Lab Exam 2: Lung Volume & capicaity | Pulse Oximetry | Urine | Renal Regulation
1/88
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
Spirometer
Measure respiratory volumes & capacities
Obstructive lung disease
Determined by FEV1/VC. conducting zone, cause increased resistance in airways. Rate a person can forcefully exhale is affected so FEV1 will be lower- 70% or lower
Restrictive lung disease
Determined with FEV1/VC. Respiratory zone, reduction in lung compliance, which decreased lung volumes & capacities. Also may be due to loss of lung tissue & scarring in lungs → fibrosis. Still 70%-80% since all volumes lowered
Forced expiratory volume in 1 second-FEV1
Rate at which a person can forcefully exhale air from their lungs in one second
What is the formula for pulmonary ventilation min-PVM?
TV (mL/breath) x BR (breaths/min) = (mL/min)
What is the formula for alveolar ventilation min-AVM?
(TV (mL/breath) - DS (mL) ) x BR (breathes/min) = (mL/min)
Dead space
Regions in conducting zone that do not contribute anything to gas exchange
Tidal volume-TV
Amount of air inhale or exhaled with each breath under resting conditions
Inspiratory reserve volume-IRV
Amount of air that can be forcefully inhaled after a normal tidal volume inspiration
Expiratory reserve volume-ERV
Amount of air that can be forcefully exhaled after a normal tidal volume expiration
Residual volume-RV
Amount of air remaining in the lungs after a forced expiration
Functional residual capacity-FRC
Volume of air remaining in lungs after a normal tidal volume expiration. ERV+RV
Vital capacity-VC
Maximum about of air that can be expired after a maximum Inspiratory effect. TV+IRV+ERV
Why can’t you measure residual volume?
There is not air movement
Why can vital capacity fluctuate?
Due to age or sex. Men and women’s lungs are made to fit their bodies. Men have higher muscle volume than women resulting in higher O2 levels.
What does the pulse oximeter measure?
the level of hemoglobin saturated with oxygen
What characteristic of skeletal muscle cells enables them to efficiently extract oxygen from the blood?
Presence of myoglobin→ oxygen-binding protein that has a higher affinity for O2 than Hb. Allows myoglobin to readily bind O2 from the bloodstream, even when O2 levels are low, ensuring constant supply for muscle activity
Which skeletal muscle fiber type will have the greatest ability to extract the O2 from the blood?
Type 1 skeletal muscle fibers. Rich in myoglobin, higher concentration of mitochondria, extensively supplied with capillaries
What do chemoreceptors detect?
Plasma levels→ increase or decrease in blood levels of O2 and pH
What happens to oxygen levels when they go from the arteries to veins?
Oxygen levels decrease. Arteries carry O2-rich blood from heart to the body, veins carry O2-poor blood back to the heart. O2 levels in blood decrease as it moves from arteries into capillaries and then into veins
Offloading at the capillaries
Substances like carbon dioxide/waste products are released from the bloodstream into the ISF, and then into the capillaries for removal. O2/nutrients are delivered from blood into the surrounding tissues to
What impact does carbon monoxide have on the reading of a pulse oximeter?
Falsely elevate pulse oximeter readings→ cannot differentiate btwn O2 and CO bound to Hb. Resulting in overestimation of true O2 saturation
Why does skeletal muscle extract O2 from Hb in the blood?
Stores it in the form of myoglobin. This stored O2 is used to fuel aerobic respiration→produces energy or muscle contraction. Metabolically active muscles create a steep O2 gradient conc. gradient, driving O2 from blood (higher) into muscle cells (lower)
Type 1 skeletal muscle fibers
Slow-twitch, oxidative. Contract slowly, use O2 & glucose to produce energy. Aerobic. Slow to fatigue, sustain long periods of activity. Posture or endurance activities
Type IIA skeletal muscle fibers
Fast-twitch, oxidative-glycolytic. Contract faster. Aerobic & anaerobic to produce energy. Walking or biking
Type IIB skeletal muscle fibers
Fast-twitch, glycolytic. Fastest contracting fibers. Anaerobic→ breakdown glucose w/o O2. Fatigue rapidly. Intense activity/short bursts, sprinting or weightlifting
Would you expect the erythrocytes in the aortic arch, which is very close to the heart, to have significantly higher O2 saturation than the erythrocytes in the more distant femoral artery?
