Self-care OSCE
1/101
Earn XP
Description and Tags
RTS station
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
102 Terms
What is chickenpox?
An acute disease caused by the varicella-zoster virus - mostly occurs in childhood.
Infectious disease
Can get after exposure to a person with shingles (not vice versa).
Symptoms of chickenpox?
Rash of red, itchy spots that turn into fluid-filled blisters - crust over to form scabs, which eventually drop off.
Spots anywhere on body incl. inside ears and mouth, palms of the hands, soles of feet, inside nappy area etc.
Itchy
Crusting usually within 5 days, and crust fall off after 1-2 weeks
Prodromal symptoms:
Nausea, malaise, myalgia, anorexia, headache, loss of appetite, fever
Treatment for chickenpox?
Paracetamol for pain + discomfort (NO IBUPROFEN - risk of secondary infection) - check age.
Topical calamine lotion – to alleviate itch.
apply with a pad of cotton wool to the affected skin as required
Virasoothe chicken pox relief cooling gel – hold bottle 10cm from skin, spray gel, if needed rub into affected area. Apply 2-3 times a day or whenever relief is needed.
Chlorphenamine - for itch - avoid if pregnant + BF, less than 1 etc.
Advice for chickenpox?
Encourage adequate fluid intake to avoid dehydration.
Dress appropriately to avoid overheating or shivering.
Wear smooth, cotton fabrics.
Keep children away from school or nursery until all vesicles have crusted over.
Keep nails short to minimise damage from scratching and secondary bacterial infection from scratching.
Advice that chickenpox is infectious from 24 hours before the rash appears until the vesicles are dry or have crusted over, usually about 5 days after the onset of the rash.
Avoid contact with immunocompromised people, pregnant women, infants aged 4 weeks or less.
Vaccine available (not part of routine childhood schedule) - but offered if vulnerable to complications of chickenpox.
What is meningitis? Symptoms?
A conditions caused by inflammation of the meninges (outer membranes covering brain and spinal cord)
Symptoms:
May have meningitis rash (non-blanching rash can be checked using ‘glass tumbler test’) - press side of glass firmly against rash - if rash does not change colour - contact doctor.
Treatment for meningitis?
Contact emergency services immediately.
What is cradle cap?
Common inflammation of the skin occuring in areas rich in sebaceous glands e.g., scalp, nasolabial folds, ears, eyebrows, chest.
Common in infants under 3 months
For some - gets better over a few weeks but can continue for 6-9 months or longer.
Exact cause = unknown - associated with presence of Malassezia yeasts (type of fungus) - excess greasy sebum accumulates on skin making dead skin cells stick to the skin – gives scaly appearance.
Not contagious.
Symptoms of cradle cap?
Greasy, yellowish or brownish patches on scalp.
Affected skin may appear red.
Scales + flakes on scalp
Yellow crusts.
Possibility of hair loss when either patch falls off or is removed.
Treatment of cradle cap?
Dentinox cradle cap shampoo:
Place small amount onto palm + rub into infant's scalp gently but firmly.
Repeat twice when washing hair every 2-3 days. Dry scalp gently after.
Do not use if skin on scalp if broke/signs of infection – e.g., blisters/redness.
Advise for cradle cap?
Reassure that is it not serious.
Symptoms don’t trouble infant
Soften scales with baby oil first, followed by gentle brushing, then wash off with baby shampoo – once a day, till scales gone – then wash scalp every 2-3 days to prevent scale build-up.
Do not pick at scalp – risk of infection.
May notice babies hair removing with scales – will grow back.
Soak crusts overnight with white petroleum jelly or slightly warmed vegetable/olive oil + shampoo in morning.
Use a greasy emollient or soap substitute e.g., emulsifying ointment – helps removes scales more easily.
Seek further medical advice if signs of infection – crusting, oozing + bleeding.
What is colic?
Colic = repeated episodes of excessive + insolable crying – with no apparent cause.
Usually starts when infant is a few weeks old until 3-4 months old.
