Metabolic Diseases: Diabetes & Obesity
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
Diabetes Mellitus: definition, what put at risk for, and prevalence in the US
-Group of metabolic diseases characterized by an elevated blood glucose concentration (i.e., hyperglycemia) as a result of defects in insulin secretion and/or an inability to use insulin
-Sustained elevated blood glucose levels place individuals at risk for microvascular and macrovascular (CV) diseases and neuropathies.
-~10% of the U.S. population
o~24% undiagnosed
types of diabetes + which most prevalent?
-Four types of diabetes:
oType 1 (T1DM)
oType 2 (T2DM)
oGestational: pregnant mother developes glucose insensitivity, higher risk develop type II
oOther specific origins: cystic fibrosis
-Most prevalent: Type 1 and Type 2
oType 2: 90%–95% of all cases
oType 1: 5%–10% of all cases
Type I DM
-most often caused by the autoimmune destruction of the insulin-producing β cells of the pancreas
oNearly absolute insulin deficiency
oHigh tendency for ketoacidosis
*”insulin dependent diabetes”
Prediabetes
-characterized by (a) elevated blood glucose in response to dietary carbohydrate (impaired glucose tolerance), and/or (b) elevated blood glucose in the fasting state (impaired fasting glucose)
oVery high risk to develop diabetes because the capacity of the β cells to hypersecrete insulin diminishes over time and becomes insufficient to restrain elevations in blood glucose
*100-125 fasting BG; reversible w/ lifestyle changes
Type 2 DM
-caused by insulin-resistant skeletal muscle, combined with an insulin secretory defect
oCommon feature: excess body fat (abdominal or central obesity)
DM: fundamental goal
