Anatomy and Physiology II - Section 1, Lesson 2
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
What is an artery?
a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries
Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries. What happens here?
nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart.
How do arteries and veins transport blood
transport blood in two distinct circuits: the systemic circuit and the pulmonary circuit.
What do arteries do in the SYSTEMIC circuit?
Systemic arteries provide blood rich in oxygen to the body’s tissues. The blood returned to the heart through systemic veins has less oxygen since much of the oxygen carried by the arteries has been delivered to the cells.
What do arteries do in the PULMONARY circuit?
arteries carry blood low in oxygen exclusively to the lungs for gas exchange
What do veins do in the PULMONARY circuit?
return freshly oxygenated blood from the lungs to the heart to be pumped back out into systemic circulation.
What do veins do in the systemic circuit?
The blood returned to the heart through systemic veins has less oxygen since much of the oxygen carried by the arteries has been delivered to the cells. They go back to the heart for reoxygenation
Why do arteries and arterioles have thicker walls and smaller lumens then veins?
because they are closer to the heart and receive blood that is surging at a far greater pressure, small lumens a characteristic that helps to maintain the pressure of blood moving through the system
What is a lumen (vessel)?
a hollow passageway through which blood flows
How thick are arteries?
Their size and wall thickness vary depending on their proximity to the heart (i.e., large arteries with thick elastic walls carry blood being pumped directly from the heart, and arteries smaller in diameter with thinner walls deliver blood to the extremities).
What are the 3 main types of arteries defined?
elastic arteries, muscular arteries, and arterioles
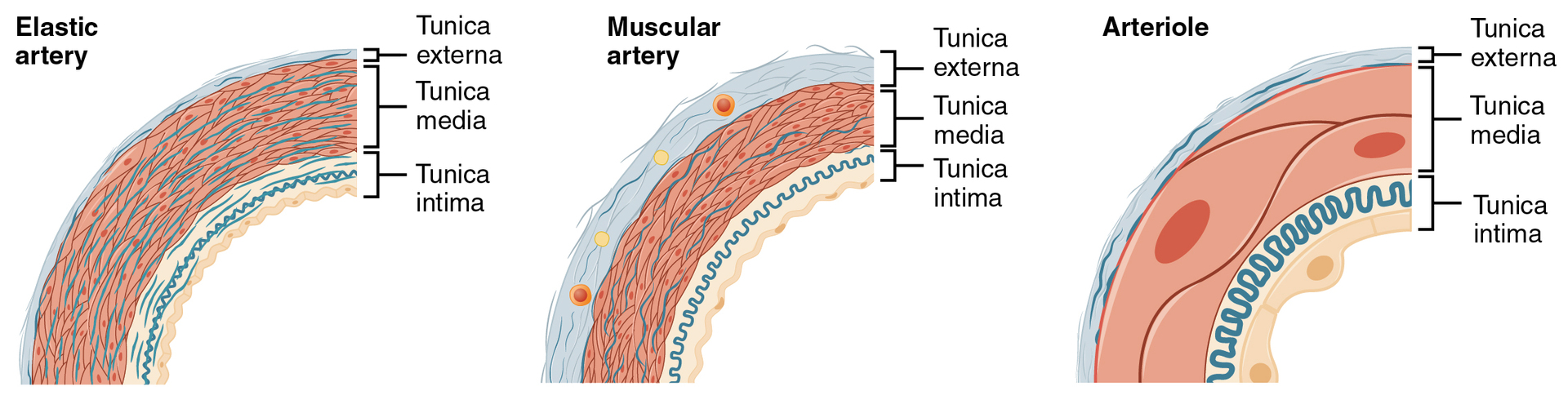
The arteries close to the heart have the thickest walls, containing a high percentage of elastic fibers in all three of their tunics. What type are these?
elastic artery (Figure 20.4). Vessels larger than 10 mm in diameter are typically elastic. Their abundant elastic fibers allow them to expand as blood pumped from the ventricles passes through them and then recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase, and blood pressure would rise to even higher levels, which would, in turn, require the heart to pump harder to increase the volume of blood expelled by each pump (the stroke volume) and maintain adequate pressure and flow. Artery walls would have to become even thicker in response to this increased pressure.
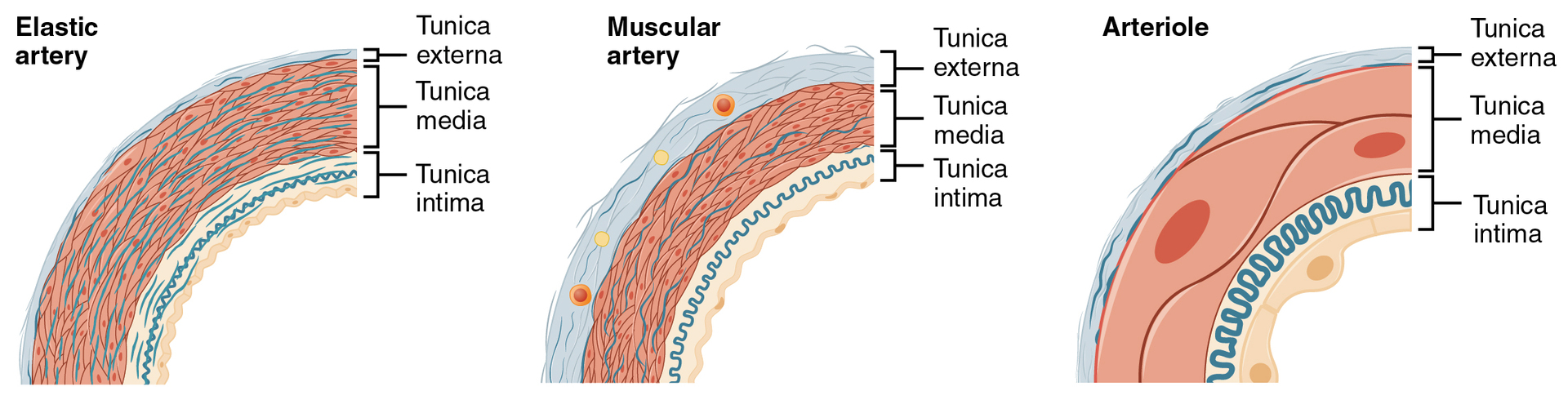
The elastic nature of artery walls help in what way?
Their abundant elastic fibers allow them to expand as blood pumped from the ventricles passes through them and then recoil after the surge has passed.The elastic recoil of the vascular wall helps to maintain the pressure gradient that drives the blood through the arterial system.
Why is an elastic artery also known as a conducting artery?
An elastic artery is also known as a conducting artery because the large diameter of the lumen enables it to accept a large volume of blood from the heart and conduct it to smaller branches.
what happens farther from the heart, where the surge of blood has dampened
the percentage of elastic fibers in an artery’s tunica intima decreases, and the amount of smooth muscle in its tunica media increases. The artery at this point is described as a muscular artery
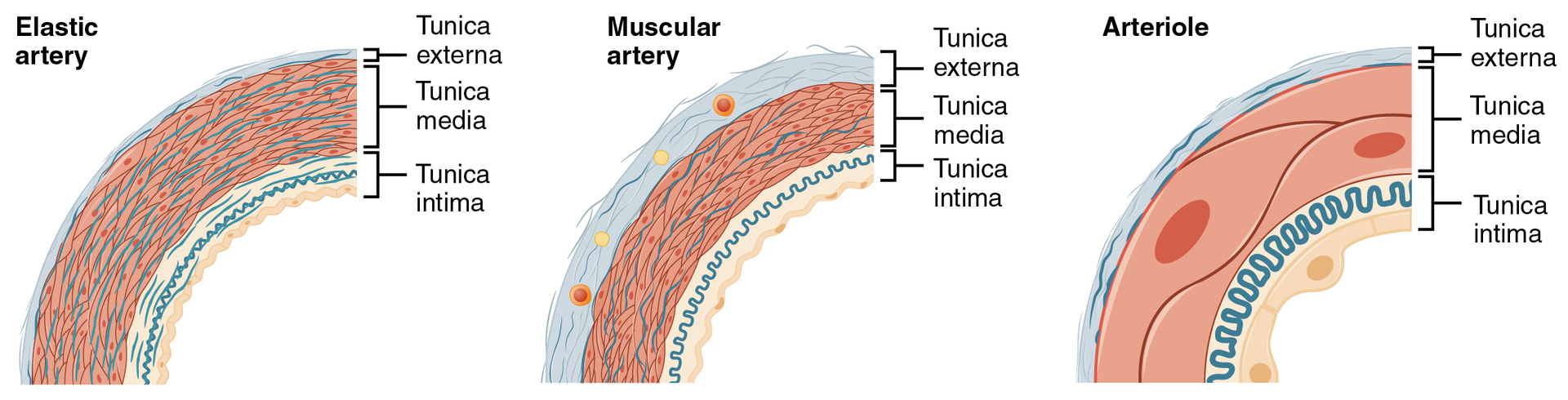
What is the diameter like for muscular arteries and what is their elasticity like?
The diameter of muscular arteries typically ranges from 0.1 mm to 10 mm. Their thick tunica media allows muscular arteries to play a leading role in vasoconstriction. In contrast, their decreased quantity of elastic fibers limits their ability to expand. Fortunately, because the blood pressure has eased by the time it reaches these more distant vessels, elasticity has become less important.
What is an arteriole?
a very small artery that leads to a capillary. Arterioles have the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica intima is intact. The tunica media is restricted to one or two smooth muscle cell layers in thickness. The tunica externa remains but is very thin (see Figure 20.4).
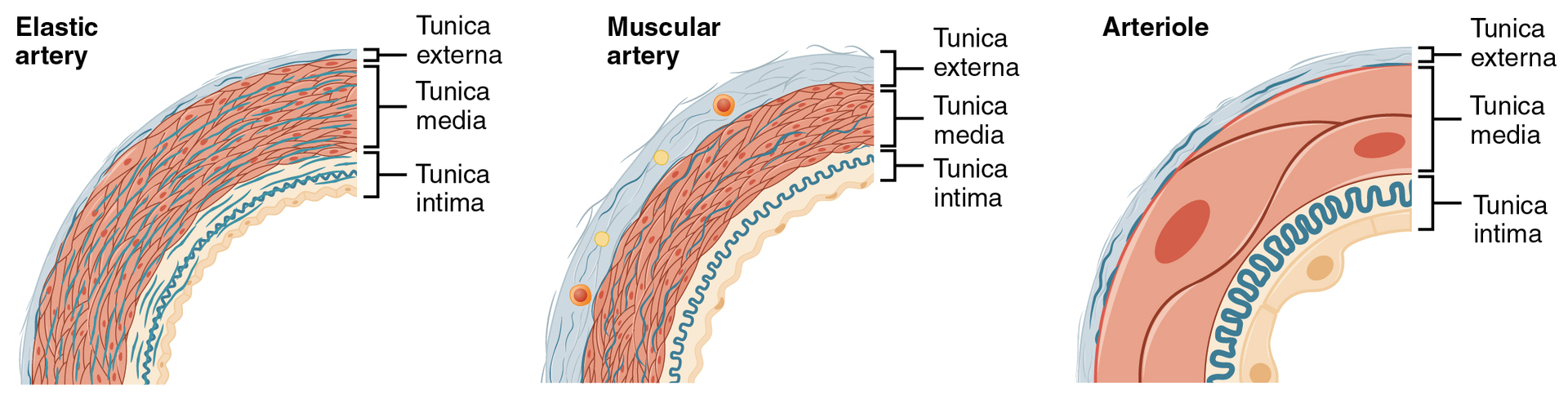
how big is the lumen in arterioles?
averaging 30 micrometers or less in diameter. The precise diameter of the lumen of an arteriole at any given moment is determined by neural and chemical controls, and vasoconstriction and vasodilation in the arterioles are the primary mechanisms for the distribution of blood flow.