NHS = a crying baby for at least 3 hours a day, 3 x a week for at least 1 week
Affects 1/5th of infants – usually improved by 3-4 months of age, resolving by 6 months
Actual cause unknown.
Can be many causes = overstimulating the baby, misinterpreting cries, GI causes e.g., GORD/constipation, cow’s milk protein
Symptoms of colic?
A crying baby for at least 3 hours a day, 3 x a week for at least 1 week
Crying often is in the late afternoon/evening until midnight
Difficult to sooth or settle the baby
Clenching their fist + look under distress
Go red in the face
Bring knees up to tummy or arch back
Tummy rumbles or very windy
Treatment for colic?
Anti-gas medication – simethicone (Mylicon drops, Infacol drops)
Infacol – 1 dropper full (0.5 mL) given before each feed. If needed, after 3-4 days this may be increased to 2 droppers full (1 mL).
Is a dispersing foam – forms when air is swallowed during feeding
Advise for colic?
Goal = soothe baby
Use a pacifier
Hold/gently rock baby through crying – if intolerable put down somewhere safe + take a few mins time out
Provide quiet/soothing sounds
Dim the lights
Wind baby after feeds
Sit baby upright when feeding to stop swallowing air
Rub tummy or place baby on tummy for a back rub
Find support groups for other parents or meet with family/friends for support
Reassure that colic will resolve
When to refer colic?
Patient/carer cannot cope
Infant not growing/putting on weight as normal
If symptoms not improved/worsens after 4 months
If baby crying with a high temp, vomiting, blood or loose stools, or decreased movement
If baby’s crying patterns/behaviour change
What is teething?
The process in which deciduous teeth (sometimes known as milk teeth or baby teeth) emerge through the gums.
Most start teething at ~6 months + symptoms can continue up to 3 years of age
Signs + symptoms usually start 3-5 days before each tooth eruption
Just before tooth eruption - gums swell + are tender to palpation
Symptoms of teeething?
Chewing on hard items – for relief
Swollen, sensitive gums
Excess drooling
Refusal to eat food
Extra fussy/irritable
Ear-rubbing
Sucking
Decreased appetite
Disturbed sleep
First bottom teeth then top
Slight fever (less than 38 degrees)
Light rash
Treatment for teething?
First try non-drug/advise
Drug treatment:
Painkillers e.g., paracetamol for pain/fever (e.g., nurofen for children/calpol infant – sugar free version)
Dose
Calgel - teething gel for children 5 months and above
Short term use – no more than 7 days
Apply pea sized amount using a clean finger up to 6 times a day, The dose may be repeated if necessary after 3 hours.
Do NOT recommend oral choline salicylate gels in infants because of risk of Reye's syndrome.
Advise for teething?
Offer reassurance that teething is normal - not an illness
Symptoms are usually mild and self-limiting
Wipe away excess drool to reduce risk of a drool rash
Rub around the affected gum with a clean finger to soothe any pain (make sure its clean)
Give non sugar pureed foods
Avoid sugary foods - decay or foods that can be broken into hard pieces
Once teeth develop – should brush twice a day – use pea sized amount of toothpaste, spit don’t rinse.
If child weaned - consider supervised use of chilled fruit or veg e.g., banana/cucumber. AVOID ICED or from freezer
Referral for teething?
High temp but cold hands/feet
Shivering
Rapid breathing
What is nappy rash?
Irritant skin condition confined to the nappy area.
Prevalence highest between 9-12 months but can occur in children up to 6 years of age.
Usually not symptoms (scratching or systemic upset) but if severe/painful, child may be distressed or uncomfortable.
Symptoms of nappy rash?
Red patches – looks sore, skin may be raised or swollen
Baby may be distressed + uncomfortable
Can be itchy + painful if untreated
Questions to ask:
Hygiene practices, type of nappy used, how often changed?
Secondary infection? – marked redness with exudates
When to refer nappy rash?
If rash persists after 4-5 days despite optimal treatment
If symptoms are severe and unexplained episodes continue to occur
If candida infection suspected – advice to not use barrier preparation till after candida infection settles – recommend a topical imidazole cream e.g., clotrimazole – apply thin layer to prevent moisture entrapment.
