Sensory Systems, Pain, and Perception in Biopsychology
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
What are the three types of sensory cortex?
Primary sensory cortex, secondary sensory cortex, and association sensory cortex.
What is the hierarchical organization of sensory systems?
Information flows through brain structures in order of increasing anatomical complexity, with sensation being less complex than perception.
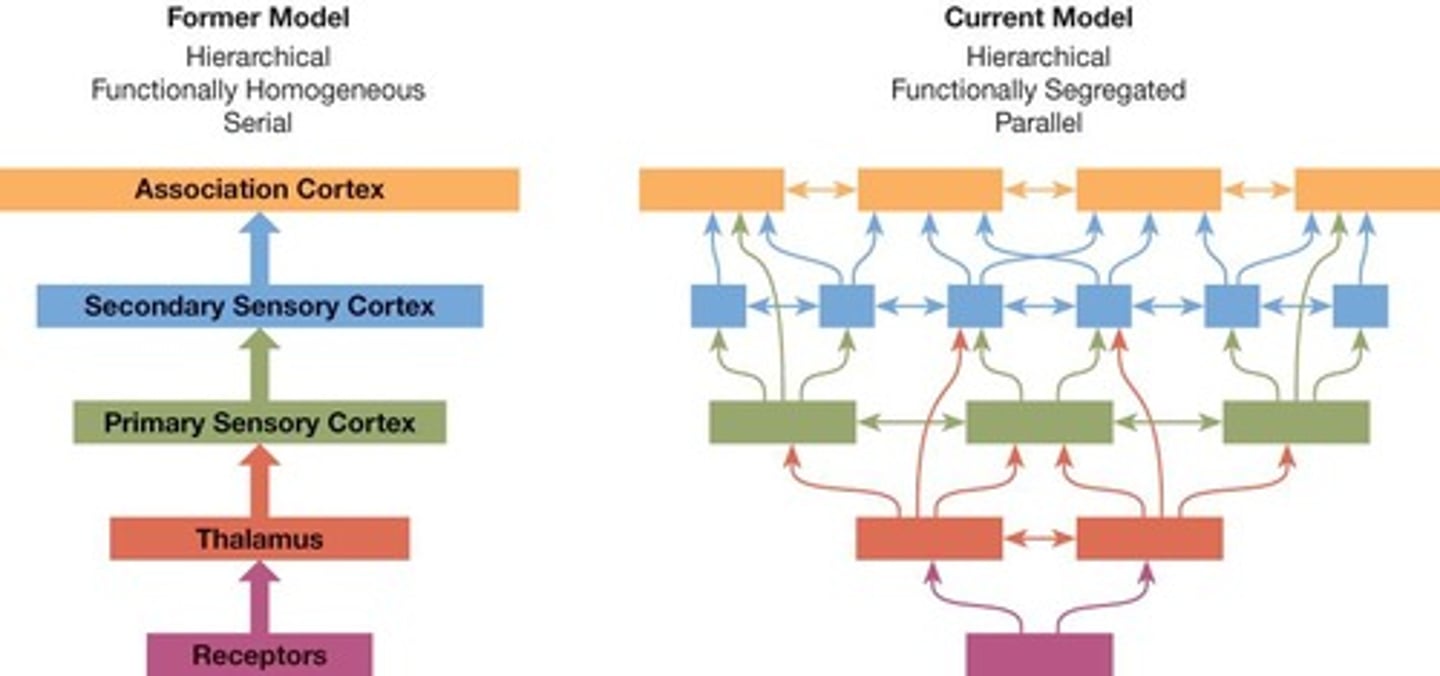
What is functional segregation in sensory systems?
Different parts of the sensory system specialize in different kinds of analysis, such as primary, secondary, and association functions.
What is parallel processing in sensory systems?
Information flows between structures simultaneously along multiple pathways.
What are the two major somatosensory pathways?
The dorsal-column medial-lemniscus system and the anterolateral system.
What does the dorsal-column medial-lemniscus system carry information about?
Touch and proprioception.
How does the anterolateral system function?
It mediates pain and temperature, with axons synapsing as soon as they enter the spinal cord.
