Oral Cavity and Gastrointestinal Tract
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
What are Aphthous ulcers (Canker sores)?
Solitary or multiple painful recurrent lesions of the oral mucosa; shallow hyperemic ulcerations covered by thin exudate and surrounded by erythem
Aphthous ulcer treatment & cause
resolve spontaneously in 7-10 days; cause unknown; increased prevalence in celiac disease, IBD, and Behçet disease
most common fungal infection of the oral cavity
candidiasis
Oral candidiasis (thrush)
White, curdlike pseudomembranes that can be scraped off, revealing an erythematous base; caused by Candida albicans
3 types of oral candidiasis
Pseudomembranous (thrush)
Erythematous
Hyperplastic
trt of candidiasis
nystatin
HSV1 vs HSV2
1: oral lesions
2: genital lesions
HSV1 sx
lymphadenopathy, fever, anorexia
causes of HSV1 reactivation
trauma, allergies, UV light, URI, pregnancy, mesntruation, excessive exposure to heat or cold
cells of HSV2 infection
ballooned with large eosinophilic intranuclear inclusion
adjacent cells fuse to form large mutlinucleated polykaryons
MC oral cavity cancer
squamous cell carcinoma (95%)
when is SCC often diagnosed?
late stages
field cancerization
exposure to carcinogens results in multiple primary tumors developed independently
associated with squamous cell carcinoma
where are SCC HPV associated lesions found?
tonsillar crypts, base of tongue, oropharynx?
do HPV + or HPV - tumors have a better prognosis?
HPV +
atresia
thin, non canalized cord replaces a segment of esophagus
mechanical obstruction
atresia is often associated with what abnormality?
a fistula connecting upper and lower esophageal pouches
MC cause of esophageal stenosis
inflammation and scarring
causes of esophageal stenosis
gerd, irradiation, caustic injury
progressive esophageal stenosis can lead to what difficulty?
swallowing liquids (starts as solids)
achalsia
failure of the lower esophagus sphincter (LES) muscle to relax
*functional obstruction
achalsia triad of causes
incomplete LES relaxation
increased LES tone
esophageal aperistalsis
*LES = lower esophageal sphincter
primary achalasia
idiopathic failure of distal esophageal inhibitory neurons
secondary achalasia
Chagas disease caused by Trypanosoma cruzi can cause (secondary) achalasia
mallory weiss syndrome
tear of distal esophagus from retching in alcoholic or bulimic or hyperemesis gravidarum
sx of mallory weiss syndrome
painless hematemesis
dx of mallory weiss syndrome
endoscopy
trt of mallory weiss syndrome
epi injection or thermal coagulation if not self-limited
is mallory-weiss or boerhaave syndrome more severe?
boerhaave syndrome
boerhaave syndrome
spontaneous esophageal rupture due to forceful vomiting, severe pain
mediastinal crunch; variety of sound including loud crackles and clicking or gurgling sounds; associated with mediastinal emphysema
hamman sign - in Boerhaave syndrome
diagnosis of boerhaave syndrome
CXR: mediastinal widening
contrast esophagram: definitive diagnostic study
trt of boerhaave syndrome
surgery if needed
mallory-weiss vs boeerhave locations
mallory-weiss : submucosa, mucosa, RIGHT posterolateral wall of the GE junction, linear lacerations
boerhaave: full thickness tear (transmural), LEFT posterolateral wall of distal esophagus
stratified squamous mucosa of the esophagus may be damaged by a variety of irritants including alcohol, corrosive acids or alkalis, excessively hot fluids, and heavy smoking. May present with pain with swallowing.
chemical esophagitis
odynophagia casues
pill-induced
infectious esophagitis (especially immunocompromised)
MCC of esophagitis
GERD
pathogenesis of GERD
decrease in LES tone or increase of abdominal pressure
delayed gastric emptying
increased gastric volume
GERD histology (normal vs significant diease)
hyperemia
significant disease: eosinophils in squamous mucosa followed by neutrophils
GERD sx
heartburn
regurgitation
dysphagia (NOT odynophagia)
overproduction of saliva
cough
hiccups
wheezing
GERD management
lifestyle
H2 blockers
PPI
endoscopy (if over 45, PPIP failed, bleeding, dysphagia, weight loss NSAIDS)
Eosinophilic esophagitis sx and trt
symptoms include food impaction, GERD-like symptoms, feeding intolerance, dysphagia;
treat with dietary restriction (e.g., milk/soy) and topical/systemic corticosteroids.
