oral mucosa
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
what is the stomodeum lined by
ectoderm
what type of epithelium is the oral cavity
stratified squamous epithelium (so it the epidermis- skin)
the oral mucosa and submucosa types are all dependent on:
location: whether it be inside the area of mastication or outside the area of mastication
what are characteristics (4) of oral mucosa/submucosa that are INSIDE the area of mastication
masticatory mucosa
keratinized epithelium
highly fibrous reticular layer
bone
what are characteristics (4) of oral mucosa/submucosa that are OUTSIDE the area of mastication
lining mucosa
non-keratinized epithelium
normal reticular layer
muscle
in what ways are features of masticatory mucosa and lining mucosa similar to our skin
have keratinized epithelium
normal reticular layer
attach to muscle
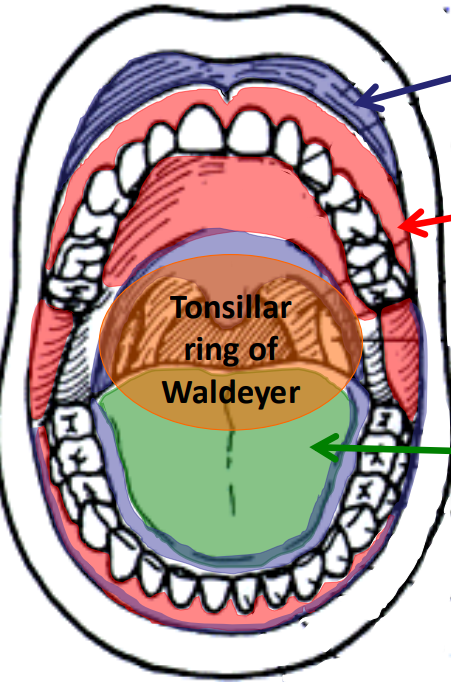
what type of mucosa is represented by the BLUE highlighted areas/arrow and how much surface area does it take up
lining mucosa- 60%
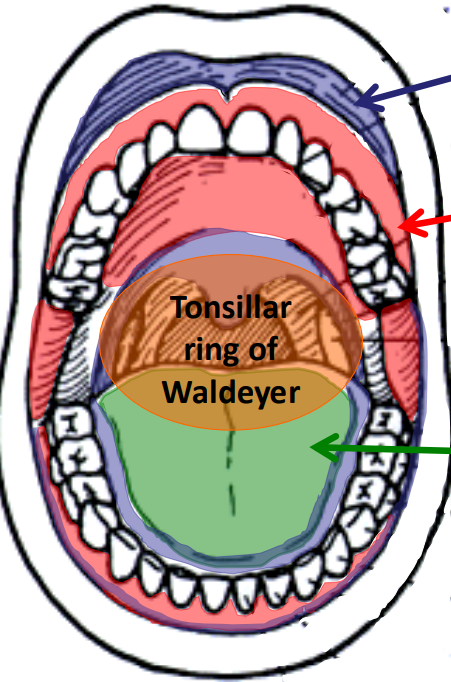
what type of mucosa is represented by the RED highlighted areas/arrow and how much surface area does is take up
masticatory mucosa- 25%
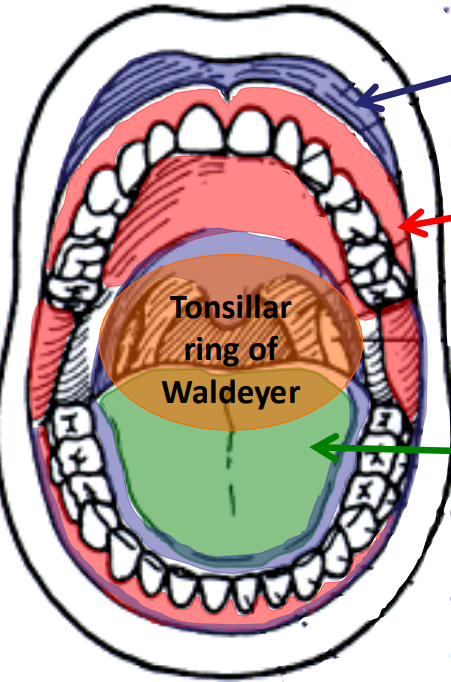
what type of mucosa is represented by the green highlighted area/arrow and how much surface area does it take up
specialized mucosa- 15%
what are the functions of the oral mucosa
mechanically protective against compressive and shearing forces
provides innate immune barrier to microorganisms, toxins, antigens
immunological defense both innate and adaptive
the oral mucosa is richly innervated providing what type of sensory outputs
modalities of:
touch
proprioception
pain
temperature
taste
salivary glands within the mucosa secrete saliva, what are some components that make up the saliva
lubricating and buffering
antibodies- sIg’s
germicides
the mucous film from saliva has what role in the oral cavity
acts as a barrier helping to retain water and electrolytes, keeping the oral cavity moist
what structure in the oral cavity is the first site to encounter inhaled/ingested microorganisms and is considered the first line of adaptive immune defense against pathogens
palatine tonsils
what type of tissue are the palatine tonsils
lymphatic tissue → mucous associated lymphoid tissue (MALT)
what are germinal centers and where are they found
in palatine tonsils: represent activated (antigen presented) B-cells becoming antibody producing plasma cells
nodules are filled w…
B cells
what are the 3 general layers of lining/masticatory mucosa from superficial to deep
epithelium- stratified squamous
lamina propria
submucosa → NOT in masticatory
epithelium of masticatory mucosa has what origin
ectodermal origin
generally, what can be found in the epithelial layers masticatory/lining mucosa
keratinocytes- 90% of cells
exocrine glands ducts
non-keratinocytes- 10% of cells
what cells are non-keratinocytes that are found in the epithelium (4)
melanocytes
langerhans cells
merkel cells
nerve endings
origin of melanocytes
neural crest
origin of langerhans cells