What can arterioles do for blood flow?
arterioles are critical in slowing down—or resisting—blood flow and, thus, causing a substantial drop in blood pressure. Because of this, you may see them referred to as resistance vessels. they will be the primary site of both resistance and regulation of blood pressure.
How are the muscle fibers in arterioles?
normally slightly contracted, causing arterioles to maintain a consistent muscle tone—in this case, referred to as vascular tone—in a similar manner to the muscular tone of skeletal muscle.
what is a capillary?
a microscopic channel that supplies blood to the tissues, a process called perfusion. The exchange of gases and other substances occurs between the blood in capillaries and the surrounding cells and their tissue fluid (interstitial fluid).
What is the diameter of a capillary?
ranges from 5–10 micrometers; the smallest are just barely wide enough for an erythrocyte to squeeze through
What is flow through capillaries often described as
microcirculation
What do the walls of capillaries consist of?
endothelial layer surrounded by a basement membrane with occasional smooth muscle fibers. There is some variation in wall structure: In a large capillary, several endothelial cells bordering each other may line the lumen; in a small capillary, there may be only a single cell layer that wraps around to contact itself.
How do capillaries function?
their walls must be leaky, allowing substances to pass through. There are three major types of capillaries, which differ according to their degree of “leakiness:”
What are the 3 types of capillaries that differ in leakiness?
continuous, fenestrated, and sinusoid capillaries
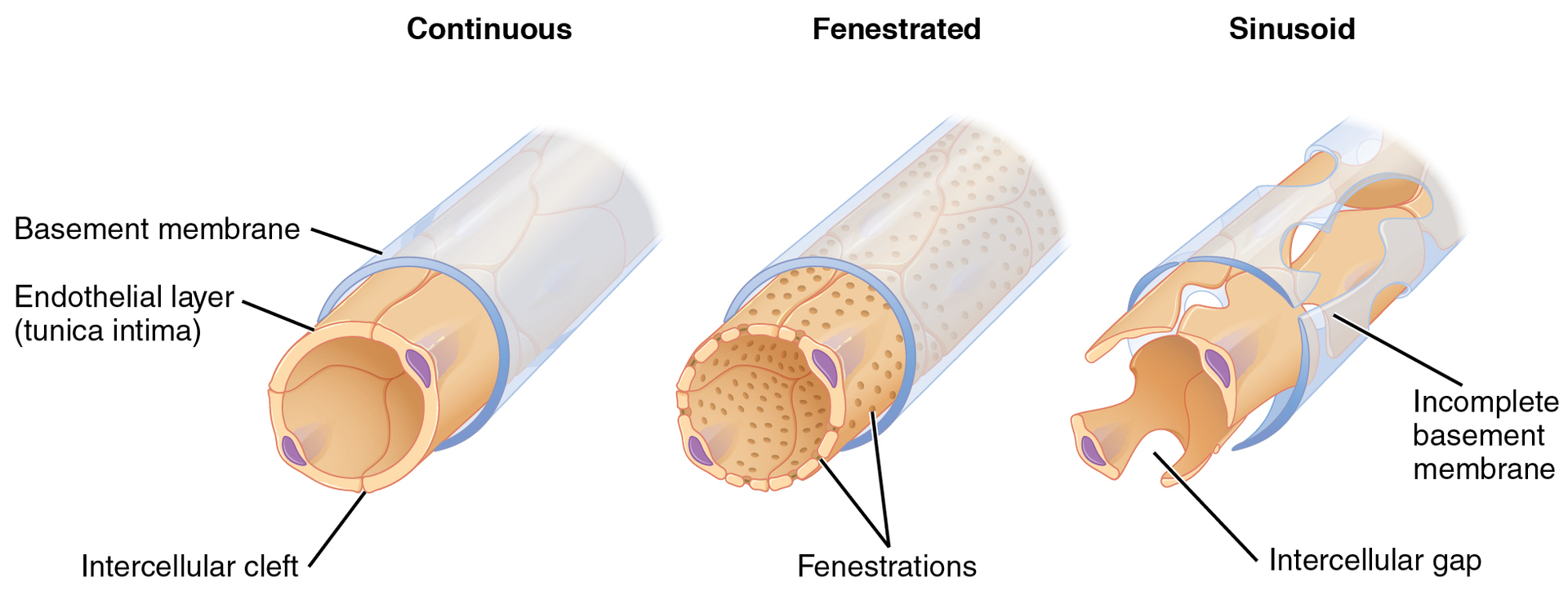
What is the most common type of capillary?
the continuous capillary
Where can the continuous capillary be found?
in almost all vascularized tissues.
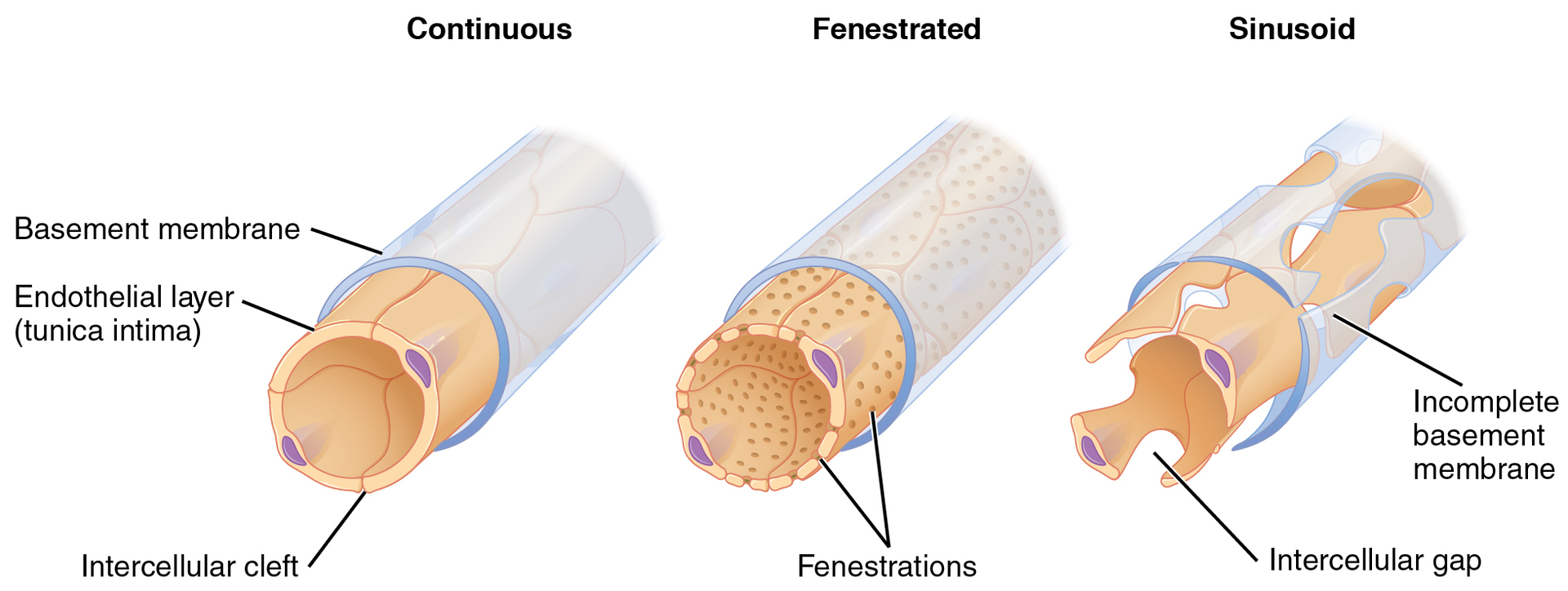
What are the walls like in continuous capillaries?
a complete endothelial lining with tight junctions between endothelial cells. Although a tight junction is usually impermeable and only allows for the passage of water and ions, they are often incomplete in capillaries, leaving intercellular clefts that allow for the exchange of water and other very small molecules between the blood plasma and the interstitial fluid.
What are substances that can be passed between cells?
metabolic products, such as glucose, water, and small hydrophobic molecules, like gases and hormones, as well as various leukocytes
What are continuous vessels not associated with the brain like?
are rich in transport vesicles, contributing to either endocytosis or exocytosis.
What are continuous vessels associated with the brain like?
part of the blood-brain barrier. Here, there are tight junctions and no intercellular clefts, plus a thick basement membrane and astrocyte extensions called end feet; these structures combine to prevent the movement of nearly all substances.
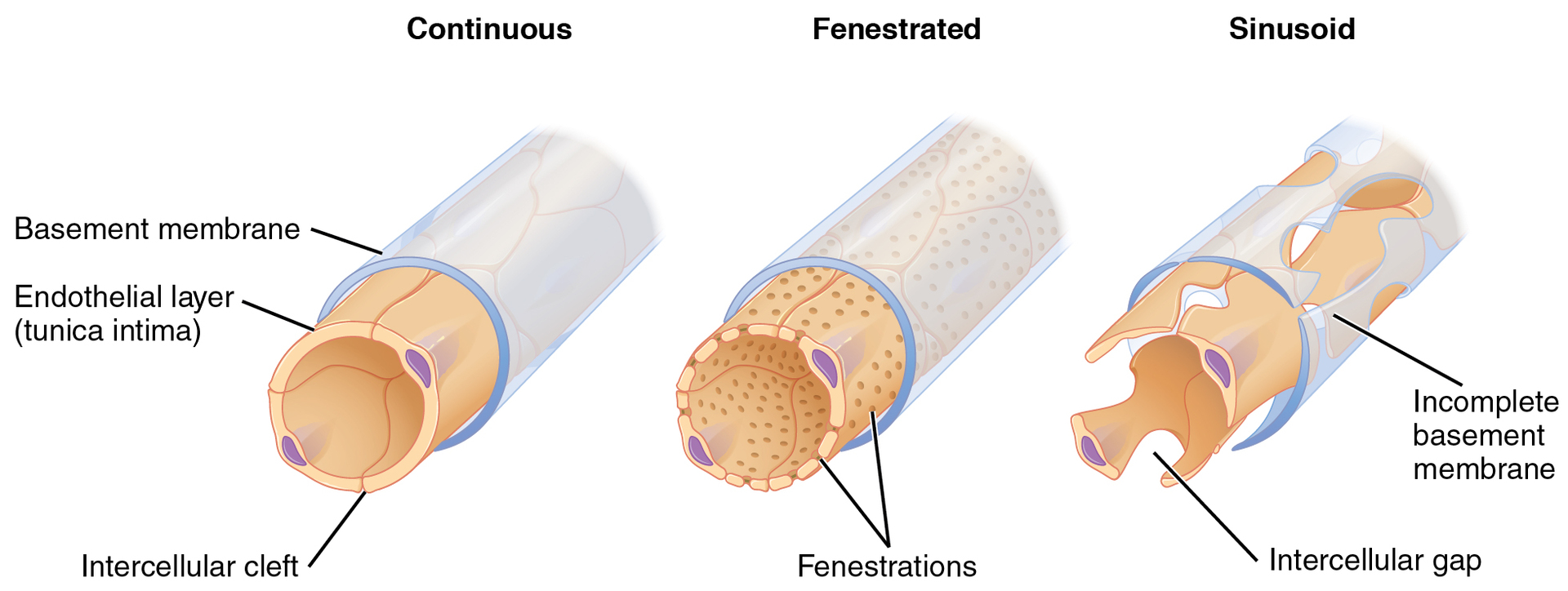
What are fenestrated capillaries like?
has pores (or fenestrations) in addition to tight junctions in the endothelial lining. These make the capillary permeable to larger molecules. The number of fenestrations and their degree of permeability vary, however, according to their location
Where are fenestrated capillaries common?
the small intestine (discussed in the Digestive System section), which is the primary site of nutrient absorption, as well as in the kidneys (discussed in the Urinary System section), which filter the blood. They are also found in the choroid plexus of the brain and many endocrine structures, including the hypothalamus, pituitary, pineal, and thyroid glands.