No, the blood is already fully oxygenated in the aortic arch, and the O2 saturation remains high even in more distant arteries like the femoral artery. Receives oxygenated blood from the aorta
In the pulmonary circuit, which blood vessels contain blood with a higher O2 saturation, the pulmonary arteries or veins?
Pulmonary veins-contain blood w/ a higher O2 saturation bc they carry oxygenated blood from the lungs to the heart
If a person was breathing pure O2 & exhibited hyperoxia with 100% Hb O2 saturation, & a lot of free O2 in the plasma, would the O2 in the plasma be detected by the pulse oximeter?
No, bc the pulse oximeter measures the saturation of Hb with O2, not the amount of dissolved O2 in the plasma
What is the Carbon monoxide (CO) affinity For hemoglobin?
Much higher affinity for Hb than O2, approximately 240 times greater
A blood sample was drawn from the radial (wrist) artery of a pt who was diagnosed w/ pneumonia. The pt’s pulse/HR was high at 102 bpm. Pulse oximetry indicated that the pt had 70%SpO2. Why do the low O2 saturation levels in the systemic blood cause HR to increase?
Low O2 saturation levels in the systemic blood trigger chemoreceptors, leading to activation of the sympathetic NS, which increases the HR to improve O2 delivery to tissues
What are the vascular elements of the nephron
Afferent arteriole. Glomerulus. Efferent arterioles. Peritubular capillaries
What are the tubular of the nephron?
Bowman’s capsule. Proximal convoluted tubule. Descending and Ascending of Henle. Distal convoluted tubule. Collecting duct
Afferent arteriole
Brings blood to the nephrons. Larger diameter
Glomerulus
Fenestrated capillaries where filtration takes place. Start and end w/ arteriole. High BP bc arterioles are high resistance vessels. Fluids and solutes are forced out of the blood throughout the entire length of this
Efferent arterioles
Takes blood away from nephrons. Smaller diameter
Peritubular capillaries
Main site of reabsorption. Low-pressure, porous capillaries adapted for absorption. Cling to adjacent real tubules. Empty into the renal venous system
Proximal convoluted tubule-PCT
Consists of cuboidal cells w/ numerous microvilli & mitochondria. Most material is reabsorbed here automatically (obligatory reabsorption)
Descending loop of Henle
Thin segment correlates with simple squamous cells that allow for water reabsorption
Ascending loop of Henle
Thick segment consists of cuboidal & columnar cells associated w/ electrolyte reabsorption
Distal convoluted tubule-DCT
Consists of cuboidal cells w/o microvilli. Site of more secretion vs absorption. Absorption is under hormonal control (selective reabsorption)
Collecting duct
Receive filtrate from multiple nephrons
Glucose GLU
Must exceed the renal threshold for reabsorption to be detected. This most commonly occurs w/ diabetic pts & occasionally w/ stress
Bilirubin BIL
Excessive amounts of this usually occur in liver disease where there is a failure to properly metabolize it
Ketones KET
Produced by the breakdown of lipids. Most common causes for increased __ values is diabetic ketoacidosis. Less common causes include prolonged fasting, starvation, & low-carb diets
Specific gravity SG
Measured with a refractometer, measures the density of the urine relative to the density of water. Measures the amount of solutes in urine. High salt diet will cause an increase
Blood/Hemoglobin BLD/HGB
Detects heme groups found within Hb and myoglobin
pH
Determined by the kidneys ability to regulate hydrogen ion & bicarbonate concentrations within the blood
Protein PRO
Proteinuria may indicate both renal & nonrenal disease
Urobilinogen URO
The liver converts some of the bilirubin into urobilinogen. If theirs too little, the liver is not waking correctly. If too much, liver disease such as hepatitis or cirrhosis
Nitrate NIT
Caused by bacterial organisms that reduced nitrate to nitrite, indicative of a urinary tract infection/bacterial infection
Leukocytes LEU
Detects the enzyme leukocyte esterase, not individual leukocytes.
