Health Psych Final Exam
1/162
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
CHRONIC DISEASE
•Conditions or illness that last 1 year or more and require ongoing medical attention
•Illnesses that are prolonged, do not resolve spontaneously, and are rarely cured completely (Centers for Disease Control)
•Modalities
–Physical
–Psychological
•It’s important to help them adjust their life to chronic illness
•Improving psychological adjustment
•Improving adherence to treatment
-Diabetes when developed takes a chronic illness and has to be constantly taking meds and doctors appointments
-Psychological chronic illnesses
-Ex: schizophrenia (random thoughts and cognitive processes, hallucinations, see things that other people can’t see or hear, delusions) takes a chronic course
-Ex: OCD (with meds sometimes they get better but they come back)
-Ex: Personality disorders (narcissistic personality disorder, BPD (emotional disturbance, impulsive behaviors)
FACTORS THAT INFLUENCE ILLNESS AND ADJUSTMENT
•Socioeconomic status (SES):
– Low SES is associated with having fewer social and psychological resources to manage illness
•Low SES is an important determinant of access to health care.
•Individuals with low SES are more likely to be Medicaid* recipients or uninsured, have poor-quality health care, and seek health care less often.
•Gender, culture, and ethnicity:
– Differences in risk factors, treatment processes, and mental and physical consequences of having a chronic disease
*Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities
Gender, culture, ethnicity differences in risk factors (African American psych)
Appraisals and adjustment
•Lazarus: What matters is not what event occurs, but how we perceive and interpret that event.
•The process of perceiving and interpreting the event is called psychological appraisal.
Appraisals can help with adjusting to chronic illness
Changing the way someone looks at having a chronic illness
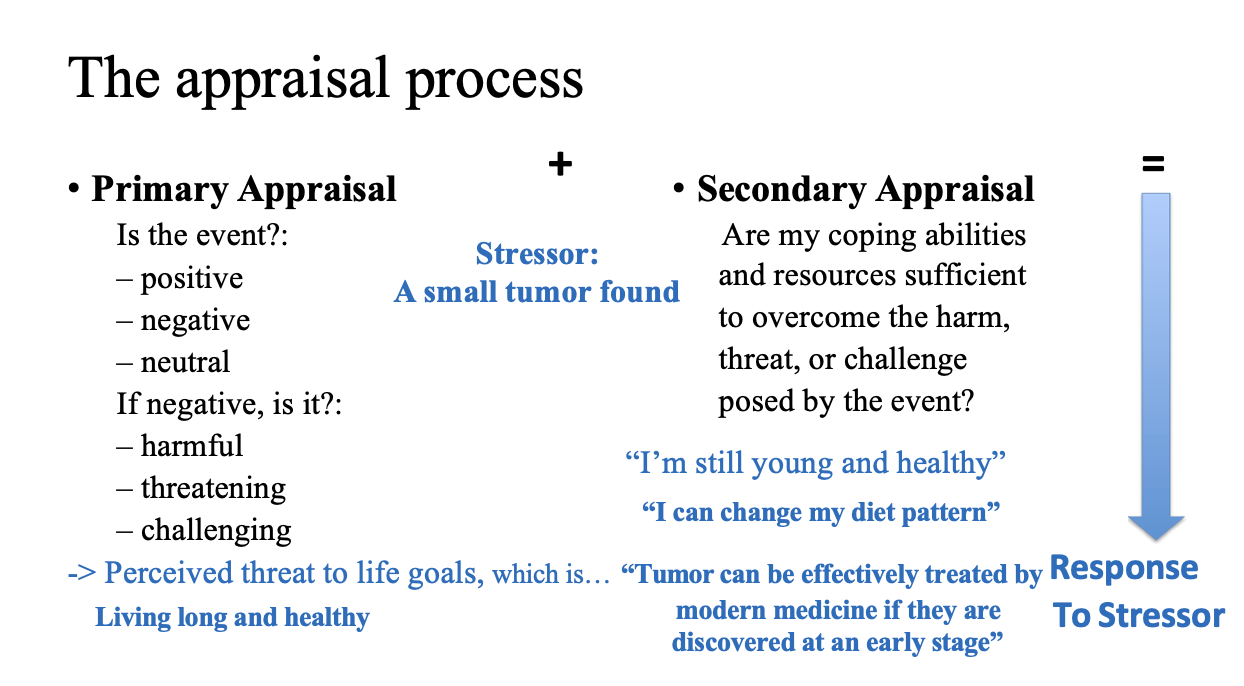
The appraisal process
•Primary Appraisal
Is the event?:
–positive
–negative
–neutral
If negative, is it?:
–harmful
–threatening
challenging
-> Perceived threat to life goals, which is…
Getting into Samsung!
•Secondary Appraisal: Are my coping abilities and resources sufficient to overcome the harm, threat, or challenge posed by the event?
-> Perceived control
“Actually,my IQ is 150”/ “My GPA is 4.2 so far”/ “And more importantly
My uncle is”:
Primary: What does the situation means to be; positive? Neutral? Doesn’t stress us. If its negative then we take another step (harmful, threatening, challenging?)
-Do I have the resources to manage this?
-Secondary: remind yourself of resources that you have that will help ypu overcome the threat
-Uncle is CEO
-Or I have a good GPA
Thinking about having a small tumor, its negative and threatening to me, this is a threat to the life goal of living long a healthy
Secondary: remind people of the resources and abilities they have to help them over come this in a positive way
ex: I'm still young and healthy and can change my diet to help fight the tumor, also if discovered early I have higher chances of treatment
Better way of helping people see the positive with illnesses
APPRAISAL PROCESSES INFLUENCE ADJUSTMENT
•How Appraisal can influence adjustment to illness?
•Perceived threat to life goals – primary appraisal
•Perceived control – secondary appraisal
•The individual’s appraisal of perceived control (having a sense of control)
can influence subsequent psychological adjustment.
•Appraisal also can help individuals find meaning
If someone has a better sense of control it can help people cope with illnesses
APPRAISAL TECHNIQUES TO PROMOTE ADJUSTMENT
1.Have a sense of control over events in your life
2.Write about your traumas
Traumas: chronic illnesses and writing about it can help people see the good.
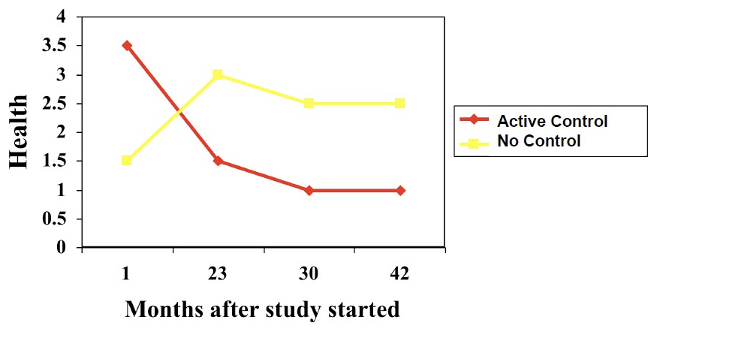
Control Over Events: Study 1
•Nursing home (요양원) residents were randomly assigned to:
–Passive control group: received plants that nurses took care of
–Active control group: chose plant to take care of themselves
Measured: health and mortality
•Results
–Residents in active control vs. passive condition were:
•Happier, more active, and more alert 1 month later
•Less likely to have died 18 months later
Takeaway message?
How can you use this lesson to help people suffering from chronic illness?
People who where actively taking care of the plant were happier and more active, they were also less likely to have died 18 months later (even if they had a lower mortality) more control has an effect
Give people with chronic illnesses a sense of control and given them choice over control over something can have huge psychological effects
Control Over Events: Study 2
•Nursing home residents were randomly assigned to:
–Passive: Residents were visited by students at pre-arranged times
–Active: Residents participated in scheduling when they would be visited
•Results
–Residents in active control vs. passive condition were:
•More hopeful, less lonely and less bored 1 month later
Rated as healthier by nurses and required less medication1month later
Pre-arranged (participants were not able to choose the time people visited)
Active (participants scheduled when they got visitors)
Active were more hopeful, less lonely and more healthier and required less medication (not just subjective but also an objective outcome)
When the active control was removed there was a big regression
When removed maybe they felt depressed from losing the active control they used to have
Having a sense of control is quite powerful when dealing with chronic illnesses
Trauma writing (aka., expressive writing)
•Writing about thoughts and feelings that arise from a traumatic or stressful life experience.
•It may help some people cope with the emotional pressure of the negative experiences.
Write about thoughts and feelings can help people cope with the emotional pressure of the negative experiences
Can help adjust to stressful life events
Trauma Writing: Study 1
•46 Healthy college students were randomly assigned to write for 20 min/day for 4 consecutive days about:
•A trauma (a trauma writing condition)
•“I want you to write about a trauma or personal trouble that you may be experiencing right now, or that you experienced at some other time in your life. I want you to write about the topic that is personally most significant to you. I want you to just let go and express yourself and write about your deepest thoughts and feelings related to this issue. Ideally it will be something that you have not talked about in detail with others.”
•A trivial topic (a trivial writing condition) – 일상의 사소한, 소소한 이야기들
Two different conditions
1.Trauma writing condition to write about trauma for 20 mins a day for four days
2.Trivial topic writing about what you ate for lunch etc
•Results
– Subjects in the trauma, compared with the trivial writing conditions had:
-fewer health care center visits 6 weeks later
-Improved immune system functioning
-Lesson?
—
1.Trauma had less health care visits suggesting they are healthier
1.Helps boost health condition and positive health outcomes
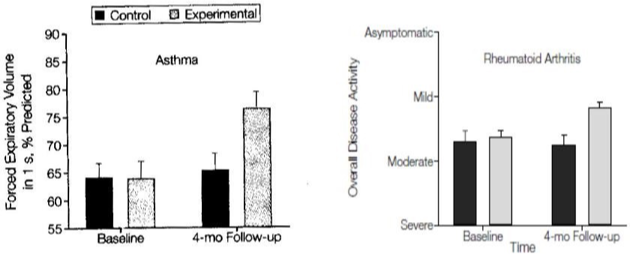
Trauma Writing: Study 2
•Asthma and arthritis (관절염) patients were randomly assigned to write 20 mins/day for 3 days about:
–A trauma (experimental condition)
–Trivial topics (control condition)
•Dependent variables: Measured pulmonary (lung) function (asthma patients) and disease symptoms (arthritis patients)
Chronic illness patients were randomly assigned to trauma vs trivial writing conditions
Led to all kinds of good health outcomes
Symptoms in patients improved after trauma writing
Baseline: Before the writing there was no significant differences
After four months there is a huge significant group difference
HOW DOES TRAUMA WRITING IMPROVE YOUR HEALTH?
•Hypothesis 1:
Inhibiting/suppressing hurts you, so may be disclosing helps you
Trauma writing can help greatly improve health conditions (helps them express themselves) helps to lessen suppression
•Hypothesis 2:
–Helps people find meaning in their circumstances.
•Finding meaning in life is a subjective perception of having one or more
specific purposes for one’s own life.
Evidence to support hypothesis one but can be another hypothesis
•Hypothesis 3:
- Helps people to affirm positive aspects of their selves.
Does inhibiting personal information lead to poor health?
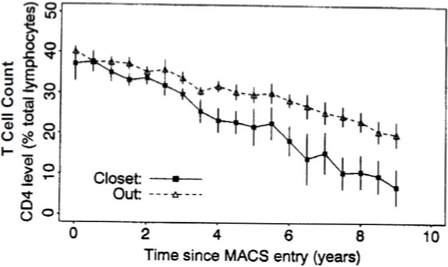
•HIV+ gay males divided into groups based on disclosure status:
–Coming out (out of closet)
–No coming out (hiding their gender(sexuality?) identities) (in the closet)
•Dependent variables:
- Measured immune function, AIDS onset, and mortality.
Immune system function declines more quickly for men hiding their gender identities (no coming out)
-> Inhibiting may hurt, and disclosure can help with chronic illness
Declines more with men who hide more identity (blue line)
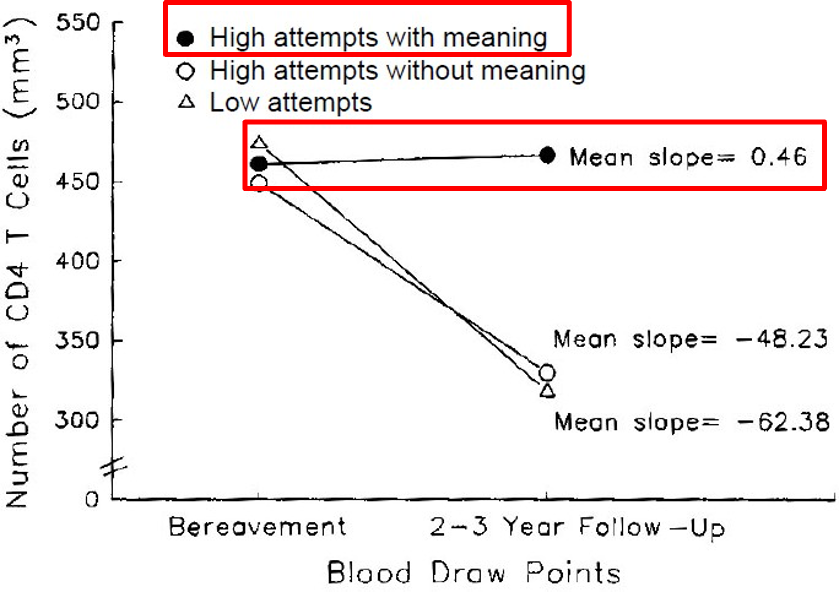
Does Finding Meaning Lead To Better Health?