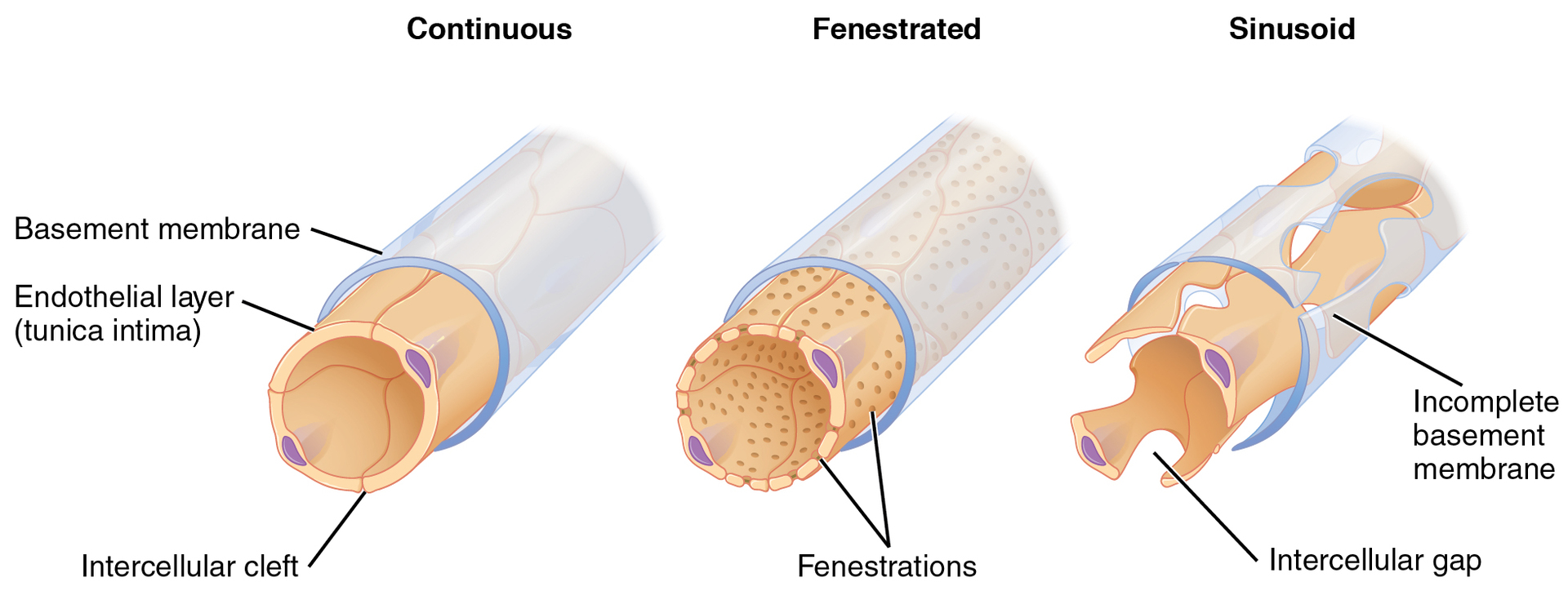
sinusoid capillary (the least common capillary are what? do what?
Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations. This gives them an appearance not unlike Swiss cheese. These very large openings allow for the passage of the largest molecules, including plasma proteins and even cells.
What is blood flow like in sinusoid capillaries?
very slow, allowing more time for the exchange of gases, nutrients, and wastes.
Where can sinusoid capillaries be found?
the liver and spleen, bone marrow, lymph nodes (where they carry lymph, not blood), and many endocrine glands, including the pituitary and adrenal glands.
when bone marrow forms new blood cells, the cells must enter the blood supply. What is the only way they can do this?
through the large openings of a sinusoid capillary; they cannot pass through the small openings of continuous or fenestrated capillaries.
Why does the liver need sinusoid capillaries?
The liver requires sinusoid capillaries because they have large gaps between endothelial cells, allowing the passage of large molecules (like proteins), blood cells, and facilitating direct contact with Kupffer cells for filtering and detoxification. This structure supports the liver’s roles in detoxification, protein synthesis, and nutrient exchange.
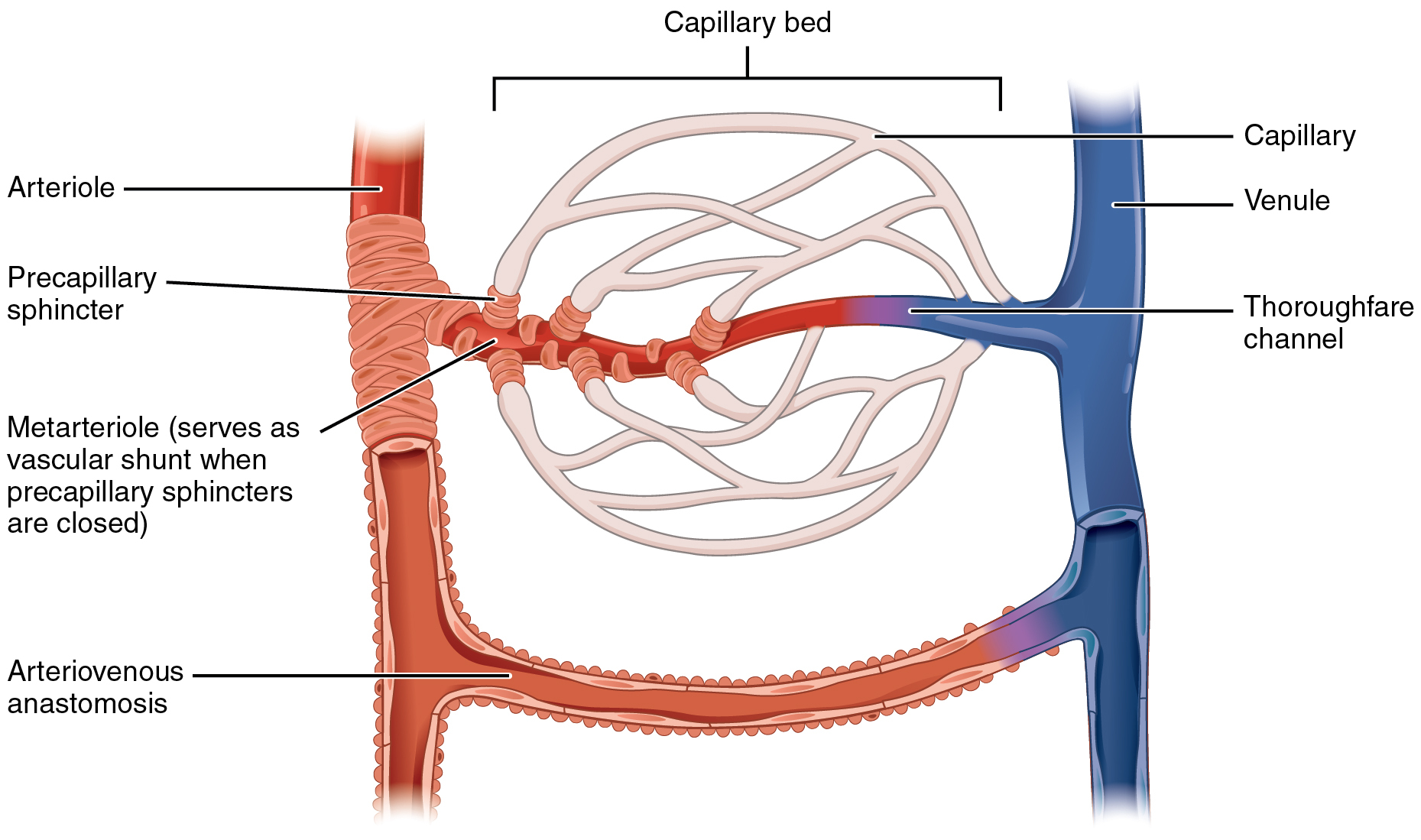
what is a metaarteriole?
a type of vessel that has structural characteristics of both an arteriole and a capillary. Slightly larger than the typical capillary, the smooth muscle of the tunica media of the metarteriole is not continuous but forms rings of smooth muscle (sphincters) prior to the entrance to the capillaries.
Where can metaarterioles be found?
they arise from a terminal arteriole and branches to supply blood to a capillary bed that may consist of 10–100 capillaries.
What tightly regulates the flow of blood from a metarteriole to the capillaries it supplies?
precapillary sphincters, circular smooth muscle cells that surround the capillary at its origin with the metarteriole. Their function is critical: If all of the capillary beds in the body were to open simultaneously, they would collectively hold every drop of blood in the body and there would be none in the arteries, arterioles, venules, veins, or the heart itself.
