Ellis and Associates Lifeguard Training
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
Professional Aspects
* Punctual - Arrive at work ahead of time.
* In proper uniform - Look neat, clean, and easily identifiable as a lifeguard (shirt, hat/visor, sunglasses).
* Prepared - Have the items you need to do the job (whistle, hydration, sun protection, etc.).
* Pleasant - Act cordially to guests and coworkers at all times; smile :).
* Attentive - Keep your eyes on the zone of protection and avoid distractions.
* Vigilant - Maintain your lifeguarding skills at peak performance level (test-ready).
* Knowledgeable - Know and enforce the facility rules.
10/20 protection standard rule
10 seconds to see it and 20 seconds to get to the scene
Distress
Patron who is having trouble
Areas of danger
Glare
Shadows
Exits
Right under chair
Zone of protection
A lifeguard station or position is assigned a specific area of responsibility.
Vigilance
Consistent and careful attention to your zones of protection.
Signs of a guest in distress
*Body position - The body will be at a diagonal or vertical position. Legs are not kicking and arms are extended out to the side. It may look like the guest is trying to reach or grab for something. The guest may have turned toward safety (a lifeguard, a wall, or a lane line).
*Movement - There will be little to no forward movement.
*Appearance - All effort is expended to stay above the water. Eyes may be open or tightly closed. Long hair may cover the face.
*Breathing - In an attempt to breathe, the head will usually be held back to keep the mouth above the surface of the water. The guest is attempting to concentrate only on breathing while on the surface. There may be little to no calling out for help.
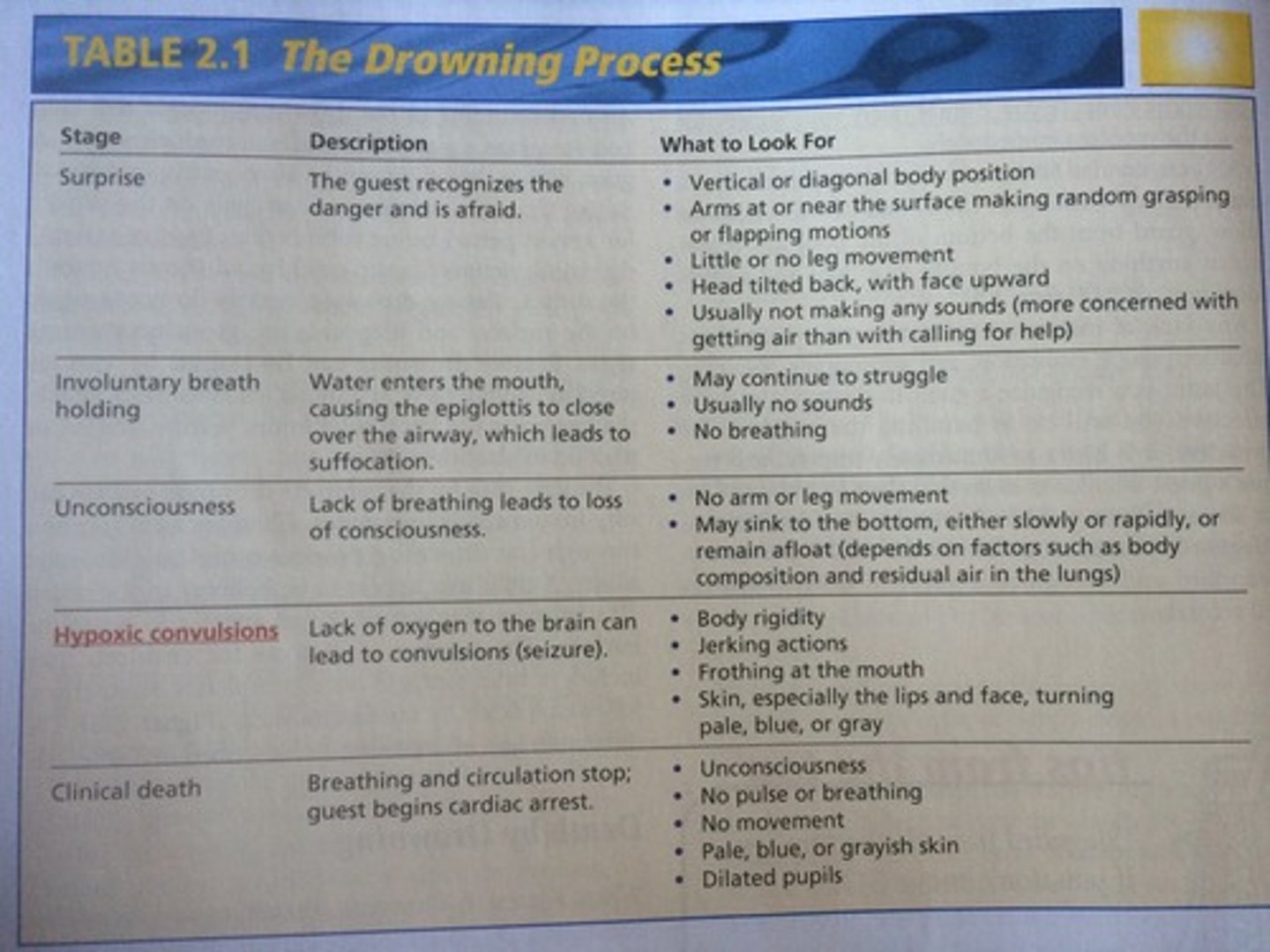
Types of drowning
Active drowning - victim may struggle on the surface of the water for a short period of time before submerging.
