General and Local Anesthetic Agents
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
Categories of Anesthetics
General Anesthetics
o Central nervous system (CNS) depressants used to
produce loss of pain sensation and consciousness and
loss of body reflexes, including paralysis of
respiratory muscles
Monitored anesthesia care (MAC): local anesthesia
along with sedation and analgesia with amnesia
Local Anesthetics
o Used to cause loss of pain sensation and feeling in a
designated area of the body
o Does not produce the systemic effects associated
with severe CNS depression
General Anesthetics
Administered by anesthesia providers
o Anesthesiologist
o Nurse anesthetist (CRNA)
o Anesthesia assistant
Goals of anesthesia
o Analgesia
Loss of pain perception
o Unconsciousness
Loss of awareness of one’s surroundings
o Amnesia
Inability to recall what took place
Agents Involved in Balanced Anesthesia
Preoperative Medications
Sedative–Hypnotics
Antiemetics
Antihistamines
Narcotics
General Anesthetics types
Inhalational anesthetics
o Volatile liquids or gases that are vaporized in oxygen
and inhaled
Parenteral anesthetics
o Administered intravenously
Adjunct anesthetics
o Drug that enhances clinical therapy when used
simultaneously with another drug
Risk Factors Associated With
General Anesthetics
CNS Factors
Cardiovascular Factors
Respiratory Factors
Renal and Hepatic Function
Risk Factors Associated With
General Anesthetics
Malignant hyperthermia
o Occurs during or after volatile inhaled general anesthesia or use of the neuromuscular blocking drug (NMBD) succinylcholine
o Sudden elevation in body temperature (greater than 104° F)
o Tachypnea, tachycardia, muscle rigidity
o Life-threatening emergency
o Treated with cardiorespiratory supportive care and
dantrolene (skeletal muscle relaxant)
Types of General Anesthetics agents
Barbiturate
Non-Barbiturate
Gas Anesthetics
Volatile Liquids
Benzodiazepine
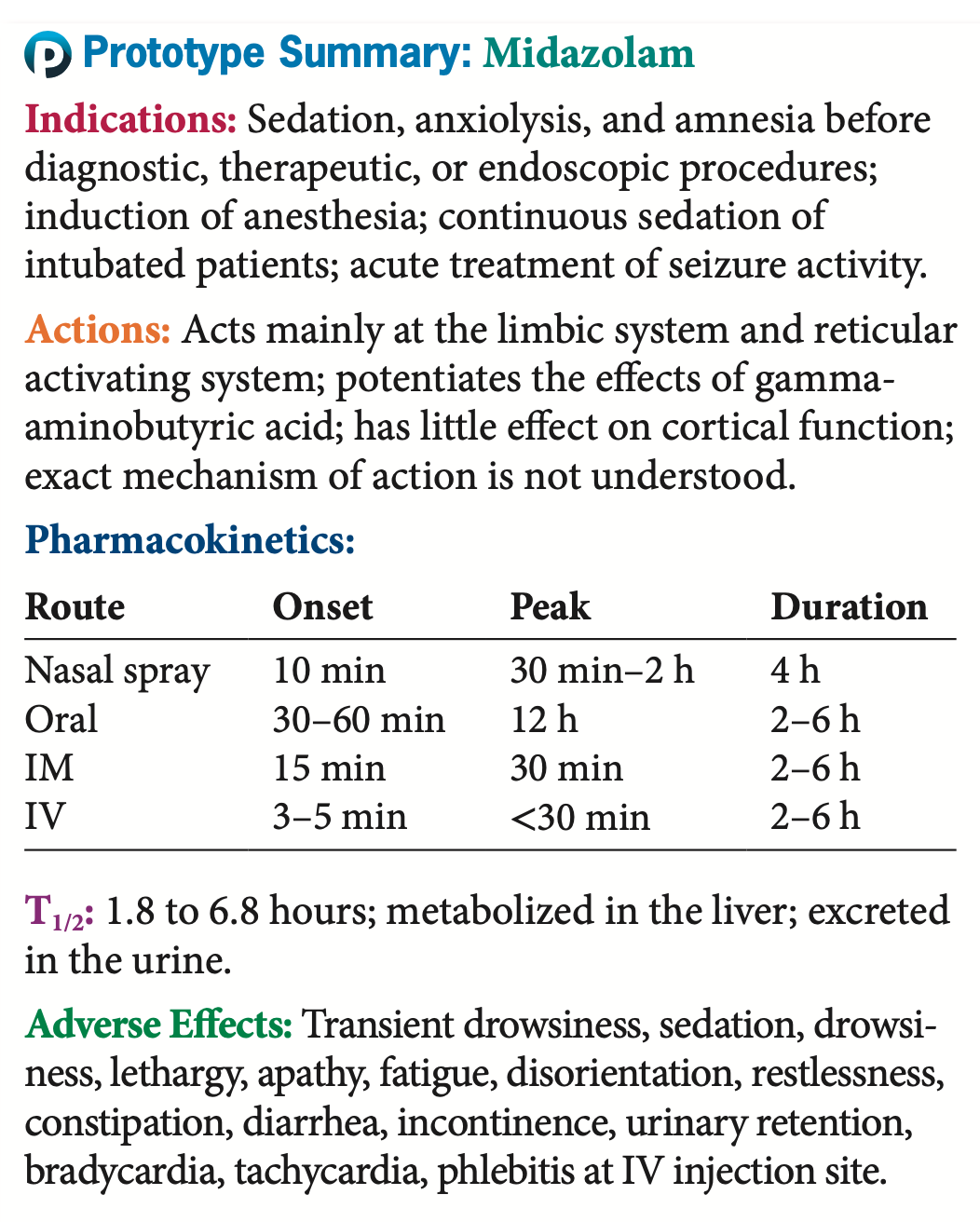
Midazolam
Indications Prior to surgery or procedure drowsiness, relieve anxiety,
and prevent any memory of the event.