monocytes
origin of merkel cells
ectodermal
origin of nerve endings
neural crest
origin of lamina propria
ectomesenchyme
generally, how do the lamina propria layers between lining mucosa and masticatory mucosa differ
in lining: lamina propria and submucosal layer have no keratinized tissue, JUST LIKE OUR SKIN
masticatory: has keratinized tissue, lots of dense fibers
what is included in the submucosal layer of lining mucosa
exocrine glands
adipocytes, connective tissue
origin of exocrine glands in submucosal layer of lining mucosa
ectodermal
origin of adipocytes, connective tissue in submucosal layer of lining mucosa
ectomesenchyme
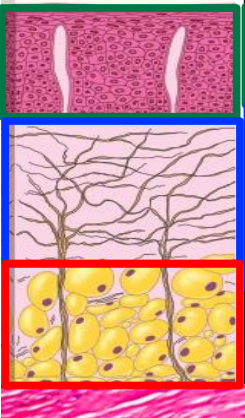
lining or masticatory mucosa
lining mucosa
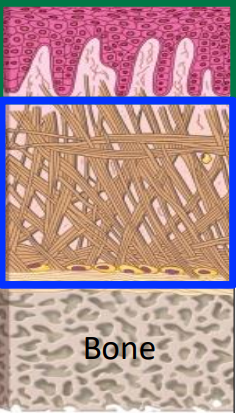
lining or masticatory mucosa
masticatory mucosa
lining mucosa is _________ (soft/firm) and ___________ (pliable/immobile)
soft and pliable
masticatory mucosa is _________ (soft/firm) and ___________ (pliable/immobile)
firm and immobile
bc lining mucosa is soft and pliable, what properties does this lead to when it comes to injections/injury
fluids easily injected
lining gapes when cut→ won’t tear or fall apart
inflammation is dispersed→ won’t rlly hurt
bc masticatory mucosa is firm and immobile, what properties does this lead to when it comes to injections/injury
injections are painful
lining tears when cut→ bc not enough space to expand
inflammation is painful
prior to tooth eruption, the epithelium is either _______________ or ______________
para-keratinized or non-keratinized
para-keratinized epithelium differs from keratinized epithelium in what (3) ways:
basophilia of the outermost layers bc of nuclei present
absence of a distinctive stratum granulosum
absence of stratum corneum

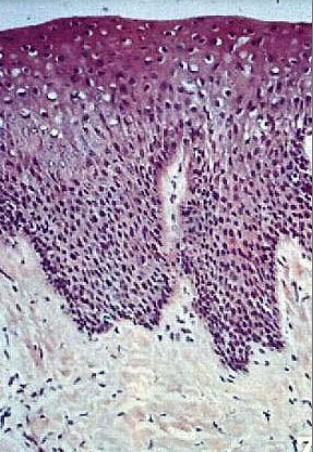
what type of epithelium is this
parakeratinized epithelium
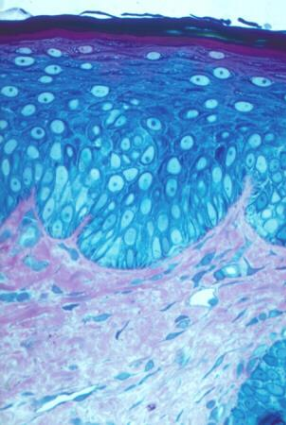
what type of epithelium is this
lining mucosa- nonkeratinized epithelium
when does keratinized stratified squamous epithelium develop
during primary tooth eruption
what type of epithelium is this
masticatory mucosa- keratinized epithelium
what is the main funx of the basal layer
to undergo mitosis for either self renewal or to replace differentiated cells above the basal layer
are keratinocytes or non-keratinocytes derived from the basal cell layer
keratinocytes → generalized term for all cells derived from basal cell layer
non-keratinocytes → non derived from basal cell layer
what are the two filament types of the cytoskeleton in epithelial cells
microfilaments
intermediate filaments
what type of filaments are the microfilaments, what size are they
actin filaments; 7 nm in diameter
what type of attachments do actin filaments have
have adherent junctions and focal adhesions
function of actin filaments
allow movement of cell surface, enabling cells to migrate, engulf particles, and divide
what type of filaments are intermediate filaments and what size are they
keratin filaments; 10 nm in diameter
what do keratin filaments attach to
desmosomes
hemidesmosomes
