as well
What is the current conclusion about schizophrenia treatment?
There is no cure, rather symptom management with first-line treatment as medication despite multiple side-effects
heterogeneity between patients makes research very difficult
What are civil commitment laws? What do they balance? What do they require?
Each province and territory has respective civil commitment laws: legal proceedings that determine if a person who has not broken the law, but has a mental disorder, may be hospitalized, even involuntarily
CIVIL COMMITMENT LAWS balance individual rights + fairness with the protection of society from the government… parens patriae and police power
Most provinces allow commitment if:
individuals have a mental disorder
the individual is a threat to themselves or others (mandatory)
they are in need of treatment
CIVIL COMMITMENT REQUIRES:
2 medical opinions, except in emergencies (1 doctor in 48 hours and 2 doctors in 1 month)
How do British Columbia and Ontario differ in civil commitment?
BRITISH COLUMBIA: having a mental illness (disease of mind), need for psychiatric treatment
care, supervision, or control are necessary to protect the person and others
or to prevent substantial mental or physical deterioration
B.C. uses a broad definition that require more judgement from the court and mental health professionals (better for patients’ interest)
ONTARIO: requiring that an individual’s mental illness will result in serious bodily harm or imminent and serious physical impairment
Ontario uses a stricter definition, prognosis will be worse for lost treatment time + legal issues are worse because of criminal offences
What are parens patriae and police power?
PARENS PATRIAE and POLICE POWER are two dictators of civil comitment
PARENS PATRIAE (state as parent) is used when citizens are unable to act in their best interest
government can exert parens patriae to protect people from hurting themselves
POLICE POWER is used when there is a need to protect the public
government can create laws and regulations to protect the public
What are specific processes to CIVIL COMMITMENT in B.C.?
In B.C.:
patients must be given oral or written notice of their individual rights
a family member must be notified
commitment can be appealed (3 person review board + patient has the right to a lawyer)
What are challenges of defining mental illness in law?
MENTAL ILLNESS as a legal concept, implies the cause of the disorder to be found in a medical disease model
In Canada: disease of the mind
terms like “insanity, mental illness, and mental disorder” are legal terms not psychiatric terms
Saskatchewan uses a PRACTICAL DEFINITION: disordered thoughts, perceptions, and thoughts vs. simply a disease
What are the distinctions between CIVIL COMMITMENT, CRIMINAL COMMITMENT, and the CHARTER OF RIGHTS?
CHARTER OF RIGHTS AND FREEDOMS: provisions that allow for people to be removed from society if they act in a way infringing on the rights of others
based on English common law + Napoleonic code in civil statutes
CRIMINAL COMMITMENT (federal): for determination of competency to stand trial or after a verdict of NCRMD
CIVIL COMMITMENT (province-based): procedure where mentally ill people who have not broken the law can be deprived of liberty and incararcerated in a mental hospital
What are the processes of criminal commitment?
CRIMINAL COMMITMENT is used when someone who has broken the law may also have a mental illness
consists of 2 legal decisions: competency to stand trial + if they are Not Criminally Responsible on Account of Mental Disorder (NCRMD)
How does CRIMINAL COMMITMENT determine if someone is competent to stand trial + what are possible outcomes?
Based on TRIAL IN ABSTENTIA - being mentally and physically present for trial
focus is on individual’s state of mind at the time of the trial based on 3 criteria
FITNESS INTERVIEW TEST-R
Does the person understand the nature and purpose of legal proceeding?
Does the person understand the likely/possible consequences of proceedings?
Can the person communicate with their lawyer?
OUTCOMES FOR THOSE NOT FIT
conditional discharge
detained in a hospital
order compulsory treatment
What are community treatment orders in mental health law? What is the rationale behind it?
COMMUNITY TREATMENT ORDERS stipulate that the person may be released into the community as long as they seek and adhere to treatment
RATIONALE: those with mental disorders may be unable to seek treatment, with deficits in insight
CONTROVERSIAL
What is NCRAMD? What are its criteria?
Not Criminally Responsible by Reason of Mental Disorder (NCRMD) is based on the principle of mens rea (criminal intent)
actus rea is involuntary action
Rather, the focus is on a person’s state of mind at the time of the crime based on 3 criteria:
suffers from a mental disorder rendering the person incapable of:
appreciating the nature of one’s behaviour
appreciating one’s behaviour is wrong
“Mental illness” here is under judicial terms defined differently in legal terms and non congruent with a DSM diagnosis
expert opioin is weighed as well as judge’s opinion
What are the controversies and realities of NCMDAR defence?
NCRMD states that a person can have a mental illness and still be criminally responsible for a crime
the disorder must be seen to directly impact the criminal action
LAY PUBLIC thinks that NCDMD is a way for guilty people to get off, but it is not used commonly
fewer than 1 in 100 defendants in felony cases file insanity pleas
and within this only 29% result in acquittal
those found NCRMD spend more time in a psychiatric institution than they would have spent in prison
In Canada most with NCRMD suffered from psychotic disorders such as that of schizophrenia
What are 3 things to remember about violence and mental illness?
Danger prediction is central to CIVIL COMMITMENT LAW
Among those incarcerated, inmates with serious mental disorders (schizophrenia) are less likely to reoffend a new violent crime following release, than inmates without mental illness.
3% of violent acts are mental illness related and a critical factor is COMORBID SUBSTANCE ABUSE
Mental health professionals are bad at judging danger, clinical interviews and specialized training have helped