NUR221: FINAL EXAM, Anti-Cancer Meds
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
activating cancer-causing oncogenes and inactivating tumor suppressor genes (genes that prevent replication of cells that have become cancerous)
How does cancer become malignant?
initiation, promotion, progression
What are the three stages that occur with malignant transformation?
cytotoxic agents -> used most often (chemo); hormones and hormone antagonists; targeted drugs
What are all of the drug classes of anti-cancer meds?
where the cell prepares to make DNA
The Cell Cycle:
What occurs during the G1 phase?
where the DNA is made; DNA synthesis
The Cell Cycle:
What occurs during the S phase?
preparing for cell division/mitosis
The Cell Cycle:
What occurs during the G2 phase?
actual cell division -> two daughter cells
The Cell Cycle:
What occurs during the mitosis phase?
ratio of dividing cells to resting cells
What is growth fraction?
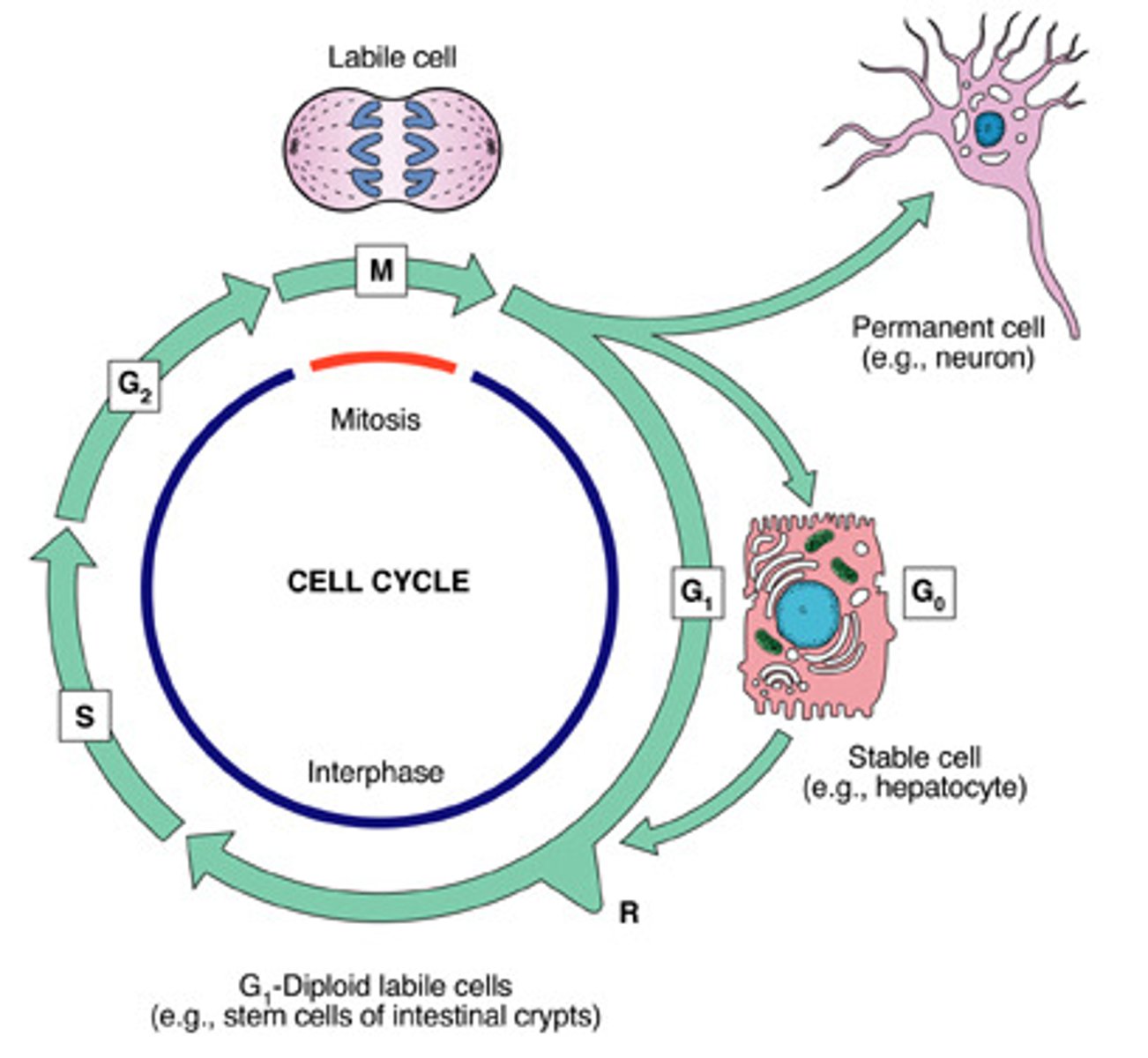
tissues with a large percentage of dividing/proliferating cells and few resting cells
What would define a HIGH growth fraction?
