Therapeutics I: CARDIO V Combined
1/224
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
225 Terms
Non-pharmacological options for arrhythmias? (four)
1. Pacemakers
2. Cardioversion
3. Catheter ablation
4. Surgery
What is an ICD?
Implantable cardioverter-defibrillator (ICD); can detect and treat potentially fatal arrythmias
Advantages of ICD? (three)
1. Widely used for reducing mortality in coronary artery disease
2. In heart failure with low ejection fraction
3. Advances in technology, dangers of long-term therapy with available drugs
Cardiac arrythmias with defined autonomic pathways? (four)
1. Arterioventricular reentry using accessory pathway
2. Arterioventricular node reentry
3. Atrial flutter
4. Ventricular tachycardia
Role of the SA node
Pacemaker/ where electrical impulse for heart arises from
Role of the AV node
Slow down impulses so that the atria can contract to fill the adjacent ventricles with blood
Pathway of electrical impulse through the heart
SA node -> AV node -> Bundle of His -> Purkinje fibers
Role of Bundle of His
Transmits cardiac impulse from AV node to the ventricular muscle
Role of Purkinje fibers
Help ventricles contract
What are the ions that establish the transmembrane potential of cardiac cells?
Na+
K+
Ca2+
Cl-
Which ions that establish the transmembrane potential of cardiac cells cannot freely diffuse across the lipid bilayer? (three)
Na+
Ca2+
Cl-
T/F: The transportation of ions across the membrane requires ion channels for diffusion.
True
Ohm's law equation
V = I*R
Three voltage gated channels?
Sodium channel
Potassium channel
Calcium channel
Resting membrane potential of the cardiomyocyte
-70 mV
At what threshold potential does a cardiomyocyte become depolarized?
-40 mV
What happens when a cardiomyocyte becomes depolarized?
Sodium channels open, Na+ ions permeate, depolarizing the membrane potential further to +40 mV
At what membrane potential do calcium channels activate?
+40 mV
When calcium channels are activated, what is simultaneously occurring? What phase is this?
Phase 1; while calcium channels are activated, sodium channels begin inactivating
Describe Phase 0
Depolarization stage: rapid depolarization occurs when sodium (Na+) channels open, allowing Na+ to enter the cell, leading to a sharp increase in membrane potential (to about +40 mV).
Describe Phase 1
Initial repolarization stage: sodium channels begin to inactivate, and some potassium channels open, causing a brief decrease in membrane potential.
Describe Phase 2
Plateau phase: Calcium channels open, allowing calcium ions to enter the cells. This balances the outward movement of potassium, resulting in a plateau of action potential.
Describe Phase 3
Repolarization phase: Potassium channels remain open, but the influx of calcium decreases. The membrane potential starts to repolarize as potassium ions exit the cell, moving back towards the resting potential.
Describe Phase 4
Resting membrane potential: The cell returns to its resting membrane potential of about -70 mV, ready for the next action potential.
What are the four main types of arrythmia?
1. Premature (extra) beats
2. Supraventricular
3. Ventricular arrythmias
4. Bradyarrythmias
Torsades is otherwise known as what?
Polymorphic ventricular tachycardia
Typical symptoms of long QT syndrome?
Dizziness
Transient loss of consciousness
What are the two forms of abnormal activity classified as a triggered automaticity
Early afterdepolarizations (EADs)
Delayed afterdepolarizations (DADs)
T/F: A triggered automaticity requires an abnormal action potential for its initiation.
False; requires a normal action potential
Factors that can precipitate or exacerbate arrythmias? (ten)
1. Ischemia
2. Hypoxia
3. Acidosis or alkalosis
4. Electrolyte imbalance
5. Excessive catecholamine exposure
6. Autonomic influences
7. Drug toxicity (digitalis)
8. Stretching
9. Scar, diseased tissue
10. Impulse formation or impulse conduction, or both
Procainamide belongs to what class of antiarrhythmics?