What happens to precapillary sphincters when the surrounding tissues need oxygen and have excess waste products
the precapillary sphincters open, allowing blood to flow through and exchange to occur before closing once more
what happens when all of the precapillary sphincters in a capillary bed are closed (as they are usually)?
blood will flow from the metarteriole directly into a thoroughfare channel and then into the venous circulation, bypassing the capillary bed entirely.
what creates what is known as a vascular shunt
If all of the precapillary sphincters in a capillary bed are closed, blood will flow from the metarteriole directly into a thoroughfare channel and then into the venous circulation, bypassing the capillary bed entirely
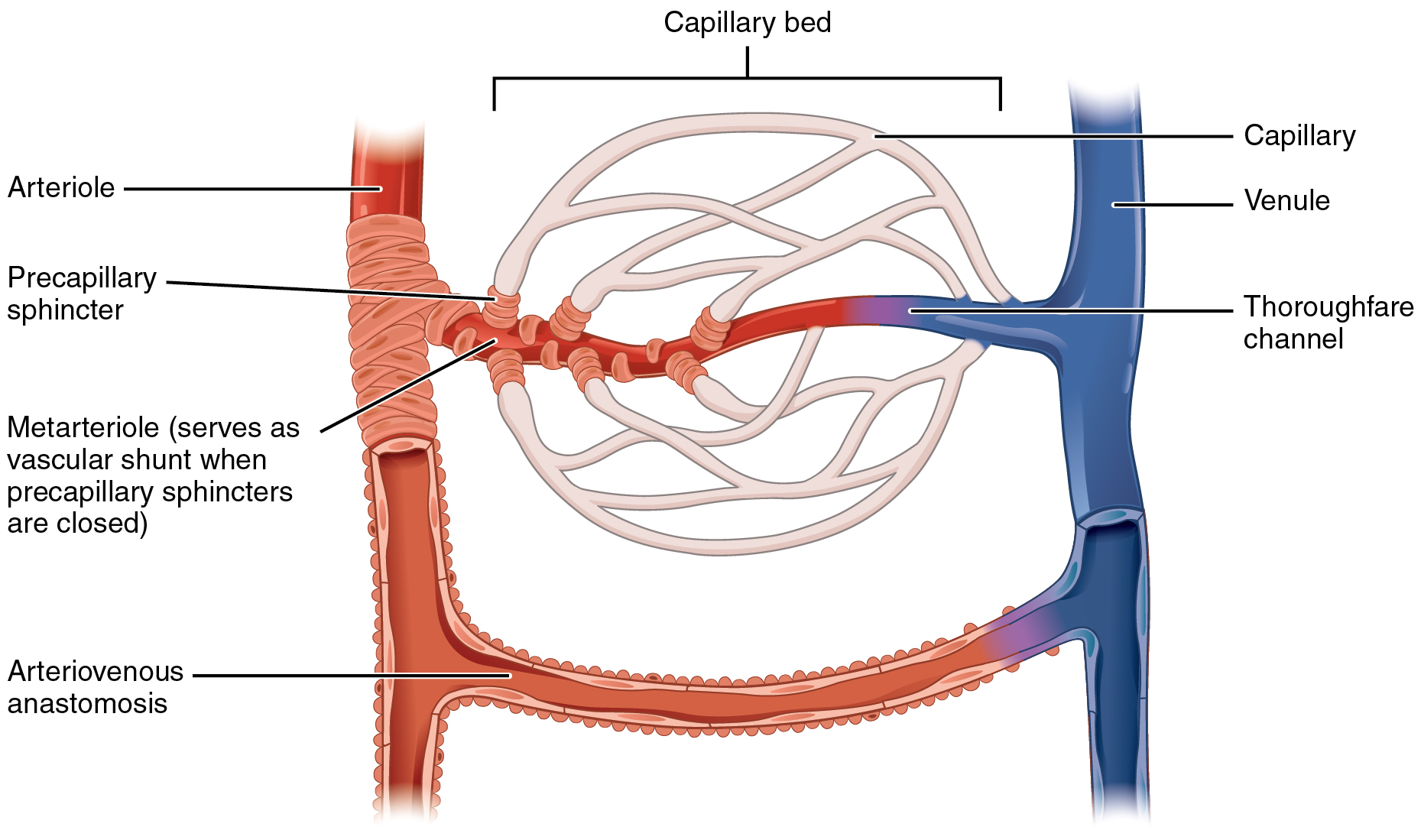
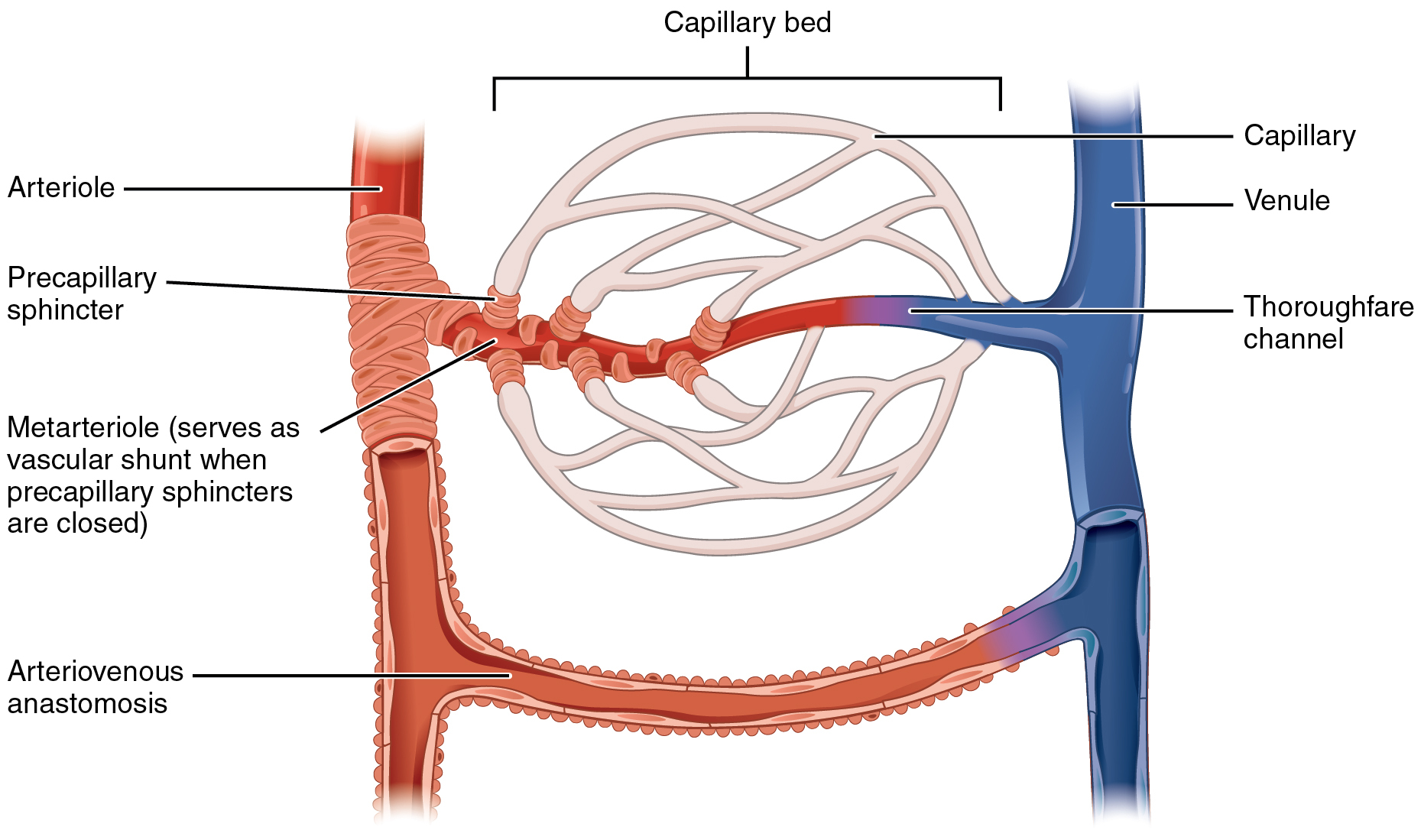
what may bypass the capillary bed and lead directly to the venous system
an arteriovenous anastomosis
what process may blood pass through from arterioles to capillaries and from capillaries to venules
vasomotion
What is vasomotion?
the intermittent contraction and relaxation of the precapillary sphincters that pushes blood from a metarteriole through to a capillary.
What controls vasomotion?
chemicals released by endothelial cells. Blood may alternately pass from arterioles directly to venules through a thoroughfare channel, therefore bypassing capillaries
Blood may alternately pass from arterioles directly to venules through a thoroughfare channel, therefore bypassing capillaries. How does this happen?
the smooth-muscle-covered proximal end of a metarteriole contracts and relaxes to regulate blood flow.
In some regions of the body, such as the liver, blood flows from one capillary network to another via a portal vein. What is this called?
a portal system. The name of the portal system refers to the location of the final capillary network (e.g., hepatic portal system).
How is blood flow through a capillary like?
it moves with an irregular, pulsating flow. This pattern (called vasomotion)
What regulates vasomotion in capillaries
chemical signals that are triggered in response to changes in internal conditions, such as oxygen, carbon dioxide, hydrogen ion, and lactic acid levels.
When might you expect vasomotion through capillaries to occur
For example, during strenuous exercise, when oxygen levels decrease and carbon dioxide, hydrogen ion, and lactic acid levels all increase, the capillary beds in skeletal muscle are open, as they would be in the digestive system when nutrients are present in the digestive tract.
when might you expect vasomotion to slow down
During sleep or rest periods, vessels in both areas are largely closed; they open only occasionally to allow oxygen and nutrient supplies to travel to the tissues to maintain basic life processes.