Passive (silent) drowning - victims can slip quickly and silently beneath the surface of the water.
The Drowning Process
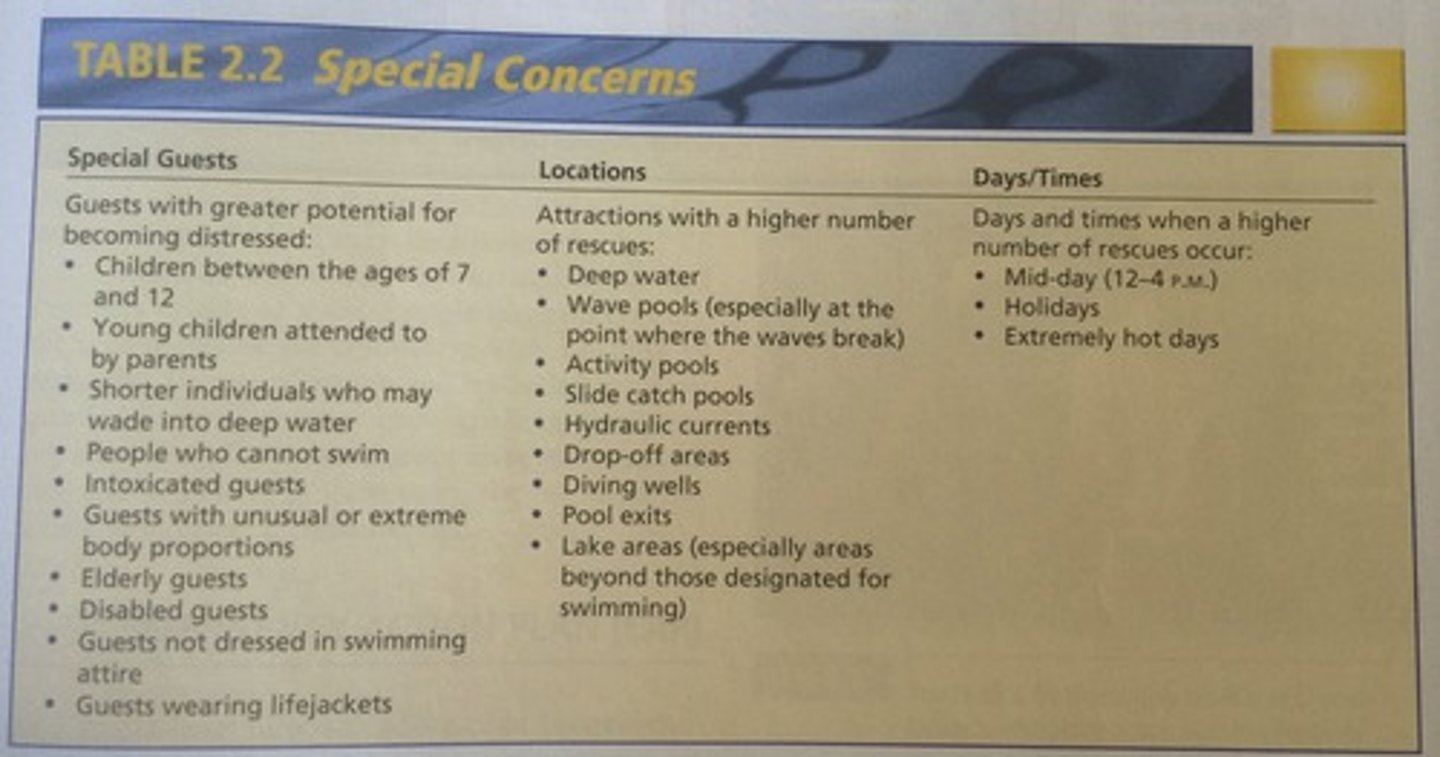
Patrons to pay special attention to:
BSI
Body Substance Isolation (protection) - Self-care, gloves, water
EAP
Emergency action plan
Supplemental responders
staff members
EMS
emergency medical services
One short whistle blast
Get attention of guest(s)
Two short whistle blows
Get attention of lifeguard(s)
One long whistle blow
Activate the EAP
Two long whistle blast
Indicate a major emergency
Hand Signals
*Pointing - Give direction. Can be used with whistle blast to indicate to guest what you would like them to do.