•Interviewed bereaved HIV+ men divided into three groups: (bereaved: deprived of a close relation or family through their death; 가족, 친족을 잃은).
–Group 1: Those who didn’t try to find meaning
–Group 2: Those who tried to find meaning and failed
–Group 3: Those who tried to find meaning and succeeded
•Dependent variable: measured immune function across time
Losing a family member
•Better Immune system function for those who found meaning
•15/40 men died during study; only 3 of these 15 had found meaning
-> Finding meaning can help with adjusting to chronic illness.
9/11 survivors
•9/11 survivors
•Survey of nearly 1,000 people 2 months after 9/11 and 2 years after 9/11
–People who were searching for meaning had higher post-traumatic stress
–People who had found meaning had fewer stress symptoms
-> It is not just searching for meaning but finding meaning that leads to better health
People who just tried to find to meaning had higher stress but when found had fewer stress
Searching (thing about the meaning but it may not be enough, in order to be powerful they have to have a deeper thinking process)
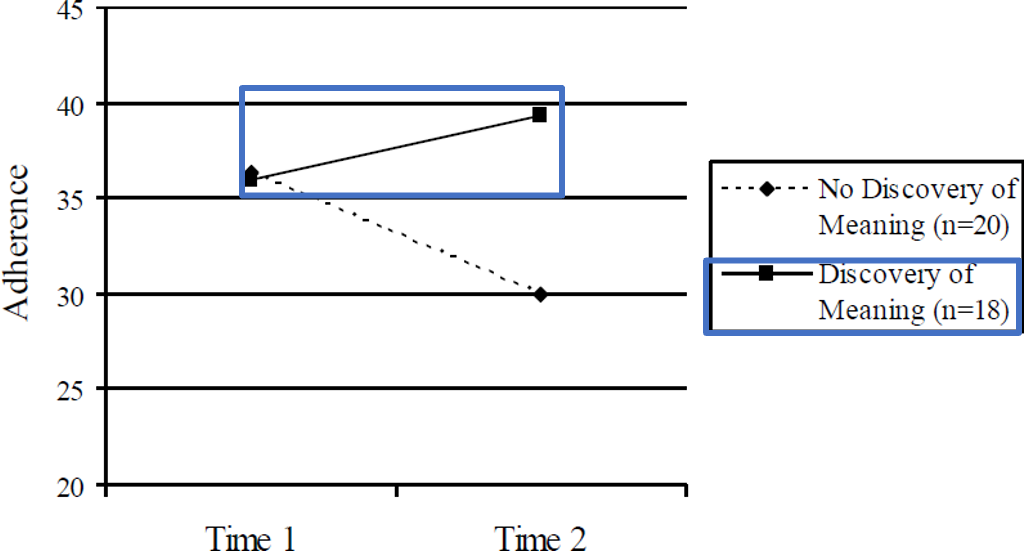
Finding Meaning and Health Behaviors
•HIV Infected Women wrote journals 2 times a week for a month
– Coded journals for signs of finding meaning
- Measured medication adherence before and after
•Examples of finding meaning
•“Knowing what I know now about being sick makes me see life in a whole different way.”
•“It made me realize how I appreciate life more now than I have in the past and I live one day at a time and try to enjoy each day to the fullest.”
•“I love life and have learned to value it dearly.”
Searching for meaning in life vs. Finding meaning
•Searching for meaning: being motivated to understand the nature and purpose of existence
•Not everyone who’s searching for meaning ends up finding meaning
•It can become stressful when the search becomes frustrating.
•If the meaning that one is focusing on is not feasible:
•This can lead to distress or unhappiness
Not everyone who searches for meaning finds it
•Finding meaning:
•Finding meaning in life is a subjective perception of having one or more specific purposes for one’s own life
•Examples:
•I understand my life’s meaning”
•“My life has a clear sense”
Higher adherence rate for those who found meaning
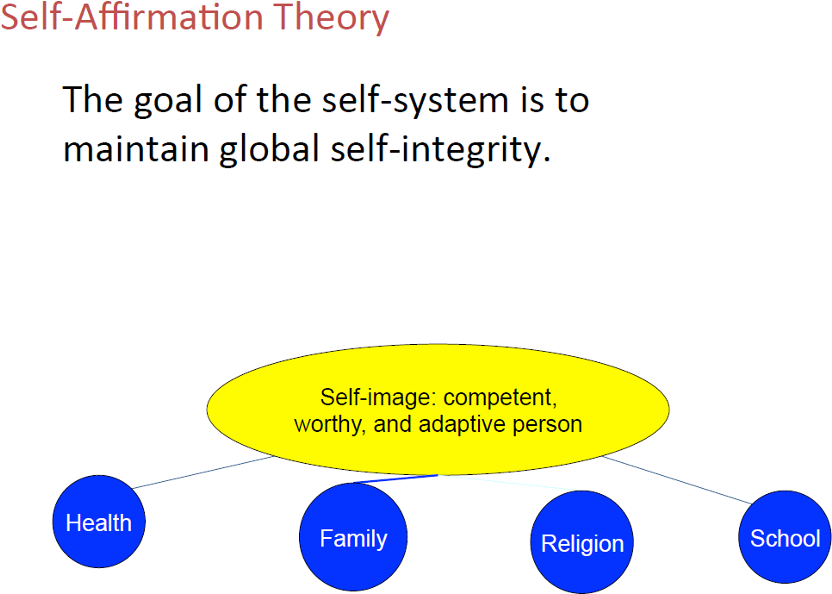
Self-affirmation and health
•Positive reflection on a valued source of self worth.
– valued relationship, religion, concern for others, hobbies, health, being affirmed by others, career/education, property
•Overall goal of the self-system is to protect one’s image of self-integrity when threatened
Protect self image which include chronic illnesses, one can use self-affrimation can protect themselves against the threat
Does Self-Affirmation Lead To Better Health?
•Early-stage breast cancer survivors (N=63) wrote 4 essays over 3 weeks
–Essays coded for self-affirmation (the amount of self-affirmation statements)
–Essays coded for searching for meaning (how much did they try to understand
the meaning of their lives?)
•Measured physical symptoms and cancer related doctor visits before writing and 3 months later (dependent)
•Affirming the self led to fewer physical symptoms and fewer cancer- related doctor visits 3 months later.
•Searching for meaning was not related to physical symptoms or cancer-related doctor visits 3 months later.
•Perhaps affirming the self is the crucial ingredient in the writing studies?
Affirming self is the core component in the trauma writing and not just searching for meaning.
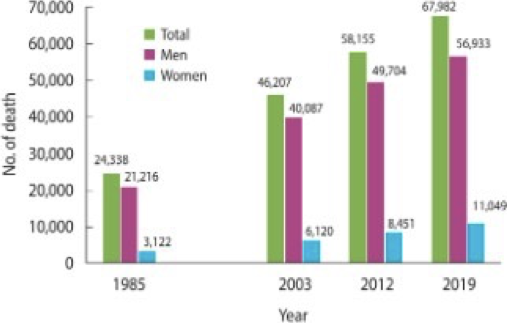
Smoking
–Most preventable cause of death in the world
–In Korea, around 60,000 people die due to tobacco- related issues
Smoking has increased drastically
•What components in smoke are dangerous?
–Cigarettes contain 4,000 compounds, 60 of those are carcinogens
•Carcinogens - substances capable of causing cancer
•Nicotine - stimulant found in cigarettes
•Tars – water-soluble residue: contains many carcinogens
Nicotine doesn’t cause cancer but instead addition
Nicotine
–Can be found in the brain 7 seconds after smoking
–Half-life* is 30-40 minutes
–Increases metabolic level and decreases appetite
*Half-life: the time it takes for the amount of a drug's active substance in your body to reduce by half.
Makes addicted to smoke and travels to the body, can travel to the brain in seven seconds, takes 30-40 mins for the amount of nicotine to reduce by half in our system.
Tobacco Use
•Who smokes?
–More men smoke than women
–Older adults have low smoking rates
–Low income people have high smoking rates
–Those with low education level have high smoking rates
Demographic info, more men than women, higher in men, lower income = higher rates of smoking
Why do people start smoking?
•Why do people start smoking?
–Genetics
–Social Pressure
–Advertising
–Weight Control
(Genetics)
–Genetic variations increase people’s vulnerability to become (and remain) smokers
•The neurotransmitter dopamine may be implicated
•(genetic) abnormalities in the dopamine system
–Genes + social environment -> smoking initiation
Plays an important role in leading individuals to many different kinds of diseases, same for smoking. Dopamine is a nervous transmitter important in reward system, smoking releases dopamine which gives of pleasure feelings.
Some genetic abnormalities are found in addicts system
Genes are not the only cause but once Genes combine with social environments (living with people who smoke can lead to smoking)
•Social Pressure
–Teens may be encouraged to smoke by their peers
•To “fit in” with social groups or what they see in
movies or media
–Teens are also more likely to smoke if they live with a smoker
•Advertising
–Curiosity may impact teens’ decisions to
begin smoking
–Anti-smoking campaigns are not a very effective way to prevent smoking according to research
Curiosity may be one of the critical reasons teens start smoking
Fear tactics aren’t very effective and one of the reasons why anti-smoking is not that effective
•Weight Control
–Young women say they use smoking to lose weight
–other unhealthy means to control their weight
•diet pills or laxatives (완하제)
Some women say smoking helps with weight control and helps them to loss weight (this may be true but in the long term its unhealthy and not helpful)
Why do people continue to smoke?
•Addiction
•Positive and Negative Reinforcement
•Optimistic Bias
•Fearing Weight Gain
When we smoke it releases dopamine and releases pleasure and its two times higher than natural methods of getting pleasure (getting a good grade, going to the gym).
•Addiction
–Nicotine is addictive
–Once people have smoked 100 cigarettes they seem to be addicted
–Low-nicotine cigarettes do not help; smokers just smoke more of them
•Positive and Negative Reinforcement
–Positive Reinforcers
•Pleasure from the smell of smoke
•Feelings of relaxation
•Satisfaction of manual needs
–Negative Reinforcers
•Avoiding withdrawal symptoms
Positive: when positive and negative when does it occur (when a positive stimuli is given)
Ex: studying as a kid and mom saying she will buy you something if you get good grades (positive reinforming)
Ex: negative when your behavior helps to avoid negative event
•Optimistic Bias
–Smokers believe they personally have a lower risk of disease and death than other smokers
–heavy smokers may overestimate their chances of living
•Fear of Weight Gain
–Smokers do gain some weight when they stop
–Women with weight concerns are more likely to smoke than those without weight concerns
Elevate metabolism
Some people do gain weight when they stop smoking
Health Consequences
•Health Consequences of Cigarette Smoking
–Cancer
–CVD
–Chronic Lower Respiratory Disease
–Other effects
•Cancer
–Leading cause of smoking-related deaths
–Male cigarette smokers have a relative risk of about 23.3 times that for nonsmokers for cancer
— —-
•Cardiovascular Disease
–Second largest cause of smoking-related deaths
–CVD risk is doubled for smokers
—- —-
•Chronic Lower Respiratory Diseases
–Chronic bronchitis (만성기관지염)- formation of scar tissue in the bronchi
–Emphysema (폐기종)- scar tissue and mucus obstruct respiratory pathways and air is trapped in the alveoli (폐포)
- —-
•Other effects
–Fire caused by cigarettes
–Disease of various body parts: mouth, kidney, bladder
–Periodontal disease
–Injuries, such as in motor vehicle crashes
Other Health Consequences
•Other effects for women
–Women are more vulnerable to lung cancer than males
–Increased risk for fertility problems, miscarriages
–Smoking women: Low birth-weight infants
—- —-
•Other effects
–Fire caused by cigarettes
–Disease of various body parts: mouth, kidney, bladder
–Periodontal disease
–Injuries, such as in motor vehicle crashes
—- —-
•Other effects
–Mental health
•People who smoke are 3 times more likely to be diagnosed with a psychiatric disorder
•May use smoking to help cope with disorder
Lots of people with ptsd get addicted to drugs including smoking. People with ptsd smoke to help cope with their symptoms
Passive Smoking
•Passive smoking - also called
environmental tobacco smoke (ETS)
–Has been linked to lung cancer, breast cancer, heart disease (CVD) , and respiratory problems in children
•Smoke exposure increases risk of sudden infant death syndrome (SIDS)
2nd degree smoking (children with smoking parents are more susceptible to these diseases) can even cause death in infants
Interventions for Reducing Smoking Rates
•Deterring Smoking (흡연억제)
–Information/education alone does not
deter people from smoking
–More successful are programs that combine information with building skills on how to refuse to smoke, signing pledges not to smoke
Educating people alone doesn’t really deter people from smoking. In order to make these programs more effective we should combine information with building skills on how to refuse to smoke and etc.