are actin or keratin filaments larger
keratin filaments
funx of keratin filaments
more structural support; provide mechanical strength to cells and tissues
desmosome funx w keratin filaments
major contributor: help w side-to-side tension
hemi-desmosome funx w keratin filaments
hold onto basal cells and underlying CT
what are the two kinds of keratin fibers you can find in the oral epithelium
keratins:
neutral/basic
acidic
which keratins are neutral/basic
CK1-CK9
which keratins are acidic
CK10-CK20
cytokeratins always occur in pairs…
one neutral and one acidic
what are the cytokeratins in masticatory mucosa
CK1 and CK10
what are the cytokeratins in lining mucosa
CK4 and CK13
what are the cytokeratins in the soft palate
CK 7, 8, 18
what are the cytokeratins that make up the basal layer
CK5 and CK14
loss of keratin ___ is one of the most valuable diagnostic criteria for discriminating carcinoma in situ from non malignancies in the oral mucosa
keratin 13
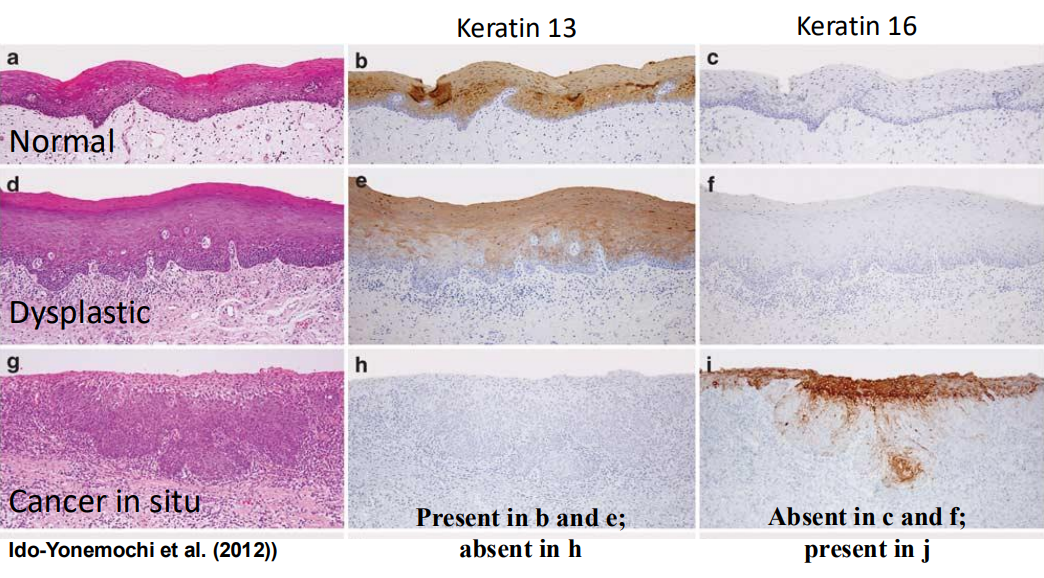
why is keratin 13 used to distinguish malignant lesions
is stable in the prickle cells of normal epithelium, and will be lost in a cause of neoplasms
what are the four layers of keratinized epithelium is masticatory mucosa from superficial to deep
keratinized layer
stratum corneum
granular layer
stratum granulosum
prickle cell layer
stratum spinosum
basal layer
stratum basale
what is going on in the basal layer of keratinized epithelium
desmosomes
keratin filaments form tonofibrils
cell divisions
hemidesmosomes→ hooked to basement membrane
what is going on in the prickle cell layer of keratinized epithelium
keratin fibrils→ from keratin filaments wrapping and building onto each other
desmosomes increasing in attachments to neighbor
formation of membrane-coating granules
what is in the granular layer of keratinized epithelium
keratin fibrils
desmosomes
keratohyalin granules forming
secretion of glycolipids from membrane coating granules
MCG also being pushed to the outside of the cell to make room for the keratohylain granules
what is in the keratinized layer of keratinized epithelium
all cell organelles lost
formation of the “cornified envelope”
glycolipids opening up
keratinohylaine granules opening up
heavy fibril network extending completely into the internal cytosol
what happens in the keratinized layer when glycolipids start to open up
these will coat the cell in a hydrophobic material and will contribute to the toughness of the plasma membrane
what happens in the keratinized layer when the keratohyalin granules are opening up
it’s contents are keratin filament associated proteins/binding proteins, and these will aid in locking the keratin fibrils together
what are the keratin filament associated proteins (KFAP, binding proteins) that are released from keratohyalin granules
filaggrin
loricrin
involucrin
where is filaggrin
synthesized in the granular layer and stored in keratohyalin granules; is the main contributor
funx of filaggrin
binds to and condenses the keratin cytoskeleton and thereby contributes to the cell compaction process that creates the squamous cell shape
