Cardiac Physiology
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
Components of Cardiac Conduction System and their Role
SA Node
Natural pacemaker of the heart
Starts the action potential
AV Node
“Backup pacemaker” in a sense
SA node AP hits AV node, but there is a bit of a pause before the AV node passes the signal along
Bundle of His (Atrioventricular bundle)
A tunnel through the fibrous skeleton
Contains right and left branches
Sends signals from the AV node to the purkinje fibers
Purkinje Fibers (Subendocardial Conducting Network)
Transfer signals to the myocardium
Cardiomyocytes structure and nuclei and Interclated Discs, Desmosomes and Gap Junctions
Cardiomyocytes are striated, branched and contain 1-2 nuclei
The sarcolemma of cardiomyocytes contains irregular thickenings called intercalated discs. These fit the myocytes together like puzzle pieces
The intercalated discs contain desmosomes (half on each neighboring cell) which help the myocyte stay connected and gap junctions which transfer AP's like a straw.
The muscle fibers connect to the fibrous skeleton of the heart, and swirl diagonally around the heart. This makes each contraction look like the heart is being "wringed"
Action Potential in Individual Cardiomocytes (3 Phases)
Depolarization Phase: Sodium entry via fast voltage gated Na+ channels
Plateau Phase: Na+ gates close. Ca+ starts to influx via slow voltage gated calcium channels while potassium effluxes
Repolarization Phase: Closure of Ca+ channels. More K+ channels open leading to more K+ outflow.
Signifficance of Refractory Period
Refractory period lasts longer than muscle contraction, preventing tetany
P Wave, P-Q interval, QRS Complex, S-T segment, T Wave
P Wave: Depolarization of atrial contractile fibers
P-Q Interval: Atrial Systole
QRS Complex: Depolarization of ventricular contractile fibers
ST Segment: Ventricular Systole (including isovolumetric contraction)
T Wave: Repolarization of Ventricular Contractile Fibers
After T Wave: Ventricular diastole (Including isovolumetric relaxation)
Note: Atrial repolarization overshadowed by QRS complex
Phases of Cardiac Cycle (5 Physical Phases)
Atrial Contraction: Atria Contracts
Isovolumetric Ventricular Contraction: Ventricle contracts to try to be higher than aortic pressure
Ventricular ejection: Ventricle wins! Blood ejected out of ventricle
Isovolumetric Relaxation: Aorta closes and ventricle relaxes without being filled
Ventricular Filling: Ventricular pressure drops below atrial and ventricle begins to fill
Cardiac AP, Mechanical Events (Cycle), Heart Sounds, Ventricular P & Vol., Aortic P
SA node fires > P wave > Atrial Contraction > Dub Sound > Ventricular volume at peak and pressure increases
AV node fires and sends it down the subendocardial conducting network > QRS Complex> Isovolumetric ventricular contraction followed by contraction > Lub Sound > Aortic and Ventricular Pressure peaks and falls > Ventricular volume falls
T wave > Ventricular repolarization > No sound > Isovolumetric ventricular relaxation followed by ventricular filling > Ventricular volume increasing while aortic and ventricular pressure decrease
Stroke volume Equation
SV = EDV – ESV
EDV Normal Values
120-130. This is the peak ventricular volume
ESV Normal Values
50-60. This is the lowest ventricular volume
What is Stroke Volume
SV = mL/beat. How much blood the heart moves in one beat
Cardiac Output Equation w/ values
CO (5.25L/min) = HR (70 bpm) x SV (70mL/beat)
3 Factors Affecting SV
Preload: The degree of stretch of the heart before contraction. Proportional to EDV.
Frank-Starling Law (More Stretch = More Contractility. Works within limits)
Factors affecting Preload (HR, Venous Return)
Contractility: The strength of a contraction at any given preload. Directly related to cytosolic calcium levels. Positive inotropes (epi, thyroxine) increase contractility. Negative inotropes (hypoxia, acidosis) decrease contractility
Afterload (Arterial BP): The pressure the ventricles must overcome before the semilunar valves open. Affected by BP and vessel structure
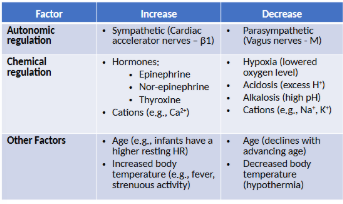
Factors Affecting HR