Rapid onset of effects and short duration of action.
Chance of addiction/dependence
Delirium in elderly patients
Preserves the patient’s ability to maintain own airway and to respond
to verbal commands
Used for diagnostic procedures and minor surgical procedures that do
not require deep anesthesia
Rapid recovery time and greater safety profile than general anesthesia
Midazolam
It is a potent amnesiac and in the benzodiazepine classification
Midazolam’s amnesiac effects occur at doses below those needed to cause sedation. It is widely used to produce amnesia or sedation for many diagnostic, therapeutic, and endoscopic procedures. Midazolam can also be used to induce anesthesia and to provide continuous sedation for intubated and mechanically ventilated patients.
Midazolam
Contraindications and Cautions
Midazolam has been associated with respiratory depres- sion and respiratory arrest, and so life support equipment should be readily available whenever it is used.
midazolam
Adverse Effects
Patients receiving any general anesthetic are at risk for skin breakdown because they will not be able to move. Care must be taken to prevent decubitus ulcer forma- tion. Patients receiving midazolam should be monitored for respiratory depression and CNS suppression
Non-Barbiturate Anesthetics
Propofol
Parenteral general anesthetic
Used for the induction and maintenance of general
anesthesia
Sedation for mechanical ventilation in ICU settings
Lower doses: sedative-hypnotic for moderate sedation
Monitor triglycerides if administered with total parenteral
nutrition
Some states prohibit administration by nurses.
Propofol
Propofol is often used for short procedures because it has a very rapid clearance, produces much less of a hangover effect, and allows for quick recovery. It is also used to maintain patients on mechanical ventilation.
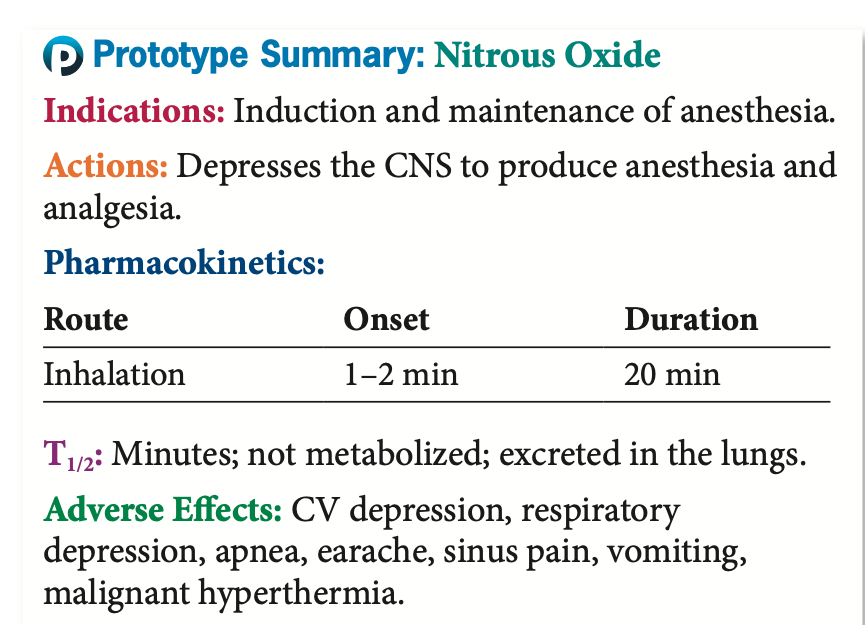
Anesthetic Gases
Nitrous Oxide
Like all inhaled drugs, anesthetic gas enters the bronchi and
alveoli, rapidly passes into the capillary system
Very flammable, associated with toxic effects
Laughing gas”
Weakest of the general anesthetic drugs
Used primarily for dental procedures or as a supplement to
other, more potent anesthetics
Actions and indications: Moves so quickly it can actually
accumulate and cause pressure in closed body compartments
such as the sinuses. A very potent analgesic
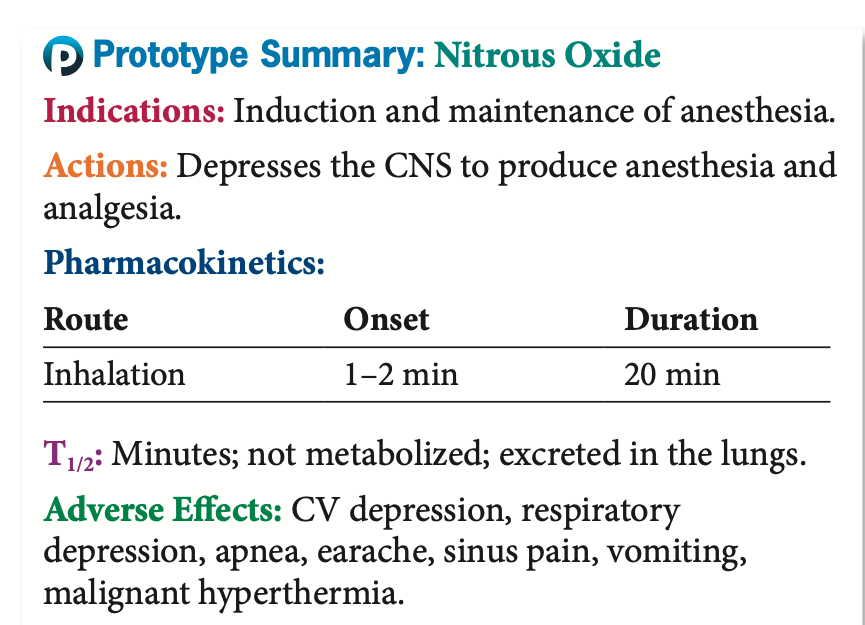
Anesthetic Gases
Pharmacokinectics and adverse effect
Pharmacokinetics: Rapid onset of action, usually within 1 to 2
minutes, and a rapid recovery period. Timing of recovery
depends on the other drugs being used
Can block the reuptake of oxygen after surgery and cause
hypoxia and pregnancy and lactation