Class 1A
Procainamide MOA
Blocks sodium channels in myocardial cells, reducing autorhythmicity and slowing conduction.
Lidocaine belongs to what class of antiarrhythmics?
Class 1B
MOA of lidocaine
Blocks sodium channels, suppresses automaticity in the HIS Purkinje system and depolarization in the ventricles
Flecainide belongs to what class of antiarrythmics?
Class 1C
Flecainide MOA
Slows conduction in cardiac tissue by altering transport of ions across cell membranes; causes slight prolongation of refractory periods; decreases the rate of rise of the action potential without affecting its duration
Propranolol belongs to what class of antiarrhythmics?
Class II
MOA of propranolol
Beta antagonist, inhibits heart rate and hearts strength of contraction
Non-selective beta blocker
Propranolol is clinically applied where?
In atrial arrythmias, and prevention of recurrent infarction and sudden death
Flecainide is clinically applied where?
In supraventricular arrythmias in patients with normal heart
Contraindicated in ischemic conditions (post MI)
Amiodarone belongs to what class of antiarrhythmics?
Class 3
MOA of amiodarone?
Delay repolarization and increase the duration of the action potential
Dofetilide belongs to what class of antiarrhythmics?
Class 3
MOA of dofetilide?
Prolongs action potential, effective refractory period
Amiodarone is clinically applied where?
Serious ventricular arrhythmias and supraventricular arrhythmias
Dofetilide is clinically applied where?
Maintenance or restoration of sinus rhythm in Afib
Verapamil belongs to what class of antiarrhythmics?
Class 4
MOA of verapamil?
Calcium channel blocker
Slows SA node automaticity and AV node conduction velocity; decreases cardiac contractility, reduces blood pressure
Class 1 antiarrhythmics can be broadly described as what?
Sodium channel blockers
Describe Class 1A antiarrhythmics
Prolong the APD and dissociate from the channel with intermediate kinetics
Describe class 1B antiarrhythmics
Shorten the APD in some tissues of the heart and dissociate from the channel with rapid kinetics
Describe class 1C antiarrhythmics
Minimal effects on the APD and dissociate from the channel with slow kinetics
Describe class 2 antiarrhythmics
Action is sympatholytic; drugs with this action reduce -adrenergic activity in the heart
Describe class 3 antiarrhythmics
Action manifests as prolongation of the APD; most drugs with this action block the rapid component of the delayed rectifier potassium current, IKr.
Describe class 4 antiarrhythmics
Calcium channel blockers
This action slows conduction in regions where the action potential upstroke is calcium dependent, i.e. the SA and AV nodes
T/F: Drugs with local anesthetic action block sodium channels and reduce the sodium current.
True
T/F: Procainamide slows the upstroke of the action potential, slows conduction, prolongs the QRS duration of the ECG, and prolongs the APD.
True yea but read that a couple times
Quinidine belongs to what class of antiarrhythmics?
Class 1A
MOA of quinidine?
Blocks sodium channels
Slows impulse conduction
Delays repolarization
Blocks vagal input to the heart
Disopyramide belongs to what class of antiarrhythmics?
Class 1A
MOA of disopyramide
Sodium channel blocker; inhibits the fast sodium channels during depolarization phase. Prolongs APD, slows rate of depolarization.
Adverse effects associated with quinidine?
Cardiotoxic effects
Excessive QT-interval prolongation and induction of torsades de pointes.
Which of the following has cardiac antimuscarinic effects?
A. Quinidine
B. Propranolol
C. Verapamil
D. Disopyramide
D. Disopyramide
Mexiletine belongs to what class of antiarrhythmics?
Class 1B
T/F: The electrophysiologic and antiarrhythmic actions of mexiletine are similar to those of lidocaine.
True
Mexiletine is applied clinically where?
Ventricular arrhythmias
T/F: Amiodarone has strong adrenergic and calcium-channel blocking actions.
False; amiodarone has weak adrenergic and calcium-channel blocking actions.