Treatment for nappy rash?
For mild nappy rash not causing discomfort – skin care advice + barrier preparation (Metanium ointment) – apply thinly at each nappy change to protect the skin.
Use daily at every nappy change. Apply a small (pea-sized) amount to the skin and spread evenly to form a thin protective layer.
Advise for nappy rash?
Dry gently after cleaning
Make sure nappy fits properly
Changes nappies often
Use high absorbency nappies – to reduce skin exposure to irritants (faeces, urine + friction)
Avoid potential irritants e.g., soaps, baby wipes (fragrant/containing alcohol), talcum powder
Use barrier creams e.g., bepanthen nappy care ointment or sudocream antiseptic cream (if there is mild erythema – thin layer only)
Bathe child daily – but not more than twice a day which can dry the skin
What is constipation?
Infrequent defection involving straining + passage of lumpy hard uncomfortable stools
Symptoms of constipation?
Unsatisfactory – infrequent stools (< 3 times per week)
Difficult stool passage (with straining or discomfort)
Incomplete bowel evacuation
Dry, hard + lumpy stool, abnormally large or small
*lower abdominal pain, discomfort, distension, bloating.
Questions to ask patient presenting with constipation?
Details of usual bowel habit?
Duration, frequency, consistency? > 14 days then refer
Age? - common in elderly, for child refer
Pain on passing stool? - anal fissure? Haemorrhoids?
Blood? - anal fissure? Haemorrhoids? GI bleed?
Other symptoms? Abdominal pain? Bloating? N+V? Fever?
Changes in diet? Fluid intake?
Tried anything?
When to refer a patient with constipation?
Not improving with treatment
Regularly constipated + lasts long time/change in bowel habit
Blood in poo
Abdominal pain – constant/intermittent
Unexpected weight loss
Very tired at all times
Non-pharmacological treatments for constipation?
Fibre rich foods? adults 30 g daily recommended – adds bulk to faeces as undigested
Increase gradually – avoids bloating/flatulence
Fluid – 2L a day
Foods with sorbitol? - act like natural osmotic laxative, 4P's fruits*
*4P's – peaches, pears, plums + prunes
Exercise – 150 mins per week
Toilet? Go when needed, unhurried, regular routine, position, privacy
If dietary measures ineffective, or waiting for them to take effect = offer oral laxatives.
Drug treatment for constipation?
Bulk-forming laxatives – 1st line
MoA: increase faecal volume, retain fluid in stool, soften faeces + increase peristalsis
Onset: work within 12-24 hours, dependent on preparation
S/E’s: flatulence + bloating first few weeks
Counselling – drink lots of water to prevent gut obstruction + dehydration
e.g., ispaghula husk e.g., Fybogel
Osmotic laxatives
MoA: draw water from intestinal wall into gut lumen - raise intra-luminal pressure thus increasing volume of contents stimulating peristalsis.
Onset: takes 4-72 hours to work dependent on drug
Add or switch to osmotic e.g., macrogrol.
lactulose second line (takes longer to work)
S/E’s: abdominal pain + bloating
E.g., macrogols (8-12 hours), lactulose (48-72 hour), glycerol
*magnesium absorbed so not recommended for chronic use
Stimulant laxatives
MoA: stimulate nerves in large intestine - increase peristalsis + gut motility
Onset: works within 8-12 hours, dependent on preparation – take at night to go toilet in morning
Add stimulant, if stool is soft but hard to pass or inadequate emptying
S/E’s: abdominal cramps, diarrhoea, lazy bowel
e.g., senna, bisacodyl, sodium picosulfate, glycerol (local irritant action), castor oil (old method)?
Stool softeners:
MoA (of faecal softeners): anionic surfactant lowers surface tension of intestinal content – fat + fluid can penetrate – emulsifies + softens stool e.g., docusate, arachis oil enema
MoA (of faecal lubricants): penetrates + softens stool – coats surface to facilitate passage
S/E’s: anal seepage, skin irritation, lipid pneumonia
e.g., liquid paraffin, arachis oil enema
Not used often.
