Parasites and Vaccines
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
Ixodes holocyclus - environment, life cycle, identification
found in coastal QLD, NSW north Vic
prefers warm, and humid weather = Spring-Summer
Host = kangaroos, bandicoots, koalas, possums
only female ticks infect
lay eggs in grass → hatch in 18-28 degrees → 1st host → jump off and grow → 2nd host (become male/female) → 3rd host (only females) → produce toxins on final host → jump off (males then feed off females)
Identification
8 legs clustered at the front of body (1st + 4th leg is darker)
anal groove
colours vary but often grey
Ixodes holocyclus - where and how does it effect host
found on head and neck of patients (looking for CO2)
most likely in skin folds = prepuce, toes, ear canals, trachea
takes 5-7 days from attachment → clinical signs → death in 24-36 hrs
can’t tell how long the tick has been on host
only x1 tick to kill host → find it and remove asap
ticks can’t live without heads
will create tick craters, left once tick is removed
Ixodes holocyclus produce neurotoxin → ascending muscle paralysis
block acetylcholine → release presynaptic neuromuscular junctions
Ixodes holocyclus - clinical signs for host
Ascending paralysis
hind limb → tetraparesis (all limbs → wobbly gait)
palpebral (blink) or change in pupil size
gag reflex and regurgitation → aspiration pneumonia (death)
megaoesophagus (sloppy)
altered voice (more in cats than dogs)
unable to urinate
respiratory paralysis (increased effort/coughing → can’t breath = death)
7 Key effected areas = “Little Bugs Like Stopping Our Little Babies”
legs, bladder, lungs, stomach, oesophagus, larynx, blink
Tick paralysis diagnostics and disease progression
Diagnosis
no actual diagnostic test
clinical signs + tick on pet (may fall off)
rule out other diseases → spinal, GIT, snake venom (bloods to rule out)
response to treatment → antiserum or tick prevention
Disease Progression
5-7 days
Tick Severity scoring = based on weakness (1-4) and respiratory (A-C)
If found tick → monitor closely for 24-48 hours
if in doubt, use antiserum
General treatment of the tick paraysis patient
Sedation
stress → increased RR = increased O2 demand + fatigue
stress → increased risk of regurg/vomit → aspiration pneumonia
Remove tick
removal method does not change outcome - just get it out!
tick clip can help finding others (sedate) - every 4 hours
acaricide spray/bath
Tick antiserum
antiserum = stop symptoms getting worse by neutralise toxins in blood
hyperimmune serum made from canine plasma
slow IV, dilute 50:50 w saline to increase safety, monitor for reaction
if reaction = stop transfusion + fluid bolus ± antihistamines/adrenaline
Oxygen
precaution to avoid hypoxemia (resp paralysis, aspiration pneumonia)
measure with SPO2 (MM + blood), and arterial blood gas
flow by O2, mask, nasal or O2 cage → if severe ventilator
Hydration
no food or drink to protect airways (can go no food 5-7 days)
IV fluid therapy only - maintenance rates only but watch for overload
Antinausea medications
prevent aspiration pneumonia + monitor, keep head elevated,
Ocular Care
unable to blink due to facial nerve paralysis
common to develop corneal ulcers and bacterial infections
stain uptake = antibiotic ointment + lubricate
no stain = prevention + lubricate
Bladder Care
urinary retention due to paralysis
can manual expression or urinary catheter
ultrasound after urination to ensure complete emptying
measure urine in bag = total volume / patient weight / time (mls/kg/hr)
Ventilation
if severe muscle fatigue (low O2, high CO2) paralysis/ aspiration pneumonia
intense nursing care
if ventilation required, at least 1- 7 days with 75% survival rate
Treatment / hospitalisation of Tick Patient
in hospital for 1-14 days
depends on = response to treatment, severity, secondary complications, owner finance
Tick grade = don’t not correspond to prognosis
tick clip to allow thorough search
tick anti-toxin serum
sedation
antibiotics
O2 support or mechanical ventilation
Animals will die from
respiration fatigue
aspiration pneumonia
lack of money for supportive care
Nursing
quiet, limited lights, limited people sedation
reduce stress
ideally sternal, but often recumbent - change position every 4hrs to prevent atrophy and lung collapse
soft bedding
if regurgitating or vomiting, keep larynx high w head down
Physio
passive range of motion
every 4-6 hours for 10-15 minutes
stop if increased stress
When can you discharge a tick patient + prevention?