what is a thoroughfare channel
continuation of the metarteriole that enables blood to bypass a capillary bed and flow directly into a venule, creating a vascular shunt
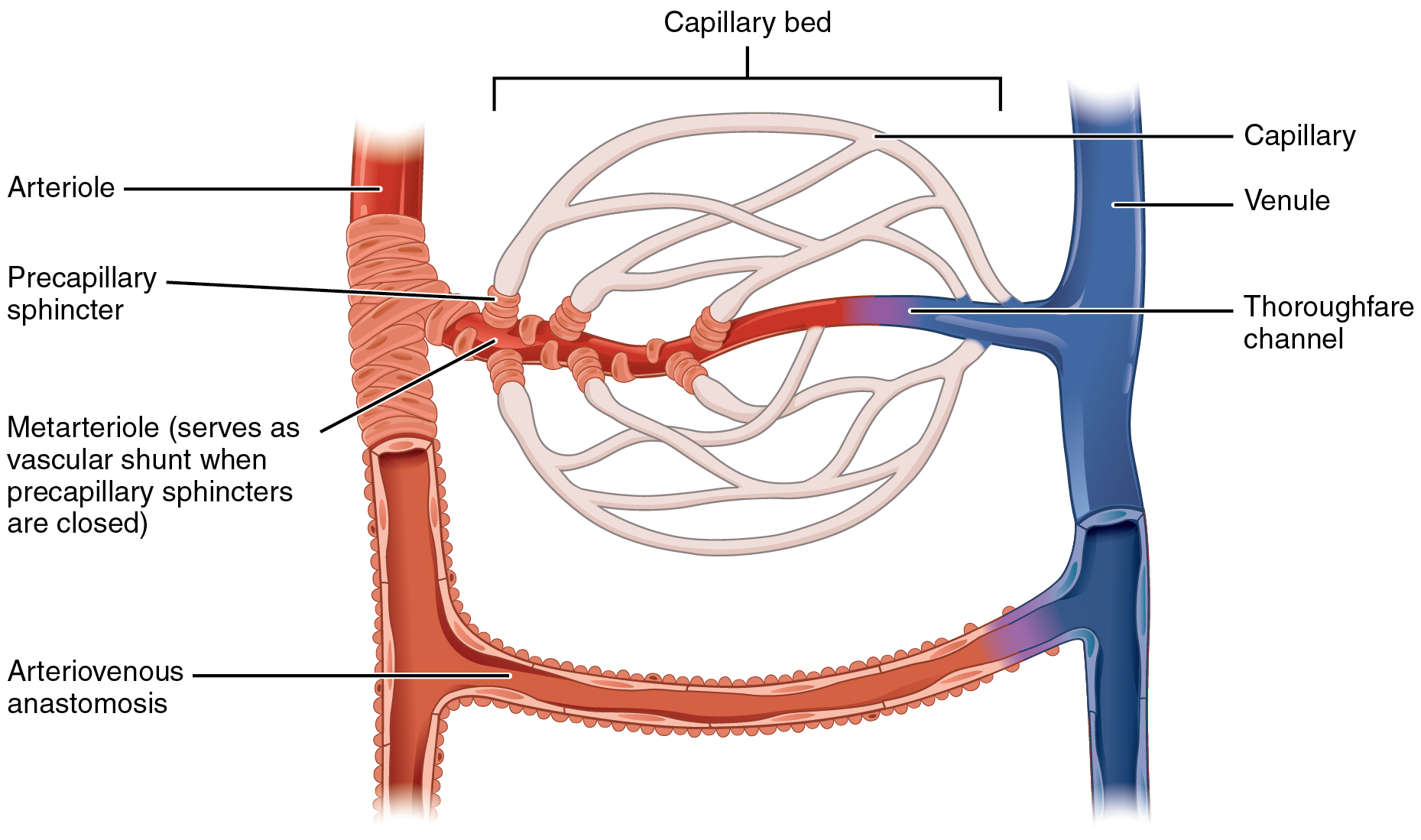
arteriovenous anastomosis
short vessel connecting an arteriole directly to a venule and bypassing the capillary beds
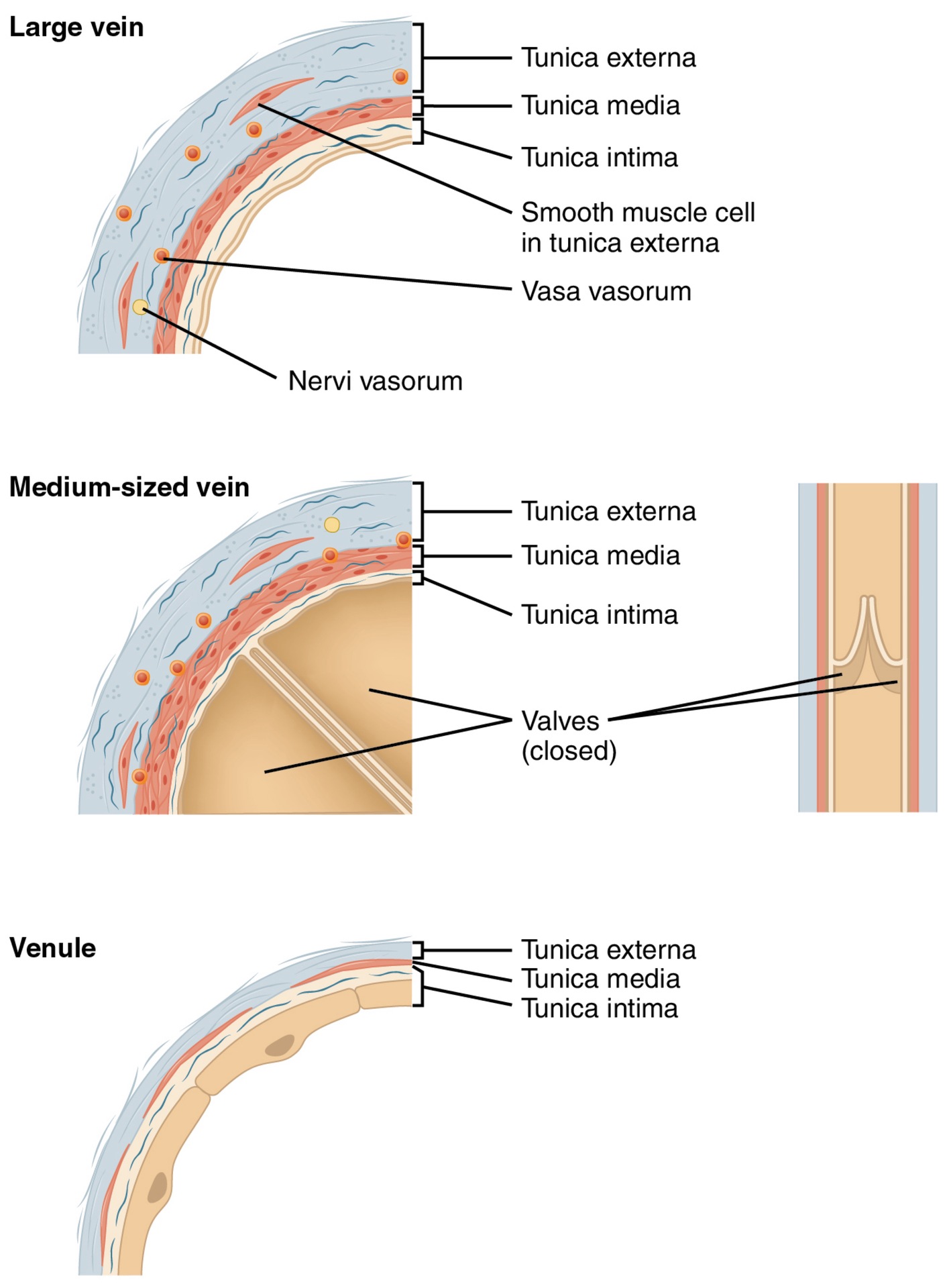
What is a vein?
a blood vessel that conducts blood toward the heart. Compared to arteries, veins are thin-walled vessels with large and irregular lumens (see Figure 20.7).
why are larger veins commonly equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow toward the capillaries caused by the inherent low blood pressure in veins as well as the pull of gravity?
Because they are low-pressure vessels
what is size like for veins?
size varies from about 0.5 mm in diameter to 3 cm, depending on their proximity to the heart
what are vein walls like?
generally have very thin walls in relation to their diameter, with large lumen. In certain regions, veins can be seen to widen, forming vascular or venous sinuses, structurally different from regular veins. They have thin endothelial walls with a complete lack of smooth muscle, leaving them reliant upon surrounding connective tissue for support.
What are superficial veins? where can they be found?
spread throughout the subcutaneous layer, deep to the skin
Where can deep veins be found?
between skeletal muscles
what are the connections that exist between superficial and deep veins calls?
anastomotic veins.
What is a venule
an extremely small vein
How big are venules?
8–100 micrometers in diameter.
how do venules turn to veins?
Postcapillary venules join multiple capillaries exiting from a capillary bed. Multiple venules join to form veins.
What are venule walls like?
The walls of venules consist of endothelium, a thin middle layer with a few muscle cells and elastic fibers, plus an outer layer of connective tissue fibers that constitute a very thin tunica externa
What are the primary sites of emigration or diapedesis, in which the white blood cells adhere to the endothelial lining of the vessels and then squeeze through adjacent cells to enter the tissue fluid.
Venules, as well as capillaries
why do hands and feet feel cold and look pale in very cold temperatures
The circulatory system has a number of built-in bypass routes that allow blood to be diverted from an artery to a vein directly, without passing through the capillary beds. This allows the body to adapt blood flow to cope with changes in the environment. For example, when the outside temperature is very low, blood is diverted away from the hands and feet to conserve the core body temperature.
how may blood pass from arterioles to capillaries and from capillaries to venules
by a process known as vasomotion. Vasomotion is the intermittent contraction and relaxation of the precapillary sphincters that pushes blood from a metarteriole through to a capillary. Vasomotion is controlled by chemicals released by endothelial cells. Blood may alternately pass from arterioles directly to venules through a thoroughfare channel, therefore bypassing capillaries. In this instance, the smooth muscle covering the proximal end of a metarteriole contracts and relaxes to regulate blood flow.
what refers to the location of the final capillary network
The name of the portal system (e.g, hepatic portal system)
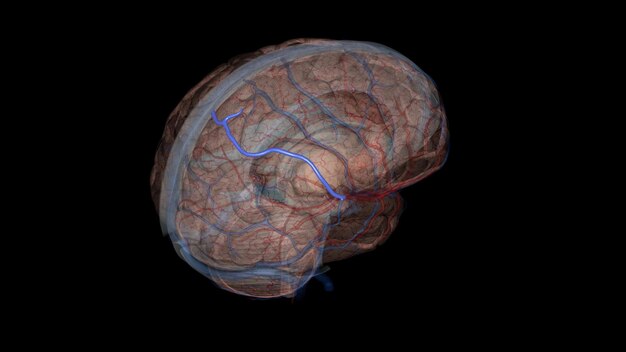
what are anastomotic veins in the brain:
the vein of Trolard, the largest superficial vein on the lateral surface of the parietal or frontal lobe that connects the superior sagittal sinus and the superficial middle cerebral vein (of Sylvius)
what is the primary purpose of the cardiovascular system
to circulate gases, nutrients, wastes, and other substances to and from the cells of the body.
Small molecules, such as gases, lipids, and lipid-soluble molecules, can diffuse directly through the membranes of the endothelial cells of the capillary wall. how can they do this?
Glucose, amino acids, and ions—including sodium, potassium, calcium, and chloride—use transporters to move through specific channels in the membrane by facilitated diffusion. Glucose, ions, and larger molecules may also leave the blood through intercellular clefts. Larger molecules can pass through the pores of fenestrated capillaries, and even large plasma proteins can pass through the great gaps in the sinusoids. Some large proteins in blood plasma can move into and out of the endothelial cells packaged within vesicles by endocytosis and exocytosis. Water moves by osmosis.
The mass movement of fluids into and out of capillary beds requires a transport mechanism far more efficient than mere diffusion (bulk flow). What does this involve?
two pressure-driven mechanisms: Volumes of fluid move from an area of higher pressure in a capillary bed to an area of lower pressure in the tissues via filtration. In contrast, the movement of fluid from an area of higher pressure in the tissues into an area of lower pressure in the capillaries is reabsorption. Two types of pressure interact to drive each of these movements: hydrostatic pressure and osmotic pressure.
What is the primary force driving fluid transport between the capillaries and tissues
(Capillary) hydrostatic pressure, which can be defined as the pressure of any fluid enclosed in a space
What is blood hydrostatic pressure?
the force exerted by the blood confined within blood vessels or heart chambers. Even more specifically, the pressure exerted by blood against the wall of a capillary is called capillary hydrostatic pressure (CHP) and is the same as capillary blood pressure. CHP is the force that drives fluid out of capillaries and into the tissues.
What happens to the hydrostatic pressure in the interstitial fluid as fluid exits a capillary and moves into tissues
the hydrostatic pressure in the interstitial fluid correspondingly rises.
As fluid exits a capillary and moves into tissues, the hydrostatic pressure in the interstitial fluid correspondingly rises. What is this called?
the interstitial fluid hydrostatic pressure (IFHP)
Generally, the capillary hydrostatic pressure (CHP) originating from the arterial pathways is considerably higher than the interstitial fluid hydrostatic pressure (IFHP). Why
because lymphatic vessels are continually absorbing excess fluid from the tissues. Thus, fluid generally moves out of the capillary and into the interstitial fluid. This process is called filtration.
CHP is higher because it originates from the arterial side, where blood is under pressure from the heart’s pumping action. In contrast, IFHP is typically low or even slightly negative, as the interstitial space has no active pump and fluid is being drained by lymphatic vessels. This pressure difference helps drive fluid out of capillaries and into tissues for nutrient and waste exchange.