When to advise stopping laxative?
Advise the person to gradually reduce and stop laxatives once the person is producing soft, formed stool without straining at least three times per week.
What is diarrhoea?
Passage of 3 or more loose or liquid stools per day (or more frequently than usual).
Acute diarrhoea - less than 14 days.
Persistent diarrhoea - more than 14 days.
Chronic diarrhoea - more than 4 weeks.
Symptoms of diarrhoea?
Passing of frequent, soft, watery stools (relative to usual habit)
Faecal urgency
Irritation of stomach lining --> stomach cramps
Nausea
Fever
Loss of appetite
Bloating/flatulence
Questions to ask person presenting with diarrhoea?
Age - children/elderly?
Nature of stool? Watery with no blood – infective? Blood (dark stool)/mucus - invasive organism (shigella) or IBD
Duration? Persistent/recurrent - IBD/IBS? Protozoal infections last longer
Relation to food? E.g., seafood?
Abdominal pain? Presence, nature, severity? Appendicitis? Diverticular disease?
Vomiting? - infective gastroenteritis
Weight loss? - refer - bowel cancer?
Travel? - esp. If fever present
Dehydration signs? - refer
Thirsty, dry mouth/tongue, poor urine output, rapid breathing, tachycardia, sunken eyes, babies – sunken fontanel, lethargy, cold, clammy, wrinkly skin, unresponsiveness
When to refer diarrhoea/red flags?
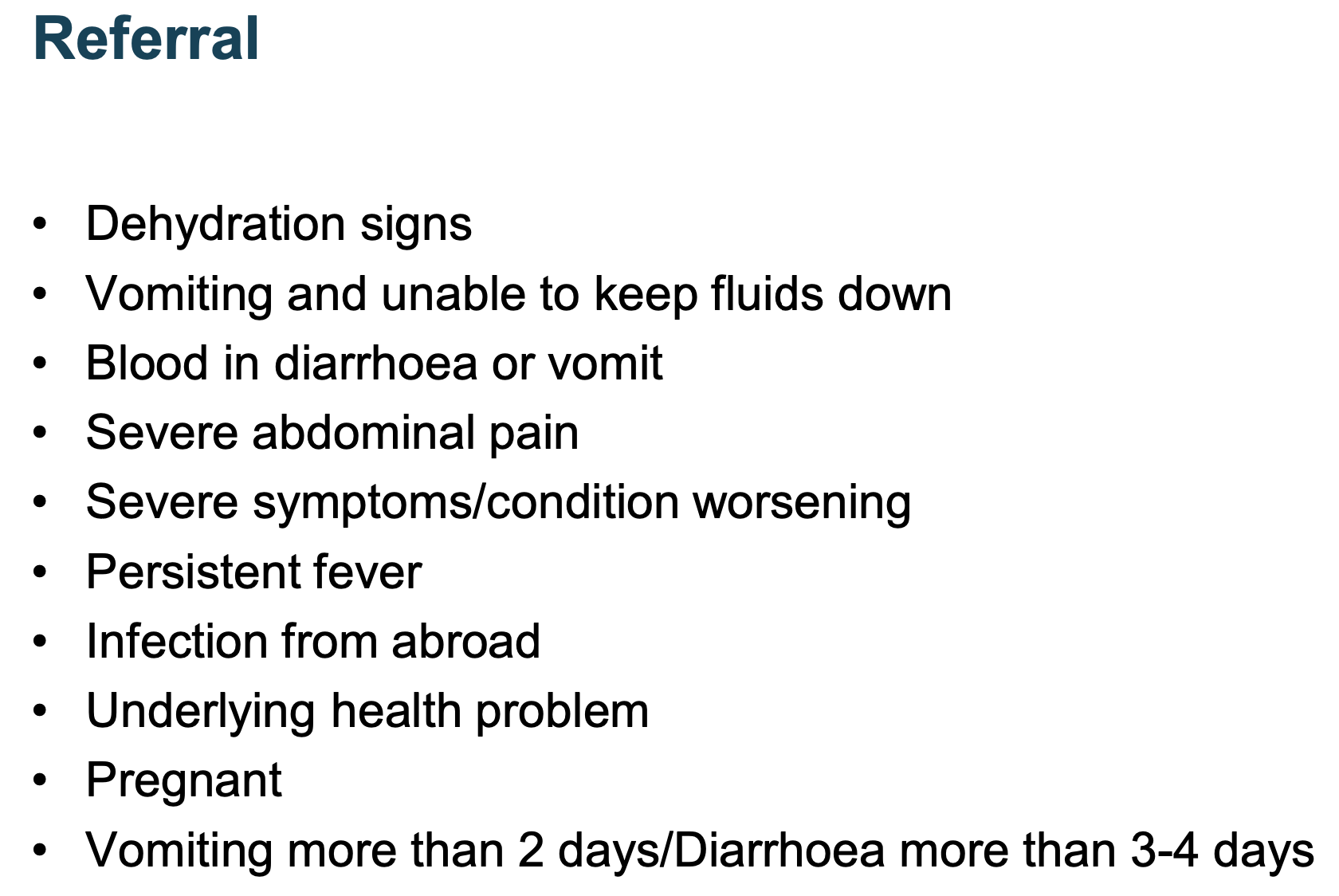
For baby + elderly if more than 1 day diarrhoea – refer due to risk of dehydration.
Chronic + recurrent should be referred regardless. Days to refer may increase as baby gets older.
Non-pharmacological treatments for diarrhoea?
Food hygiene practice, handwashing, stay at home at least 48 hours after last episode
Lifestyle:
Stay at home + rest, drink fluids with small sips, avoid fizzy drinks, breast/bottle feeds to baby (do not dilute formula), small sips of water between feeds for babies on formula or solids, eat when you can small/light meals, plain foods
Treatment for diarrhoea?
Oral rehydration therapy – 1st line
Glucose + electrolytes
Dietary – small, light meals with plain foods