must be able to stand and ideally walking
have a gag relfex and able to eat as normal
try water trial first → soft food
monitor closely to avoid vomiting and regurgitation
able to urinate
discharge with instructions - strict rest
Prevention
oral chews and tablets or spot on to prevent
manual visual tick search is best
Where is heartworm found - host and environment
dogs are natural hosts but wild variations (dingos) that limits us from eradication, also zoonotic
found in east coast of Australia
only 20% of dogs show clinical signs (resp, lethargy, right sided heart failure) = ideally prevent
Environment
natural disasters
changes in natural climate conditions
online adoption → pet transport
pet owners travelling in infected areas
non-compliance w medications
60 species of mosquitos are known vectors
Lifecyle of Dirofilaria Immitis (Heat worm)
Microfilariae (young heartworm) and antigen detectable in blood by 180 days - 9 months post infection
L1 → L2 → L3 (2 weeks in mozzie - intermediate host)
L3 use proboscis to inject → create hole → migrate to heart/lungs
L4 = prevention products target larvae
topical or oral every month, mixed dose = reduced efficacy
Proheart = every 12 month INJ (previous 3months also)
Immature adults
Adult = 6 months will produce antigens and microfilaria
survive in pulmonary vessels for 90-120 days
live in heart and lungs for 7 years if untreated
30cm in length
can be found on radiograph and ultrasound
damage pulmonary vessels
proliferation and inflammation of vessels → scaring
permeant damage - occurs before antigen tests are positive
How do you test for Heartworm and what are the benefits?
Tests | Benefits |
Microfilaria
|
|
Adults
|
|
Reasons for false negative/positive results for adult heartworm tests
False-Negative Result | False-Positives Results |
|
|
Reasons for positive or negative results when testing microfilaria
Positive | Negative |
|
|
Heartworm Preventative
daily tablets = inconvenient and forgotten
monthly product = available everywhere, sometimes forgotten, can be misinterpreted with what is required
annual injection = 100% compliance as vet is in control (ProHeart)
Preventatives = Macrocyclic Lactones (ML’s)
Avermectins
Selamectin = Revolution
Ivermectin = HeartGard or Exelpet
Milbemycin
Moxidectin = ProHeart INJ, Advocate, Simparica,
gold standard, broad spectrum
protects from birth + can be taylored for vaccination and desexing protocols
best compliance
Milbemycin Oxime = NexGaurd, Sentinel, Comfortis Plus
Roundworm Lifecycle
dogs and cats → pot belly
ingest infected eggs from soil OR eat secondary host OR in utero OR via milk from mother
Pre-patent period = 2-4 weeks
adult worms life in small intestine
Clinical signs = pot belly, but also weight loss, dull coat, vomiting, intestinal obstruction
is zoonotic → visceral and ocular larval infection
eggs passes in faeces and develop over 1-4 weeks in environment
Hookworm Lifecycle
dogs and cats (most common worm) but mostly puppies → anaemia
ingest larvae from soil OR in utero OR via milk from mother OR worms burrow into skin
Pre-patent period = 2-4 weeks
adult worms life in small intestine
Clinical signs = severe blood loss → anaemia, blood diarrhoea, vomiting, weight loss
Is zoonotic → gut infection and cutaneous larval infection
eggs pass in faeces
Whipworm Lifecycle
only dogs (rare) → straining + blood in diarrhoea
ingest infected eggs from soil
Pre-patent period = 10-12 weeks
adult worms life in caecum
Clinical signs = straining to defecate, bloody/mucoid diarrhoea,
not zoonotic
eggs pass in faeces
Tapeworm Lifecycle
dogs and cats → anal irritation / scooting
ingest flea larvae during grooming
Pre-patent period = 2-3 weeks
tapeworms within the flea will develop to adult tapeworms in small intestine
Clinical signs = anal irritation → scooting, segments of worms in faeces
is zoonotic → very minor signs
eggs pass in faeces
Types of Tapeworm
Flea tapeworm
Taenia tapeworm = rodents intermediate → livestock
Hydatid tapeworm = uncooked meat/organs of intermediate → dogs
Hydatids = fluid cyst in liver or lungs of sheep, cattle, people
Sheep measles = cyst in sheep muscle from dog tapeworm
Bladder worms = large cyst in liver/abdomen of sheep from dog tapeworm
Giardia Lifecycle
dogs and cats → diarrhoea
ingest cyst from environment / contaminated water
trophozoites emerge from cyst and attach to mucosa of small intestine
Clinical signs = diarrhoea
trophozoite create cysts and pass in faeces
ONLY treat Giardia if animal is showing clinical signs!