Adverse effects: Acute sinus and middle-ear pain, bowel
obstruction and pneumothorax
Drug-drug interactions: CNS depressants
Methods of Administering
Local Analgesics
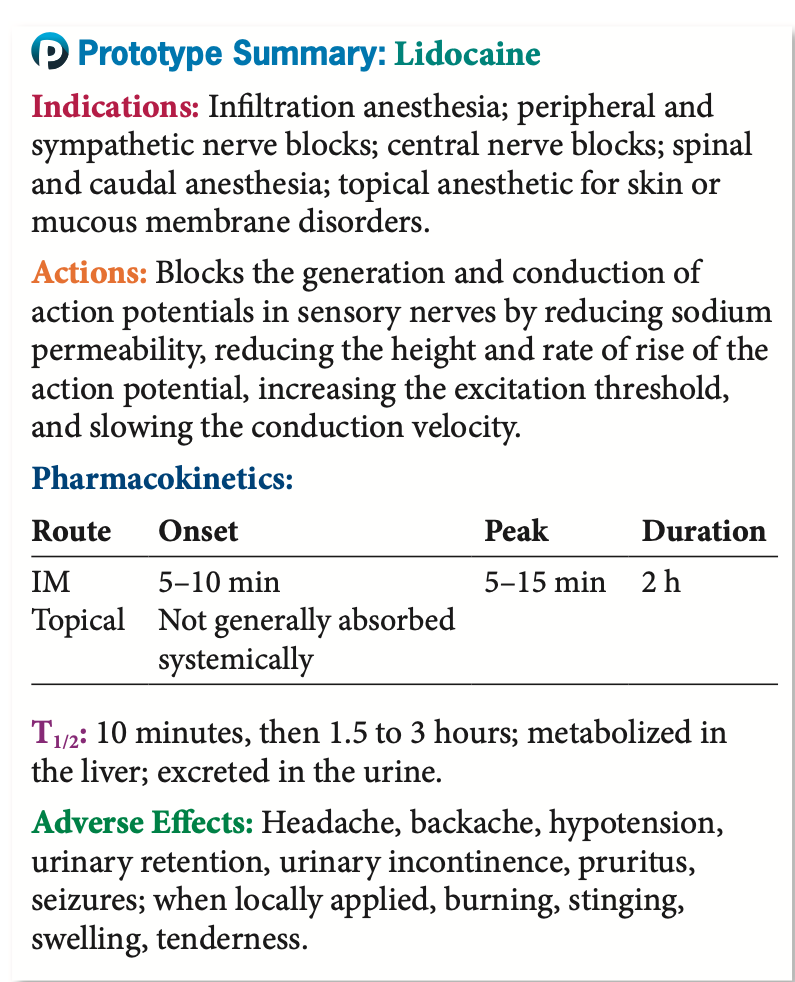
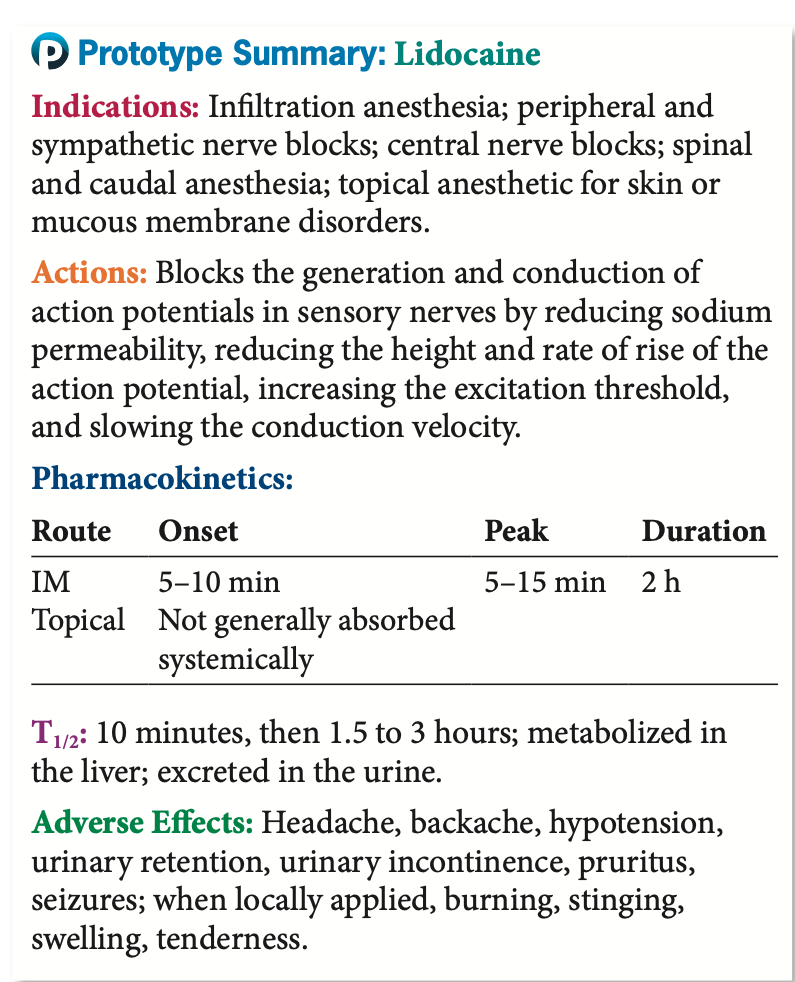
Lidocaine
Topical Administration: Although systemic absorption is rare with topical application, it can occur if there is damage or breakdown of the tissues in the area, if large portions of the body are covered in topical anesthetic, or if an occlusive barrier is placed over the topical anesthetic.
Infiltration: Infiltration local anesthesia involves injecting the anesthetic directly into the tissues to be treated
Field Block: Field block local anesthesia involves injecting the anesthetic all around the area that will be affected by the procedure or surgery. (tooth extractions)
Nerve Block: Nerve block local anesthesia involves injecting the anes- thetic at some point along the nerve or nerves that run to and from the region in which the loss of pain sensation or muscle paralysis is desired.
Intravenous Regional Anesthesia: V regional local anesthesia, or “Bier block,” involves carefully exsanguinating blood from the patient’s arm or leg by compression tourniquets. The anesthetic is injected into the vein of the limb that requires the anesthesia, and tourniquets are used to prevent the anesthetic from entering the general circulation.