tissues with mostly resting cells (not dividing)
What would define a LOW growth fraction?
tissues with high growth fraction -> cytotoxic agents more active against dividing cells; where chemo side effects are seen
What kind of growth fraction is chemotherapy more TOXIC to?
disrupt DNA synthesis and mitosis; hair, bone marrow, GI lining are highly impacted
What do cytotoxic agents do?
breast, lung, prostate, and colon cancer have low growth fraction and don't respond to chemo as well as acute lymphocytic leukemia, Hodgkin's disease
Obstacles to Successful Chemo:
What should be known with the cancer's response to chemo?
lacks selective toxicity to cancer cells
Obstacles to Successful Chemo:
What should be known with the dose-limiting toxicity to normal cells?
one cell can proliferate and cause relapse; chemo is systemic
Obstacles to Successful Chemo:
What should be known with cure requires elimination of every malignant cell?
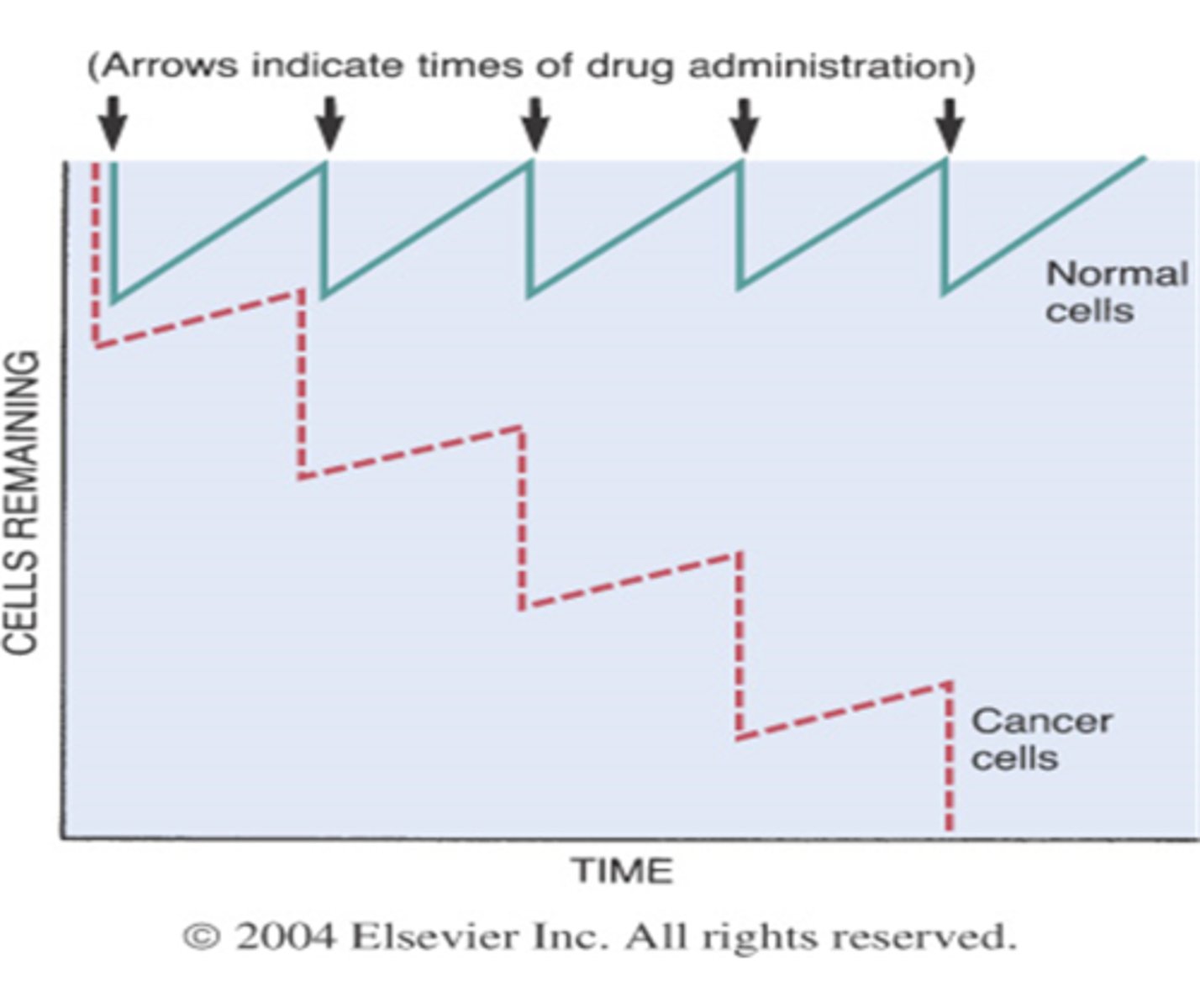
at any given dose, drug will kill constant percentage of malignant cells regardless of how many cells are actually present
Obstacles to Successful Chemo:
What should be known with the kinetics of drug-induced cell kill?