What are the types of cutaneous receptors?
Free nerve endings, Pacinian corpuscles, Merkel receptors, and Ruffini corpuscles.
What is astereognosia?
The loss of the ability to recognize objects by touch.
What is asomatognosia?
The loss of the ability to recognize parts of one's own body.
What is the rubber-hand illusion?
A phenomenon where a person perceives a rubber hand as their own when both their hidden hand and the rubber hand are stroked synchronously.
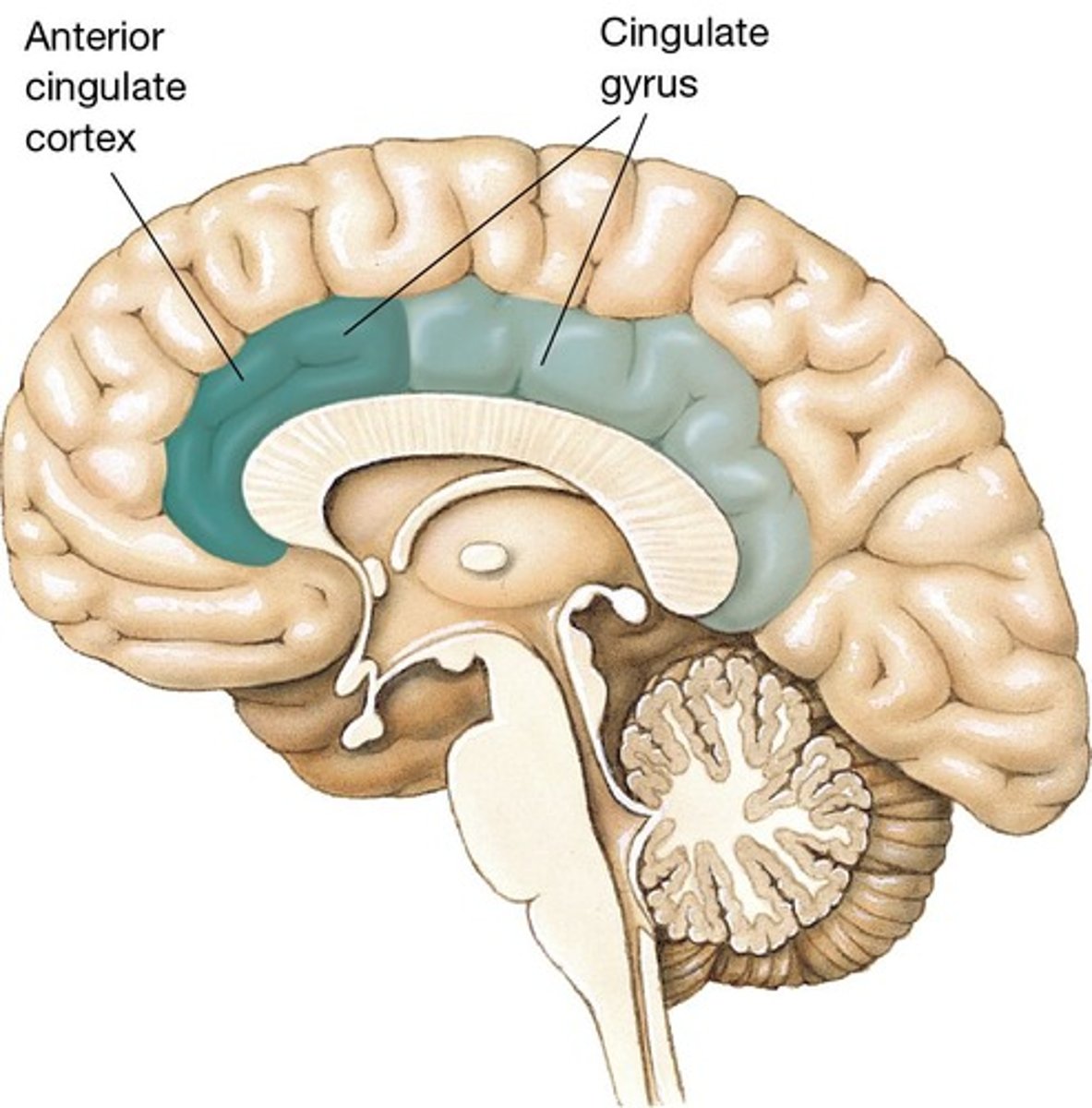
What role does the anterior cingulate cortex play in pain perception?