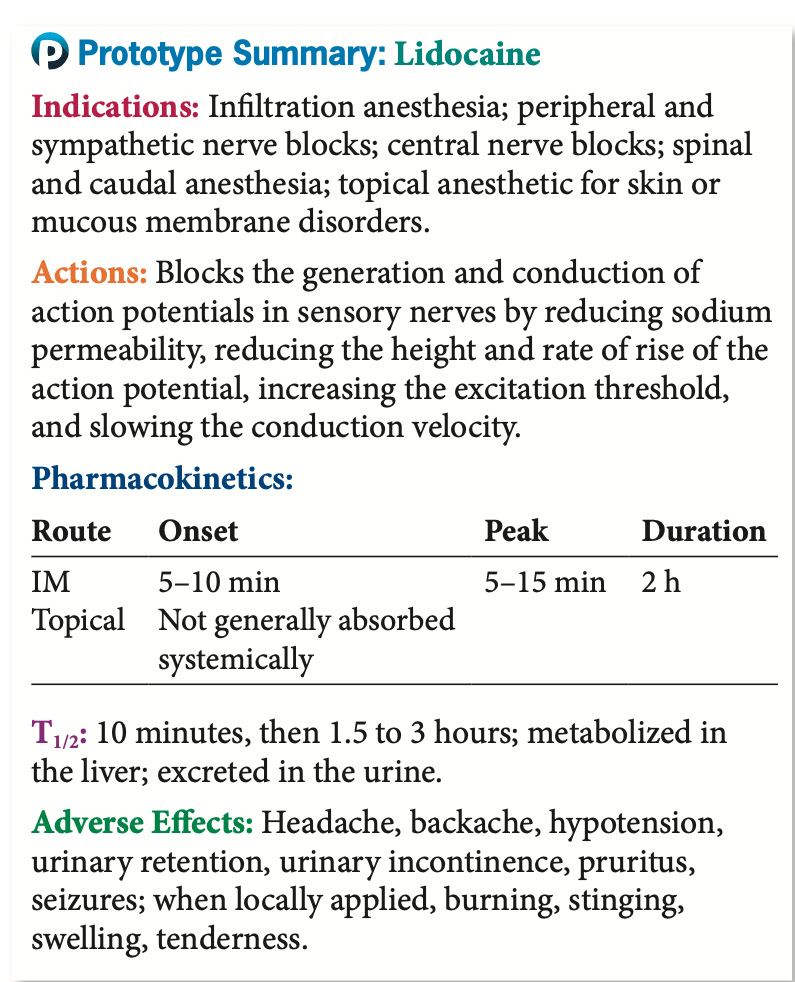
Local Anesthetic:
Adverse Effects
Usually limited
Adverse effects result if:
o Inadvertent intravascular injection
o Excessive dose or rate of injection
o Slow metabolic breakdown
o Injection into highly vascular tissue
o Allergy
Generally limited
Most common with “ester type” anesthetics
Local Anesthetic:
Adverse Effects
“Spinal headache”
A spinal headache is a type of headache that occurs due to a decrease in cerebrospinal fluid (CSF) pressure in the space around the spinal cord.
70% of patients who either experience
inadvertent dural puncture during epidural
anesthesia or undergo intrathecal anesthesia.