-Fundamental goal for the management of DM: glycemic control using diet, exercise, and medications (insulin or oral hypoglycemic agents)
-Intensive treatment to control blood glucose reduces the risk of progression of diabetic complications.
-Glycosylated hemoglobin (HbA1): reflects mean blood glucose control over the past 2–3 months
oGeneral individual goal: <6.5%
-Focus on management of other comorbidities and CVD risk factors
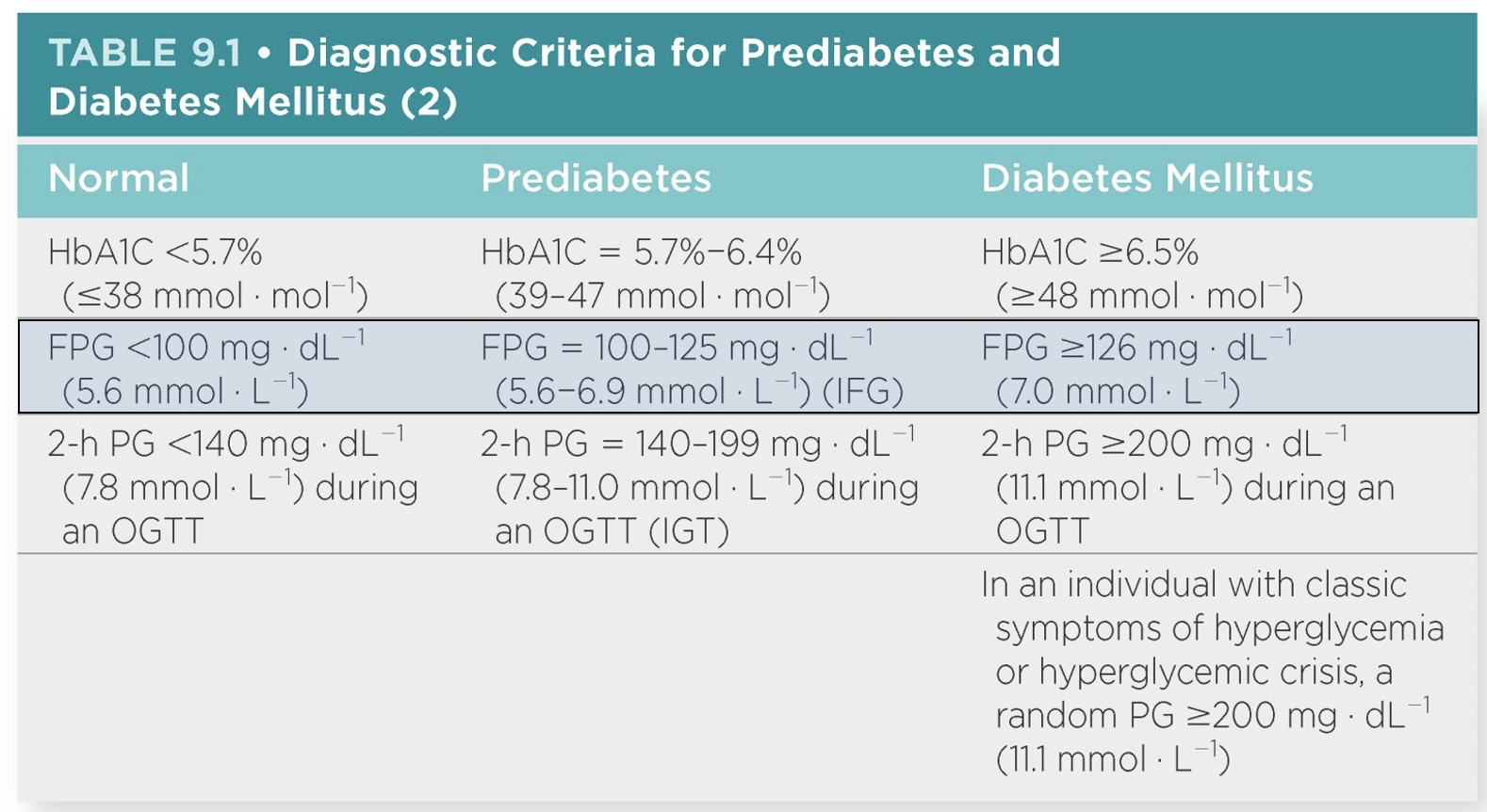
Blood glucose Diagnostic Criteria for Prediabetes and DM
*”HbAIC”=long term control; “2hr PG”=drink sugary substance and wait 2 hours to see how body responds
-Normal: <100
-Pre: 100-125
*do lifestyle modifications to reverse (ex: weight loss, diet)
-DM: >126
DM: Benefits of regular exercise
*one of the most effective treatments…
-Assists in preventing diabetes-related health complications, insulin resistance, and Type 2 diabetes
-Improved glucose tolerance, increased insulin sensitivity, and decreased HbA1C
-For individuals with T1DM, T2DM, or prediabetes: improvements in CVD risk factors and well-being
-May prevent or delay the transition from prediabetes to T2DM
-Moderate intensity exercise totaling 150 min ∙ wk−1 is associated with reduced morbidity and mortality in observational studies including those with DM.
*but if obese may need ~double this
v-nterruption of sedentary time is beneficial for glycemic control.
DM: Exercise testing
-DM has high association with CAD (*so can refer for full CV testing)
-ECG stress testing may be indicated for individuals with DM, who have been sedentary and/or desire vigorous intensity activities.
-Silent ischemia in individuals with DM often goes undetected.
*no chest pain, shortness of breath, etc. (don’t feel symptoms)
oAnnual CVD risk factor assessments should be conducted.