Urinometer
Measures the specific gravity of urine. Low SG indicates signs of diabetes or kidney problems
Refractometer
Determines density or specific gravity of a solution
What is chloride concentration and what is the test for?
Using 20% potassium chromate solution added to the urine sample, & adding 2.9% nitration solution, observe a color change that approximates the chloride ion concentration in our sample. Once solution stay reddish brown & does not revert back to yellow, can use drop count to determine chloride ion concentration
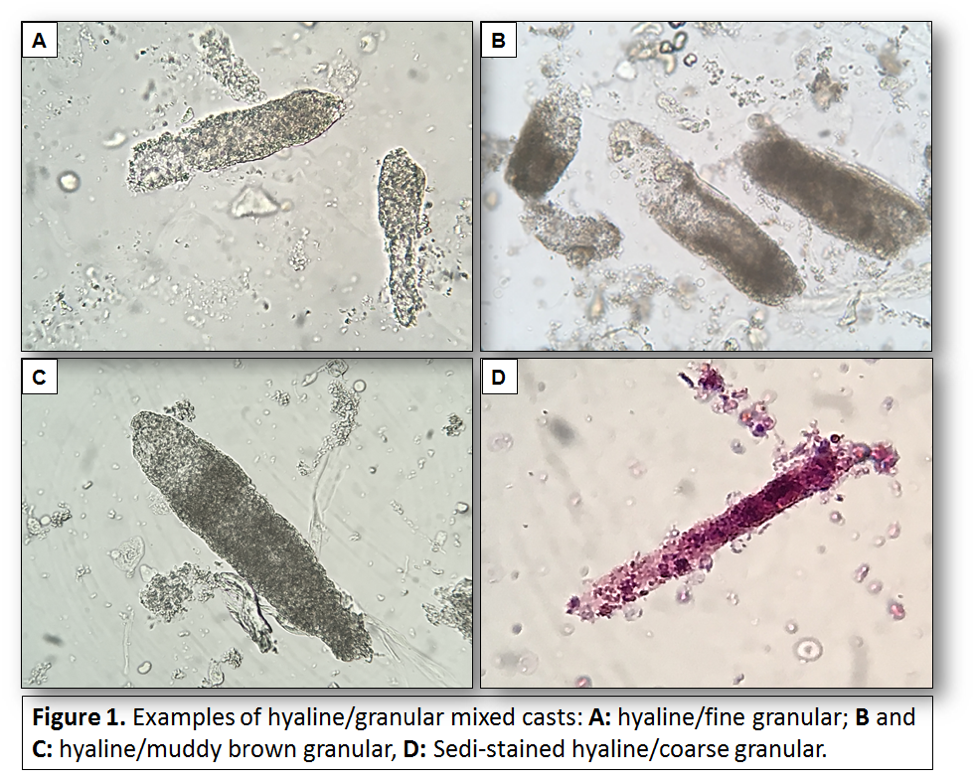
If a urine sediment sample had an elevated number of casts, what does this suggest?
Kidney disease, bc you’re flushing out more than normal
A urine sample tests positive for a high number of WBC, but a sedi-stain shows the WBC are free, not aggregated into a cellular cast. What does this suggest?
Bacterial infection of the bladder
A urine sample tests positive for glucose, but neg for RBC what does this suggest?
Diabetes mellitus
A urine sample tests pos for glucose & very high for RBC. Is this indicative of early stages of diabetes mellitus or nephron damage?