Usually self-limiting
Treatment: bed rest, analgesics, caffeine, blood
patch
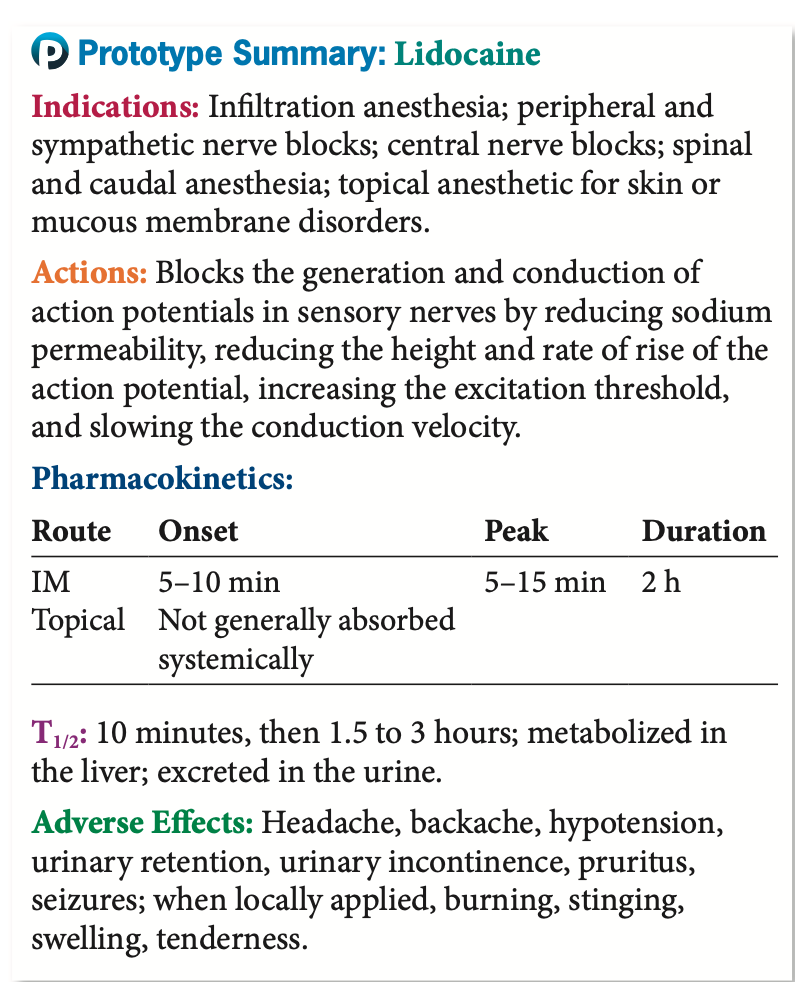
Local Anesthetic Agents
Actions
o Temporary interruption in the production and conduction of nerve
impulses
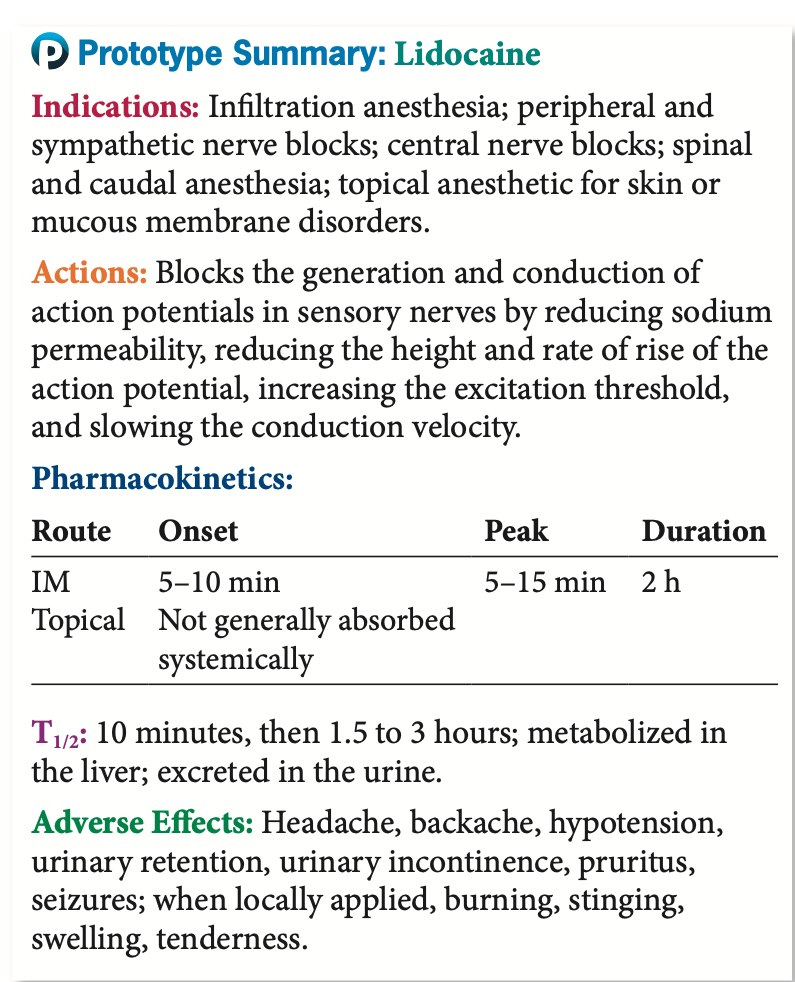
Local Anesthetic Agents
Pharmacokinetics
The amide local anesthetics are metabolized more slowly in the liver, and serum levels of these drugs can increase and lead to toxicity.
The ester local anesthetics are broken down immediately in the plasma by enzymes called plasma esterases.
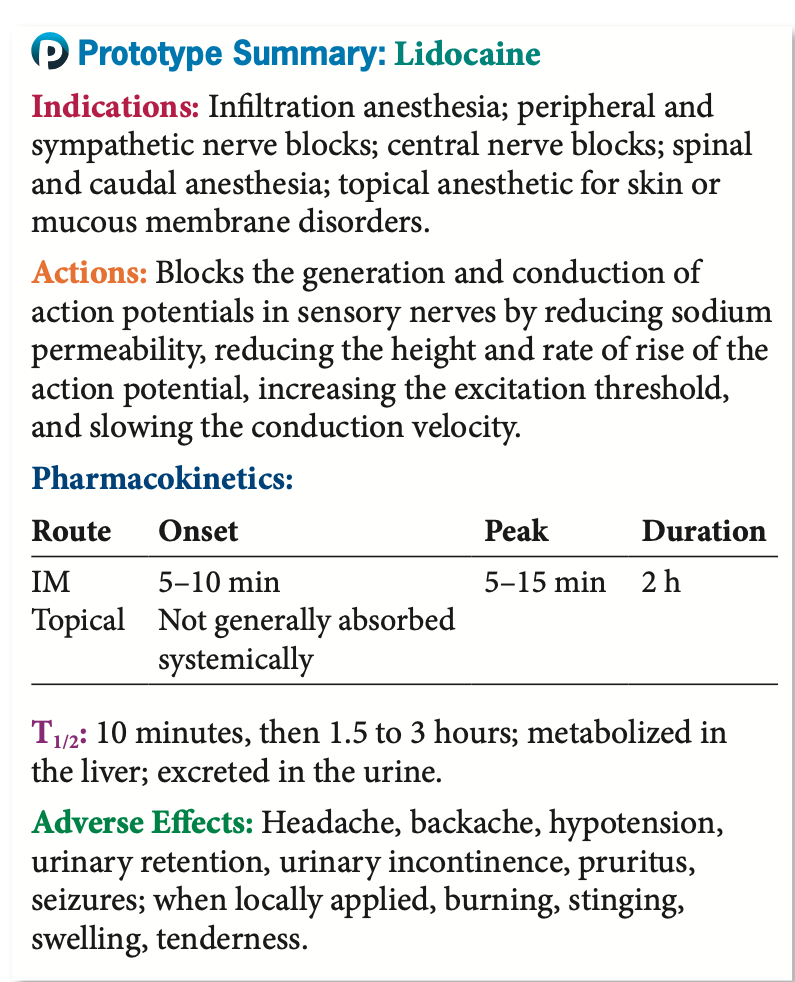
Local Anesthetic Agents