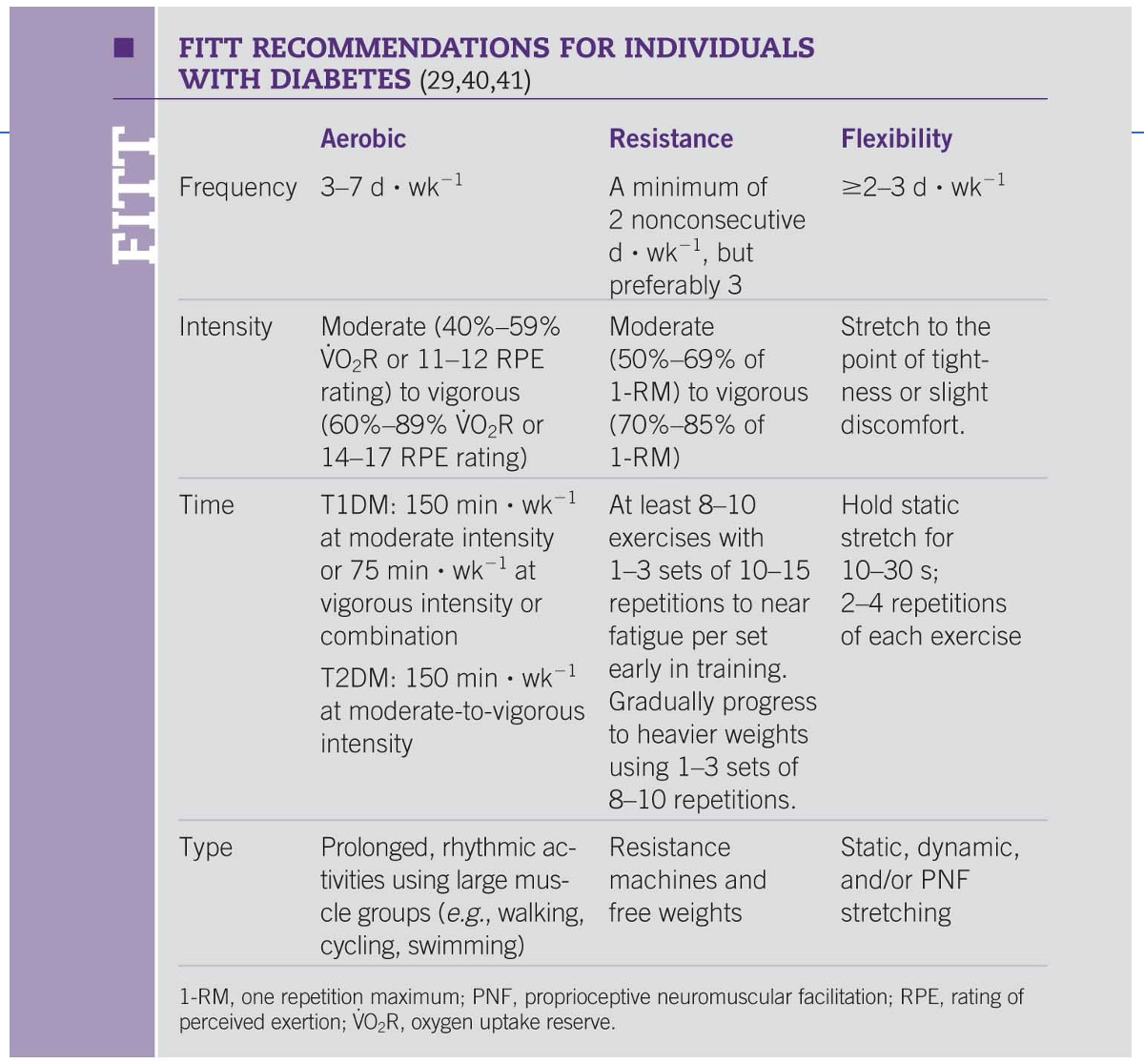
DM: Exercise Rx
-DM without complications: standard FITT principle for healthy adults
*but recognize BG pre and during exercise
-DM and other complications or comorbidities: modified as appropriate
-Common issues: healthy weight loss and maintenance of appropriate body weight
-Similar benefits for resistance and aerobic exercise on cardiovascular risk factors and safety
*RT increases muscle=better glucose intake, not for wl
*Aerobic: more effective for CV factors
-Maximizing the cardiovascular benefits resulting from exercise is a key outcome for diabetics; therefore, an exercise frequency of greater than 3 d · wk−1 is suggested.
DM: FITT
Aerobic
-3-7 days/week
-moderate
-time depends: 150 or >150 if weight is an issue
-type: do what enjoy, but think about glucose control
RT
-standard
Flexibility
-may or may not be important
DM: aerobic Exercise training considerations
-Co-morbid conditions: CVD, overweight, and obesity
*often come w/ sedentary lifestyle, so start lower and build up
-Due to low initial fitness levels, most individuals with T2DM require at least 150 min ∙ wk−1 of moderate to vigorous aerobic exercise to gain optimal CVD risk reduction.
-High intensity intervals during moderate intensity aerobic exercise may be useful to lessen the decline in blood glucose during the early postexercise recovery period.