Damage to nephron bc if you just had diabetes you would not see RBCs
Glycosuria
Excretion of glucose in the urine. The filtration rate of glucose exceeds the reabsorption rate in the proximal tubules
Hemoglobinuria
The presence of free Hb in the urine. Indicates intravascular hemolysis, where RBCs are destroyed within bloodstream, releasing Hb into the plasma which is then filtered by the kidneys
Ketonuria
The presence of ketone bodies in the urine. Arises when the body metabolizes fat for energy due to insufficient carb intake, starvation, or uncontrolled diabetes
Proteinuria
Presence of abnormal quantities of protein in the urine, which can be a sign of kidney damage or disease
Bilirubinuria
Presence of bilirubin in the urine. Bilirubin is a breakdown product of heme, & its presence in urine suggests liver disease or biliary obstruction, preventing normal bilirubin excretion
Obligatory reabsorption
The bulk of sodium & water reabsorption occurs in the PCT. This occurs regardless of your state of hydration or sodium levels in blood. Further reabsorption occurs in loop of henle
Selective reabsorption
In the distal tubule and collecting duct, further sodium & water reabsorption occurs may take place, but only under hormonal control. These hormones are selectively released from their source organs when sodium or water levels are low in the ECF
If you eat a diet that is high in salt & low in water, which of the two hormones (ADH or aldosterone) will primarily be secretes?
ADH bc the high salt concentration will cause an increase in osmolarity the hypothalamic osmoreceptors will detect the high osmolarity, signaling he hypothalamus to release ADH to reabsorb water & dilute plasma
The SG of proximal tubule fluid ranges from 1.007 to 1.010. Does this indicate that the body is hydrated or dehydrated?
Hydrated, it secretes more water when the body is hydrated, indicating the kidneys can produce a more dilute urine & effectively eliminate waste products
If the SG of urine is 1.020what caused the filtrate to increase its SG btwn the bowman’s capsule & collecting duct of the nephron?
CD- ADH causes an increase in membrane permeability to water, causing the filtrate to be more concentrated, increasing SG
If you are drinking a beer, how will your urine output & SG of the urine change over a 2 hour period of beer drinking?
Urine output will increase and the specific gravity of your urine will decrease alcohol inhibits the release of ADH preventing water reabsorption since water is not being reabsorbed. The filtrate is dilute, causing a decrease and solute concentration lowering the SG.
Primary active transport
The soluble uses energy to move against its concentration for reabsorption in the nephron.
Primary active transport example
Sodium: I’m the apical side of the endothelial cells, the sodium diffuses down a membrane protein down its concentration gradient (more Na+ In cell then in the ECF). Once it reaches basil lateral side of cell, it gets secreted into the ISF through a Na+/K+ ATPase
Secondary active transport
The solute moves across its concentration gradient with the help of the electrochemical gradient caused by another molecule, moving down its concentration gradient
Secondary active transport example:
Sodium: on the apical side of the endothelial cells, Glucose gets pulled into the cell against its concentration gradient through a symporter protein (SGLT) As sodium diffuse is down its concentration gradient
Normal urine output per day is much less than the daily GFR. Why?