cancer cells have same surface antigens as normal cells; anti-cancer drugs are immunosuppressants; immune system might be compromised of cancer itself
Obstacles to Successful Chemo:
What should be known with anti-cancer meds receive little help from host defenses?
smallest detectable cancer is 1cm, but it contains about 1 billion cells
Why are screenings and early detection so important with cancer diagnosis?
normal cells must repopulate faster than cancer cells
In order for INTERMITTENT chemotherapy to work, what has to occur?
suppression of drug resistance -> low probability of developing 2 or more mutations
What is the 1st benefit of combination chemo?
increased cancer cell killing -> different MOA; one may kill in mitosis, one may kill in synthesis
What is the 2nd benefit of combination chemo?
reduced injury to normal cells -> avoid overlapping toxicities
What is the 3rd benefit of combination chemo?
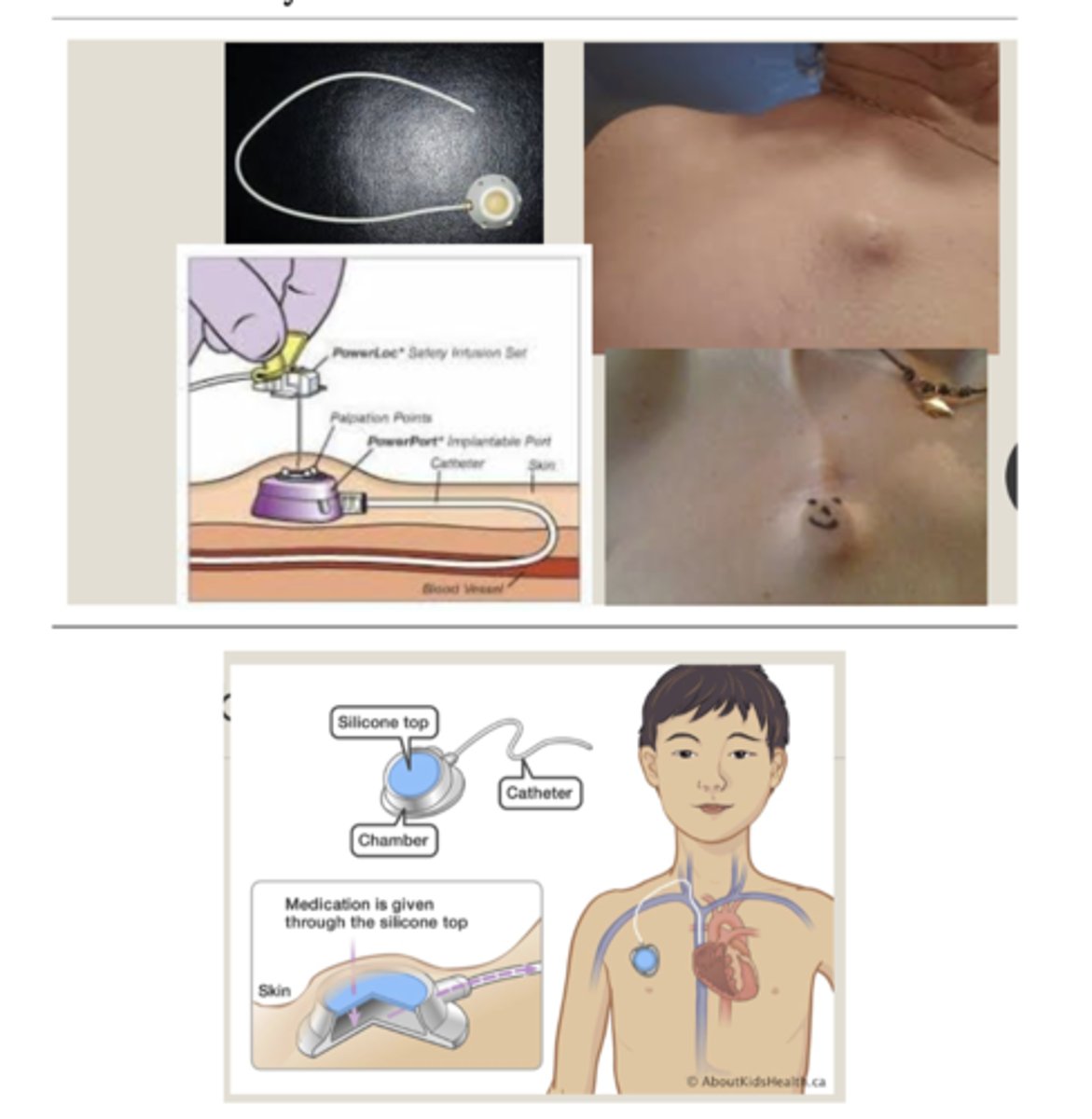
central line or port; very damaging to peripheral vessels -> increasing pain and side effects (if vein ruptures or infiltrates, it's going to kill all of the cells around it)
How is chemotherapy delivered?
2500-7000; less than 500 leads to neutropenic precautions
Bone Marrow Suppression:
What are the normal levels of neutrophils in the body?
150,000-450,000; bleeding precautions if low
Bone Marrow Suppression:
What are the normal levels of platelets in the body?
stomatitis; N/V; alopecia
What are all of the side effects of chemotherapy?
inflammation of oral mucosa -> can go all the way through GI tract; develops within a few days, can persist for 2 weeks post-treatment
