Comprehensive Guide to Pediatric Feeding, Eating, Sleep, and Rest Interventions
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
Feeding
Setting up and bringing food to mouth.
Eating
Manipulating the food or fluid in the mouth and swallowing.
Pediatric Feeding Disorder
Impaired oral intake that is not age-appropriate and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction.
Common Challenges Associated with Feeding and Eating
Gastroesophageal reflux disease (GERD), food allergies, poor oral motor function, difficulties with tongue function, drooling, and challenging behaviors such as gagging and sensory-related responses.
Collaboration in OT Practitioners
Collaboration with child, family and caregivers, psychology, nutrition, medicine, and speech language pathology.
Multidisciplinary Approaches
Can lead to successful weaning from tube feedings, increased oral intake, improved mealtime behaviors, and reducing parenting stress.
Holistic Approach to Interventions
Focus on safety, universal precautions, and recognizing signs of distress.
Adaptive Equipment
Includes Dycem, scoop dish, suction cup dishes, light-weight utensils, built-up handle, universal cuff, utensils with shorter or curved handles, cups with handle or wide base or lid, long straw used in cup with cup holder, adapted seating with stable tray, and stabilizing elbow on table/tray to reduce physical demands.
Promote Grasp & Release & AROM
Utilizes biomechanical and developmental approach, motor learning techniques, ROM, strengthening, endurance, and coordination.
Phases of Eating and Swallowing
Includes oral preparatory (container to oral manipulation = food bolus), oral propulsive (moves bolus posteriorly), pharyngeal (swallow is triggered), and esophageal (food moves through the esophagus towards stomach).
Positioning: Oral Prep Phase for Infants
Midline positioning with full support of head and body and gently flexed posture is ideal for infants who are breast and body feeding.
Positioning: Oral Prep Phase for Older Children
Aim for >90/90/feet flat on the surface; slight flexion in trunk and neck facilitates swallowing.
Choking Hazard Position
Supine poses choking hazard.

Recommended Positioning for Suck-Swallow-Breathing Coordination
Side-lying on incline may be recommended.
Upright Position Recommendation
4-6 months = more upright position recommended.
High-Chair Adaptation
High-chairs can be adapted with small towels to maximize lateral support, stability, alignment, and improve oral motor skills for oral intake.
Lips and cheeks
Adequate lip closure and lip seal are needed for sucking and oral control (prevent spillage and drooling).
Structural differences
Such as a cleft > adaptive equipment, positioning.
Abnormal tightness
Requires AROM/PROM.
Weakness
Requires strengthening.
Tongue
Activities include silly faces in the mirror, licking lollipops, frosting, and whipped cream.
Dissociation from jaw
Refers to the ability to move the tongue independently from the jaw.
Lateralization
Beneficial for children with a tongue thrust; present spoon or food to the side of the mouth instead of midline.
Jaw
Issues include open mouthed posture, drooling, food/liquid loss during feeding/drinking.
Non-nutritive chewing
Repetitive chewing on a resistive device (p & q).
Adaptive bottle systems
May benefit infants with weak suck, limited endurance, and/or anatomic differences.

Introduction to straws
Best with a smaller straw, which requires less suction and delivers smaller amounts of liquid.
Sippy cups
Available in different spout varieties and non-spill valves.

U-Shaped cut out cups
Helps maintain a neutral head position for children with extensor tone or poor head control.