It may play a role in the emotional response to pain.
What is the gate-control theory of pain?
A theory suggesting that the spinal cord contains a neurological 'gate' that can block or allow pain signals to the brain.
What is Substance P?
A neuropeptide that plays a crucial role in pain transmission and modulation, encoded by the TAC1 gene.
How is Substance P released in the spinal cord?
It is released from sensory neurons that synapse with second-order neurons in the dorsal horn.
What triggers the release of Substance P?
Noxious stimuli, inflammatory mediators, and injury to tissues.
What is the somatosensory homunculus?
A representation of the body in the primary somatosensory cortex, organized somatotopically.
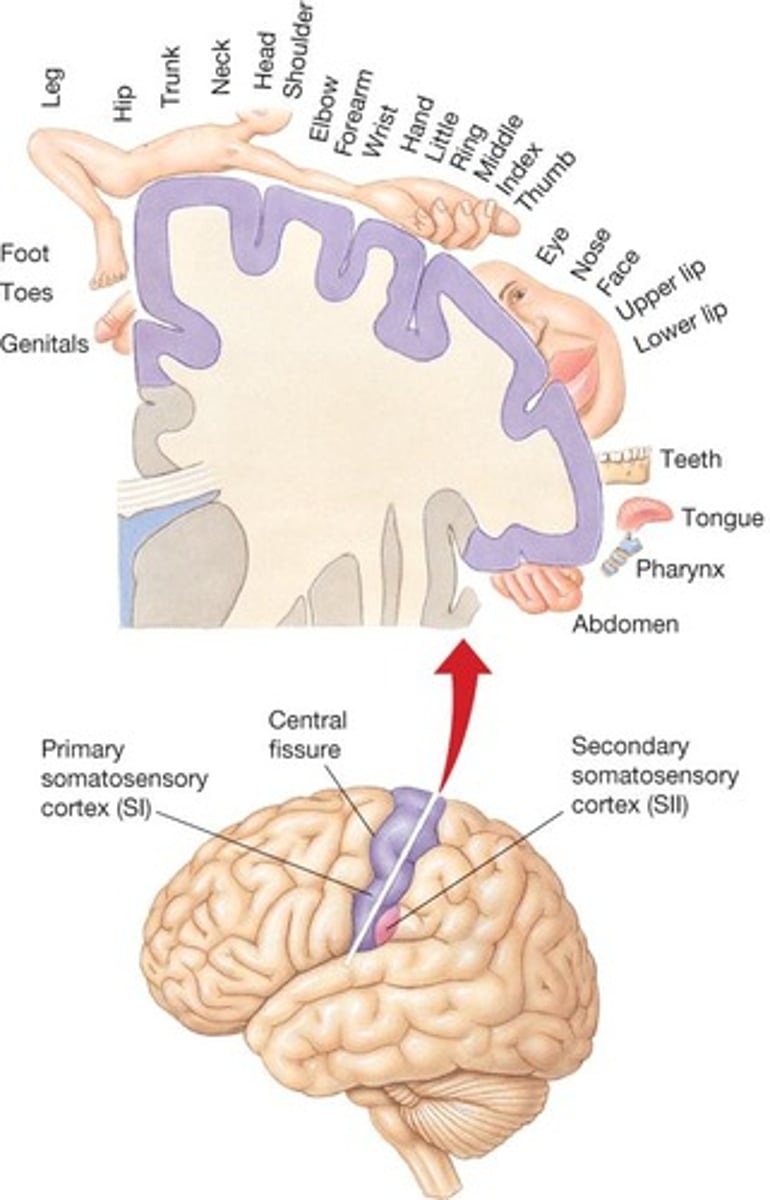
What happens when there is damage to the primary somatosensory cortex?