Does flecainide prolong the action potential and/or the QT interval?
A. Yes
B. No
B. No
Despite blocking certain potassium channels, it does not prolong the action potential or the QT interval.
Sotalol belongs to what class of antiarrhythmics?
Class 2 and Class 3
T/F: Verapamil selectively blocks activated L-type calcium channels.
False; Verapamil blocks both activated and inactivated L-type calcium channels.
T/F: Verapamil can suppress both early and delayed afterdepolarizations.
True
Dronedarone ___________ sinus rate and prolongs AV nodal conduction and refractoriness.
A. reduces
B. increases
A. Reduces
Describe a supraventricular arrhythmia
Originates from ABOVE the bundle of His
Types of supraventricular arrhythmias? (four)
1. Afib
2. Aflutter
3. Paroxysmal supraventricular tachycardia
4. Autonomic atrial tachycardia
Describe a ventricular arrhythmia
Originates from BELOW the bundle of His
Types of ventricular arrhythmias? (three)
1. Premature ventricular complexes
2. Ventricular tachycardia
3. Ventricular fibrillation
Define atrial fibrillation
A supraventricular arrhythmia with uncoordinated atrial activation and consequently ineffective atrial contraction
Afib is defined by what kind of heartrate? Bpm?
Chaotic, rapid (300-500 bpm); irregular atrial rhythm
Conditions which predispose a person to Afib?
Advanced age
Smoking
Physical activity
Alcohol
Obesity
Height
Blood pressure (HTN)
Resting heart rate
Diabetes
Cardiovascular conditions which predispose a person to Afib?
HF
CAD
VHD
Cardiac surgery
Acute cases which can precipitate Afib?
Thyrotoxicosis
Surgery
Alcohol withdrawal
Sepsis
Excessive physical exertion
T/F: Afib is a progressive disease.
True
Describe AF Stage 2
Evidence of structural or electrical findings further predisposing a patient to AF
(atrial enlargement, frequent atrial ectopy)
Describe AF Stage 3
Has diagnosed AF
Paroxysmal, persistent, long-standing persistent, or successful AF ablation
Describe AF Stage 4
Permanent AF
Testing used to diagnose AF?
12-lead ECG (gold standard)
Holter/event monitor (paroxysmal)
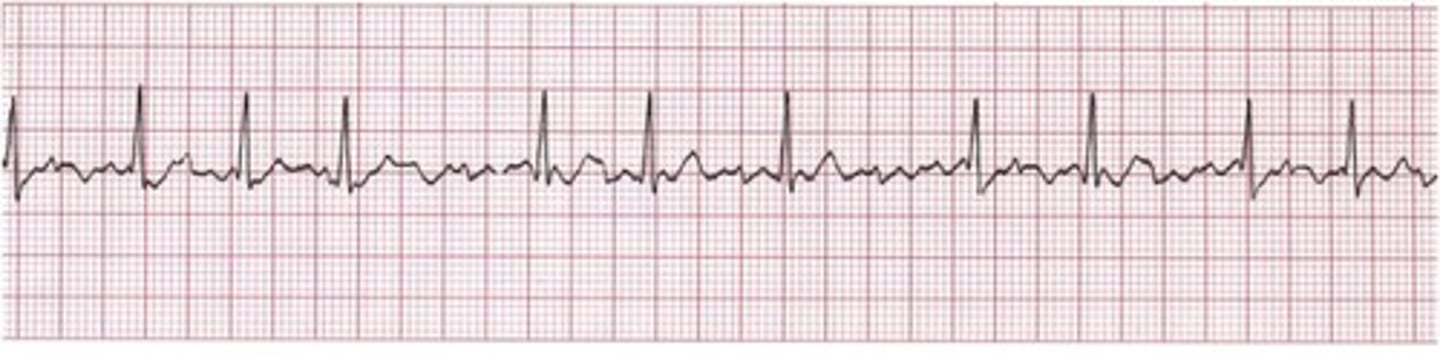
Afib graph looks like what?