*bc take insulin and exercise, thus timing (ex: same time everyday, snacks, time take insulin) and type important
-Over time a greater emphasis on vigorous intensity aerobic exercise can ensue if not contraindicated by complications.
oHIIT and continuous training are recommended for better overall blood glucose control. (*higher HR but also breaks)
oFor T2DM, allow no more than two consecutive days without aerobic exercise to prevent a period of excessive decline of insulin action.
DM: RT Exercise training considerations
-Resistance training should be encouraged for individuals with DM or prediabetes.
oUse appropriate progression due to increased risk of tendinopathy & limited joint mobility
-During combined training, completing resistance training prior to aerobic training may lower the risk of hypoglycemia in individuals with T1DM.
oSimilar effect for HIT training (combining anaerobic and aerobic exercise)
-Individuals with DM and retinopathy are at risk for vitreous hemorrhage.
*blood vessels in eyes rupture → blindness
oAvoid activities that dramatically elevate BP. (*avoid RT or high BP)
oAnyone with severe diabetic retinopathy should avoid vigorous intensity aerobic and resistance exercise, jumping, jarring, and head-down activities, and the Valsalva maneuver.
*benefits, but nor for hypoglycemia
DM: autonomic neuropathy
-During exercise, autonomic neuropathy may cause chronotropic incompetence, attenuated VO2 kinetics, and anhidrosis (poor sweating mechanism).
*disregulation of CV system (HR, BP); not normal HR response; breathes faster; bad heat control
-In the presence of autonomic neuropathy, the following should be considered:
oMonitor for signs and symptoms of silent ischemia (unusual shortness of breath or high back pain) because of the inability to perceive angina.
*no classic chest pain no more of a significant sign
oMonitor BP before and after exercise to manage hypotension (*no good Q) and hypertension associated with vigorous intensity exercise.
oHR and BP responses to exercise may be blunted secondary to autonomic dysfunction. RPE should be used to assess exercise intensity.
*overall: hard to work with; worry about CVD, stroke; so Rx concerning and necessary
DM: Peripheral neuropathy
-For individuals with peripheral neuropathy, special precautions should be taken to prevent blisters on the feet. (*can’t feel pain)
oFeet should be kept dry and the use of silica gel or air midsoles as well as polyester or blend socks should be used.
oAll individuals should closely examine their feet daily to detect and treat sores or ulcers early. (*ex: infected wound so need amputation)
-For individuals with nephropathy, exercise does not appear to accelerate progression of kidney disease even though protein excretion acutely increases after exercise.
*exercise not good or bad
DM: BG special considerations
-Blood glucose monitoring is recommended when beginning a new exercise program or when there is a history of unstable blood glucose during exercise.
*technology better today, but need to remember to turn down during exercise and return after
-Most insulin users will need to consume carbohydrates (up to 15 g) prior to exercise participation when starting blood glucose levels are ≤100 mg ∙ dL−1.
oPrior to planned exercise, rapid- or short-acting insulin doses may have to be reduced to prevent hypoglycemia.
oMonitor blood glucose levels before, after, and occasionally during exercise.
-Hypoglycemia risk is higher during and immediately following exercise but can occur up to 12 hours or more postexercise.
DM: Hypoglcemia
-Hypoglycemia (blood glucose <70 mg ∙ dL−1 ; <3.9 mmol ∙ L−1): relative contraindication to beginning an acute bout of exercise
*don’t exercise until raise BG!
oSymptomatic or asymptomatic (hypoglycemic unawareness)
oCommon symptoms: shakiness, weakness, abnormal sweating, nervousness, anxiety, tingling of the mouth and fingers, and hunger
-Consider changing insulin timing, reducing insulin doses, and/or increasing carbohydrate intake to prevent hypoglycemia and hyperglycemia during and after exercise.
oEarly morning exercise may be best, resulting in elevations in blood glucose levels instead of the usual decrease with moderate activity.
DM: Hyperglycemia
-Hyperglycemia (blood glucose ≥250 mg ∙ dL−1 or 13.9 mmol ∙ L−1) with or without ketosis is a concern for individuals with T1DM
*give medication, lower BG so can exercise
oSymptoms: polyuria, fatigue, weakness, increased thirst, and acetone breath
oStable hyperglycemia: moderate intensity exercise may proceed with frequent monitoring and ensure adequate hydration
-Exercise should be postponed when both hyperglycemia and ketones are evident
oIndividuals with T1DM check for urine ketones when blood glucose levels are ≥250 mg ∙ dL−1 (13.9 mmol ∙ L−1) before starting to exercise.