*Raised clenched fist - Help is needed. Can be used with whistle blast.
*Crosses arms above the head - Signal to stop dispatch. Generally used on slides, tube rides, or other water attractions.
*Thumbs up - All is right to resume activity.
*Tapping the top of your head - Signals "Watch my area."
Assist
Occurs when you help a guest, either from deck or water while still being able to maintain zone coverage within 10/20 standard
Rescue
Occurs when a guest would not be able to get to the pool surface or deck without lifeguard intervention. (EAP activated)
Order of a rescue
Whistle
Point
Turn off machines
Jump in
Golden Rule of guest relations:
"Treat guests as you would like to be treated--with respect."
C.A.R.E. philosophy
*Confidence - Maintain an adequate level of personal lifeguarding knowledge and skills, enhanced through appropriate initial and in-service training at your specific facility. Displaying a professional, enthusiastic image gives others confidence in your abilities.
*Alertness - Remain in a constant states of readiness.
*Responsiveness - React in the appropriate manner when faced with an emergency.
*Empathy - Try to understand your guests' needs, wants, and emotions by placing yourself in their position.
D.E.A.L. with difficult situations
*Define the problem - Get a clear understanding of the problem.
Evaluate your options - Examine alternatives, considering the consequences now and in the future.
*Act now - Take action, based on the information you have acquired.
*Look at outcomes - Try to solve the problem to your and the guest's satisfaction. To avoid repeating similar circumstances, see if there is an opportunity for coworkers to learn from this situation.
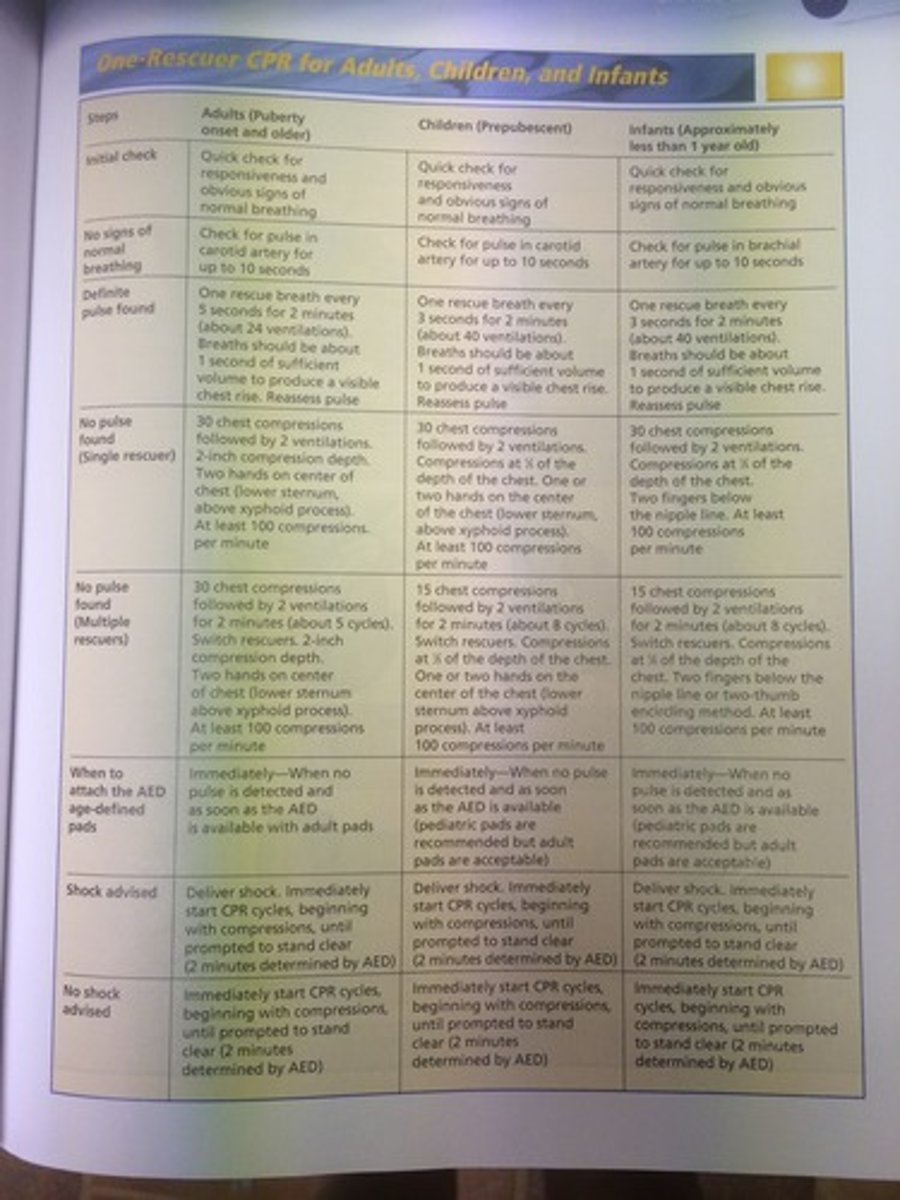
Rescue breaths for adults
1 breath every 5 seconds. Cycle is 2 minutes = 24 breaths.
Rescue breaths for children or infants
1 breath every 3 seconds. Cycle is 2 minutes = 40 breaths.
FBAO
Foreign Body Airway Obstruction
FBAO on Responsive Adult or Child
Perform the Heimlich maneuver:
1. Place fist against guest's abdomen, with your thumb just above the guest's navel.
2. Grasp fist with other hand and press into abdomen using quick inward and upward thrusts.
3. Continue until object is removed or guest becomes unconscious.