Indication
o For infiltration anesthesia, peripheral nerve block, spinal anesthesia, and
the relief of pain
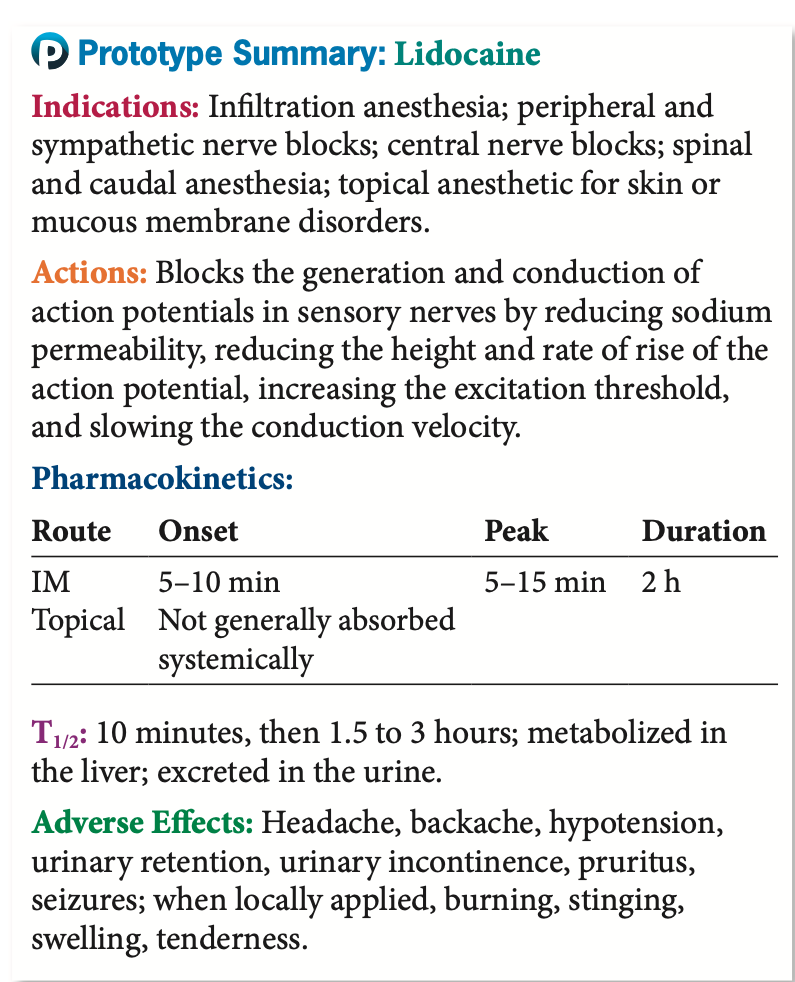
Local Anesthetic Agents
Contraindications
o Known allergy, heart block, shock, decreased plasma esterases
history of allergy to any one of these agents or to parabens to avoid hypersensitivity reactions; heart block, which could be greatly exacerbated with systemic absorption at very high levels; shock, which could alter the local delivery and absorption of these drugs; and decreased plasma esterases, which could result in toxic levels of the ester-type local anesthetics.