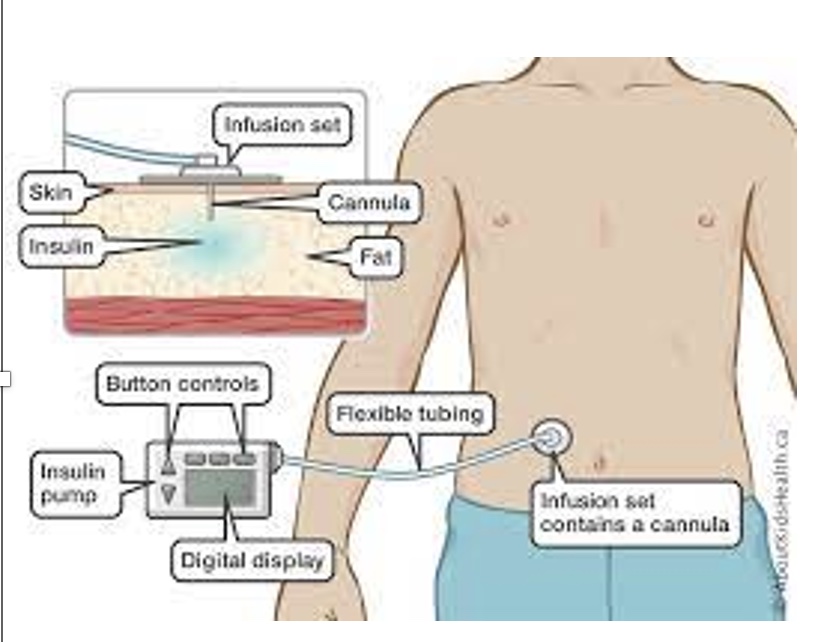
Insulin pumps
*may have to adjust during exercise
-For T1DM using insulin pumps, insulin delivery during exercise can be markedly reduced by decreasing the basal rate or disconnecting the pump for short durations, depending on the intensity and duration of exercise.
oReducing basal insulin delivery rates for up to 12 hours postexercise may be necessary to avoid later-onset hypoglycemia.
-Continuous glucose monitors may be useful in detecting patterns in blood glucose across multiple days and evaluating the effects of exercise.
DM: special considerations (in general)
-Individuals who have experienced exercise-induced hypoglycemia should ideally exercise with a partner or under supervision.
-During exercise, carry medical ID, a cell phone, and glucose tablets or other rapid carbohydrate treatment for hypoglycemia.
-In older individuals with T2DM, the joint occurrence of hypoglycemia unawareness and deteriorated cognitive function is a critical factor that needs to be considered.
-Regardless of initial blood glucose levels, vigorous activity may cause elevations in glucose.
oMay need small doses of supplemental insulin to lower postexercise hyperglycemia
-Dehydration resulting from polyuria secondary to hyperglycemia may contribute to a compromised thermoregulatory response and/or elevated blood glucose levels.
+higher risk of dehydration bc pee a lot
-Given the likelihood that thermoregulation in hot and cold environments is impaired, additional precautions for heat and cold illness are warranted.
Overweight and Obesity: BMI’s + prevalence in US
-Overweight: BMI of 25–29.9 kg · m−2
-Obesity: BMI of 30 kg · m−2 or greater
*dif scales to classify obesity
-~70% of U.S. adults are classified overweight/obese
o40% obese; 7% extremely obese (BMI ≥40 kg ∙ m−2)
-Ethnic and gender disparities
-32% of children and adolescents are overweight or obese.
*often carry into adulthood; nurture and nature
-Linked to numerous chronic diseases: CVD, DM, some forms of cancer, and musculoskeletal problems
*more GI tract cancer bc less transit time
-Obesity-related conditions account for ~7% of total health care costs in the U.S; Direct and indirect costs of obesity are in excess of $190 billion annually.
*often associated w/ HD, metabolic disease, and pulmonary disease
*often more sedentary, bad diet, and poor health=lot health risk
*debate if a disease or a lifestyle
OW and Obesity: weight loss by the numbers + does PA help?