Eosinophilic esophagitis cardinal histology
epithelial infiltration by large numbers of eosinophils superficially and away from GE junction; patients often atopic;
Barrett esophagus pathophysiology
Replacement of normal squamous epithelium with metaplastic columnar epithelium (intestinal metaplasia with goblet cells) in distal esophagus due to long-standing reflux; intestinal metaplasia shows goblet cells.
What is the progression of the epithelium in Barrett Esophagus?
progression sequence: metaplasia → dysplasia → adenocarcinoma
What is the pathogenesis of Barret Esophagus?
prolonged and recurrent acid reflux attack causes inflammation leading ulceration of squamous cells
Healing occurs that change the cells
acidic pH in the distal esophagus from reflux differentiate the cells into columnar epithelial
Stomach protective layers
Surface foveolar mucin protects epithelium;
rich vascular supply delivers oxygen and bicarbonate and washes away acid;
gastric mucosa renews every 2-6 days.
Acute gastritis sx
transient mucosal inflammation
sx: dyspepsia, n/v
severe: erosion, ulcer, hemorrhage, melena
Acute gastritis causes
nsaids, etoh, smoking,, bisphosphonates, chemo, salmonellosis, trauma
Chronic gastritis cause & patho
Helicobacter pylori = S-shaped gram-negative rod
secretes enzymes/toxins causing mucosal damage
neutrophils recruited and contribute to injury
Peptic ulcer disease (PUD) cause
H. pylori
2nd is NSAIDS
*smoking and alcohol will exacerbate the disease and delay healing
Peptic ulcer disease (PUD) - duodenal or gastric more common?
duodenal ulcers occur more often than gastric (5x)
ages of PUD
typical age ranges: duodenal 30-55, gastric 55-70;
sx of PUD gastric vs duodenal
symptoms: dyspepsia, burning/gnawing pain radiating to back; gastric pain worse postprandial
duodenal pain often relieved by food.
most common cause of non-hemorrhagic GI bleed
PUD
what do PUD ulcers look like?
sharply punched out, round
MC malignancy of the stomach
Gastric adenocarcinoma
Gastric adenocarcinoma epidemology
Epidemiology varies by geography (higher in Chile, Japan, E Europe), lower socioeconomic
gastric adenoma pathogenesis
CDH1 mutation
familial
loss of E-cadherom function
familial adenomatous polyposis
APC/TP53 gene
H.pylori
IL-1 beta
EBV
proximal stomach
TP53 mutation
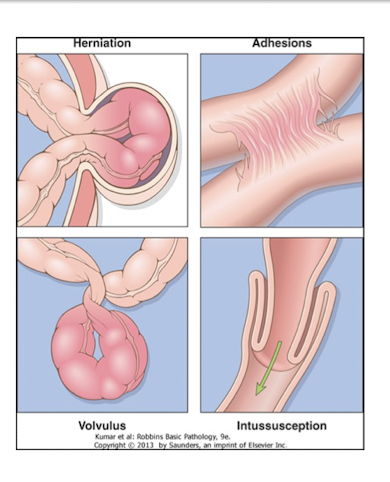
Small and large intestines — obstruction types
herniation, adhesions, volvulus, intussusception, neoplasm
Small bowel obstruction (SBO) Most common cause
adhesions (prior surgery)
Small bowel obstruction symptoms and trt
N/V, abdominal pain, distention; findings: high-pitched tinkling bowel sounds early, silent late; KUB shows air-fluid levels;
treatment: NG tube, bowel rest, surgery if not resolved in 24 hr.
Large bowel obstruction Most common cause
neoplasm
what is Hirschsprung disease?
Congenital aganglionic megacolon caused by absence of Meissner and Auerbach autonomic plexuses in a bowel segment causing inability or difficulty to pass stool
Hirschsprung disease sx and trt
presents with constipation, vomiting, failure to thrive, delayed passage of meconium; diagnosis via barium enema and confirmed with rectal biopsy;
treatment = resection of affected bowel.