Side Effects of Chemo:
What is stomatitis?
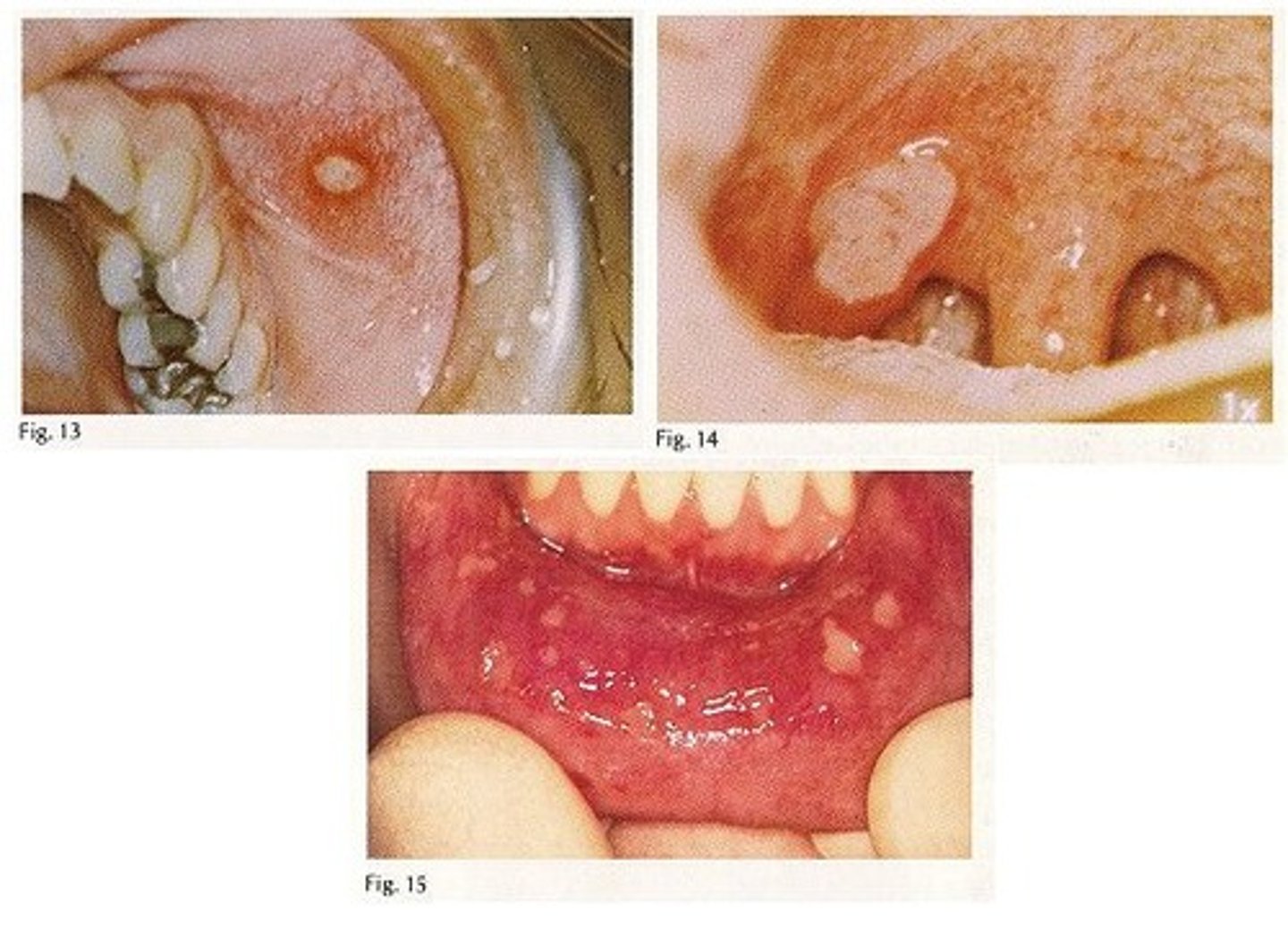
anorexia due to discomfort with eating; ulceration; risk for oral candidiasis
Side Effects of Chemo:
What are the impacts of stomatitis?
caused by direct stimulation of chemoreceptor trigger zone in the brain; pre-medicate prior to treatment; immediate and dramatic, may persist for hours/days
Side Effects of Chemo:
What occurs with nausea and vomiting?
Ondansetron (Zofran); side effects = HA, constipation, diarrhea, dizziness, QT prolongation
Side Effects of Chemo:
What is the medication that is used for nausea and vomiting?
injury to hair follicles due to cytotoxic meds; begins 7-10 days post-treatment; regeneration begins 1-2 months after last course of treatment
Side Effects of Chemo:
What occurs with alopecia?
vasoconstriction and reduces drug delivery to hair follicles -> causes HA
Side Effects of Chemo:
With reducing alopecia, what is cold capping?

alkylating agents; platinum compounds; anti-metabolites; mitotic inhibitors
What are all of the types of cytotoxic medications?
an alkylating agent; can kill at any time during the cell cycle
Cytotoxic Medications:
What is Cyclophosphamide?
a platinum compound; can kill at any time during the cell cycle, INCLUDING the resting phase
Cytotoxic Medications:
What is Cisplatin?
a folic acid analog anti-metabolite; works in the synthesis phase by disrupting DNA
Cytotoxic Medications:
What is Methotrexate?
a pyrimidine analog anti-metabolite; works in the synthesis phase by killing dividing cells