What is the net pressure that drives reabsorption—the movement of fluid from the interstitial fluid back into the capillaries
osmotic pressure (sometimes referred to as oncotic pressure). Whereas hydrostatic pressure forces fluid out of the capillary, osmotic pressure draws fluid back in
What determines osmotic pressure?
osmotic concentration gradients, that is, the difference in the solute-to-water concentrations in the blood and tissue fluid. A region higher in solute concentration (and lower in water concentration) draws water across a semipermeable membrane from a region higher in water concentration (and lower in solute concentration).
in osmotic pressure in blood and tissue fluid, the formed elements of blood do not contribute to osmotic concentration gradients. What does?
the plasma proteins that play the key role. Solutes also move across the capillary wall according to their concentration gradient, but overall, the concentrations should be similar and not have a significant impact on osmosis.
Because of their large size and chemical structure, plasma proteins are not truly solutes. What does this mean?
they do not dissolve but are dispersed or suspended in their fluid medium, forming a colloid rather than a solution.
What is the pressure created by the concentration of colloidal proteins in the blood called
the blood colloidal osmotic pressure (BCOP). Its effect on capillary exchange accounts for the reabsorption of water
The plasma proteins suspended in blood cannot move across the semipermeable capillary cell membrane, and so they remain in the plasma. What is a result of this?