Key: Information and helpful behavioral strategies
Quitting Smoking
•Quitting Smoking Without Therapy
–44% of smokers try to quit each year, and 64% of those try so without treatment
–Success rate is 60%; abstinence length around 7 years
•Quitting Smoking Using Pharmacological
(약물적) Approaches
–Nicotine replacement such as gums, inhalers, patches
–Drugs (e.g., bupropion) are used to decrease withdrawal symptoms
•Effective for many but not for teenagers
Drugs combined with psychological help can help reduce withdrawals can help boost the treatment ethicaisy
•Quitting Smoking Using A Psychological Intervention
–Cognitive behavioral approaches, group therapy, contracts, behavior modification are all types of interventions that can be used
–Most effective programs include both a counseling component and a pharmacological component
Medication and counseling by itself may not help but combined its more beneficial
Who quits? Who does not? (Smoking)
– Young smokers, women smokers, lower educated smokers have more difficulty quitting
•Preventing Relapse (재발)
–Relapse is common and 22% of people who relapse actually smoke at a higher rate after relapse
–Self-quitters have high relapse rate
–Behavioral relapse prevention techniques are most important 1-3 months after quitting when vulnerability to start smoking again is high
Effects of Quitting
•One possible negative effect of quitting is weight gain
–Women gain 6 lbs and men 11 lbs after quitting
•Physical exercise can stop weight gain
–However weight gain is still better than continued smoking
•Positive effects of quitting:
–Reduces mortality by 36%
–Quitting smoking by age 35 adds 7-8 years of life expectancy
PSYCHOLOGY OF EATING
•Why is it important?
–Do it several times a day
–Food choices impact health
–Source of pleasure/reinforcement
–Crucial for sustaining life
It’s important cause we eat several times a day
•Cuts across all areas of psychology
–Developmental: How infants regulate food intake
–Cognitive: Memory/cognitions impact how much is eaten
–Social: Eating is influenced by other people and situations
–Clinical: Disordered eating
–Health: Eating has clear health effects
Personality:Individualdifferencesineatinghabits
PSYCHOLOGICAL QUESTIONS ABOUT EATING
1.What determines how much people eat?
2.What are the psychological effects of hunger & starvation?
•Individual differences
•Cognitive factors
•Social/emotional factors
•Developmental factors
Situationalfactors
What makes us eat something and what makes us stop eating.
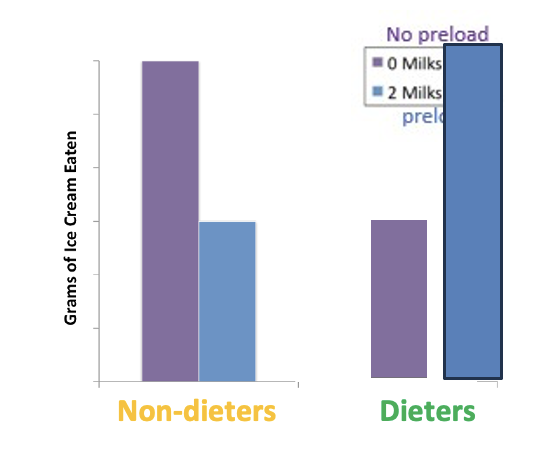
Diet Study
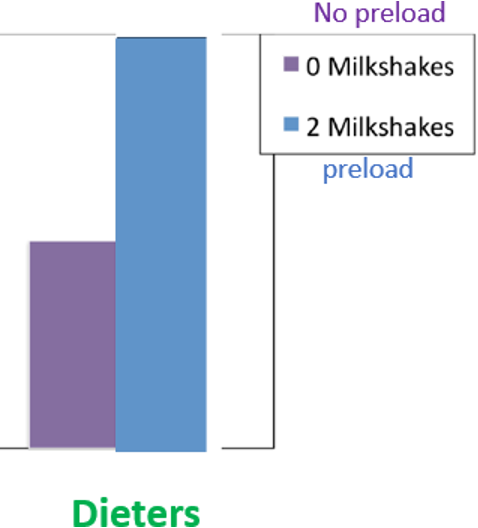
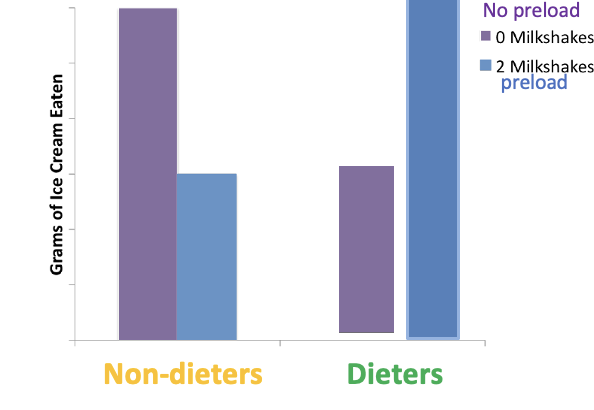
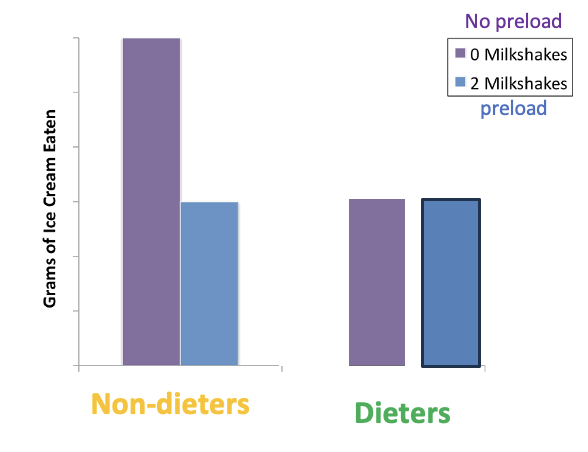
Series of studies of what determines how much people eat and looked at different factors. Recruited people into two groups dieters, and non-dieters
Have half of each group drink a milkshake called preload (having people have a milkshake before they measure the dependent)
Dieters 1- no milkshake
Dieters 2 – milkshake
Non-dieters 1 - no milkshake
Non-dieters 2 – milkshake
Then measured dependent variable (how much icecream does each participant have)
Purple had no milkshakes
Yellow= nondieters
Green= dieters
Nondieters (more people who had no milkshakes ate more icecream, people they are more hungry) non-dieters with preload ate less cause they were full
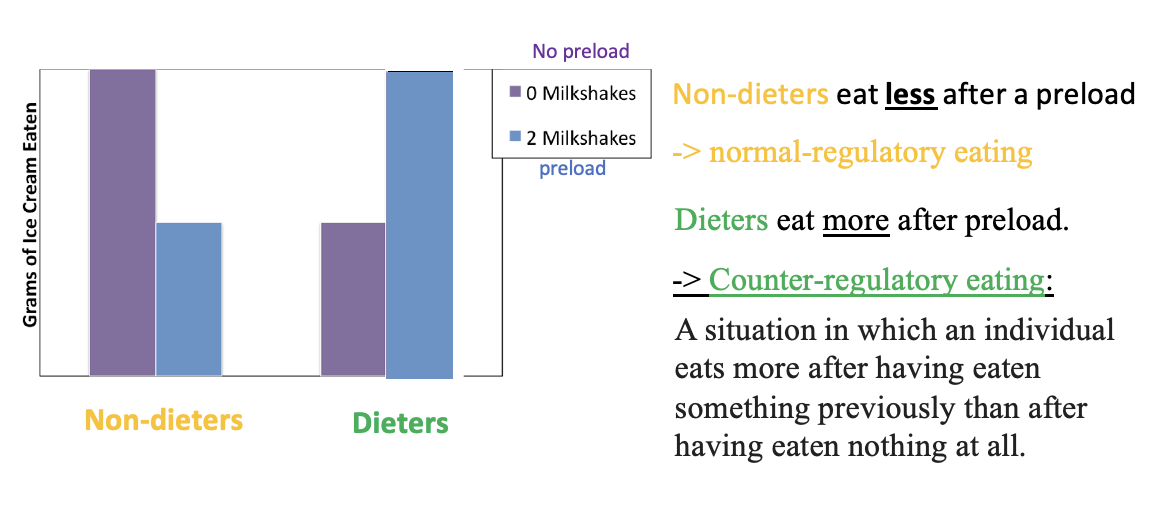
Counter-regulatory eating
•Why dieters eat more after a preload?
•When they receive no preload, their diet scheme remains intact
•They can still achieve their diet goals by restricting
food consumption
•So, they eat only a minimal amount of ice cream
•However, when they receive a preload (“they’re forced to consume milkshake)
•Dieters’ diet scheme gets distracted or fails
•They think there is no point of continuing restrict diet
•So, they eat more ice cream (“the what-the-hell-effect”)
With no preload the diet scheme remains (sticking to strike diet) still achieve diet goals (this is why they only had half of the icecream
With preload the dieter scheme gets restricted and failed (everything is over and there is no point in dieting) eating more cause it doesn’t matter anymore.
IMPORTANT CONTRIBUTIONS
1.Dieters regulate their eating differently than non-dieters
2.Dieting may lead to binge eating
3. Recognized dieters are an important group for psychologists to study
4.Invented a new methodology (preload) for studying eating
Whenever eating scheme is messed up the whole scheme is ruined
CONSUMPTION WHEN A NON-FAT PRELOAD IS LABELED AS HIGH FAT
Non-dieters eat less after a preload. It doesn’t matter whether they think the preload is high fat.
Dieters eat if they think the preload is fat.
— —
New study (similar but) Preload people were given nonfat milkshake but labeled as high fat (liars smh)
What the hell effect (its over so I don’t care anymore)
CONSUMPTION WHEN A HIGH-FAT PRELOAD IS LABELED AS NON-FAT
Non-dieters eat less after a preload. It doesn’t matter whether they think the preload is non-fat.
Dieters do NOT eat if they think the preload is .
Same study but milkshake high fat is labeled as nonfat (even worse liars)
Same amount for dieters (since its nonfat people feel less worried about diet and its still apart of their diet)
CONSUMPTION WHEN OTHERS ARE IN THE ROOM
Non-dieters eat less after a preload. It doesn’t matter if another person is in the room.
Dieters do NOT eat if there is in the room.
Because social presence triggers self-consciousness and reduces disinhibited eating
Same design but eating icecream in the presence of others
CONSUMPTION WHEN STRESSED (Dieting)
ÞIn this study, all participants were exposed to a manipulation condition that induced some level of stress.
ÞSubsequently, the researchers examined the differences in eating behavior following a preload between the dieters and non-dieters.
Non-dieterseatlessafterapreload. Itdoesn’tmatteriftheyarestressed
Dieters eat even after a preload if they are stressed
When stress is added it further impairs self-control increases amplified counter-regulatory eating
CONCLUSIONS FROM LAB STUDIES OF EATING:
•The eating of non-dieters is influenced more by: hunger than by cognitive, social, or emotional factors:
–They eat less after a preload milkshake
–It doesn’t matter whether they think the preload milkshake is high fat
–It doesn’t matter if another person is in the room
–It doesn’t matter if they are stressed
•The eating of dieters is influenced more by cognitive, social, and emotional factors than by hunger:
–They eat more after a preload
–If they think the preload milkshake is high fat,
–If they think the preload milkshake is low fat, they
–If there is another person in the room, they after a preload
–They eat after stress
COGNITION AND EATING: MEMORY
Subjects:
–Patients with memory intact (기억력 정상) (Control group)
–Patients with dense amnesia (기억상실증) (Study group)
Design:
–Patients brought lunch
–Patients eat lunch and trays are cleared
–Patients distracted for 20 minutes
–Patients brought another lunch
Question: Do Patients with amnesia eat the second lunch?
Results: They ate the meal, as they had no memory of the first meal
DEVELOPMENT AND EATING
•Question: How many calories do children eat from day to day if they are allowed to decide for themselves?
•Study:
–Children were allowed to eat as much as they want, with no adult input, for 6
days.
–Amount eaten was measured by meal and by day
•Results:
Children were bad at regulating calories at individual meals. But they regulated well over the course of each day.
Some kids skipped breakfast and were so mad at eating three regular meals, but they regulated well over the course of the days. (if skipped breakfast than eat more at lunch and dinner) still the require calories needed
PSYCHOLOGICAL EFFECTS OF HUNGER
•Hungry people become:
–Irritable
–Unreasonable
–Weak
–Apathetic (무감정의)
•They also:
–May have hallucinations (환각)
–can become obsessed with food
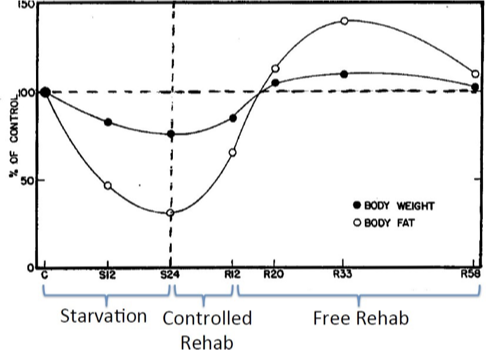
SEMI-STARVATION STUDY
36 conscientious objectors (양심적 병역거부자) from World War-II
(A conscientious objector is an individual who has claimed the right to refuse to perform military service)
•Lived in dorms for one year:
–Control period: ~3 months
•3,200 cals/day
–Semi-starvation period: ~6 months
•1570 cals/day
–Controlled eating rehabilitation: ~3 months
•2000-3200 cals/day
–Free eating rehabilitation: ~3 months +
•Unlimited cals/day
3. PSYCHOLOGICAL EFFECTS OF STARVATION
•Obsession with food
•Eating rituals
•Weak
•Tired
•Irritable
•No self control
Anxious
•Nervous
•Self-centered
•Apathetic
•Clinical Depression
•Psychotic (조현병적) reactions: e.g., hallucinations
(in 1/6th of the subjects)
PRIMARY CONCLUSIONS
1)The amount of food people eat is based on hunger, dieting status, cognitive, social, emotional, and developmental factors
2)Starvation can lead to psychological disturbances and food obsessions, and these effects last long after food becomes available.