All ages - if under 1, need to be referred
Dioralyte relief
Loperamide – 2nd line
MoA: slows small and large intestine transit by decreasing bowel motility through action on opioid receptors in gut.
Can increase absorption of fluid + electrolytes
Over 12 years
S/Es’s: No central effects, BBB.
Not many ADR's – only constipation/megacolon
e.g., Imodium
Over 12 years: 2 capsules initially followed by 1 capsule after each loose stool. The usual dose is 3-4 capsules a day. Maximum of 6 capsules (12mg) daily. If symptoms do not improve within 2 days, usage should be stopped and a doctor consulted.
What is dyspepsia?
General pain/discomfort in upper abdomen = oesophagus, stomach + duodenum.
Dyspepsia is a non-specific term used to describe indigestion. It covers the symptoms of GORD:
Aetiology – related to stomach acid – inflammation + excess.
Symptoms of dyspepsia?
Heartburn, bloating, belching, flatulence, feeling of fullness, nausea, nocturnal cough, hoarse voice.
Comes + goes
Usually related to eating
Look at triggers e.g., smoking, heavy drinking, overweight, lifestyle, drugs, food, pregnancy etc.
Questions to ask when person presents with dyspepsia?
Frequency, duration + pattern of symptoms
Family history of GI malignancy
Age
Dyspepsia – young adults, >50s other pathology more likely
Location of pain
Dyspepsia – above umbilicus/central, heartburn – behind sternum, below umbilicus – IBS, diverticulitis
Pain radiation
CV (MI), angina, biliary colic
Pain severity
Dyspepsia – mild to moderate
Other symptoms e.g., ask about alarm symptoms + signs of anaemia
Aggravating/relieving symptoms – ulcers
Lifestyle factors
Review medicines
Red flag signs for GORD?
Dysphagia (difficulty swallowing) at any age gets an immediate two week wait referral for endoscopy - critical red flag
Aged over 55 (this is generally the cut-off for urgent versus routine referrals)
Weight loss
Upper abdominal pain
Reflux
Treatment-resistant dyspepsia
Nausea and vomiting
Upper abdominal mass on palpation
Low haemoglobin (anaemia)
Raised platelet count
Non-pharmacological treatments for dyspepsia?