Extra spiky
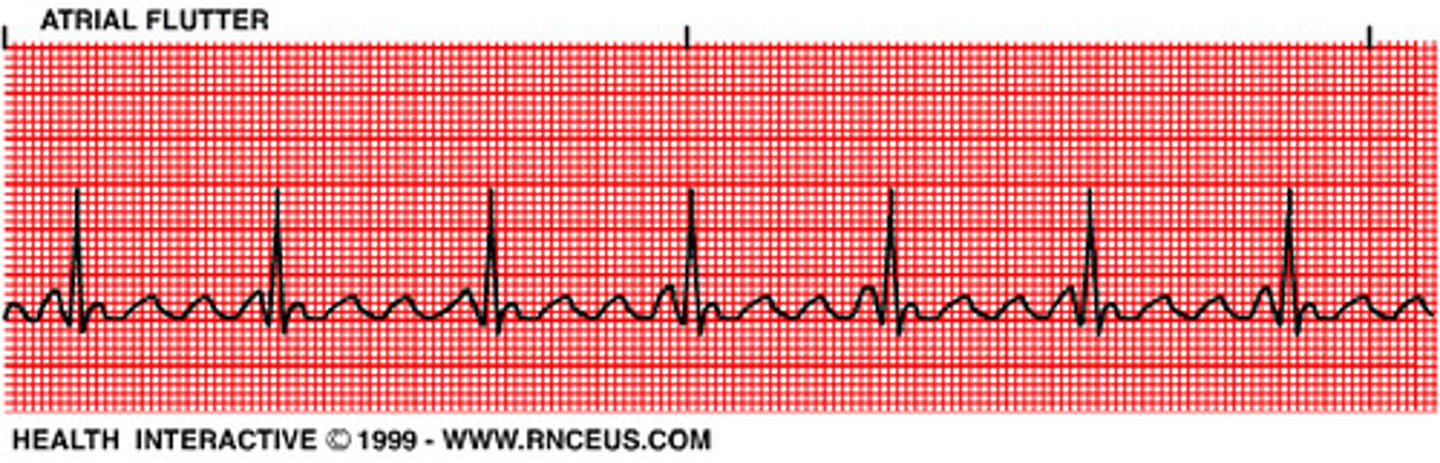
Aflutter graph looks like what?
More squiggly in the middle
What are the FDA-cleared Direct to Consumer monitor types? (four)
Apple Watch
Fitbit sense
Samsung Galaxy Watch 3
Withings ScanWatch
Clinical characteristics of AF?
Palpitations, exertional fatigue, lightheadedness, exercise intolerance, dyspnea
Syncope is possible but uncommon
What are the 4As of AF management?
Access to All Aspects of Care for All
What does SOS stand for in AF management?
Stroke risk
Optimize (modifiable risk factors)
Symptom management
What does HEAD 2 TOES stand for in AF management?
Heart failure, exercise, arterial hypertension, diabetes, tobacco, obesity, ethanol, sleep
These are the most common/pertinent risk factors for AF
Primary prevention recommendations (LRFM) for management of AF?
Patients at increased risk of AF should receive comprehensive guideline-directed LRFM for AF, targeting obesity, physical inactivity, unhealthy alcohol consumption, smoking, diabetes, and hypertension.
What is the recommended percentage weight loss for secondary prevention in AF management?
Target of 10%
What is the recommended weekly physical fitness guideline for secondary prevention in AF management?
210 minutes/wk
Which risk score assessment do we prefer for assessing AF risk?
CHADS-VASc
T/F: For stroke management in Afib, we prefer DOACs over warfarin.
True
DOACs include? (four)
Apixaban
Dabigatran
Edoxaban
Rivaroxaban
T/F: ASA alone or with clopidogrel is an acceptable alternative to DOAC or warfarin in stroke management of AF.
False; only in the presence of another indication