blood has a higher colloidal concentration and lower water concentration than tissue fluid. It therefore attracts water. We can also say that the BCOP is higher than the interstitial fluid colloidal osmotic pressure (IFCOP)which is always very low because interstitial fluid contains few proteins.
BCOP is higher than the interstitial fluid colloidal osmotic pressure (IFCOP), which is always very low because interstitial fluid contains few proteins. Thus
water is drawn from the tissue fluid back into the capillary, carrying dissolved molecules with it. This difference in colloidal osmotic pressure accounts for reabsorption.
What is the normal unit used to express pressures within the cardiovascular system
millimeters of mercury (mm Hg).
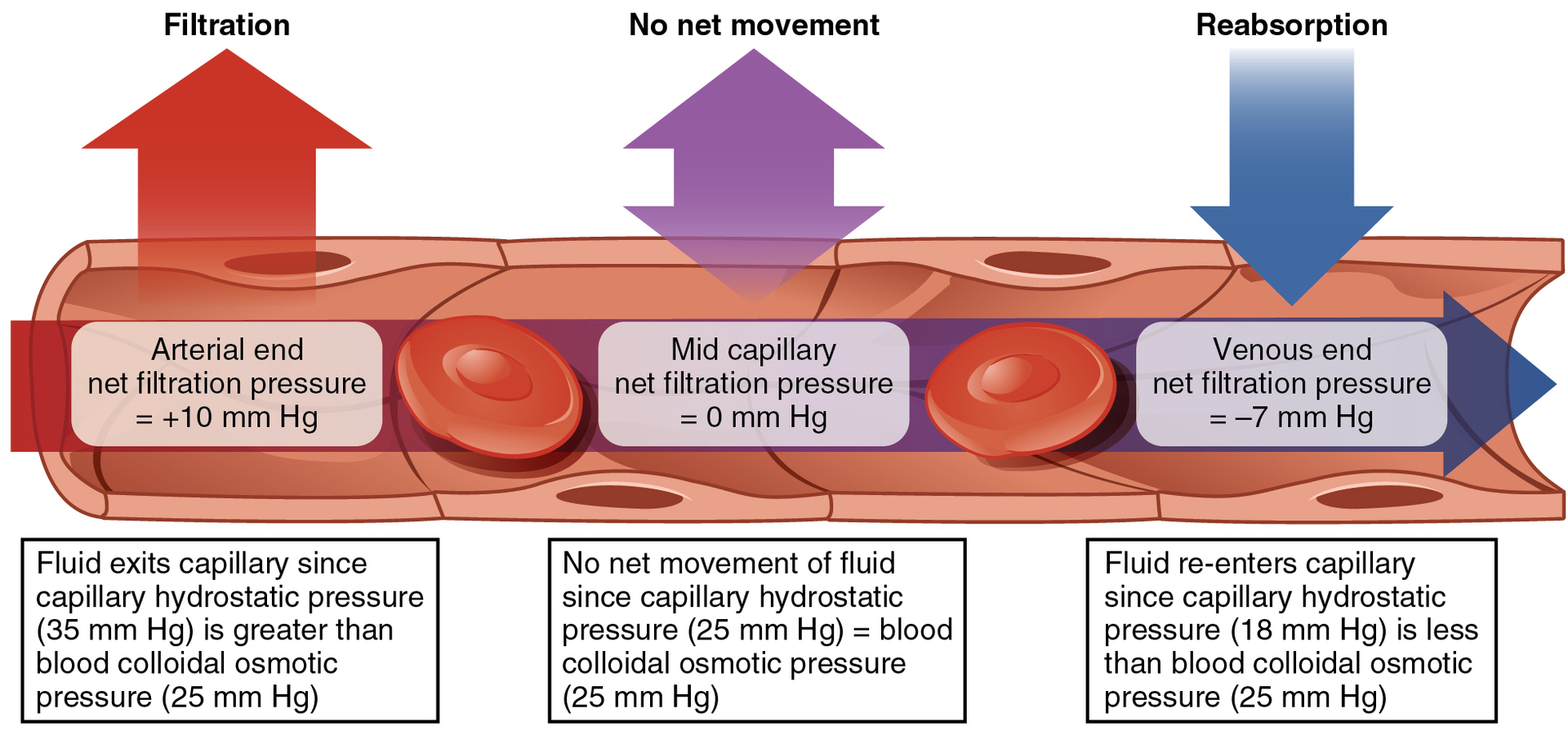
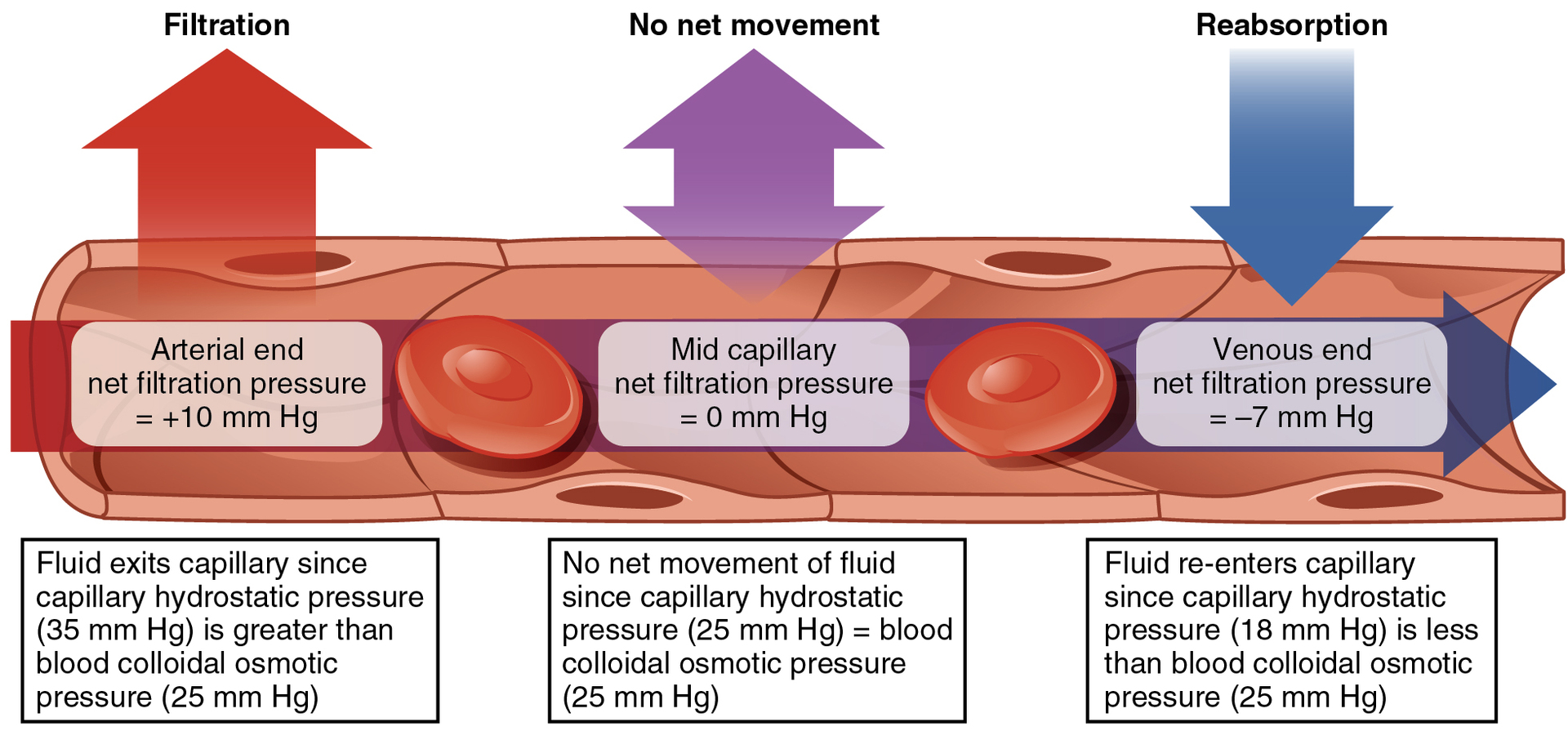
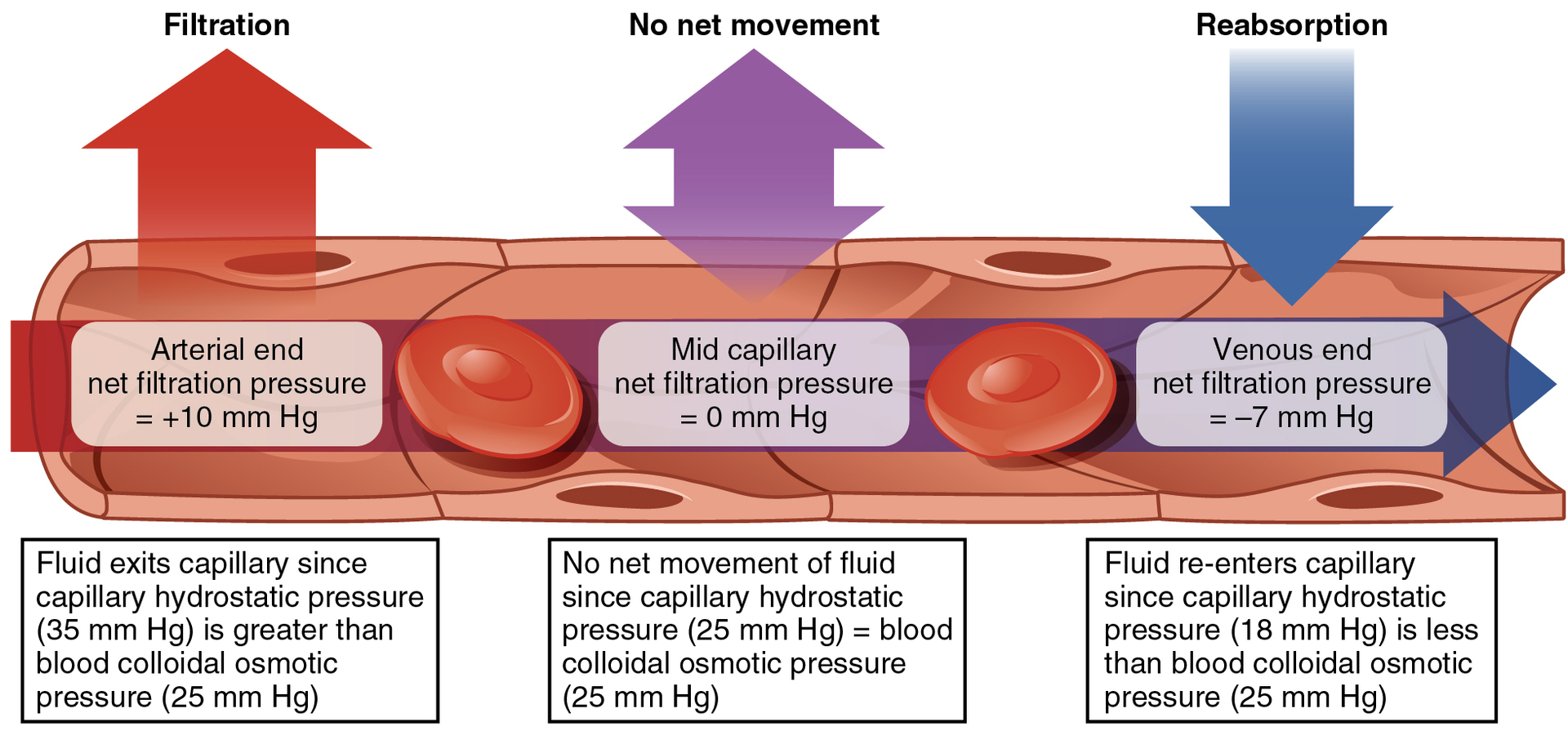
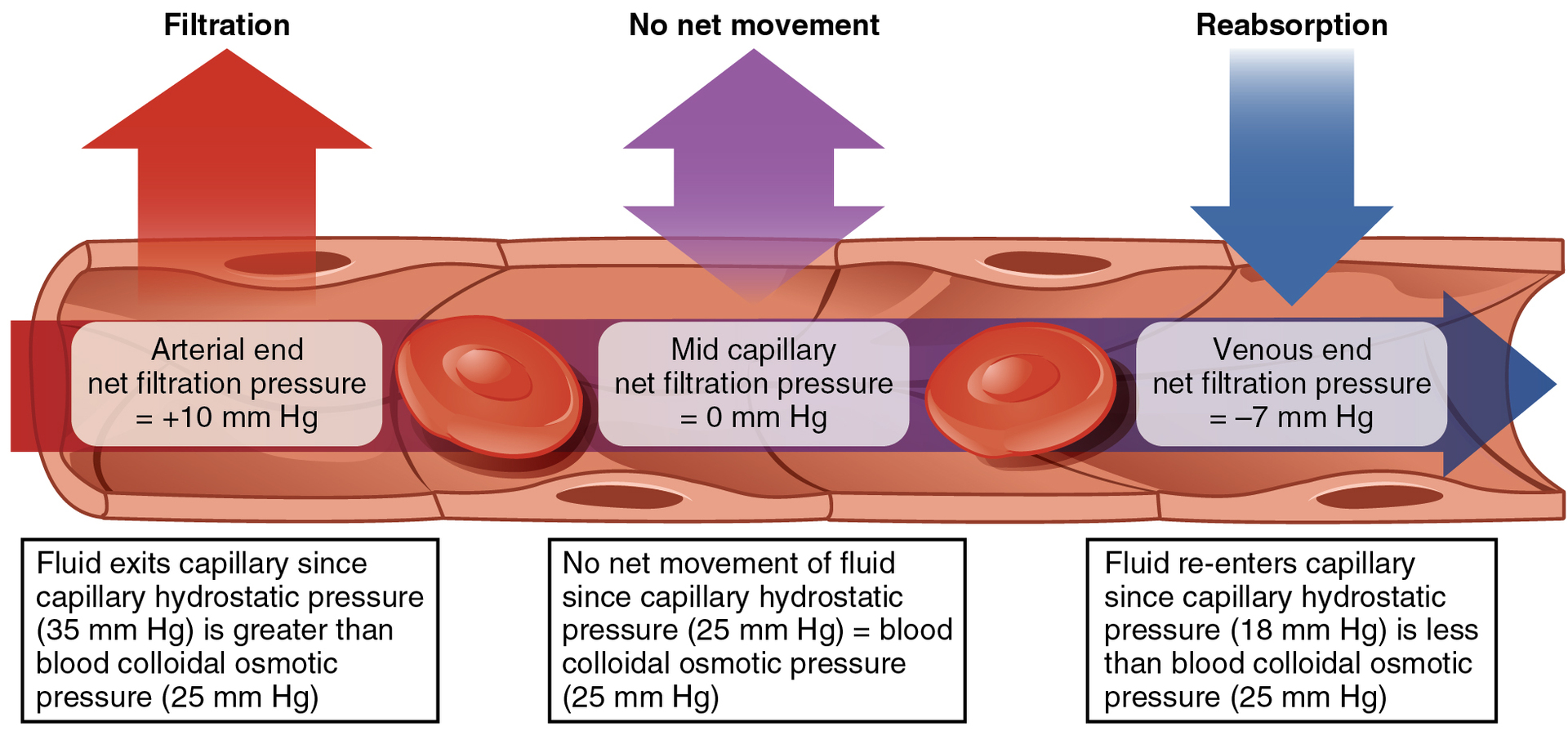
When blood leaving an arteriole first enters a capillary bed, how is the CHP
quite high—about 35 mm Hg. Gradually, this initial CHP declines as the blood moves through the capillary so that by the time the blood has reached the venous end, the CHP has dropped to approximately 18 mm Hg.
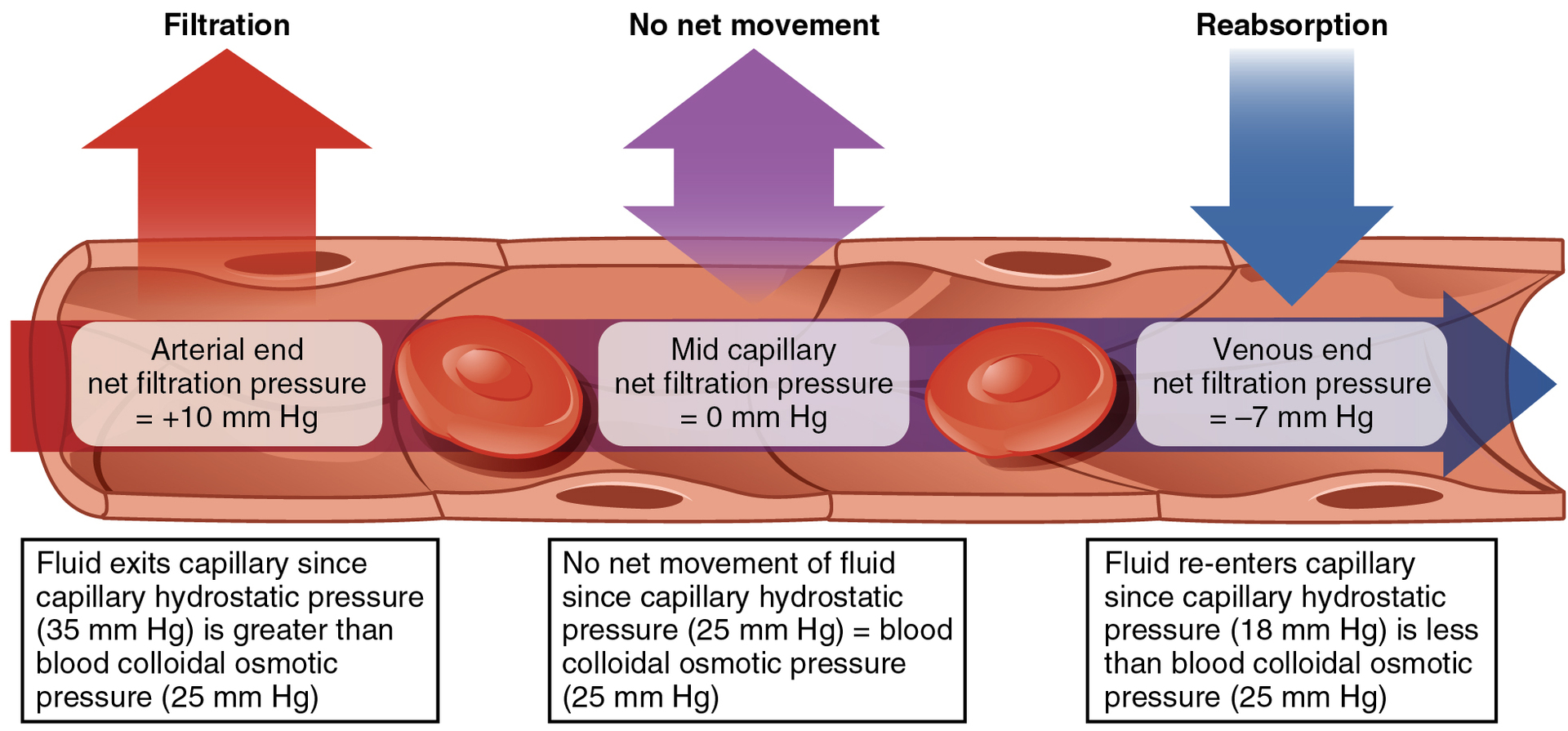
In comparison to CHP declining as blood moves through a capillary, what are plasma proteins like?
they remain suspended in the blood, so the BCOP remains fairly constant at about 25 mm Hg throughout the length of the capillary and considerably above the osmotic pressure in the interstitial fluid.