There are minor effects on tactual sensitivity due to numerous parallel pathways.
What are bimodal neurons?
Neurons in the posterior parietal cortex that respond to both somatosensory and visual stimuli.
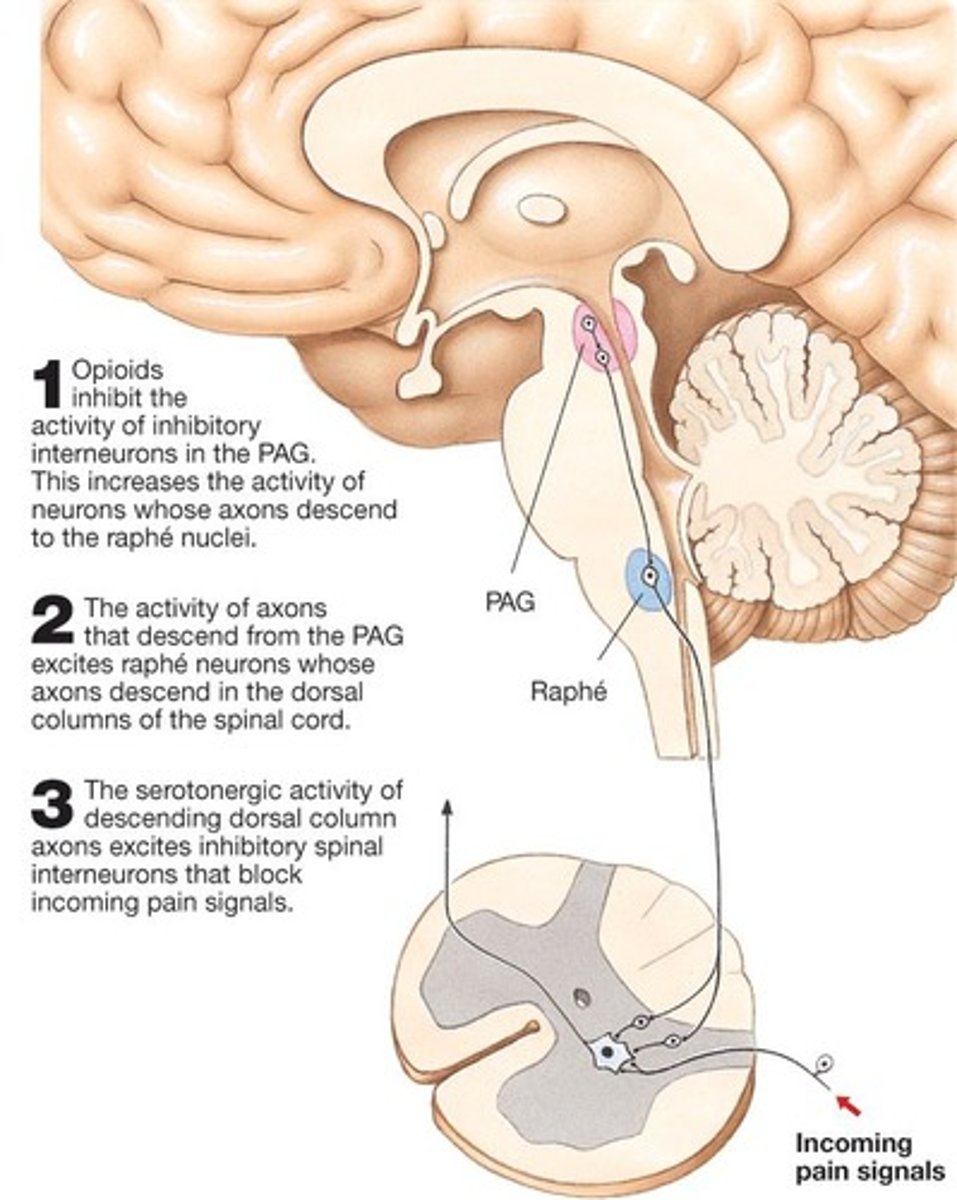
What is the significance of the descending analgesia circuit?