-Sustained weight loss of 3%–5% is likely to result in clinically meaningful reductions in triglycerides, blood glucose and HbA1C levels, and the risk of developing T2DM.
oWeight regain averages ~30%–50% of initial weight loss within 1 year of terminating weight loss treatment. (*often reestablish poor habits, don’t have meds need, etc.)
-Combining reductions in energy intake(EI) with increases in energy expenditure (EE) typically result in an initial 5%–10% reduction in body weight.
-Modest impact of PA on the magnitude of weight loss observed across the initial weight loss intervention compared with reductions in EI
-The combination of moderate reductions in EI with adequate levels of PA maximizes weight loss in individuals with overweight and obesity.
*but difficult bc really high volume not realistic
OW and Obesity: Dose-response relationships
-Dose-response relationship (ACSM position stand):
o<150 mins/wk of PA promotes minimal weight loss
*but still lower mortality and CV risk factors
o>150 mins/wk of PA results in modest weight loss of ~2–3 kg, and
o>225–420 mins/wk of PA results in a 5- to 7.5-kg weight loss
*but need really high volume for significant weight loss; time burden
-No consistent evidence for the amount of PA to prevent weight regain
oMay require more than 150 min/wk or 30 minutes of PA on most days/wk
oSome evidence supports ~200–300 min/wk of PA during weight maintenance to reduce weight regain after weight loss
OW and Obesity: Exercise testing
*don’t have to unless they have other ACSM risk factors
-Not necessary prior to beginning low-to-moderate intensity exercise
-Risk of other comorbidities associated with CVD risk
-The timing of medications, particularly β-blockers and antidiabetic medications, should be considered.
-The presence of musculoskeletal and orthopedic conditions may necessitate the need for using leg or arm ergometry.
-Low exercise capacity may necessitate a low initial workload (2–3 METs) and small increments per testing stage (0.5–1.0 MET).
-Exercise equipment must have adequate weight specifications.
-Ensure appropriate BP cuff size is used.
*max test hard w/ obese patieint