Hirschsprung disease is associated with what disorder
Down Syndrome
Volvulus
Twisting of bowel on itself
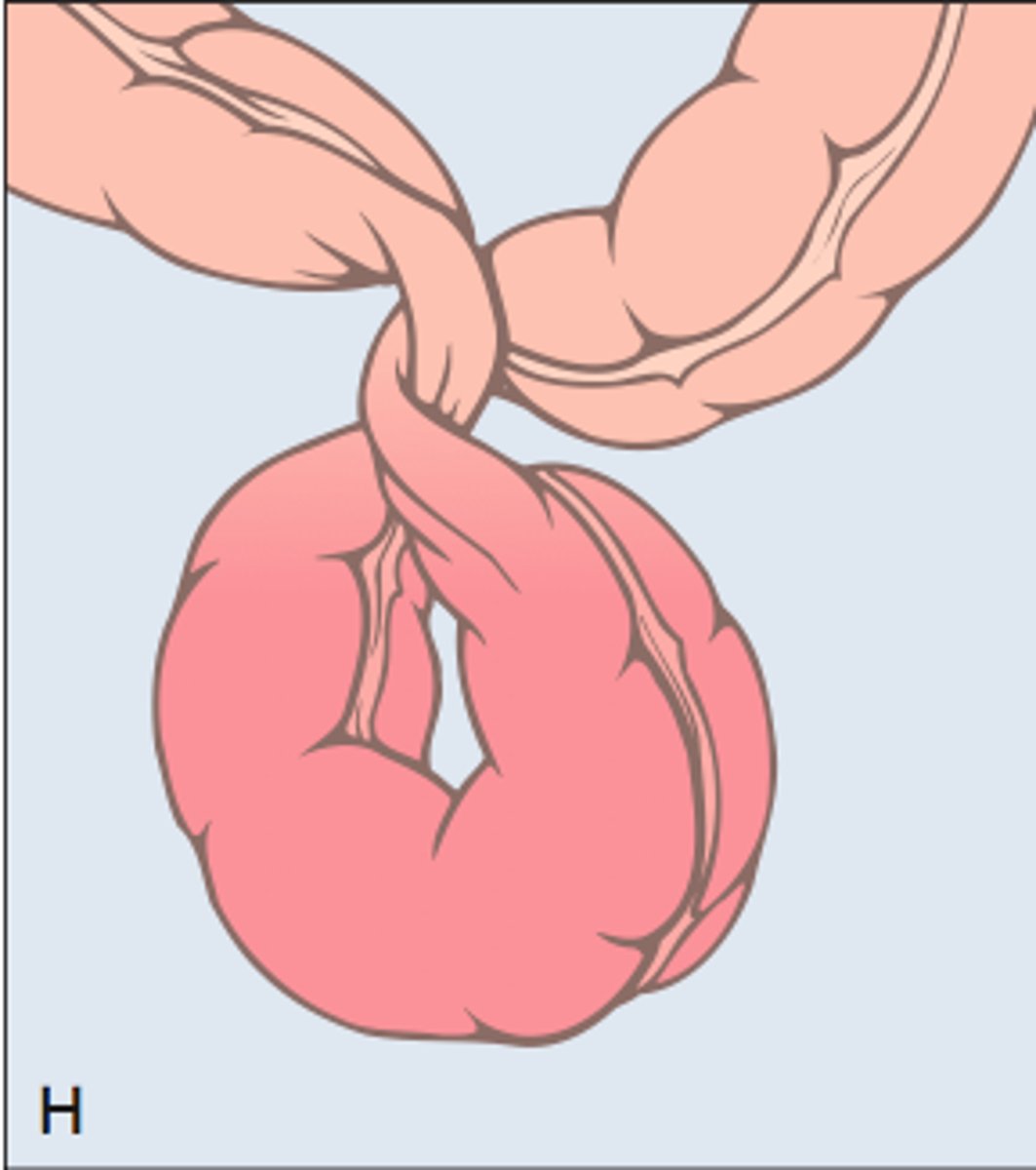
volvulus is mc where?
most commonly sigmoid colon;
volvulus sx and trt
causes crampy abdominal pain, N/V, tympany; diagnosis with abdominal x-ray showing distention;
treatment = endoscopic decompression or surgery if unresolved.