BMI: Korean standards
•BMI 23-24.9 kg/m2 : Overweight (과체중)
•BMI 25-29.9 kg/m2 : Stage 1 obesity
•BMI 30-34.9 kg/m2 : Stage 2 obesity
•BMI ≥ 35 kg/m2 : Stage 3 obesity
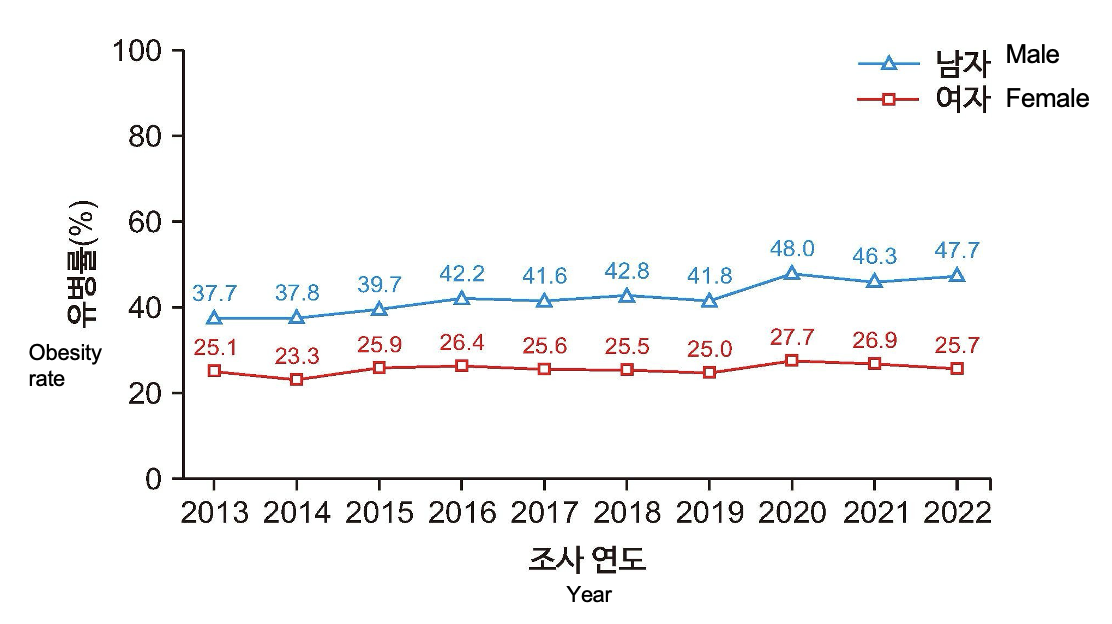
RATES OF OBESITY AND OVERWEIGHT 1998-2019
The prevalence of obesity over the past 10 years
Rates are going up over time.
What are driving factors? Rise in food industry (regular burger compared to the new burger)
More impossible to live in the united states without a car compared to korea where the subway system is better. This may be a cause for the increase in obesity
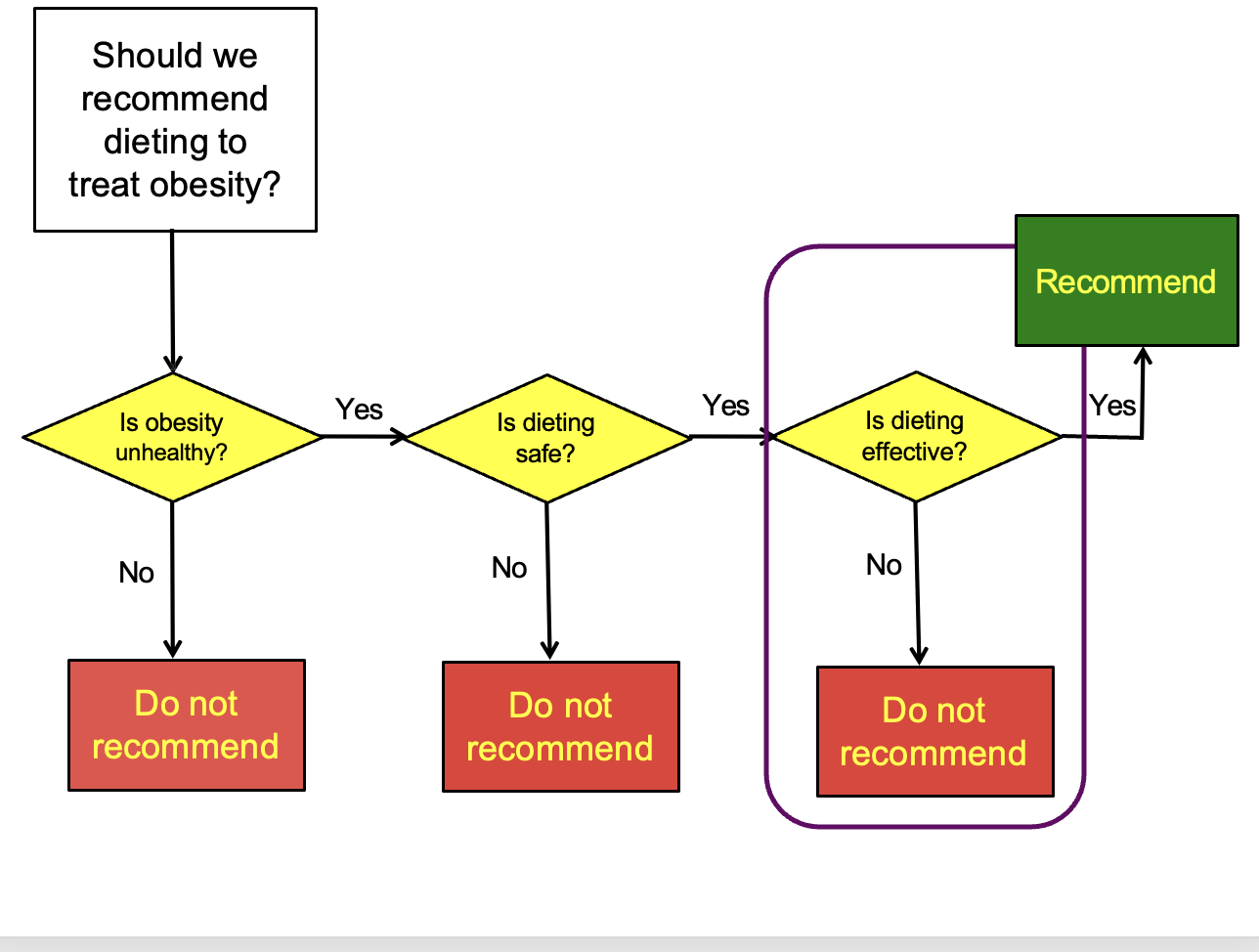
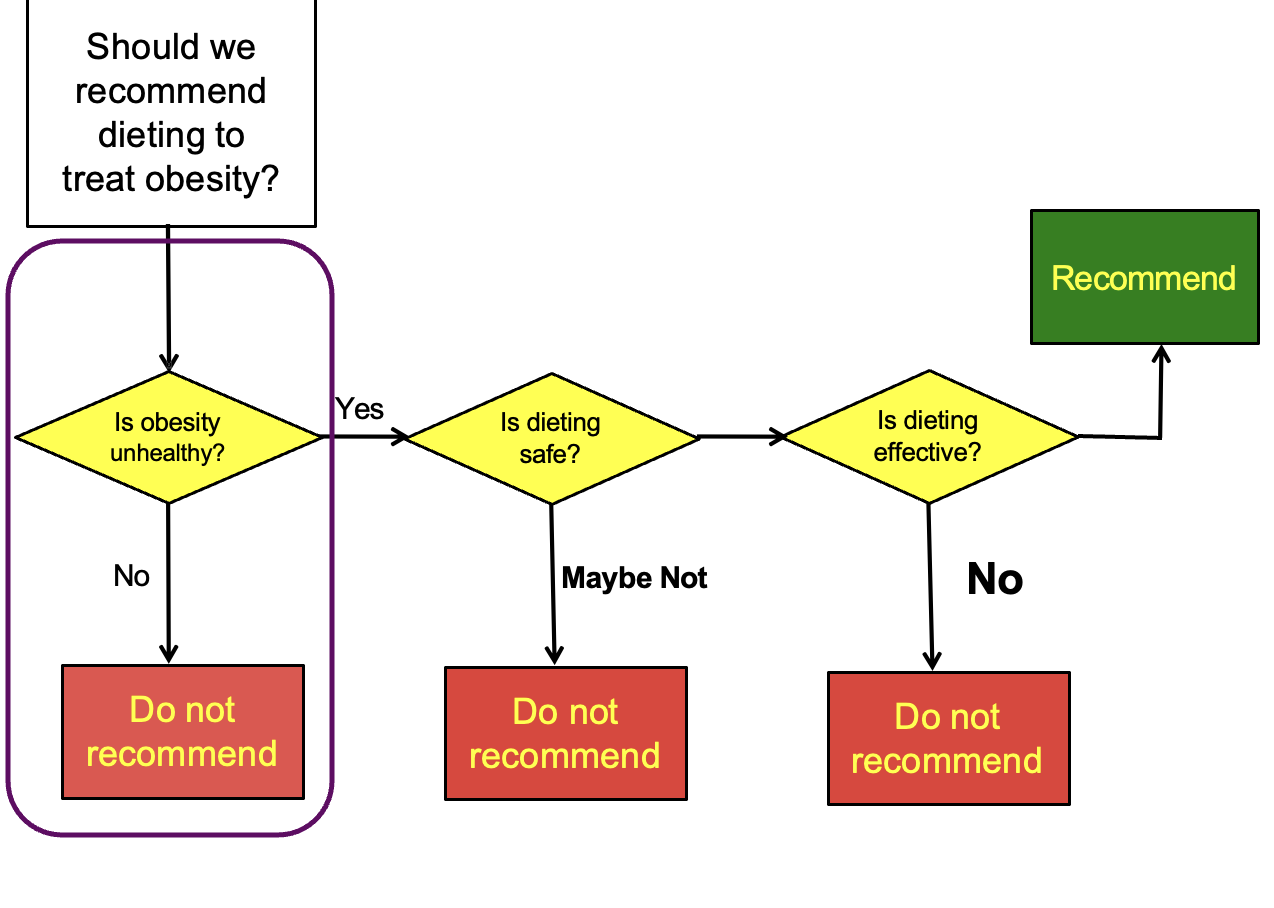
IS DIETING THE ANSWER TO THE PROBLEM OF OBESITY?
•Should doctors recommend diets to treat obesity?
•Psychologists should determine the following first
–test safety (first in non-humans, then humans)
–test efficacy
LONG-TERM DIET STUDIES
•Studies with control groups (n=21)
–Avg. weight change of dieters: Lost 2 lbs
–Avg. weight change of controls: Gained 1 lb
–Not a statistically significant difference!
–Diet may not be effective.
On average people only lose about 2lbs
•Studies without control groups (n=13)
–Initial weight loss: 39 pounds
–Ultimate gain-back: 32 pounds
–Having been on diet led to losing 7 pounds, which
was not very satisfying outcome!
–Is diet effective?
% who regain more than they lost: 31% to 64%
-> These people ended up gaining more in a long run.
-> These studies also included many systematic biases.
31-64 percent gained more weight than what they lost
Diets don’t seem to be that effective
BIAS: SELF-REPORTED WEIGHTS
Independent evidence: People under-report their weight by about 8 pounds, and obese people tend to under-report by more than that.
61% of all follow-up weights in these studies were self-reported.
-> Findings about weight loss may have been exaggerated by people’s tendency to under-report.
Self-report tend to have people underreport their weight 8 pounds under and obese people tend to do more underreporting.