It involves pathways that modulate pain perception, including the PAG to raphé nuclei to dorsal columns and dorsal horns of the spinal cord.
What is the role of the PAG in pain control?
Stimulation of the PAG can cause analgesia.
What is the difference between exteroceptive and proprioceptive systems?
Exteroceptive systems respond to external stimuli (touch, temperature, pain), while proprioceptive systems provide information about body position.
What is the function of free nerve endings?
They respond to pain and temperature.
What are Pacinian corpuscles responsible for?
They are deep fast-adapting touch receptors.
What do Ruffini corpuscles detect?
They are slow-adapting touch receptors.
What is the significance of the thermal grid illusion?
It demonstrates how pain perception can be influenced by the surrounding context and stimuli.
What is Substance P and where is it primarily released from?
Substance P is a neuropeptide primarily released from primary afferent neurons.
Where in the spinal cord is Substance P released?
Substance P is released from sensory neurons that synapse with second-order neurons in the dorsal horn.
What types of cells can release Substance P in response to injury?
Non-neuronal cells such as mast cells and immune cells can release Substance P in response to tissue injury or inflammation.
What receptor does Substance P primarily act on?
Substance P primarily acts on the neurokinin-1 receptor (NK1R).
What role does Substance P play in pain pathways?
Substance P promotes the transmission of pain signals in the spinal cord and brain.
How does Substance P contribute to the inflammatory response?
Substance P facilitates the release of other pro-inflammatory substances, perpetuating inflammation and pain.
What is neuropathic pain and how is it characterized?
Neuropathic pain is severe/chronic pain from no known stimulus, often provoked by normally non-painful stimuli (allodynia).
What can increased levels of Substance P lead to in pain pathways?
Increased levels of Substance P can lead to sensitization of pain pathways, resulting in heightened pain responses.
What is allodynia?
Allodynia is a condition where even mild stimuli produce intense pain.
What are NK1 receptor antagonists used for?
NK1 receptor antagonists are used to block the action of Substance P, aiming to reduce pain transmission and improve pain management.
What is fibromyalgia?
Fibromyalgia is a complex chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive issues.
What is central sensitization in the context of fibromyalgia?
Central sensitization refers to increased sensitivity of the central nervous system (CNS) to stimuli, amplifying nociceptive signals.
How do neurotransmitter levels affect fibromyalgia?
In fibromyalgia, elevated glutamate levels and decreased serotonin levels are associated with pain processing and mood regulation.
What is the role of the HPA axis in fibromyalgia?
The HPA axis regulates stress responses; dysregulation can lead to abnormal cortisol levels affecting pain sensitivity and immune function.
What are some structural changes observed in the brains of fibromyalgia patients?
Neuroimaging studies show alterations in brain structure and function, particularly in the anterior cingulate cortex and insula.
What is the significance of the COMT gene in fibromyalgia?
The COMT gene is involved in the breakdown of catecholamines; variants can influence pain perception and emotional responses.
How do environmental factors interact with genetics in fibromyalgia?
Environmental factors like trauma and stress can interact with genetic predispositions, influencing the development of fibromyalgia.
What is the role of cytokines in fibromyalgia?
Cytokines like IL-6 and TNF-α are pro-inflammatory and are linked to heightened pain sensitivity and chronic pain conditions.
What is the function of cortisol in fibromyalgia?
Cortisol is a glucocorticoid hormone that regulates stress responses; dysregulation can amplify pain and fatigue symptoms.
What are thyroid hormones' roles in fibromyalgia?
Thyroid hormones are crucial for metabolic regulation; dysregulation can exacerbate fatigue and pain in fibromyalgia.
What is the function of neuropeptide Y (NPY) in fibromyalgia?
NPY is involved in stress response and pain modulation; altered levels can influence pain perception and emotional responses.
What is the relationship between Substance P and chronic pain?
Persistent activation of the NK1R due to excess Substance P can contribute to the maintenance of chronic pain states.
What is the role of calcitonin gene-related peptide (CGRP) in fibromyalgia?
CGRP promotes vasodilation and is involved in nociceptive processing; elevated levels may contribute to heightened pain responses.