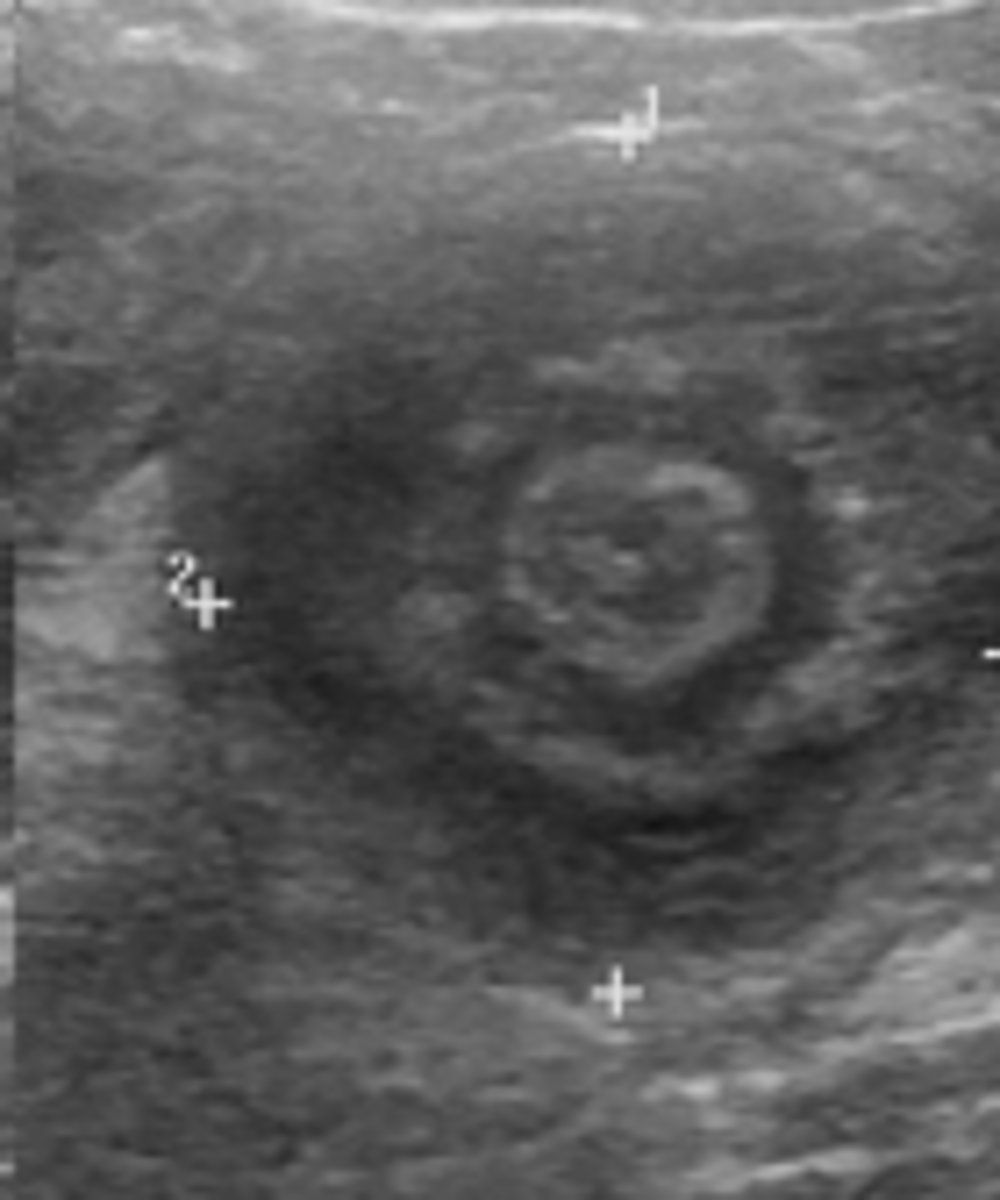
Intussusception usually happens in
children
Intussusception
Telescoping of intestine into distal segment
intussusception is associated with what illness?
rotavirus
intussusception diagnosis and trt
children diagnosed and treated with barium or air enema (diagnostic + therapeutic);
adults often require CT diagnosis and surgery.
intussusception CT sign
bulls seye
what is celiac disease?