Dieting may not be effective (it may be recommended to not recommend dieting for obese people)
MECHANISMS OF DIET FAILURE
Dieting is costly (thousands of dollars)
Psychological pathways: on diet, diet scheme can be violated (milkshake diet scheme) can lead to overeating
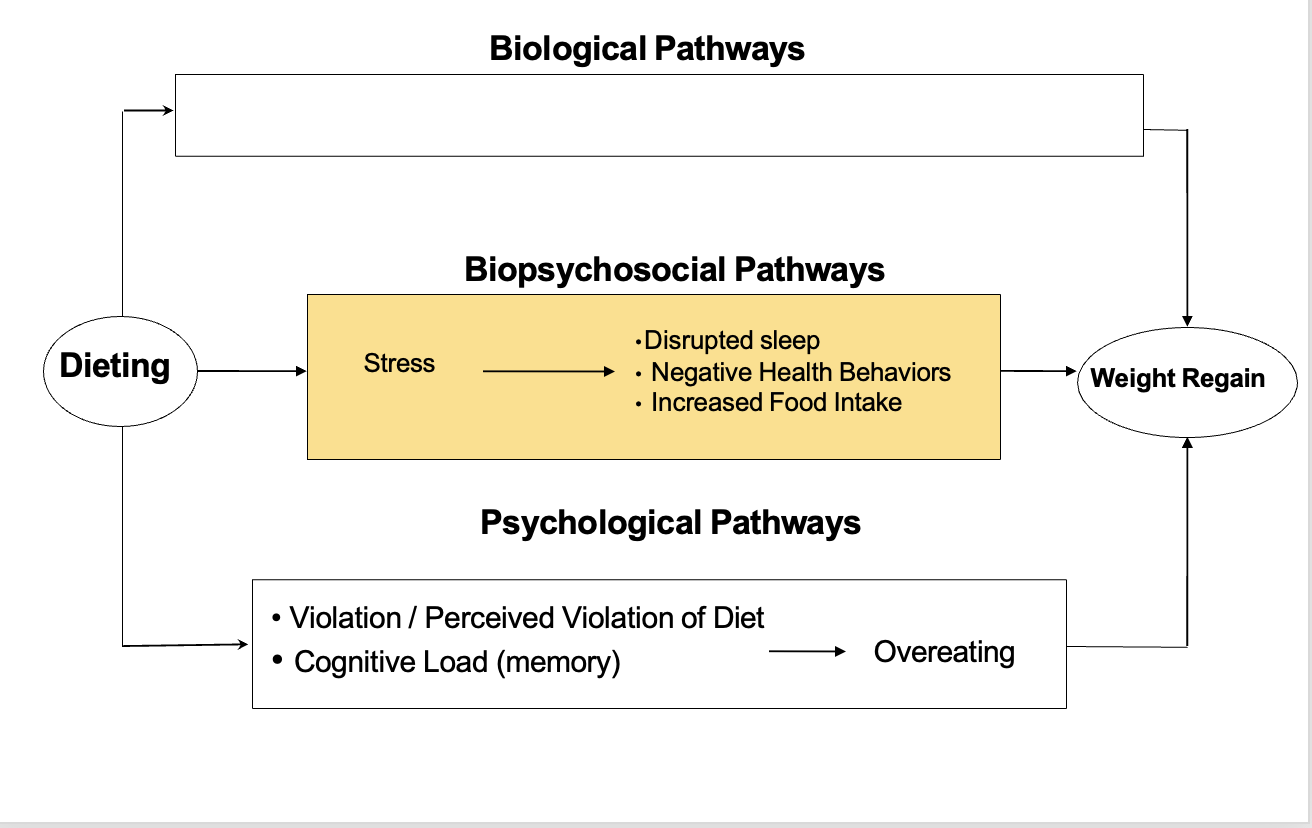
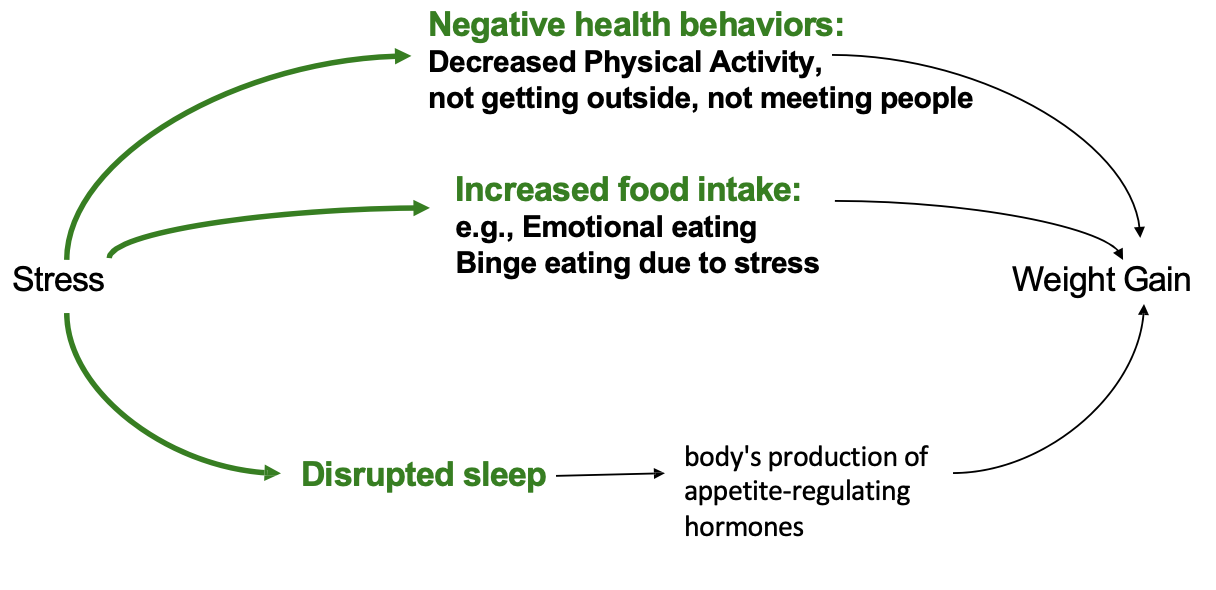
HOW MIGHT STRESS LEAD TO WEIGHT GAIN?
Stress can lead to increase in food intake leading to weight gain
IS DIETING SAFE?
There is evidence that dieting can lead to:
Stress – and its consequences
Mood problems: depression, guilt, shame
Cognitive Impairments (e.g., preoccupation with
food)
Negative health outcomes
Weight cycling (weight gain, yoyo)
Depends on who you are
OBESITY-HEALTH Outcomes
Physical health impacts
•Type 2 diabetes, hypertension, stroke, Coronary Artery Disease, asthma, chronic back pain, etc
Impact on mental health
•overweight may be a stigma
•The obesity discrimination can lead to some mental disorders/bad mental health
•Low self-esteem, mood disorders, interpersonal communication problems, quality of life
Picture: The relation between obesity and health outcomes among women with breast cancers (Majed et al., 2017)
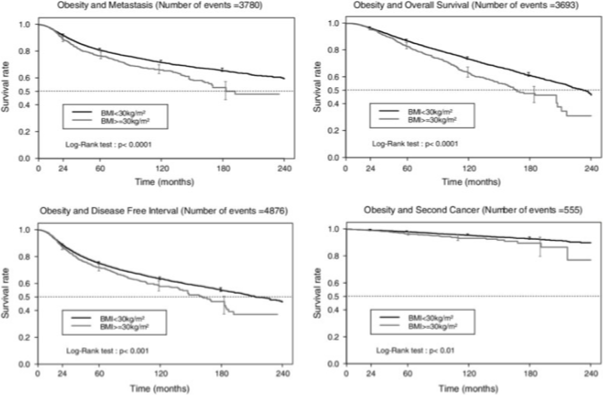
Should we recommend dieting to treat obesity?
Based on the data from the last slide then yes obesity is unhealthy and needs to be helped. Dieting can be uneffective and instead we should be recommending exercise and movement.
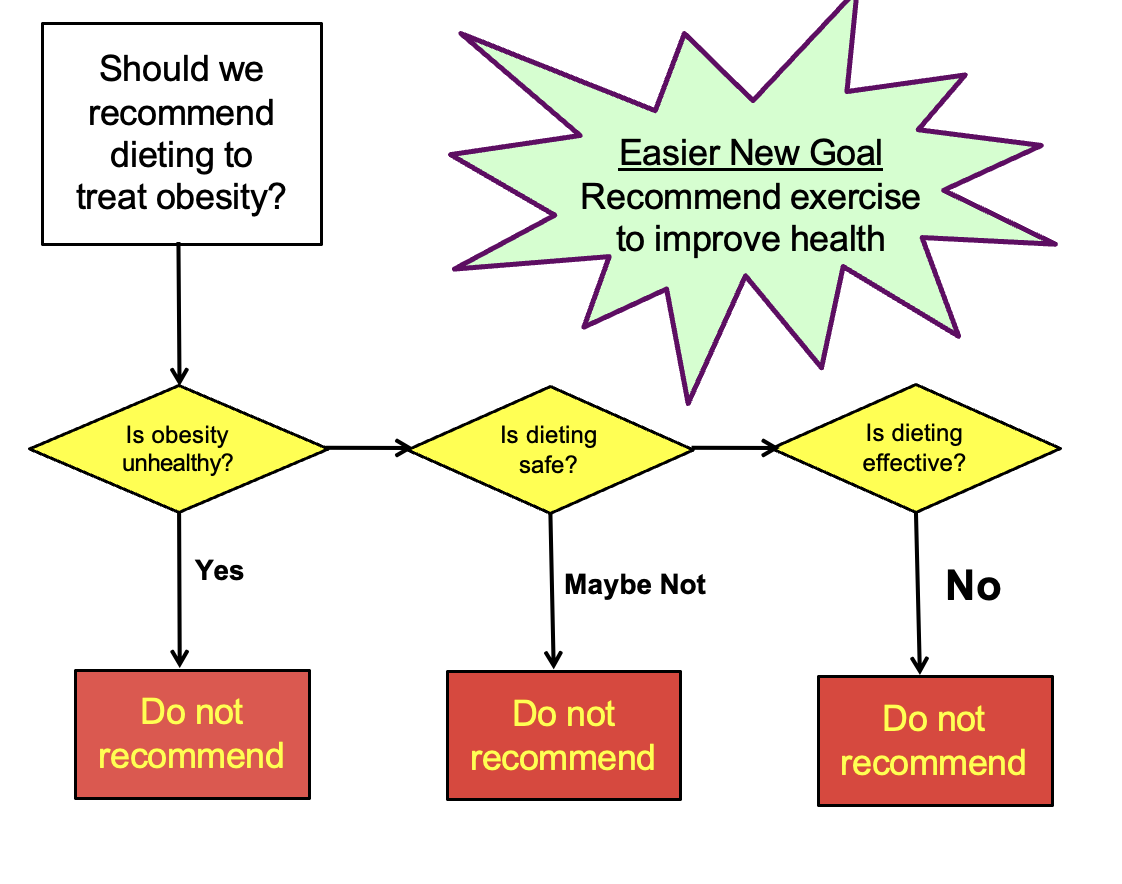
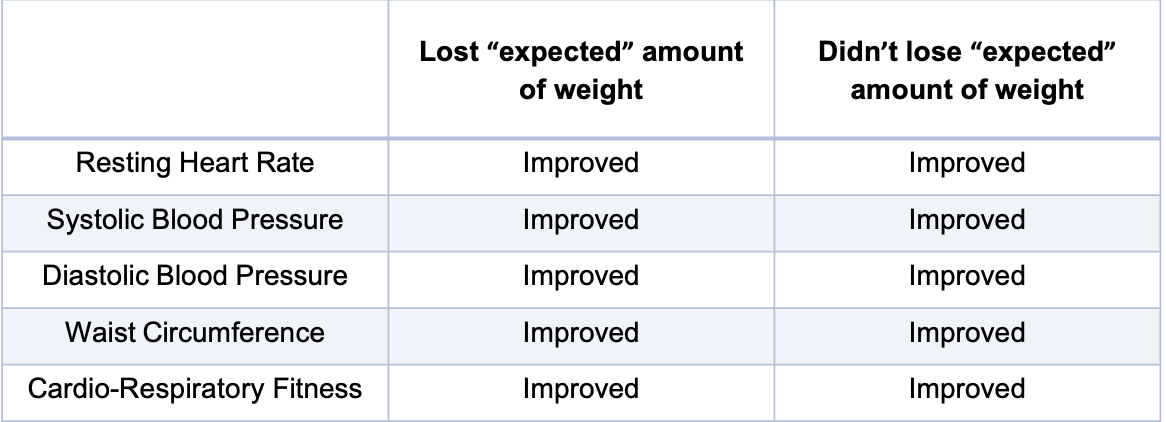
EFFECTS OF EXERCISE ON HEALTH
•Study
–58 obese subjects
–Exercise 5x/week for 12 weeks
–Sessions completed in lab and burned 500 calories
•Average weight loss: 7 lbs
–Some subjects gained, others lost…
The effect of weight loss doesn’t seem to be that dramatic and some even gained weight
•Study
–58 obese subjects
–Exercise 5x/week for 12 weeks @ 70% heart rate
–Sessions completed in lab and burned 500 calories
•Average weight loss: 7 lbs
–Some subjects gained, others lost…
But all of these participants even if they lost weight or not improved their health outcomes. The power of exercise is not about weight loss but improving health outcomes
•Conclusion
•Exercise may not be very effective for losing weight
•But, it can make people healthier by improving many other health-related conditions
WHAT IS PAIN?
•Pain is
•“an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.”
•(The International Association for the Study of Pain)
Not just a physical experience but also emotional,
WHY DO WE HAVE PAIN?
•It provides constant feedback about the body enabling us to make adjustments to how we act and behave.
• Gives a warning sign that something is wrong, resulting in protective behavior.
•It triggers help-seeking behavior.
•It has psychological consequences and can generate fear and anxiety.
Pain can help with seeking behavior (getting hurt and asking family for help, (ex: please get me some water)
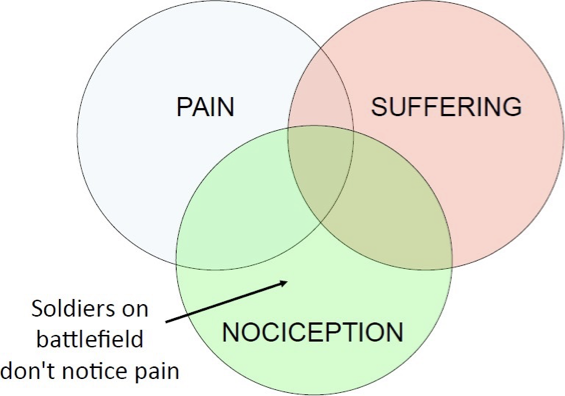
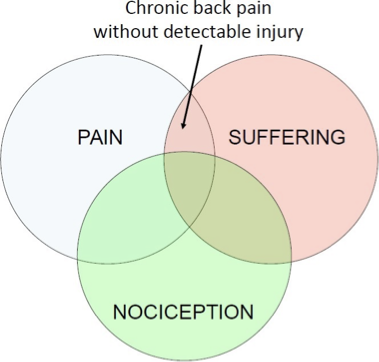
Three concepts of Pain
1.Pain
A conscious experience
–Pain can occur without any detectable tissue damage
–A pain stimulus doesn’t always cause pain
–People can be in pain without exhibiting pain behaviors
–People can exhibit pain behaviors without being in pain
-Sensory and emotional, conscious experience (sometimes when you are asleep you wont feel bad)
-Pain stimulus doesn’t always cause pain (ex: boxing, don’t experience pain much people of anxiety and adrenaline)
-People can be in pain without showing it
-And people can act like they are in pain when they are not (aka soccer players)
2.Suffering
An emotional response
–Suffering can happen in the absence of pain
–Pain can happen without suffering
-Ex: getting a flu shot, the needles are not extremely painful so
-Emotional response
-Ex: lifting weights it painful, will have massive muscle pain but not suffering (some people enjoy it cause it proves they worked out)
3.Nociception(침해수용)/nociceptors(통각수용기)
The collection of signals in the nervous system that are triggered by an injury.