98% of the water being filtered gets reabsorbed back into the body
Give an example of a molecule that is reabsorbed by both selective and a obligatory reabsorption
Water undergoes, obligatory reabsorption, and the PCT and DLOH but is selective in the collecting duct as Reabsorption is controlled by vasopressin
Vasopressin ADH
Targets the CD to increase water reabsorption. Allows insertion of water channels (aquaporins) in apical surface of epithelial cells, increasing water perm
Aldosterone
Targets cells of the DCT and cortical portion of CD; increases reabsorption of of sodium from the glomerular filtrate, returning Na+ to the blood, in exchange for potassium, which is secreted from the blood into the renal tubules
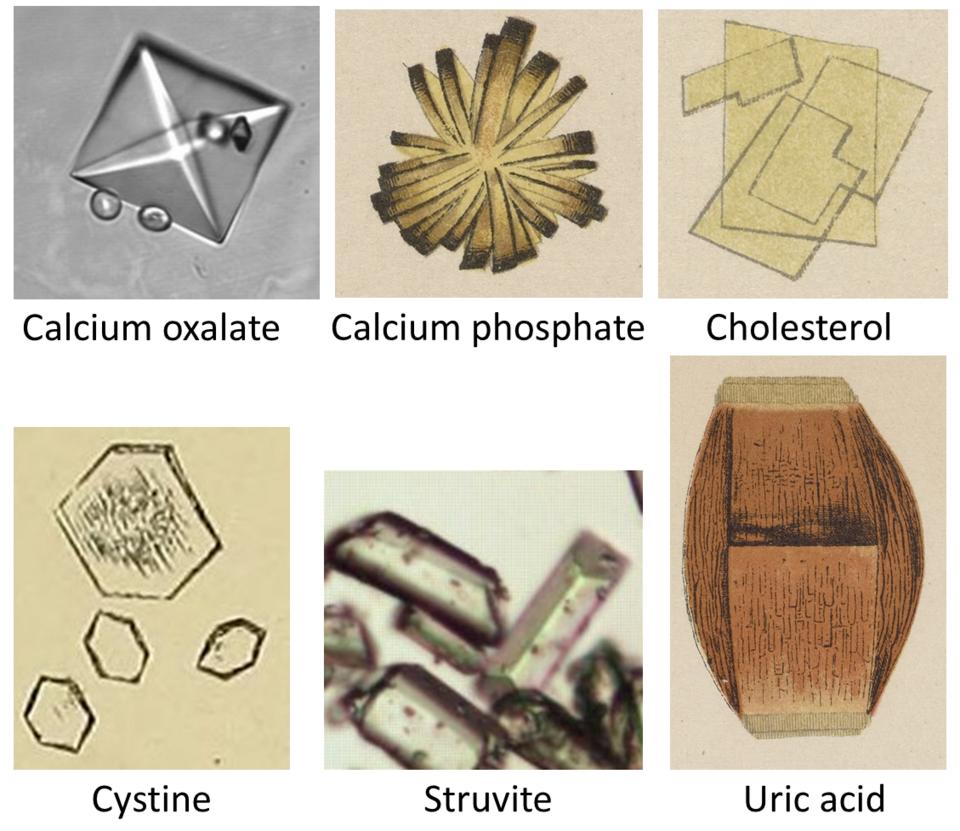
Crystals in urine
Elevated levels caused by dehydration
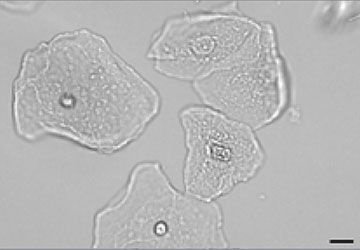
Squamous epithelium cells
Caused by shedding of the epithelium/urinary tract
Casts in urine
Can be made of WBCs, RBCs, kidney cells. Caused by dehydration, low urine flow, strenuous exercise, kidney disease, infection
What is the importance of FEV1/VC ratio?
It is an indicator and an assessing lung function. It helps in differentiate between obstructive and restrictive lung disease.
Using a spirometer, how can you diagnose Obstructive and restrictive pathologies?
If the pts FEV1/VC Is below 0.7 they have obstructive lung disease. This is due to lower FEV1 Levels. If it is 0.7–0.8 they have restrictive lung disease because both values will be lower making ratio look normal.
If an individual undergoes hypoventilation, what effect would this have on the CO2 and pH levels in the extracellular fluid relative to normal conditions?
Increase CO2 levels & decrease pH
How does hyperventilation impact pH relative to the resting condition?
is an increased rate in depth of breathing that exceeds the bodies need to remove CO2, leading to a decrease in CO2 levels and increase in pH (respiratory alkalosis)
How does hyperpnea impact pH relative to the resting condition?
Is an increase in ventilation that is appropriately matched to an increase in metabolic rate resulting in relatively stable CO2 levels in pH compared to resting conditions
What type of breathing results in acidosis?
Hypoventilation
Under what circumstances would you have elevated nitrite levels in the urine?
Bacterial infection of the bladder
Explain why the color of urine is sometimes not a good indicator of hydration levels of the individual?
Factors like food, vitamin medications or medical condition conditions can alter urine colors