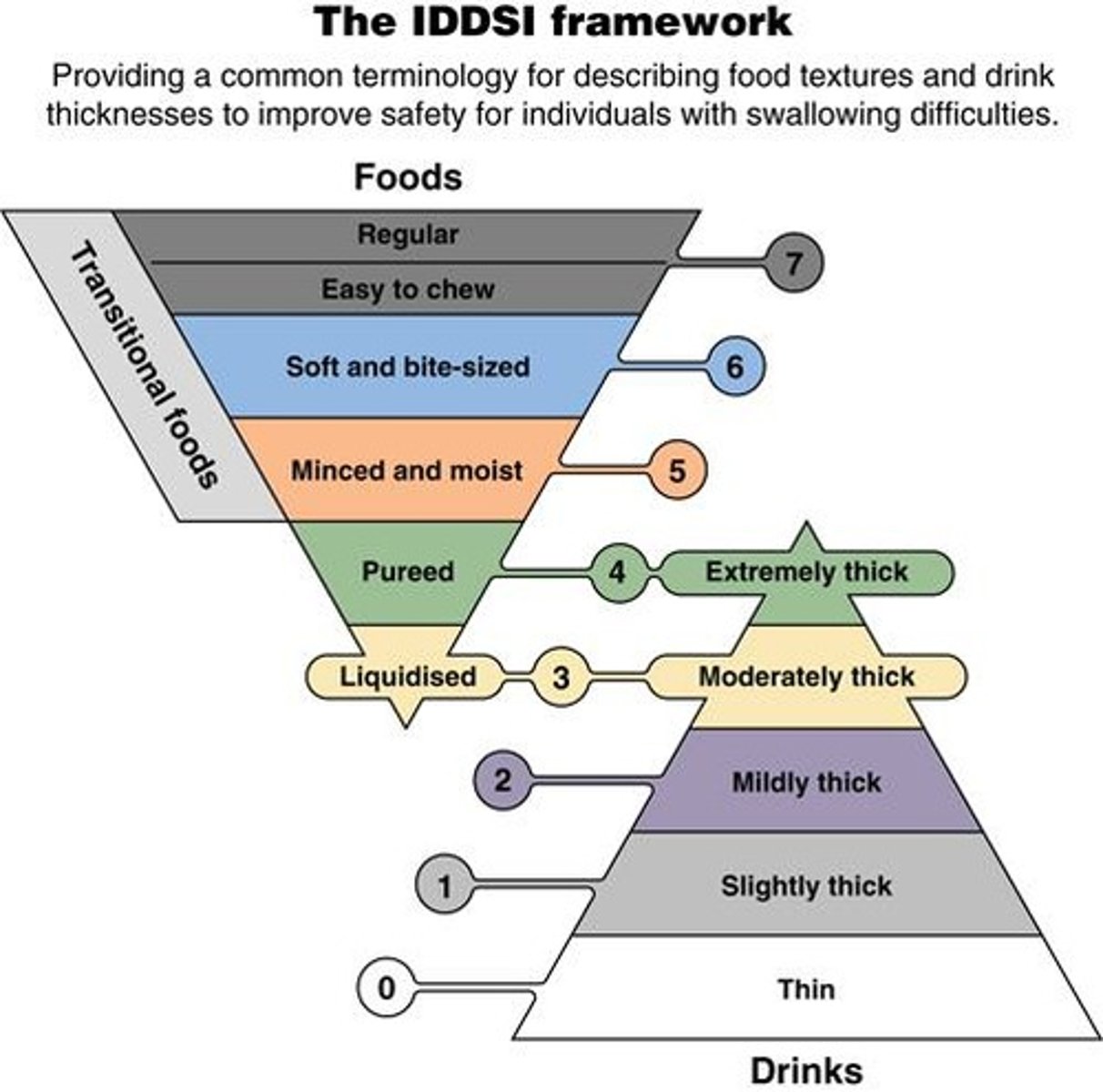
Thickened liquids
Considered for improving swallowing safety.
Aspiration
Food in airway before, during, or after a swallow, which can lead to lung disease, pneumonia, and other medical problems.
Signs of aspiration
Refer to Box 11.4.
VFSS
Videofluoroscopic swallow study.
FEES
Fiberoptic evaluation of swallowing.
Non-oral feeding methods
Such as tube feeding may be required.
Chin tuck
Reduces laryngeal opening; may be contraindicated for infants with softening of the cartilage of the larynx or trachea.
Natural chin tuck
Promoted via straw or straw style sports bottle.
Empty spoon technique
Offering an empty spoon in the same way as a bite of food may stimulate oral movements to prompt a second swallow.
Pace of oral feeding
Recommendations should allow the child sufficient time to swallow between bites.
Modification to food consistency
Thin liquids offered from an open cup are most difficult to control during swallowing.
Thickened liquid examples
Simply thick, Gelmix, Purathick.
Blenderized foods
Regular fruits and vegetables, baby foods, yogurt, and pudding may be blenderized to make thickened smoothies or shakes for older children.
Behavioral interventions
Create new positive interactions and child associations around feeding activities and mealtimes.
Positive reinforcement
Use positive reinforcement and ignore or redirect inappropriate behaviors.
Systematic Desensitization
A therapeutic approach used to reduce anxiety by gradually exposing a person to the feared object or context.