Peripheral (PNS) and central nervous system (CNS) information about the internal or external stimuli, as generated by the activation of nociceptors (통각수용기).
Nociceptors register mechanical (crushing), chemical (poison), and thermal (burns) stimuli.
-Mechanic information, the processing of pain signals in the nervous system simulated by Nociceptors (not equal to pain or even pain signals)
-Pain signal can occur inside of your body (stomach pain)
•What happens to nociception and pain during anesthesia?
•Example:
•general anesthesia (수면마취; 全身麻醉)- nociception without pain
•using a local anesthetic on the site of injury (국소마취): stop all the nociceptive signals arising from it and no pain – no nociception & no pain
General (going into surgery going under while being unconious so they don’t feel pain)
Local (numbing the area but still awake)
Nociception is the body’s detection of pain (feeling something sharp and sending signals to the brain that something is sharp) Alert system
Pain is the feeling or experience that comes after nociception (what you actually experience)
stress-induced analgesia
Extreme stress can block pain
GATE CONTROL THEORY
•It suggests that spinal cord contains a neurological 'gate’:
•First theory to incorporate both the psychological and physiological side of pain
•How pain is transmitted:
– injury -> nociceptors activate and transmit information to dorsal horn (part of spinal cord) -> dorsal horn (척수후각) acts as the gateway
Ex: person finger gets damages nociceptor activates and travels through the nervous system to the dorsal horn acts as a gateway (sometimes open/closed) when open can get to the brain eventually/if closed then wont go to the brain
•What influences whether the gate opens or shuts?
•Factors that close the gate
•Relaxation
•Mental Factors: distraction, meditation, expectations, emotions
•Activity – exercise, massage (배 아플 때 문지르는 행동 등)
When gate is close you won't feel the pain, some ways to close the gate (relaxation, distraction, meditation, expectations (symptom improvement), doing mild exercise can shut down the gate (as a kid stomach hurting and feeling better after massaging)
MYTH #1: INFANTS DON’T FEEL PAIN?
•Previously believed that infants’ nervous systems weren’t fully developed
•However, recent research says:
•Babies do indeed feel pain (e.g., circumcisions)
•They process pain similarly to adults
•Infants still not receiving adequate pain medications
MYTH #2: CHILDREN DON’T FEEL PAIN AS INTENSELY AS ADULTS?
•Yes, they do!
•As indicated by behavioral & physiological indicators
•they may just lack proper expressive vocabulary
•Children also not receiving adequate levels of pain medications
Measure pain level using behavioral and physiological (rate of pain, cordizal (Stress level) in infant babies for pain level)
MYTH #3: PAIN IS A NORMAL PART OF THE AGING PROCESS
•Nope!
•But, because elderly people believe this myth, they are the group least likely to report pain.
•Consequences of underreporting:
•Leads to reduced quality of life
•Increases functional impairment, depression, and sleep disturbance
•Often results in undertreatment, especially in cognitively impaired elders
Elderly people can feel more pain but its not normal
MYTH #4: PAIN ALWAYS HAS PHYSICAL CAUSE
•Nope! Not all pain has a physical cause.
–85% of people with chronic back pain have no identifiable physical cause of the pain
–95% of people with chronic headaches have no identifiable physical cause of the pain
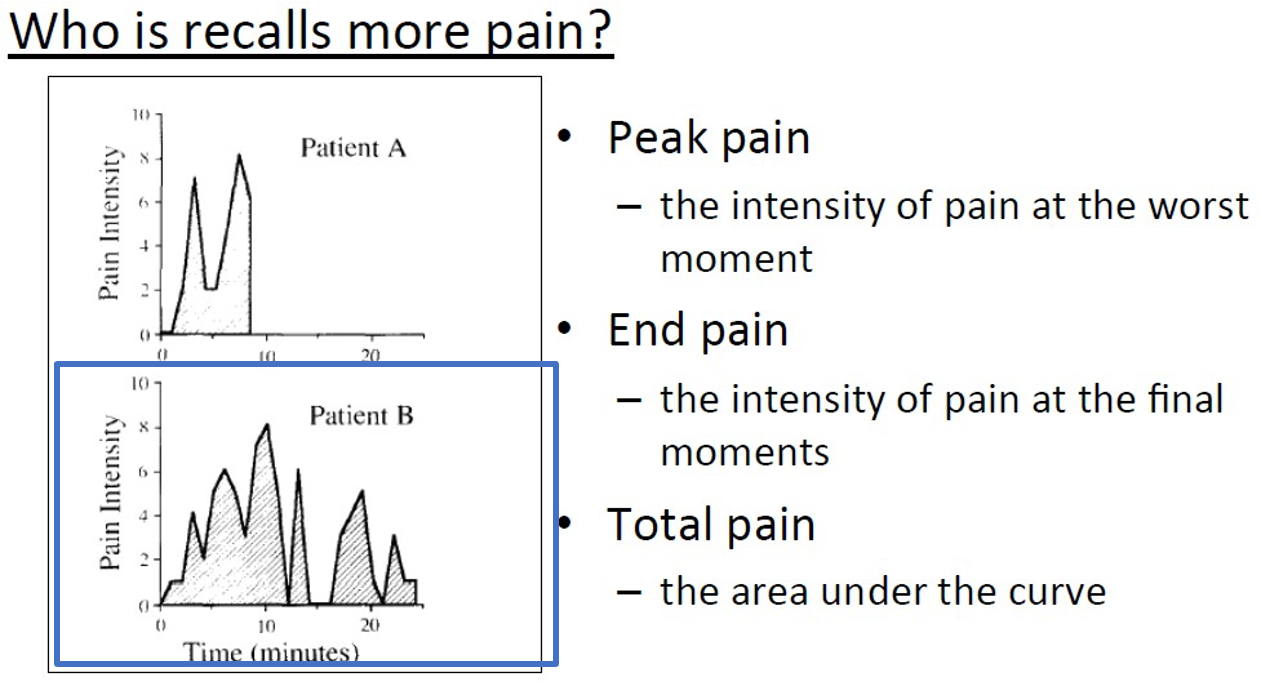
MYTH #5: THE LONGER PAIN ENDURES THE MORE PAINFUL THE MEMORY
•A study of pain and memory (Redelmeier, 1996)
•The investigators recorded in real-time the intensity of pain experienced by patients undergoing colonoscopy (대장내시경) and lithotripsy (신장결석제거술)
•patients' retrospective evaluations of the total pain of the procedure were recorded
The level of pain is not the same as the level of pain remembered
•Results
•Patients' judgments of total pain were strongly correlated with
•the peak intensity of pain
•the intensity of pain recorded during the last 3 min of the procedure
• Lengthy procedures were not remembered as particularly aversive
Study:
-> Memories of pain largely reflect the intensity of pain at the worst part and at the final part of the experience.
Duration was the same (25 mins) the lower the better, higher the worst pain
WHAT HELPS PATIENTS COPE WITH STRESSFUL MEDICAL PROCEDURES?
coping with the procedure itself
Provide description of procedure
what actions will be taken, the timing of actions, and the likely outcomes
coping with the accompanying negative feelings
Relaxation techniques
Describe sensations they may feel and provide training in relaxation
Meditation
Distraction
Distract yourself by focusing on another activity
Distract yourself by focusing on the pain-inducing event, but reinterpret the event
•Study examples
•Distraction/attention/redirection
•Gall bladder surgery study
•Patients randomly assigned to a room with and without windows looking out on a natural scene
=> Patients randomly assigned to a room with windows had shorter hospital stays
•Social support/modeling
•Coronary bypass patients who had the least stress and
shortest stays had roommates who were postoperative (예전에
수술 경험이 있는; didn’t matter what type of surgery)
Ex: Having a roommate who had a similar procedure in the past will help with stress and shortest stay.
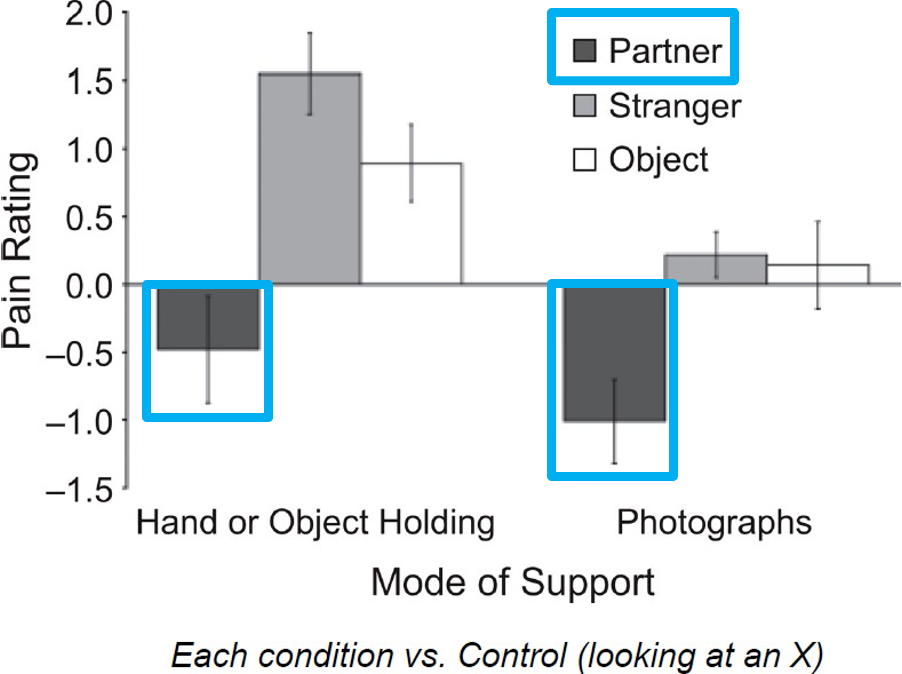
WHAT HELPS PEOPLE COPE WITH BRIEF PAIN?
•Social Support
–Participants completed a heat-pain task 7 times:
•Holding different objects:
–Partner’s hand
–Stranger’s hand
–An object
•While looking at a picture of:
–Partner
–Stranger
–An object
An“X”sign(control condition)
Participants were enduring pain while holding or looking at objects
Just looking at loved ones or holding loved ones can help you cope with pain, highlights the importance of social support
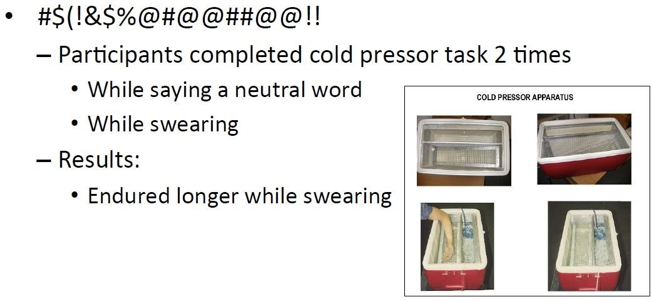
WHAT HELPS PEOPLE COPE WITH BRIEF PAIN? prt 2
Swearing
Participants completed cold pressor task 2 times
While saying a neutral word
While swearing
Results: endured longer while swearing
Cold pressor, one with control word, and one with swearing (lasted longer when swearing)
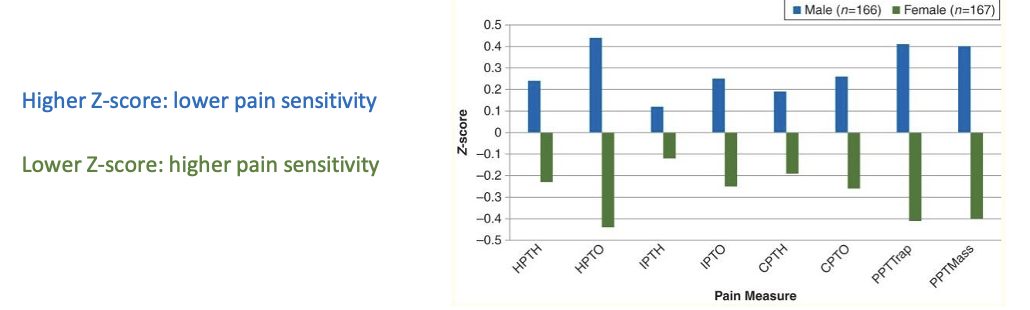
GENDER AND PAIN
•Research evidence suggests that men and women differ in their responses to pain
•increased pain sensitivity and risk for clinical pain – women
•Pain prevalence (유병률/빈도)
•greater pain prevalence among women relative to men
Higher percent of women report to having pain
•Field studies
–Male patients rate intensity of pain as lower than female patients
•Lab studies
–Men tolerate more pain then women
•Summary
•The findings from clinical studies demonstrate that women are at substantially higher risk for many common pain conditions.