FBAO on Responsive Infant
DO NOT PERFORM HEIMLICH ON INFANTS UNDER ONE YEAR OF AGE.
1. Support head and neck, lay infant face down on your forearm and lower arm to leg.
2. Administer five firm back blows between shoulder blades with heel of hand.
3. With continued support, roll baby face up.
4. Firmly give five chest thrusts on infant's sternum, between nipple line.
5. Repeat steps until object is removed or infant goes unconscious.
FBAO on Unresponsive Adult, Child, or Infant
1. 30 chest compressions
2. Open airway and check for foreign object. If visible use finger sweep on adult and child, or pluck object for infant to remove.
3. If invisible, give two breaths
4. Continue chest compressions and breaths until airway is cleared or EMS arrives.
Ventricular fibrillation (V-fib)
Electrical impulses become chaotic and the heart's pump has an incorrect rhythum
Ventricular tachycardia (V-tach)
Heart beats too quickly to pump blood effectively
CPR
Cardiopulmonary resuscitation
AED
Automated external defibrillator
Assessing the Situation
Assess the scene safety first and take proper BSI precautions.
1. Check responsiveness.
2. If guest does not respond, activate EAP to retrieve an AED.
3. If guest is breathing and no spinal injury is suspected, roll into recovery position.
4. If guest is not breathing, check pulse for 10 seconds.
5. If there is a pulse but no breathing, open airway and provide rescue breathing for two minutes, then reassess.
6. If no pulse and no breathing, begin CPR. Reassess every two minutes.
7. Apply AED if available.
8. Continue care until EMS arrives.
Adult, One Rescuer CPR
30 chest compressions - Two breaths
Depth of chest compressions on an Adult
2 inches
Child, One Rescuer CPR
30 chest compressions - Two breaths
Depth of chest compressions on a Child
2 inches (1/3 total depth of chest)
Infant, One Rescuer CPR
30 compressions - Two breaths
Depth of chest compressions on an Infant
1 1/2 inches (1/3 total depth of chest)
Adult, Multiple-Rescuer CPR
30 compressions - Two breaths
Child, Multiple-Rescuer CPR
15 compressions - Two breaths
Infant, Multiple-Rescuer CPR
15 compressions - Two breaths
Flow rate for oxygen tank
15 lpm (liters per minute)
Under what psi should oxygen tank be replaced?