Cognitive Behavioral Therapy
A type of psychotherapy that helps individuals understand the thoughts and feelings that influence behaviors.
Regular Exposure to Non-Preferred Foods
Evidence suggests that it takes multiple presentations of a food before a child feels comfortable with it.
Structuring Mealtimes
Helps promote hunger cues and less access to less nutritious foods.
Environmental Adaptations
Changes made to the environment to promote better eating habits and safety.
Consistent Meal-Times
Promotes routine and stability in eating habits.
Self-Feeding Effort
The effort involved in self-feeding impacts oral motor skills, swallowing safety, and overall length of meal.
Ideal Meal Periods
Meal periods of 15-30 minutes are considered ideal.
GI Disorders and Neuromuscular Challenges
These conditions benefit from shorter, more frequent meal-times.
Limit Distractors
Reducing distractions helps promote independence and safety during meals.
Oral-Motor Challenges
May benefit from tough textures presented first during meals.
Hypersensitivity
Characterized by gagging with advanced consistencies or a lack of flexibility in food tolerance.
Hyposensitivity
Frequently seeks input by mouthing toys, decreased awareness of drooling, and/or overstuffing while eating.
Deep Pressure
Applied from distal to proximal to provide sensory input.
Oral Exploration through Play
Involves using teethers, vibrating toys, and self-directed touch in a child-controlled motivating context.
Food Chaining
A method that begins with a preferred food and gradually introduces new foods that are similar in texture.
Sleep
A reversible state where one is perceptually disengaged from and unresponsive to the environment.
Circadian Rhythm
A biological clock that operates in 24-hour cycles, influenced by light, mealtimes, temperature, bedtime routines, and physical activity.
Melatonin Release
The clock alerts the body and brain to release melatonin after dusk when it gets dark.
Sleep Problems
Can disrupt family dynamics and lead to cognitive and behavioral issues in children.
Consequences of Sleep Deprivation
May result in stress, irritability, reduced concentration, sleepiness, and impaired sleep quality.
Sufficient sleep
Associated with rest and overall well-being.
Rest
Quiet and effortless actions that interrupt physical and mental energy.
Rest time activities
Should be different from regular activities to promote relaxation.
SUIDS or SIDS
Sudden unexplained infant death syndrome, a broad spectrum of explained and unexpected deaths of previously healthy infants under a year.
Unsafe sleeping environments
Environments with soft surfaces or objects that can block an airway, shared sleeping with another person or pet, or infant's position leading to airway blockage or entrapment.
Factors negatively influencing sleep
Using technology before bedtime, light from technology sources, high-intensity social activities, school policies, low socioeconomic backgrounds, using child's sleeping space as punishment, and validating irrational fears.
Factors positively influencing sleep
Environmental modifications, soothing sounds, comfortable temperature, predictable caring relationships, calming bedtime routines, and use of favorite items.
Lifestyle Modifications
Consistent bedtime and wake-up time, dark and quiet bedroom, avoidance of excessive fluids, caffeine, vigorous activity, and limiting screen time.
OT Interventions
Cognitive behavioral training for insomnia, promoting positive self-talk, journaling, guided imagery, and educating parents about sleep benefits.
Cognitive behavioral training for insomnia
CBT-I, a method to improve sleep through cognitive and behavioral strategies.
Mindfulness
A practice that involves being present and fully engaging with the moment.
Yoga
A physical and mental practice that combines postures, breathing exercises, and meditation.
Progressive Muscle Relaxation
A technique to reduce muscle tension and promote relaxation.
Calming sounds
Sounds such as white noise that help soothe children to sleep.
Soothing aromas
Scents like lavender, cinnamon, and baby powder that promote relaxation.
Comfortable temperature
An optimal sleeping environment that is neither too hot nor too cold.
Predictable caring relationships
Relationships that provide emotional support and care to children.
Calming and supportive bedtime routines
Routines that help children wind down and prepare for sleep.
Bed-time routine
A series of activities performed before sleep, such as a bath close to bedtime.
External noise
Sounds from outside the bedroom that can disrupt sleep.
Excessive fluids before bedtime
Consumption of drinks that may lead to nighttime awakenings for bathroom use.
Caffeine before bedtime
Intake of stimulants that can interfere with the ability to fall asleep.
Vigorous activity before bedtime
Engagement in high-energy activities that may hinder the ability to relax and sleep.