What causes a sick person to get better?
1.Natural History:
–The illness runs its course
–
2.Active Treatment:
–Active aspects of treatment (pharmacological, surgical, physical) help the person.
–Taking medication
–
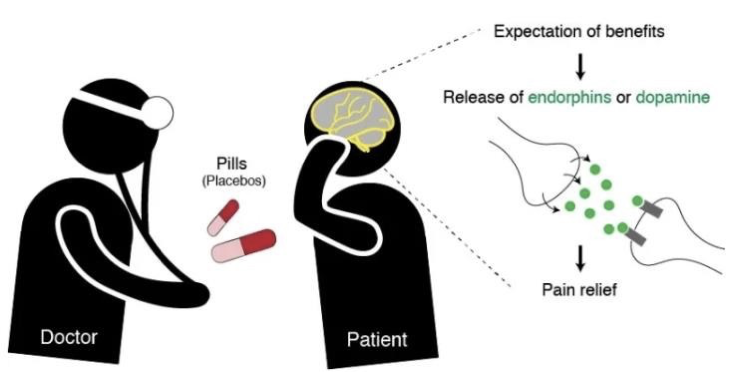
3.Placebo Effects:
–Non-specific aspects of treatment (context, delivery method, thoughts and beliefs) helps the person.
Placebos
•Placebo (위약; 假藥)- inactive substance or condition that has the appearance of an active treatment
•Health research: treatment group (medication) vs. control group (no med) vs. placebo group (placebo)
The purpose of add a placebo is to prove that the medication works better then the placebo
Placebo effects
•Placebo effects
•Any beneficial effects of taking a medicine that cannot be attributed to the treatment itself
–A belief in the effectiveness of a treatment boosts
the treatment’s effectiveness
–Both expectancy and learning can contribute to this
Placebo effects: real-life examples
•Sugar pills:
-use of sugar pills in medical studies is quite common
-Patients are given a sugar pill,
- but they still report feeling better after taking it
•Brand-name medications:
– Brand-name medications often have a stronger placebo effect than generic medications
(복제약).
Researchers would us pills filled with sugar and see how it helps with treatments (many people say they feel better after taking the sugar pills, just the expectation of feeling better makes them feel like the pills worked)
Branded named medication (have a stronger placebo effect even though none branded names are said to work less because the name is not associated with it)
Placebo example: Skin rash study
Subjects were rubbed with non-poisonous leaves
Told it was real poison ivy
Results?
All developed a rash
(Told it was posion but it wasn’t developed a rash)
Subjects were rubbed with real poison ivy
Told it was non-posionous leaves
Results
Non developed rash
Told leaves are non poison but told it was not and they didn’t developed a rash (placebo can also effect physical effects and changes)
3 more examples of placebo effects
1. Placebo acupuncture for irritable bowel syndrome (IBS)
(If giving patients fake acupuncture would work for IBS)
Placebo acupuncture for irritable bowel syndrome (IBS)
•Sham (fake) acupuncture vs wait-list control group
–Sham acupuncture group: Twice a week for three weeks
–Wait-list control: didn’t receive anything
Wait-list Subjects: 28%
Sham acupuncture Subjects: 44%
People in the waitlist control reported 28% of pain relief (natural history, disease gets better without treatment)
Sham reported 44% pain relief (placebo effect)
2.Placebo arthroscopic knee surgery
•Real surgery (sedation + incision + surgery)
•Sham surgery (sedation + incision): placebo group
•Results
–The real surgery group did not report less pain or better function than the placebo group
•Both groups
–regained ability to walk in same time
2 year follow-up: 40%of those in both groups completely recovered
No significant difference between the pain rating or function level between both groups
Placebo morphine with dental surgery
•Participants underwent dental surgery
–Treatment group: received intravenous (IV 정맥주사) drip of morphine
–Placebo group: received IV drip of saline (식염수)
•Results
–Both groups had high levels of pain relief!
History Placebos
•Henry Beecher (1955)
•Observed the effects of placebos on a variety of conditions
•Placebos may be responsible for about 35% of improvements (1/3)
•The degree of placebo effects may differ depending on the types of conditions
Placebo works because of one’s belief and expectation of it working
May differ depending on the conditions
Meta-analysis (메타분석) of placebo studies
•130 Studies with placebo group and control group
–Placebos work for pain
–Placebos work when outcome is measured subjectively
and continuously
–Placebos work for some objectively measured outcomes but not all
•Do we conclude “Therefore placebos don’t work…”?
• Conclusion? Placebos work for certain problems under certain conditions
(objectively measure, blood pressure, heart rate a tool to measure these)
Lots of disorders show placebo effects
•Allergies
•Anxiety/Panic Disorders
•Asthma
•Bipolar/Depression
•Cough
•Crohn’s Disease/Colitis
•Epilepsy
•Erectile Dysfunction
Herpes
•Hypertension
•Irritable Bowel
•Migraine
•Nausea
•Pain
•PMS
•Reflux
Ulcers
Disorders NOT supported by placebo effects
•Cancer treatment
•HIV
•Kidney disease
Blindness or deafness
BUT… do help with side
effects from treatment
What determines if placebos work
1.How the health-care provider behaves
2.Characteristics of the patient
3.Situational factors
Provider behavior matters
Patients given tranquilizer by doctor who expressed:
Confidence: 77%
Doubt : 10 %
Patients with irritable bowel syndrome given:
Nothing: 28%
Sham acupuncture: 44%
Shame accupuncture with a warm and positive doctor: 62%
Sham and warm have a better rates of improvement
Placebo-prone personality?
No data to prove that personality types effect how placebo have a impact on
Situational factors
•Positive > Negative prior experience
•High > Low expectations
•Medical settings > Non-medical
•Complicated instructions > Simple instructions
•Prescribed drugs > Prescribed behavior change
•Yucky tasting pills > Good tasting pills (“Good medicine tastes bitter”)
•Pill Color Matters!
Cool colors: Tranquilizing or sedating
Hot colors: Stimulating
If one has high expectations then it can boost up the placebo effect (better to believe that the treatment will work)
Decrease anxiety (Placebos)
•Decrease anxiety•Decrease anxiety
–Reduce physical symptoms of stress
•Upset stomach
•Diarrhea
•Trouble sleeping
–Not all placebo effects have to do with these things
•Endorphin release
–Endogenous opioids naturally produced by the body
•When you give someone a placebo, their body releases endorphins, which relieve your pain.
–The more believable the placebo, the more likely it is to work:
•In brain imaging study, the more that patients expected the placebo to work, the more brain activity in their opioid receptors.
Endogenous (released in body naturally)
•Expectations
Changes brains activity releasing hormones Endorphins releases pain relief
How do placebos work?
•Prior experience with the drug is not necessary
•A placebo can do the opposite of the active drug
•You don’t typically see placebo effects in the absence of an expectation
WHO IS HEALTHIER: MALES OR FEMALES?
•Mortality (the number of deaths within a particular society; 사망률)
–Lifespan
–Death rates
–Causes
•Morbidity (the # of people who have a disease in a particular population; 이환률) (rate of illness)
–Disability (# of days the person misses work because of illness)
–Hospital usage (How often people go to see a doctor)
–Physician visits (의사 방문횟수)
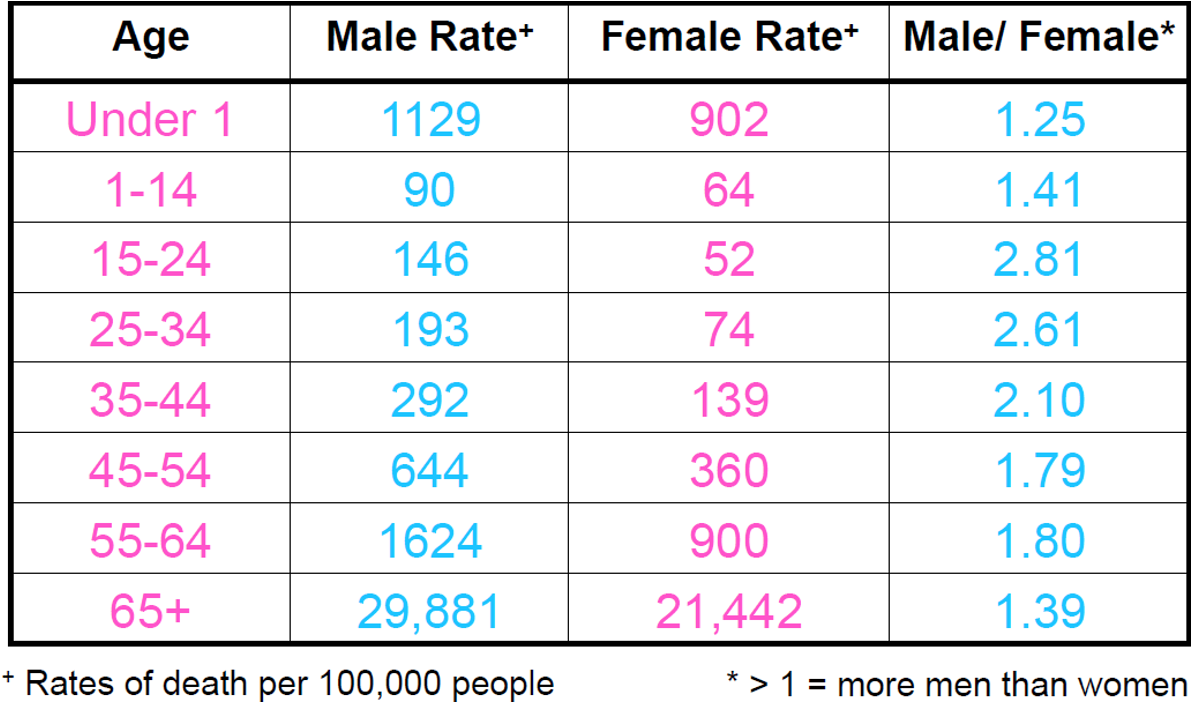
MORTALITY: GENDER DIFFERENCES IN LIFESPAN
Who live longer? Males or Females?
•Females have a longer lifespan then males
•Females live ~ 5 years longer (81.30 vs 76.30)
On average females have a longer life span than males
Greater than 1 men have a higher death rate, across all age groups females live longer than males
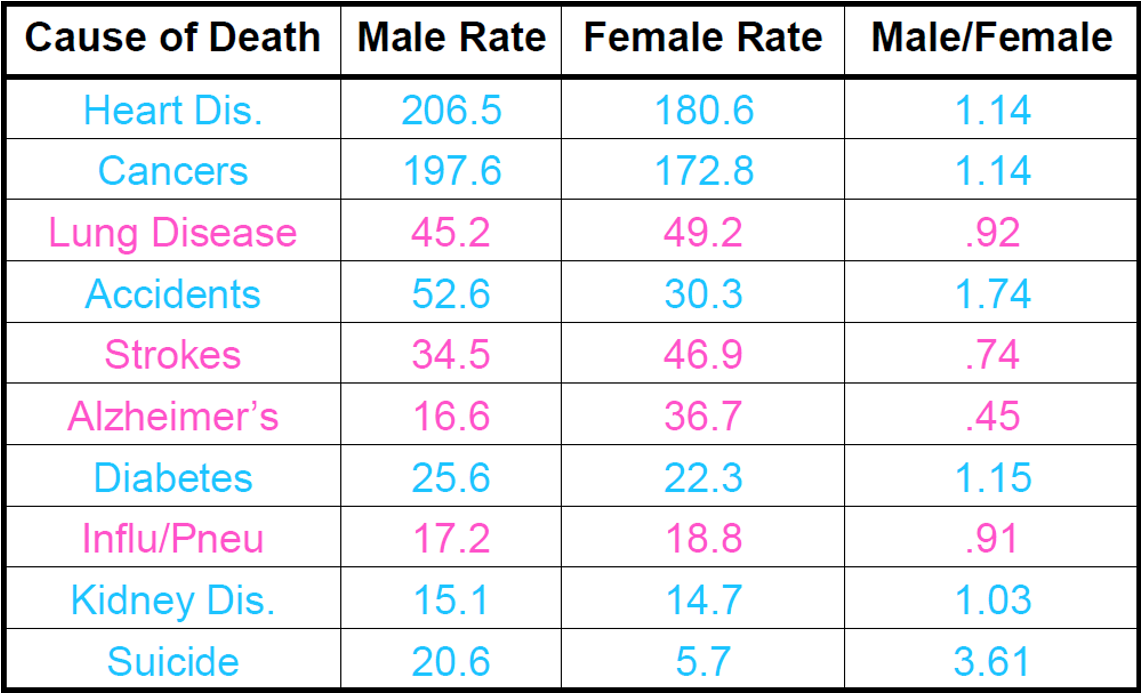
MORTALITY: GENDER DIFFERENCES IN RATES OF DEATH ACROSS CAUSES
Men are mostly to die from heart disease, cancers, accidents, diabetes, kidney, suicide than females.