1,200 psi
Fitting sizes for BVMs
15 mm/22 mm
Distance an extricated patron needs to be from the water's edge.
6 feet
AVPU Responsiveness Scale
Alert - Responding appropriately
Verbal - Responding to only loud verbal stimulus
Pain - Responding to only painful stimulus
Unresponsive - Not responding
DOTS Secondary Check
Deformity
Open wounds
Tenderness or pain
Swelling and discoloration
SAMPLE
Signs or Symptoms
Allergies
Medications
Past Pertinent History
Last intake (food or water or drugs?)
Events leading up to
Heart Attack
- Signs:
Chest pressure or pain that last more than a few minutes, and may spread to shoulders, neck, jaw, or arms, Breathing difficulty, Dizziness, Sweating, Nausea, Fatigue
- Care:
1. Activate EAP
2. Make guest comfortable
3. If guest has prescribed meds, assist with use
4. Provide 1 regular aspirin or 4 chewable aspirin if available.
Stroke
- Signs:
Weakness or numbness on one side of the body, Vision problems, Problems speaking, Dizziness or loss of balance, Confusion, Sudden severe headache
- Care:
1. Activate EAP
2. Make guest comfortable
3. If vomiting occurs, roll guest into side (recovery position)
Heat Emergencies
Heat cramps, heat exhaustion, and heat stroke.
- Signs and symptoms:
Muscle cramps (common in legs and abdomen), Dizziness, Nausea/vomiting, Fatigue, Severe headache, Extreme thirst, Hot skin (either wet or dry), Rapid pulse, Mental confusion (including unconsciousness), Seizure
- Care:
* Have guest stop strenuous activity and rest in a cool location.
* Remove any heavy or restricting clothing
* Provide cool water or sports drink (about half a glass every 15 minutes) if guest is alert and not nauseous
* Gently stretch affected muscles if heat cramps are suspected.
* Apply cool, wet towels or sheets.
* Put ice packs at armpits, groin, or sides of the neck if guest has a decreased level of consciousness.
* If condition does not improve quickly, activate EAP.
Cold Emergencies
Hypothermia.
- Signs:
Uncontrollable shivering, Confusion, Sluggishness, Cold skin
- Care:
1. Move guest out of the cold and make guest comfortable
2. Replace any wet clothing with dry clothing, covering guest's head, and insulating guest with towels or blankets.
3. Provide warm, sugary beverages if guest is alert and able to swallow
4. Seek medical attention if condition is severe.
Fainting
-Signs or Symptoms:
Nausea, Weakness, Chills, Abdominal pain, Dizziness, Headache
-Causes:
Hyperventilation, Hypoglycemia (low), Heart problems, Dehydration, Blood loss, Psychological stress
-Care:
*Have guest lie down on flat surface. If guest has already fainted, look for signs of head or spinal injury and treat.
*Check responsiveness, breathing, and pulse.
*If guests vomits, roll and suction.
*Loosen restrictive clothing
*Activate EAP
Seizures
-Signs or Symptoms:
Abdominal sensations, unusual behavior, muscle rigidity, or altered levels of consciousness
-Causes:
Drug overdoes, Hypoglycemia (low), Fever, Head Injury, *Infection
-Care:
*Protect guest from injury. Move objects that might cause injury.
*Roll guest into recovery position to keep airway clear.
*Place thin, soft object between guest head and floor.