OW and Obesity: Exercise Rx
-Aerobic: needs to progress from 150-300 minutes to get weight loss
-Goals:
oMaximize amount of caloric expenditure to enhance amount of weight loss
oIntegrate exercise into individual’s lifestyle to prepare for successful weight loss maintenance
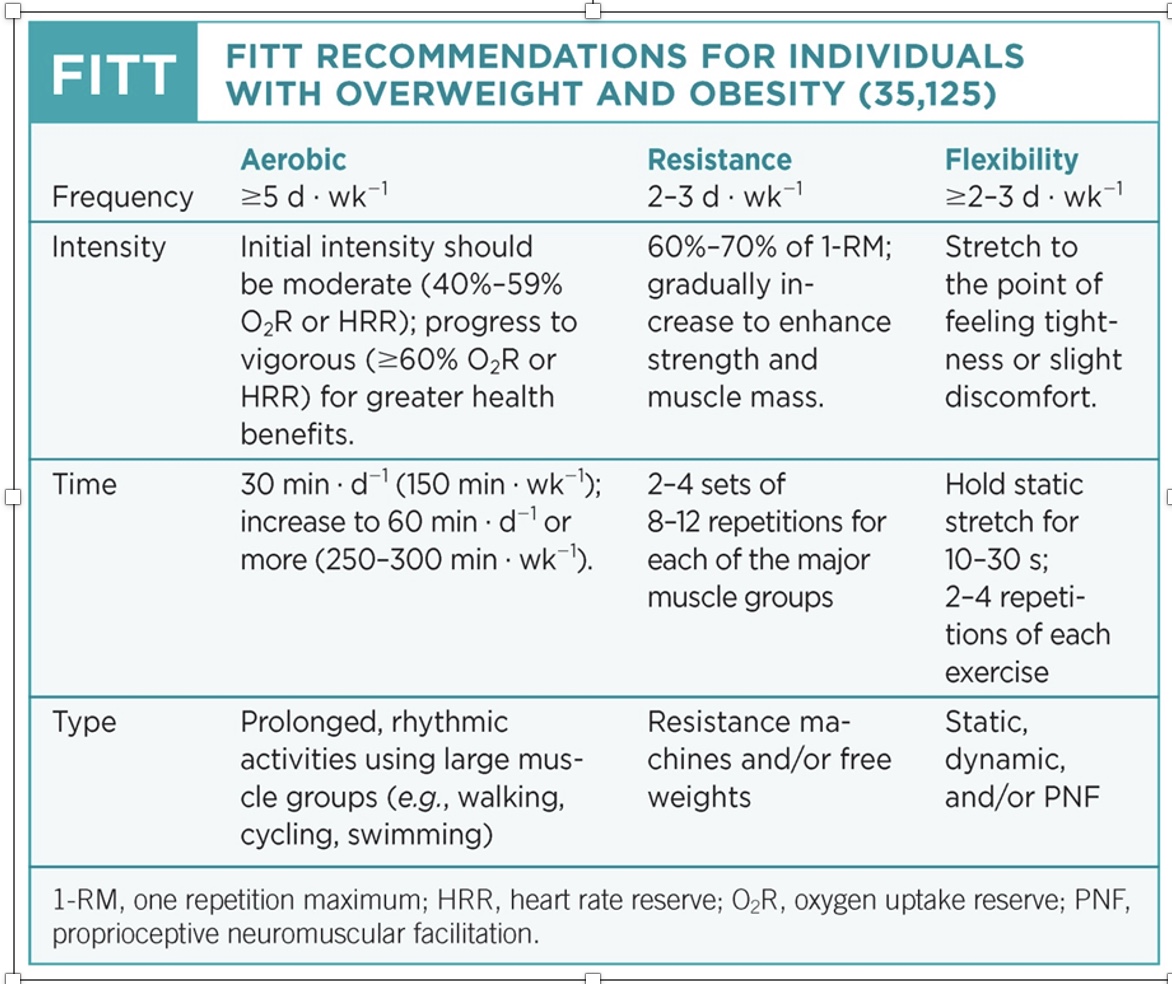
OW and Obesity: Exercise training considerations
-Long-term weight loss maintenance: progress to at least 250 min ∙ wk−1 (>2,000 kcal ∙ wk−1) of moderate-to-vigorous exercise
oExercise and PA should be performed on 5–7 d ∙ wk−1.
-Resistance training alone does not result in clinically significant weight loss.
oThe addition of resistance exercise to energy restriction may not prevent the loss of fat-free mass or the observed reduction in resting EE.
oResistance exercise may enhance muscular strength and physical function.
oAdditional health benefits: improvements in CVD and DM risk factors and other chronic disease risk factors
*RT effective, but by self doesn’t promote weight loss; can hide aerobic in and build up
OW and Obesity: general treatment strategies
-Goal setting: target a minimal reduction in body weight of at least 3%–10% of initial body weight over 3–6 months
-Target Energy Intake: a reduction of 500–1,000 kcal ∙ d−1 is adequate to elicit a weight loss of 1–2 lb ∙ wk−1 (0.5–0.9 kg ∙ wk−1)
*but consider psychological reasons too
-Weight loss beyond 5%–10% may require more aggressive nutrition, exercise, and behavioral intervention.
oFor those who do not respond to any degree of lifestyle intervention, medical treatments such as medications or surgery may be appropriate.
OW and Obesity: Hospital intervention treatment strategies
-Medically indicated very low–calorie diets (<1,500 kcal · d−1) can result in greater initial weight loss amounts.
oOnly used for selected individuals and for short periods of time.
oUsually in an in-patient, controlled environment
*establish compliance before surgery
-Incorporate opportunities to enhance communication between health care professionals, registered dietitian nutritionists, and exercise professionals and individuals with overweight and obesity following the initial weight loss period.