How do you diagnose and treat internal parasites?
Vetscan Imagyst = new microscope equipment than analysis sample and identifies intestinal parasites / eggs
Faecal float
Clinical signs
Treatment - all product specific
Hookworm and Roundworm = 2, 4, 8, 12 weeks, monthly till months, then every 3 months. Before and after pregnancy
Whipworm = 6-8 weeks after 3 months old
Tapeworms = every 3 months
Hydatid Tapeworm = every 6 weeks
Giardia = only treat if infected, treat for 3 consecutive days
Fleas Lifecycle and Characteristics
dogs and cats → itching on back, pelvis, tail = anaemia
eggs (50%) hatch into larvae in environment within 2-5 days
larvae (35%) feed for 5-21 days on adult flea faeces / debris in environment
pupae (10%) develop inside a debris coated silk fibre cocoon
adult fleas (5%)
emerge from cocoon after 3-28 days
feed on blood host = microliters of blood daily = anaemia
mating occurs within 8-12 hours
produce 20 eggs per day = 5000 eggs in life
Characteristics
wingless, laterally flattened with backward projecting spines
move quickly in hair + can jump up to 35 cm
stimulated by physical pressure, CO2 and heat
seek light and move up hair / immediately seek host + feed
Ticks Lifecyle
dogs, cats, humans → anaemia or paralysis
Paralysis tick, Bush Tick or Brown Dog Tick
Eggs hatch
Larvae attach to 1st host = small mammal (rodent)
Larvae falls off and becomes a Nymph
Nymph attach to 2nd host = small mammal, dog, cat, human
Nymph falls off and becomes a Adult
Adult attach to 3rd host = mammal, dog, cat, human
females engorge and feed off blood → produce toxin
lay eggs
Prevention = up to date with tick prevention, checked daily, clincial signs
Ear Mites (Otodectes cynotis)
dogs and cats (mainly younger) → itchy ears
contagious, spread via contact
causes ear infestation = canal inflammation, redness, swelling
clinical signs =
brown waxy/crumbly discharge from ears
pruritis/ itchy
secondary self trauma and yeast or bacterial infections
Demodex Canis Mites (Mange)
just dogs, all ages → patchy hair loss or disease
infected by close contact from infested mother
live and reproduce in hair follicle and sebaceous glands
dogs are predisposed if = specific genetics or immune disorders
all dogs have low numbers of mites
Signs =
patchy hair loss
thickened and pustular skin
can have secondary infections of pruritis
lead to life threatening disease
Sarcoptes scabiei Mites (Mange)
dogs and cats - very itchy skin
tunnel into skin → intense itching → alopecia
usually start at elbow or ear but can travel to ventrum
highly contagious, spread via contact to dogs, cats and humans
if one animal has it, treat all before they develop signs
humans will resolve spontaneously in 12-14 days
Define vaccines and herd immunity
Vaccines
critical to health and welfare
apart of annual visit
educate about preventative health = aid early disease detection
individualised protocol
develop immunity to disease to reduce side effects at re-exposure
can have reactions but they are minor and resolve with time
must be stored cold, and generally not frozen - always record
Herd Immunity
Herd immunity = level of resistance to the spread of a disease within a population
high vaccination rates = increased herd immunity = less disease
What vaccines should be given to dogs and cats?
Dog | Cat |
|
|
|
|
|
|
Horses = tetanus, strangles, equine herpes, Hendra (+ rotavirus if breeding)
How do you create immunity for disease?