Before OTC
Lifestyle measures:
Reduce tea, coffee and alcohol
Weight loss
Avoid smoking
Smaller, lighter meals
Avoid heavy meals before bedtime
Stay upright after meals rather than lying flat
Review medication
Treatments for dyspepsia?
Alginates - floats on top of stomach contents e.g., Gaviscon
Antacids - neutralise stomach acids (alkali), fast acting (1h)
Good for isolated, occasional symptoms – can impair absorption of other drugs (interact) - leave gap
What is irritable bowel syndrome (IBS)?
A chronic, relapsing, and often debilitating disorder of gut-brain interaction.
resulting in troublesome abdominal and intestinal symptoms.
can significantly impact the patient’s life.
Symptoms of IBS?
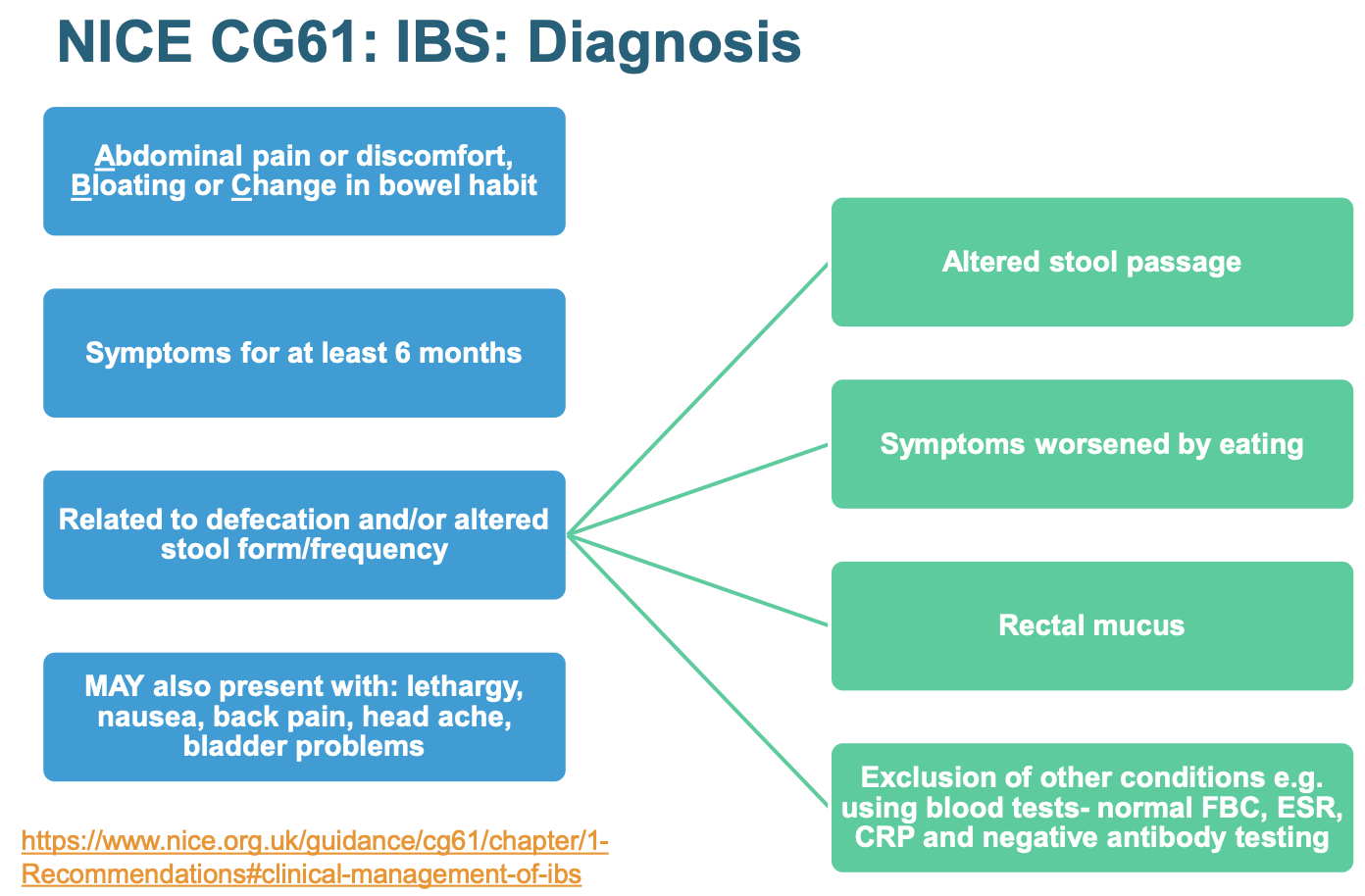
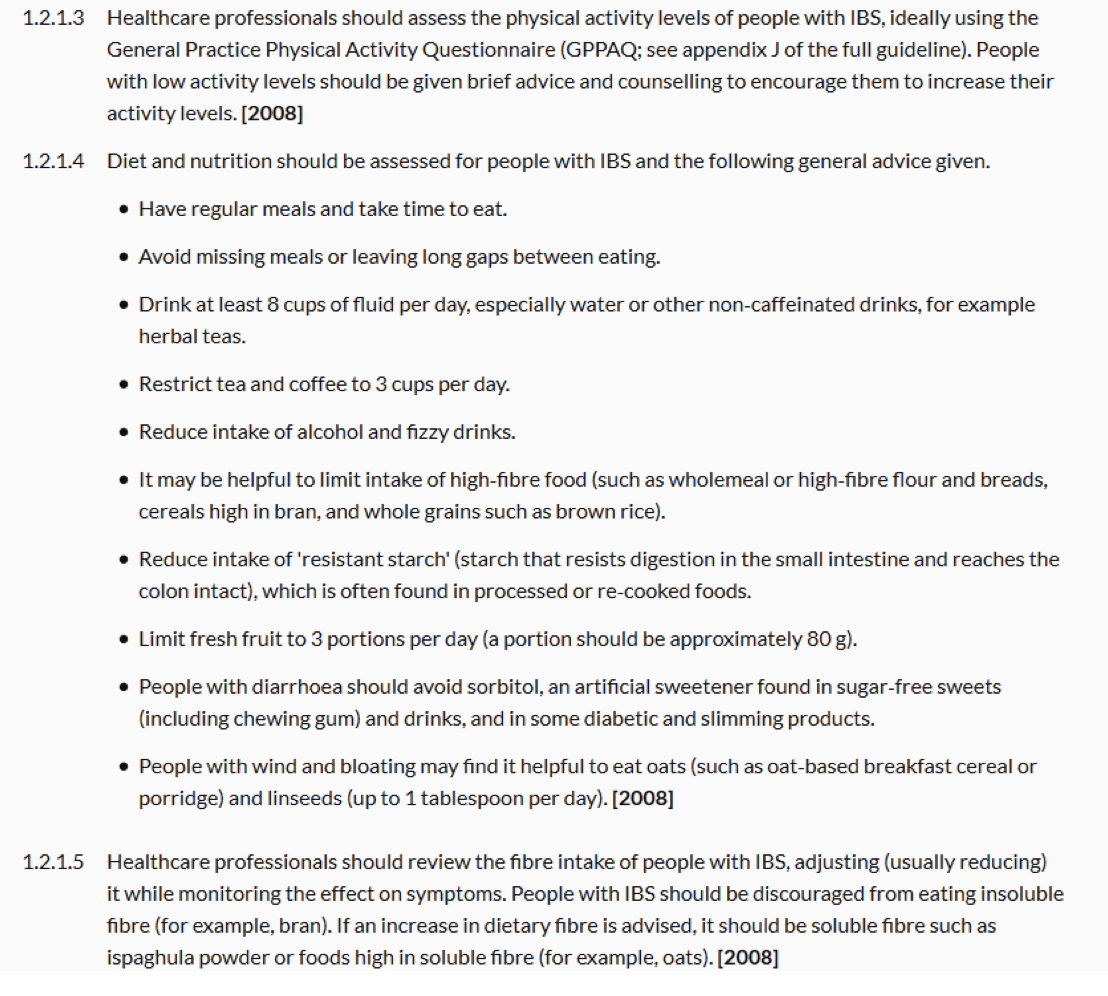
Advise for IBS?