*Activate EAP
Shock
-Causes:
Injury from blood loss, Fluid loss (severe vomiting, diarrhea, or burns), *Severe allergic reaction (anaphylaxis) to offending agent, chemical, or toxin
-Signs and Symptoms:
Anxiety, Cool, pale, moist skin, Rapid breathing or difficulty breathing, Rapid pulse, Weakness, Hives, itching, and swelling
-Care:
*Place guest on back as long as no difficulty breathing. If unresponsive and vomiting place in recovery position
*Maintain normal body temperature
*Provide oxygen
*Determine if guest has medication for allergic reactions, help guest self-administer
*Activate EAP
Diabetic Emergencies
**Hypoglycemia (low blood sugar)
-Signs and Symptoms:
Sweating, Rapid pulse, Shakiness, dizziness, weakness, Decreased coordination, Difficulty concentrating, Blurred vision, Headache, Trouble performing routine tasks
**Hyperglycemia (high blood sugar)
-Signs and Symptoms:
Dry, parched mouth, Extreme thirst, Frequent urination, General weakness, Fruity breath, Nausea and vomiting, Abdominal pain, Deep, rapid breathing
-Care:
*For conscious guest who are able to swallow, ask to describe specific treatment needs and provide foods that contain sugar.
*Unresponsive guest, activate EAP
Asthma Attacks
-Causes:
10/3 protection standard
A lifeguard has 10 seconds to complete scan and recognize that a guest is in distress.
Should guest in distress become submerged, the lifeguard(s) should complete a bottom search of the entire zone and ultimately recover the guest within 3 minutes.
CPR CHART
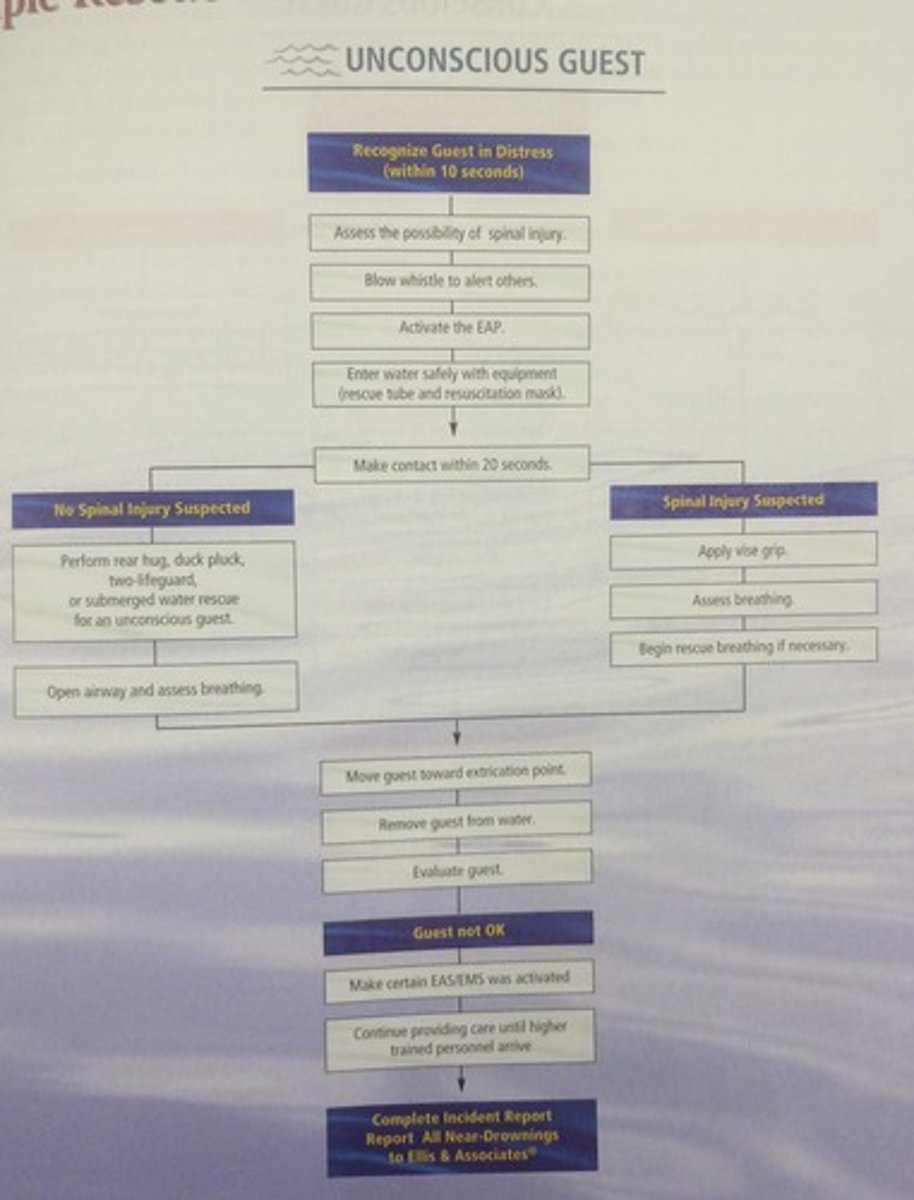
Flow chart of an unconscious guest
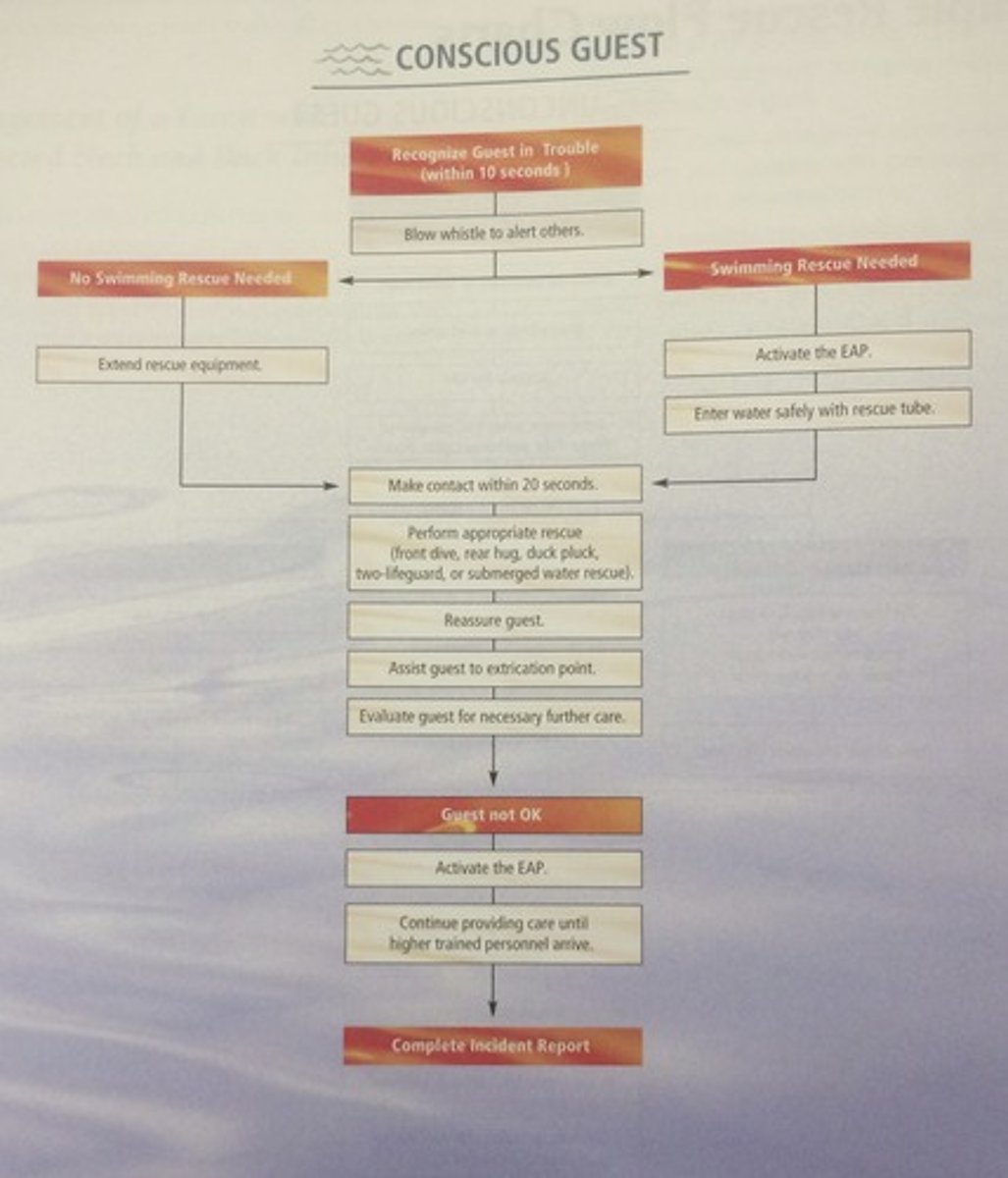
Flow chart of an conscious guest