Females are healthier (Overall females are healthier than males)
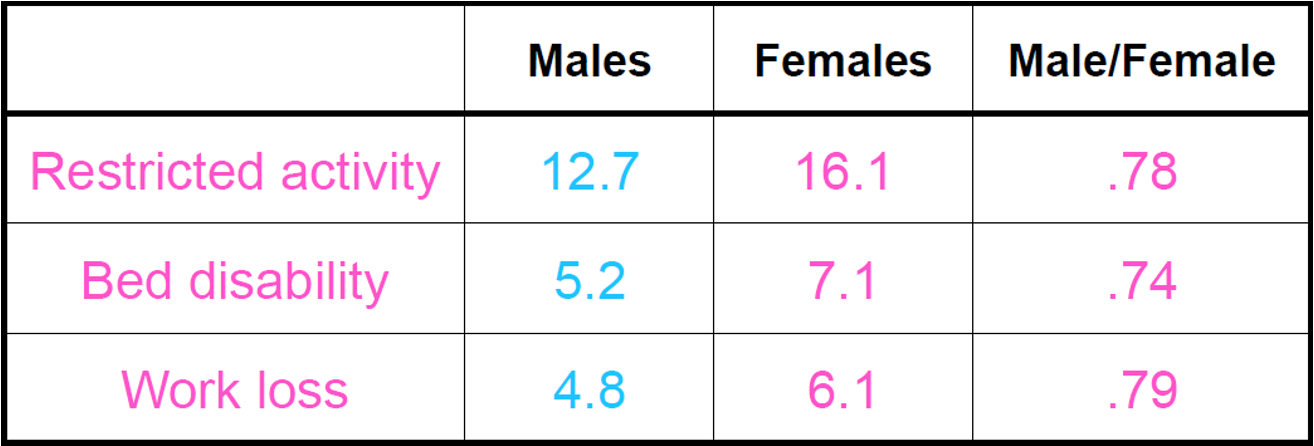
MORBIDITY: GENDER DIFFERENCES IN DAYS OF DISABILITY
Disability bed days were defined as days in which a person was kept in bed for more than one-half of the day due to illness or injury
On average males where not able to do activity or restricted activity at 12.7
But females with 16.1 tend to have more sick days than males (females take more days off due to illness compared to males)
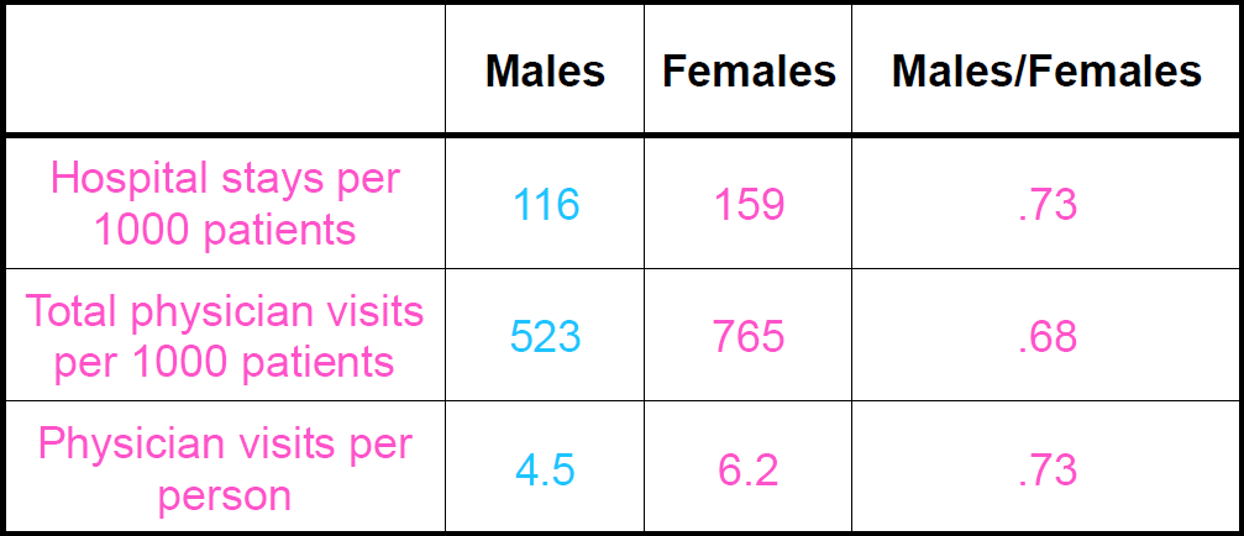
MORBIDITY: GENDER DIFFERENCES IN HOSPITAL USAGE
Males are healthier
Males are healthier with morbidity findings
Mortality and morbidity conflict with each other
HOW CAN WE MAKE SENSE OF THIS?
•Males and females have different pattern of illness:
–Females are sick more often, but with less serious ailments
–Males are sick less often, but with more serious ailments
WHY ARE THERE HEALTH DIFFERENCES BETWEEN MALES AND FEMALES?
1.Biology
2.Health behaviors
3.Utilization of the medical system
4.Social support, stress, and social roles
5.Gender differences in illness patterns
SOURCES OF BIOLOGICAL DIFFERENCES
•Hormone differences (e.g., cardiovascular system)
–Estrogen vs. testosterone
-Estrogen: good for your heart by keeping cardiovascular tissue healthy
-Testosterone: may increase the risk of heart attack and stroke
•Reproductive function
•Higher percentage of body fat in women
=> higher body fat may protect against heart disease death among women
•Body fat is accumulated on different parts of body across males and females => different health outcomes
Its possible that there are hormone differences between genders (estrogen vs testosterone)
Estrogen known to be female hormone (good for heart by keeping cardiovascular tissue healthy)
More body fat in females by protect against heart disease in death among women
Body fat is in different parts of the body (more dangerous to have fat around belly (most men) compared to body fat in hip area (women))
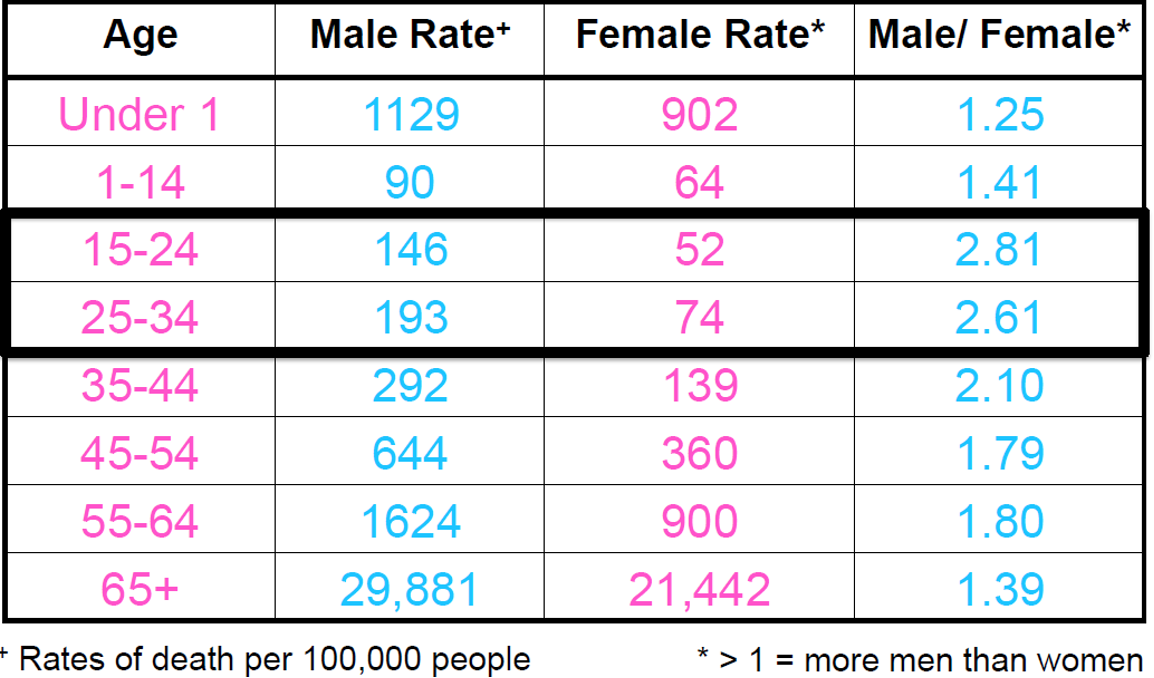
GENDER DIFFERENCES IN DEATH RATES ACROSS THE LIFESPAN
15-24 25-34 (males tend to die at a way higher rate of death than in females)
•Young adult males engaged in more risky behaviors than did females.
•Among youth engaged in health risk behaviors, males reported greater frequency and increases in rates over time for most risk behaviors
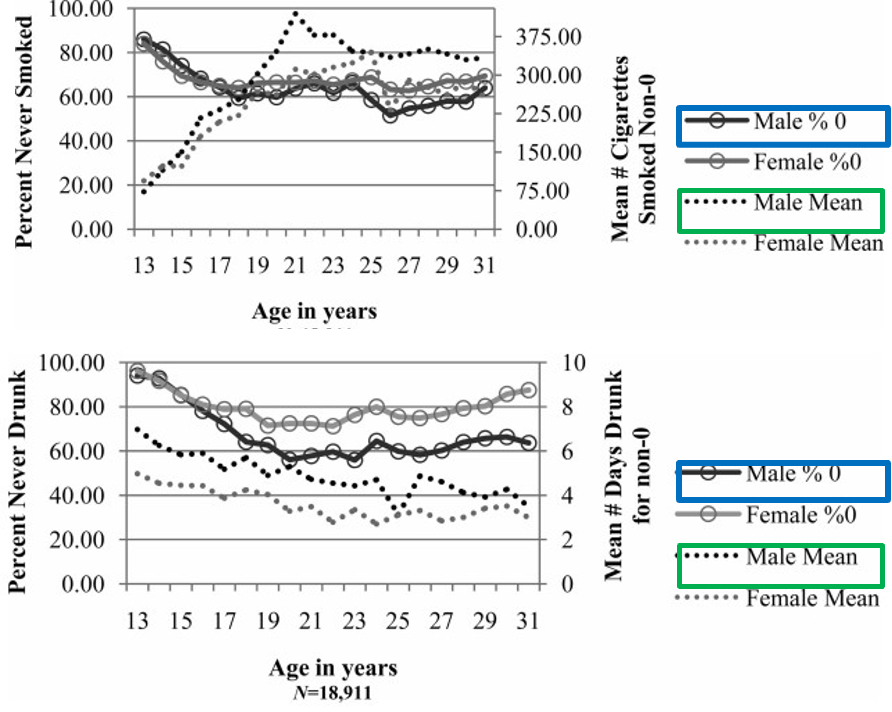
Graph: The left y-axis indicates the percentage of males and females who have never engaged in the behavior
The right y-axis indicates the mean for those males and females who have engaged in the behavior.
Young adult males engage in risky behaviors more then do females
Males have worst outcome, but with the male mean are higher, (more likely to engage in unhealthy behaviors compared to females)
Males have lower percent of never being drunk but male means have a higher days drunk
GENDER DIFFERENCES IN HEALTH CARE UTILIZATION
Why are men less likely to utilize health care services?
•Males tend not admit to being sick (i.e., cultural/gender norms; “Man should
be strong” )
•Males are less likely to notice symptoms (more insensitive to symptoms)
Males are less likely to interact with Dr’s when taking care of kids or elderly
Physician contacts (higher the better)
Possible that males tend not admit to being sick (cultural norms)
Social support, stress, and social roles
Relationship Between Gender, Stress, and Quality of Social Support (Kneavel,
2020)
-Stress: Females > Males
Social support quality:Females >Males
Females have higher stress than males, but reported to higher social support than men
GENDER DIFFERENCES IN ILLNESS PATTERNS
(1)Some illnesses are noticed late in women
–Example: Heart disease
•Considered a “male” disease even though it’s the #1 cause of death for women in the US
•Referred (전원되다) to specialists only 60% as often as men
•With the same symptoms and abnormal tests
-Men are referred for further tests 40% of time
-Women are referred for further test 4% of time
•Consequences: twice as likely to die after coronary artery surgery (females) *low rates of referral due to late detection of heart diseases in females
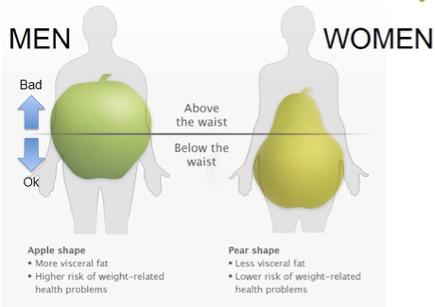
Some factors that are unhealthy in men are assumed to be unhealthy in women
– Example 1: Overweight
•It isn’t how much, but where.
•With obesity:
•Men are exposed to a higher risk of weight-related problems
– Example 2: Cholesterol
•Increases risk of heart disease in men
•Not a clear relationship for women
•Estrogen may be protective (may play as a protective factor from heart disease in females)
AGE AND HEALTH: STEREOTYPES ABOUT AGING
•Mostly negative
–Dependent
–Debilitated (쇠약한)
–Helpless
- Weak
– Cranky
•A few positive
–Wise
–Accomplished
Astute
NEGATIVE AGING STEREOTYPES
•Pervasive in our culture
•Even children know them
•Reinforced constantly
•Likely to be internalized while young
•Stronger than negative stereotypes of any other stigmatized group.
•More powerful than actual experience
AGING SELF-STEREOTYPES
•As people get older they continue to believe aging stereotypes
–They become self-stereotypes.
•In-group preference* not seen for old people:
–Their attitudes toward old people are just as negative as young people’s attitudes toward old people.
*in-group preference: people within each group are favorable to each other
Old people don’t get support from old people as well as young