Immune-mediated enteropathy triggered by gluten ingestion
Celiac disease pathogenesis
gliadin deamidated by tissue transglutaminase interacts with HLA-DQ2/DQ8 → CD4+ T cell activation and cytokine-mediated tissue damage
symptoms: weight loss, chronic diarrhea, iron deficiency anemia, failure to thrive in children; labs show malabsorption (Fe, Ca, Vit D, B12), IgA endomysial antibody positive.
Celiac disease sx and lab findings
symptoms: weight loss, chronic diarrhea, iron deficiency anemia, failure to thrive in children;
labs show malabsorption (Fe, Ca, Vit D, B12), IgA endomysial antibody positive.
Celiac disease associated dz
DDM, thyroiditis, Sjögren;
Celiac disease — extraintestinal sx
Dermatitis herpetiformis (pruritic papulovesicles on extensor surfaces) occurs in <10% but almost all with the skin disorder have celiac
Celiac disease causes an increased risk of what cancer?
enteropathy-associated T-cell lymphoma.
Celiac disease diagnosis and management
Diagnosis via serology (anti-tTG, endomysial antibodies) and duodenal biopsy (villous atrophy, crypt hyperplasia); treatment = strict gluten-free diet, nutrition support, involvement of dietician, avoidance of barley/rye/oats/wheat and cross-contamination; corticosteroids (e.g., budesonide) or prednisone may be used in refractory cases.
Inflammatory bowel disease (IBD)
Chronic idiopathic relapsing disorders (Crohn disease and ulcerative colitis) with interplay of genetics, microbiota, epithelial dysfunction, and mucosal immune responses
Is Inflammatory bowel disease (IBD) an autoimmune dz?
Crohn's and UC are not considered classic autoimmune diseases but involve dysregulated mucosal immunity.
IBD pathogenesis
Activated T cells drive disease progression; mucosal immunity and MALT (IgA) dysregulation; environmental triggers (microbes, diet) in genetically susceptible individuals; NOD2 mutation associated with Crohn disease (but <10% with mutation develop disease).
where can crohns occur?
May affect any GI segment, most commonly terminal ileum, ileocecal valve, cecum;
Crohn disease hallmarks
transmural inflammation with creeping fat, serosal reaction, ulcers, strictures, skip lesions, cobblestoning; noncaseating granulomas in ~35% of cases.
Crohn disease — clinical features
Abdominal pain, weight loss, fever, diarrhea, perianal fistulas, arthralgias, iritis/uveitis, sacroilitis, migratory polyarthritis, erythema nodosum, iron deficiency/hematochezia possible.
where does UC occur?
Continuous mucosal disease starting at rectum and extending proximally
Ulcerative colitis hallmarks
superficial mucosal inflammation limited to mucosa and submucosa; broad-based ulcers, pseudopolyps (mucosal bridges), granulomas typically absent.
megacolon typically occurs where
transverses colon
sx of toxic megacolon
leukocytosis, fever, emergency (perf risk)
Ulcerative colitis — clinical features
Bloody diarrhea, lower abdominal cramps relieved by defecation
Diverticulosis
Outpouchings of colonic mucosa/submucosa (false diverticula) through muscularis
how does Diverticulosis develop?
develops under conditions of elevated intraluminal pressure; taeniae coli anatomy contributes to focal weakness.
Diverticulosis usually occurs where and in who?
sigmoid colon, >80
Diverticulitis
Occurs in 15-20% of patients with diverticulosis when a diverticulum undergoes microperforation and inflammation
Diverticulitis sx and trt
LLQ pain, fever, leukocytosis; CT for diagnosis if not resolving with conservative therapy; avoid barium/colonoscopy in acute phase.
Diverticulitis complications
May lead to abscess, microperforation, peritonitis; outpatient treatment possible for mild disease