where is loricrin
expressed in the superficial layers of keratinized and nonkeratinized oral epithelia
funx of loricrin
binds to the ends of keratin and contributes toward cornification
funx of involucrin
binds to loricrin and helps to create the cornified envelope
what areas can show variation of keratinized and parakeratinized
parts of hard palate and much of the gingiva
what causes parakeratinization
due to incomplete removal of organelles from the granular layer
what are the 4 layers of non-keratinized epithelium from superficial to deep
surface layer
stratum superficiale
intermediate layer
stratum inermedium
prickle cell layer
stratum spinosum
basal layer
stratum basale
how does the basal layer of nonkeratinized epithelium compare to keratinized epithelium
no difference:
desmosomes- maybe fewer
keratin filaments
cells division
what is the difference between the prickle cell layer of keratinized vs nonkeratinized epithelium
no desmosomes, both will have:
keratin filaments
membrane-coating granules
what is in the intermediate layer of nonkeratinized epithelium
glycogen vesicles
what is in the surface layers of nonkeratinized epithelium
incomplete removal of organelles → cells are still alive!
what is the purpose of having glycogen vesicles in the intermediate layer of non-keratinized tissue
nutrients will be diffusing from basal layer, but this mode is insufficient for cells that are still alive in the surface layer compared to keratinized tissue, where you usually do not worry ab bc they are dead. glycogen vesicles supply nutrients for live cells that are in the surface layer
what are melanocytes
contain the pigment melanin
what layer can melanocytes typically be found
in basal layer
what is melanin packaged into
melanosomes
how is melanin formed
through the oxidation of tyrosine—DOPA—melanin
cytoplasmic extensions establish contacts with over ____ keratinocytes
30
melanosomes are ‘injected’ into oral keratinocytes, what is the funx of this
to form a protective shield against UV-radiation
what are Langerhan cells
antibody to’ lamgerin’ L cell protein; antigen presenting, dendritic cell that will present antigens to T cells, also play a role as macrophages
langerhan cells are derived from…
bone marrow- monocytes
what layer are langerhan’s cells present, why
in stratum spinosum → will scan the epithelium for antigens
characteristics of langerhan cells
motile → have no desmosome attachments to keratinocytes to be able to migrate to regional lymph vessels
what layer can merkel’s cell be found
has desmosomal attachments to basal layers of epithelial cells
precursor to Merkel’s cell
are differentiated basal cells
what do cytoplasms of Merkel’s cell contain
keratin filaments → CK20
small granules containing neuropeptides → SP, ViP
characteristics of Merkel’s cells
slowly adapting mechanoreceptor- touch
abundent in hard and soft palate, mandibular gingiva
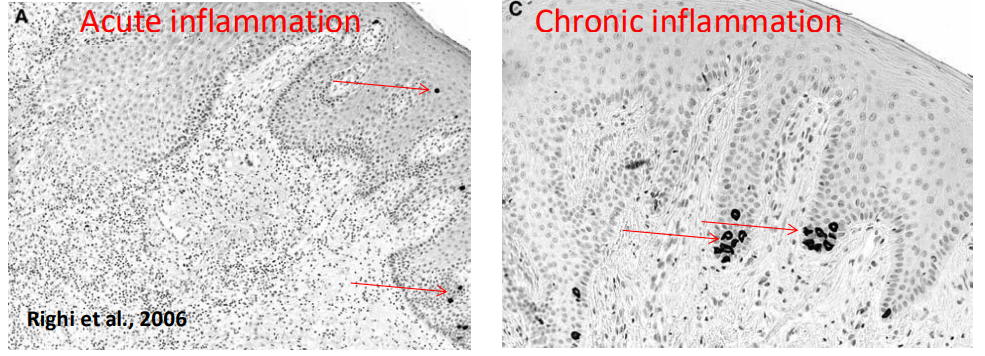
how do Merkel’s cell respond to inflammation
will inc in acute inflammation
will jump substantially in number in chronic inflammation