Antigens are foreign substances that stimulate an immune response → develop “protective” immune to the whole or element of pathogen
Mechanical immunity = physical barriers (skin)
Non-specific immunity = normal WBC attacking foreign material
Specific Adaptative immunity = develop with exposure
These all the provide either (ideally both)
Humoral immunity = antibodies
Y shaped proteins that recognise and bind to antigen
passive or actively acquired (bodies immune system)
extracellular pathogens
uses Antigen presenting Cells, helper T cells and B cells to create Plasma and Memory cells
Cell mediated immunity = WBC that remember
cytotoxic T cells that recognise antigens on surface of infected cells and destroys them
hard to measure
intracellular pathogens
uses help T cells and cytotoxic T cells to destroy infection
Both of which then assist in pathogen removal and development of memory cells (boosters) = increased rapid immune response
What is mucosal immunity? Where can you get it?
IgM = produced briefly in the blood when immune is first exposure
IgG = long lasting antibodies in blood
IgE = produced in response to allergies and parasites
IgD = in humans
IgA = produced at mucosal surfaces in response to local application of antigens
INJ vaccines = IgM and IgG = systemic immunity (reduce response)
Intra nasal + oral vaccines = IgA = mucosal immunity (stop penetration)
Describe Intranasal vs Oral Vaccines
Intra Nasal | Oral |
|
|
Pros
Cons
| Pros
Cons
|
Describe Injectable Live vs Killed Vaccines
Live Vaccines | Killed Vaccines |
virus/bacteria is alive in vaccine to induce protective immune response but not capable of causing disease | virus/bacteria is killed before administration. May contain an adjuvant to assist into the stimulation of immune response |
Pros
Cons
| Pros
Cons
|
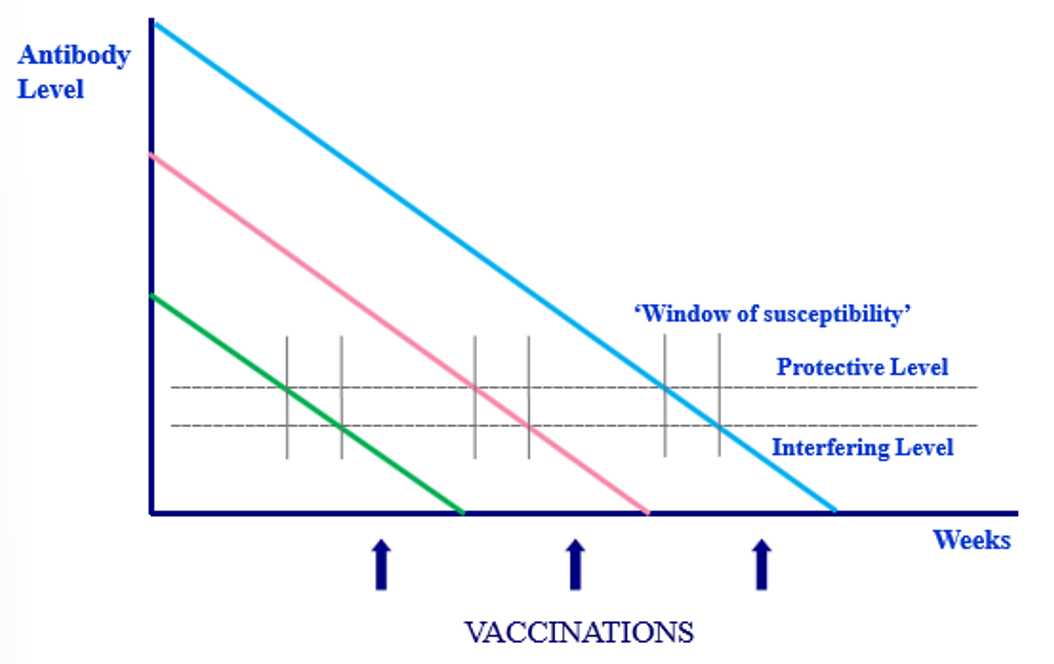
Considerations for Puppy Vaccines
maternal antibodies
protect young animals
last for varying periods
but neutralise vaccines → will only respond to vaccine when low number of maternal antibodies left (hard to measure)
must deliver in the window of susceptibility - hence multiple
at 6-8 weeks, then 10-12 weeks, then 16 weeks, then annual
All core vaccines (C3) need to be delivered before 10-12 weeks
Wil need annual or tri-annual boosters
Parvo vaccine covers all 3 strands of parvo virus