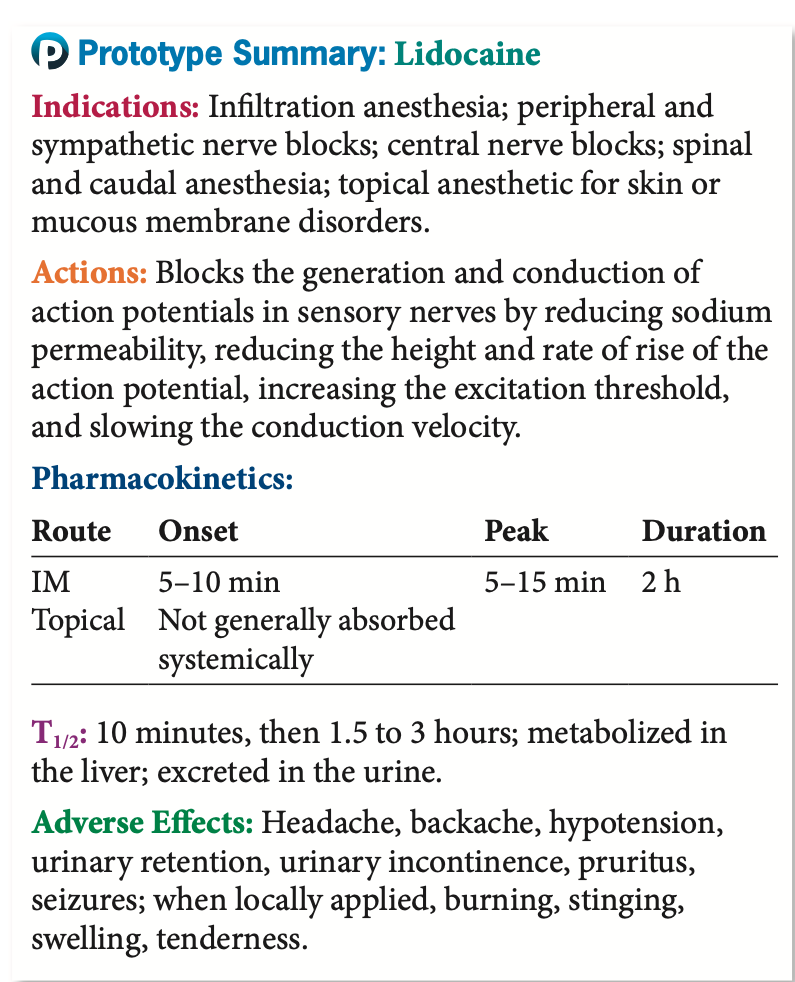
Local Anesthetic Agents
Adverse Effects
o Headache, restlessness, anxiety, blurred vision, nausea, vomiting, myocardial depression
The adverse effects of these drugs may be related to their local blocking of sensation (e.g., skin breakdown, self- injury, biting oneself if used in the oral cavity) There are risks of CNS effects such as headache, restlessness, anxiety, dizziness, tremors, blurred vision, and backache; GI effects such as nausea and vomiting; CV effects such as peripheral vasodilation, myocardial depression, arrhythmias, and blood pressure changes, all of which may lead to fatal cardiac arrest; and respiratory arrest
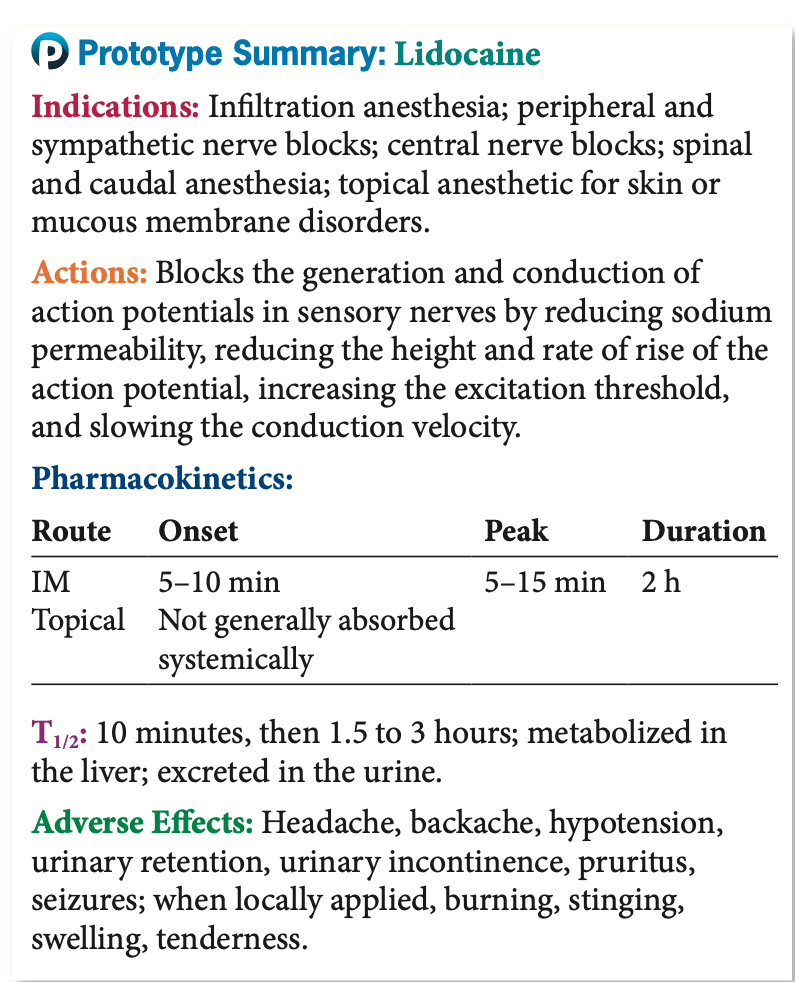
Local Anesthetic Agents
Drug-Drug Interactions
o Succinycholine
o Epinephrine
When local anesthetics and succinylcholine are given together, increased and prolonged neuromuscular blockade occurs. When used in combination with epinephrine, there is risk of vasoconstriction causing gangrene.