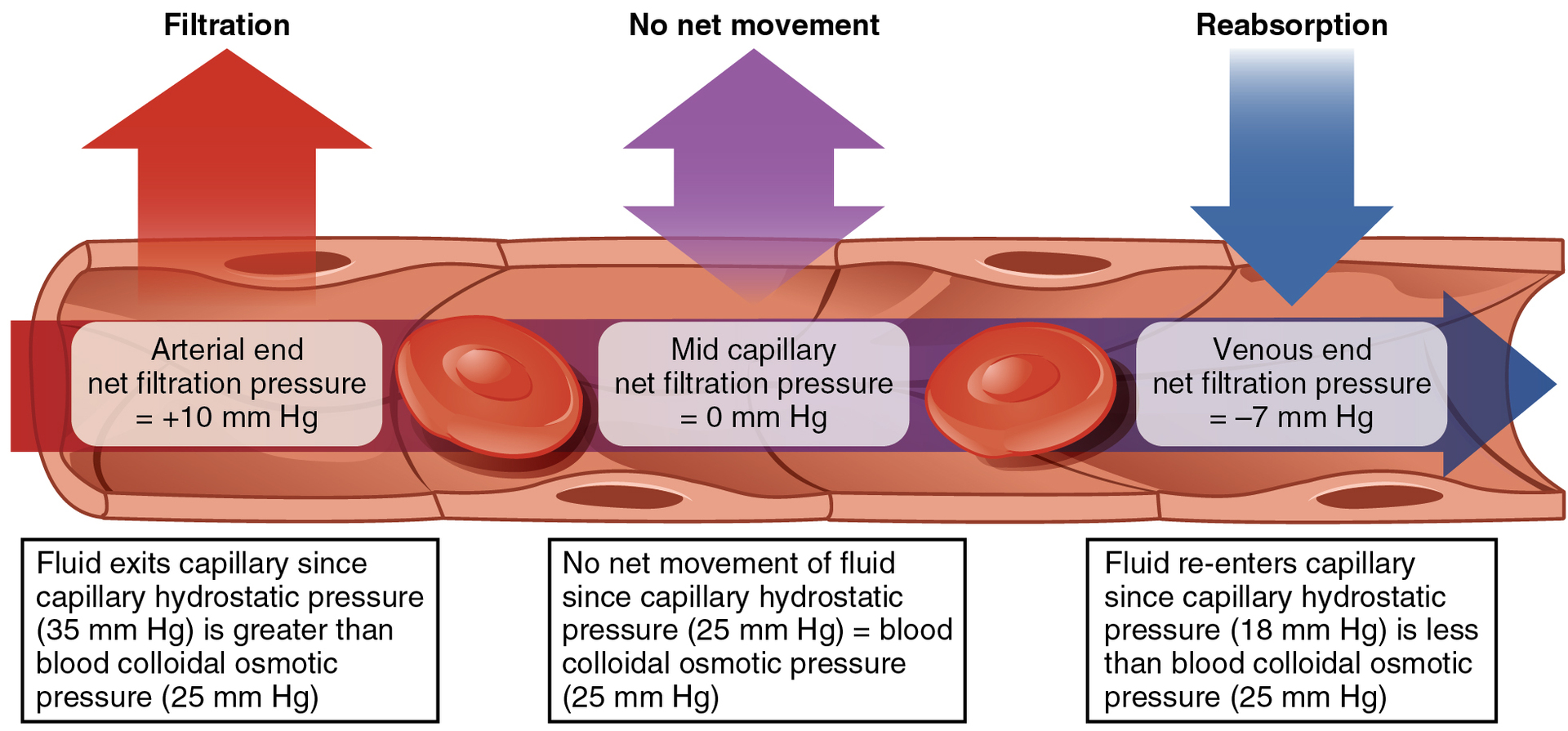
what is the net filtration pressure (NFP)
represents the interaction of the hydrostatic and osmotic pressures, driving fluid out of the capillary. It is equal to the difference between the CHP and the BCOP.
What is filtration by definition
the movement of fluid out of the capillary, when reabsorption is occurring,
What happens to NFP during filtration?
the NFP is a positive number
NFP changes at different points in a capillary bed. What happens close to the arterial end of a capillary?
it is approximately 10 mm Hg, because the CHP of 35 mm Hg minus the BCOP of 25 mm Hg equals 10 mm Hg. Recall that the hydrostatic and osmotic pressures of the interstitial fluid are essentially negligible. Thus, the NFP of 10 mm Hg drives a net movement of fluid out of the capillary at the arterial end.
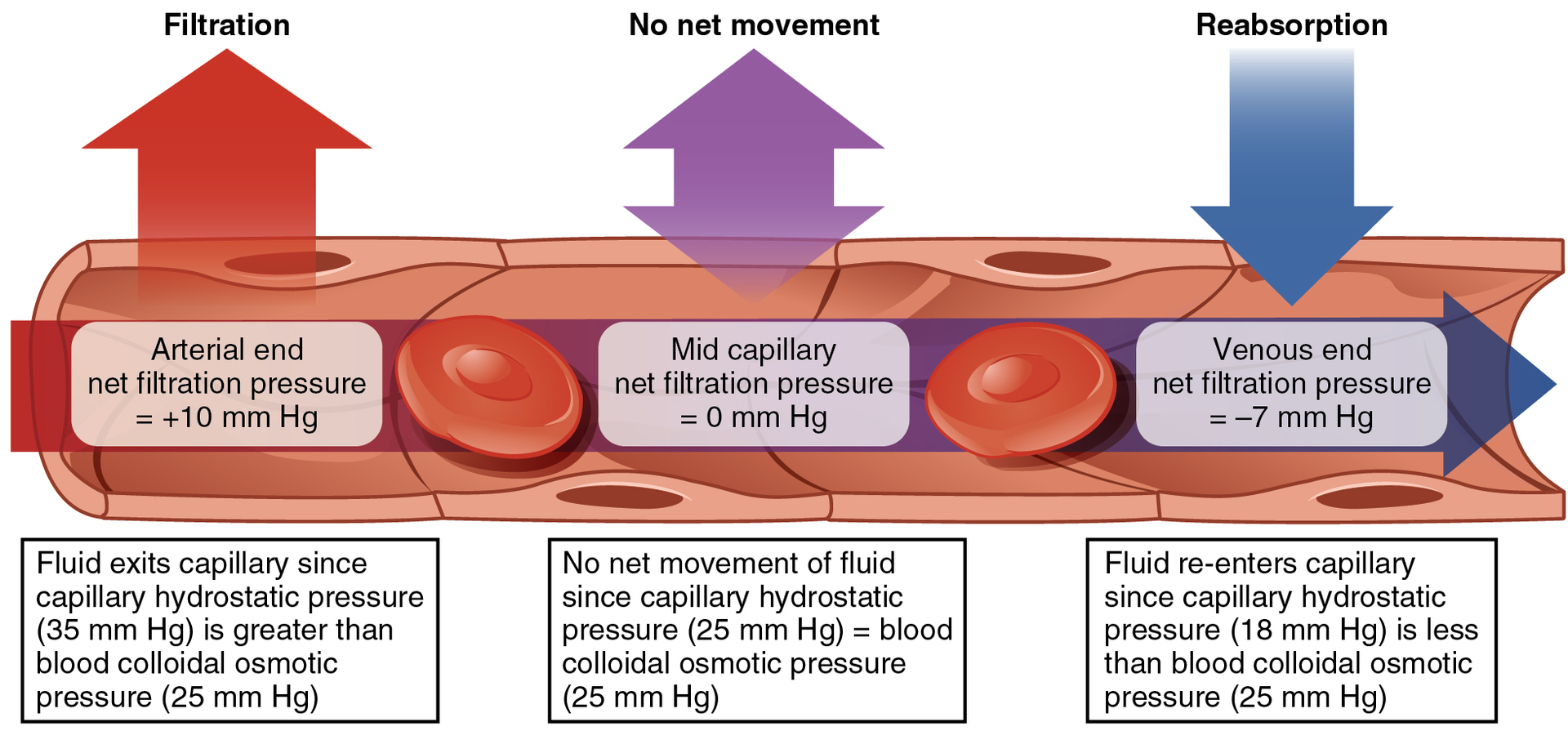
Net Filtration Pressure (NFP) changes at different points in a capillary bed. What happens at approximately the middle of the capillary
the CHP is about the same as the BCOP of 25 mm Hg, so the NFP drops to zero. At this point, there is no net change of volume: Fluid moves out of the capillary at the same rate as it moves into the capillary.
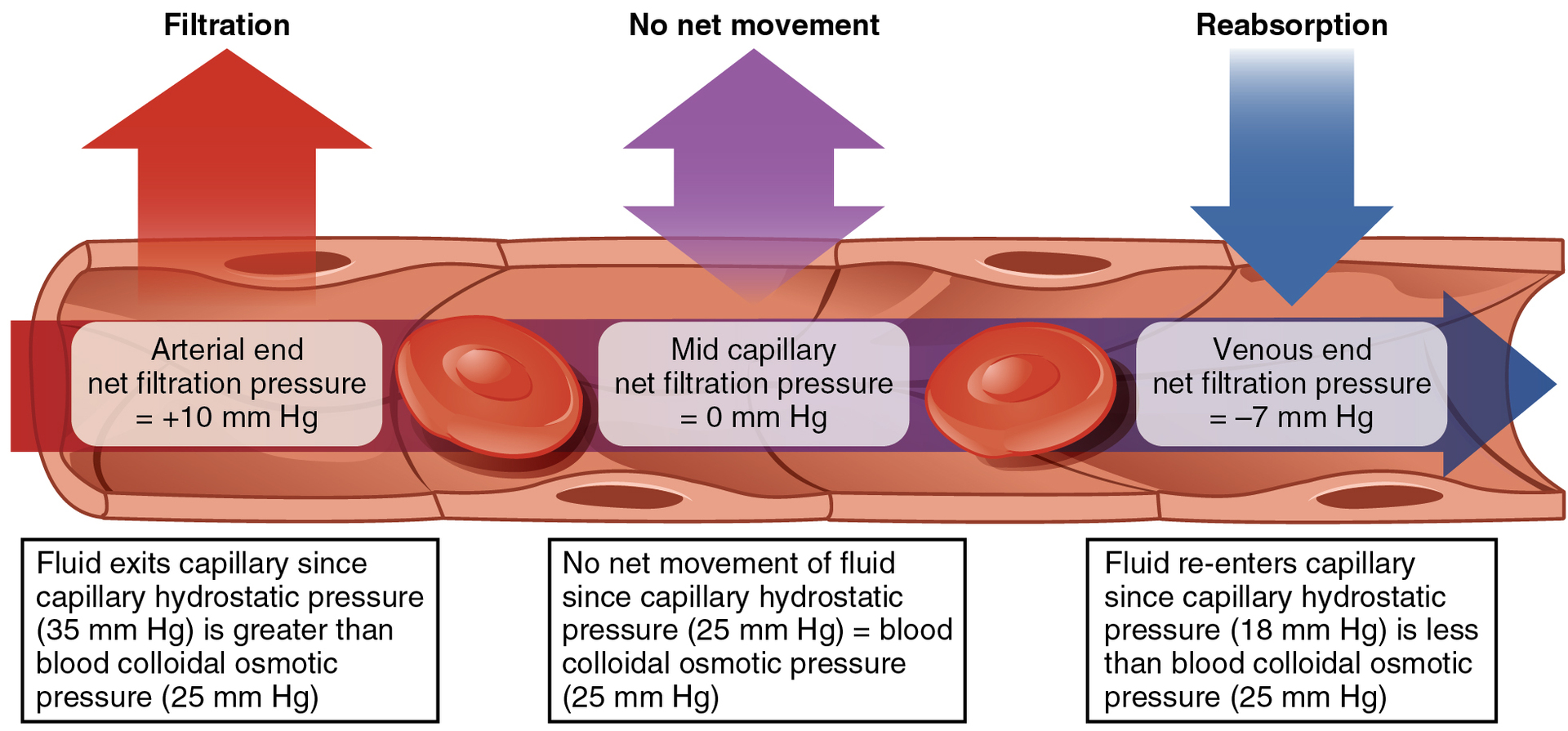
Net Filtration Pressure (NFP) changes at different points in a capillary bed. What happens near the venous end of the capillary?
the CHP has dwindled to about 18 mm Hg due to loss of fluid. Because the BCOP remains steady at 25 mm Hg, water is drawn into the capillary, that is, reabsorption occurs. Another way of expressing this is to say that at the venous end of the capillary, there is an NFP of −7 mm Hg.
Transcytosis is a less common method of capillary exchange. what is it for?
It is a mechanism important in the movement of large, lipid-insoluble molecules that cannot pass through capillary walls in any other way, e.g., the hormone insulin and maternal antibodies.
Transcytosis is the movement of substances across a capillary wall endothelial cell by the following process: what encloses Substances in the blood
pinocytic vesicles.
Transcytosis is the movement of substances across a capillary wall endothelial cell by the following process: The vesicles enter endothelial cells by
endocytosis (cells absorb the vesicles by incorporating them with their membrane).