Cytotoxic Medications:
What is Flurouracil?
a mitotic inhibitor; kills during the mitosis phase
Cytotoxic Medications:
What is Vincristine?
cure, prolongation of life, palliative treatment -> depends on type of cancer, responsiveness to chemo, and general health of pt
Decision to Treat with Chemo:
What are the basic benefits of chemo?
a score less than 40 indicates pt is unlikely to tolerate chemo (100 is the best)
Decision to Treat with Chemo:
What is the Karnofsky Performance Scale?
used primarily for breast and prostate cancers; mimic or block the actions of endogenous hormones
What do hormonal agents do for cancer?
blocks estrogen receptors (blocks action of estrogen); used for established breast cancer disease and for reducing occurrence in high-risk pts
Breast Cancer Treatment:
What is Tamoxifen?
can only use it for 5 years due to risk of endometrial cancer; hot flashes, fluid retention, vaginal discharge, menstrual irregularities, teratogenesis
Breast Cancer Treatment:
What are the adverse effects of Tamoxifen?
inhibits gonadotropin release, suppressing ovarian and testicular steroidogenesis -> blocks creation of estrogen and testosterone
Hormonal Treatment:
What is Leuprolide (Leupron)?
generally well tolerated; hot flashes; testosterone loss may aggravate bone pain
Breast Cancer Treatment:
What are the adverse effects of Leuprolide (Leupron)?
designed to bind with specific targets to suppress tumor growth; goal to destroy cancer cells without destroying normal cells
What do targeted drugs do with cancer?