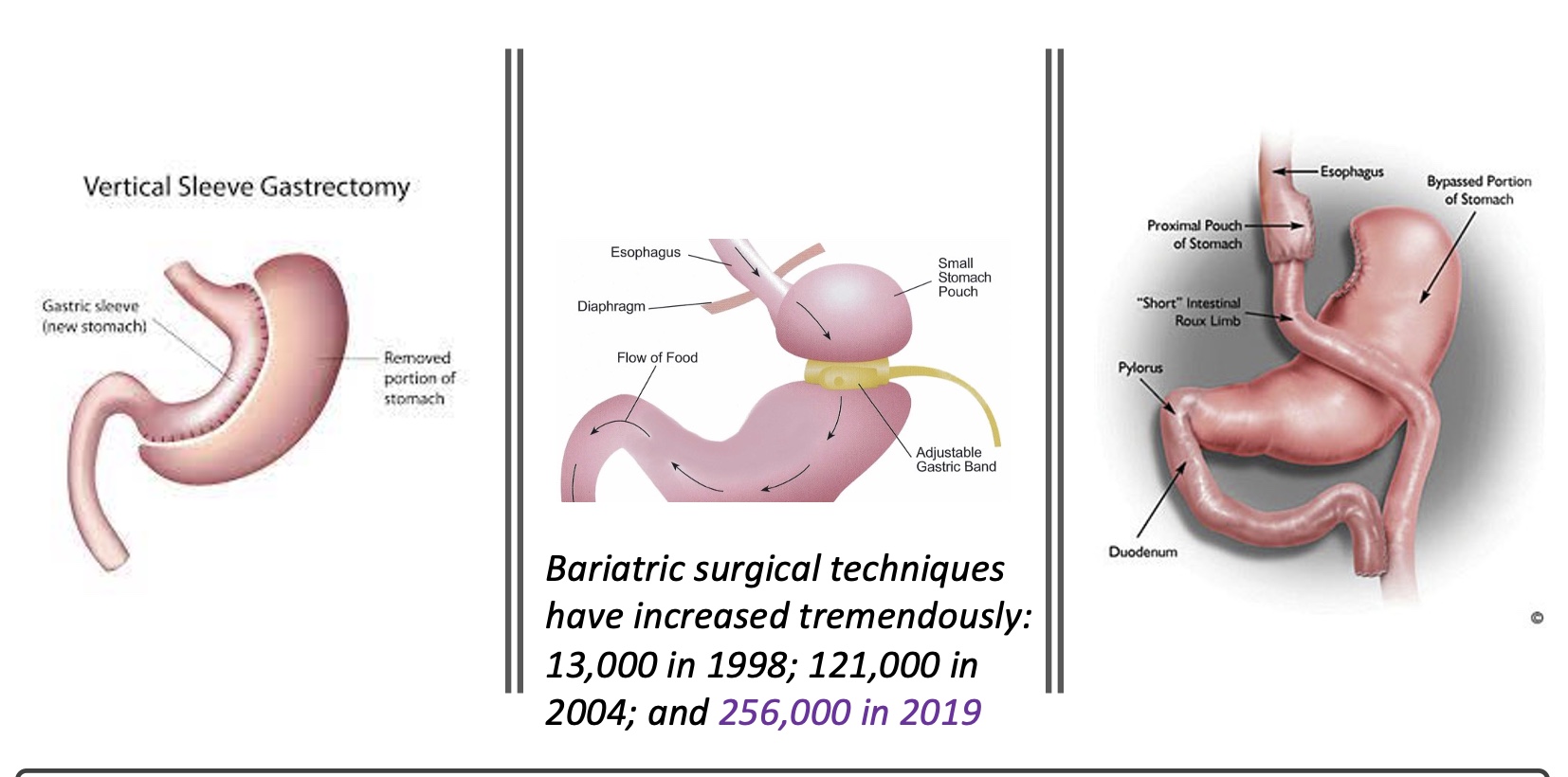
Bariatric Surgery
-May be indicated for individuals with a BMI ≥40 kg ∙ m−2 or those with comorbid risk factors and BMI ≥35 kg ∙ m−2
-Exercise will likely facilitate the achievement and maintenance of energy balance post-surgery.
oEvidence of improved insulin sensitivity and CRF following surgery
oOnce cleared for post-surgery exercise, follow the FITT principle for overweight and obese individuals.
oIndividuals with a history of orthopedic injuries should be assessed to reduce the risk of aggravation by weight-bearing exercise.
Options
-vertical sleeve gastrectomy: more common now bc still use stomach
-gastric band: most common; feel full quicker (so need to change lifestyle otherwise could die)
-complete gastric bypass: eating any large volume causes distress; but lose stomach nutrition