Treatment for IBS
Antispasmodics for cramps (e.g., mebeverine, alverine, hyoscine butylbromide or peppermint oil) - alongside dietary + lifestyle advice.
Bulk-forming laxatives (e.g., ispaghula husk) for constipation
can be used for diarrhoea too - adds fibre to stool - less watery.
avoid lactulose - S/E: bloating + flatulence - retains liquid in gut adding to bloating symptoms)
Loperamide - antimotility agent for diarrhoea
Advise on adjusting doses of laxative or antimotility agent dependent on response - shown by stool consistency.
Aiim = soft, well-formed stool (Bristol stool form scale type 4)
What are haemorrhoids?
Swellings that develop from lining of anus + lower rectum
Widen + engorge with blood
Pressure in + around anus
Internal:
Prolapsed – hang out, spring/push back
External:
Small lump develops on outside edge of anus
Many have no symptoms but can itch/painful
Thrombosed – intense pain, immediate treatment
Symptoms of haemorrhoids?
Bleeding after defecation
Faecal soiling
Mucus discharge
Pruritus ani – anal itch + irritation
Pain – dull ache, intense if prolapsed + strangulated – may not relate to defecation
Feeling bowel not emptied
May be asymptomatic
Advice for haemorrhoids?
Increase dietary fibre e.g., wholegrain rice, wholewheat pasta, fruit, veg etc - reduce constipation risk
Increase fluid intake - reduce constipation risk
Cut down on caffeine and alcohol
Avoid medications that cause constipation e.g., co-codamol
Fibre supplements – ispaghula, sterculia, methylcellulose
Anal hygiene – clean + dry, pat not rap, can use wipes
Toileting – go when needed, no straining
Losing weight if overweight
Treatment for haemorrhoids?
Analgesia e.g., paracetamol
Avoid opioids – constipation, avoid NSAID's – bleeding
Creams, ointments, suppositories, or sprays
Combo of ingredients = local anaesthetics, skin protectants/lubricants, astringents, antiseptics + topical corticosteroids
E.g., anusol cream
Laxatives? - if constipated
Refer if severe, non-responsive or recurrent symptoms – unresponsive to OTC
What are mouth ulcers?
Cannot be passed from person to person and cause is mainly unknown.
Offer recurrent.
Symptoms of mouth ulcers?
Aphthous ulcers (minor):
Roundish, grey-white in colour, lesions inside mouth, swollen
Location – cheeks, tongue + inside lips
Small, shallow with a rim – clearly defined
Painful
Affect eating + drinking
Usually more than one at a time
Treatment of mouth ulcers?
Gels, pastes, mouthwashes, liquids + pastilles
Local anaesthetic e.g., lidocaine + benzocaine
Apply prn but check license
Anbesol gel – max every 3 hours
Local analgesic e.g., choline salicylate + salicylic acid
Every 3 hours approx. directly to ulcer
Bonjela gel – max every 3 hours
Antibacterial e.g., chlorhexidine
Corsodyl MW + iglu pastilles
Protective base e.g., carmellose - orabase
Advise for mouth ulcer?
Spicy, salty or acidic food
Don’t eat rough or crunchy foods
Avoid hot drinks
Wash hands before + after treatment
Frequent application
When to refer mouth ulcer?
Located towards back of mouth
Ulcers caused by major trauma
Multiple ulcers in mouth or one big ulcer
Irregular shaped ulcers
Painless ulcers
Children under 10 years
More than 14 days (3 weeks MUST refer)
Major
Herpetiform
Left a scar or elsewhere on body
What is head lice?
Tiny, grey-brown insects, size of sesame seed on the head.
Cling to hair with claws, feeds on blood from scalp
Transmitted by head-to-head contact (no jumping).
Symptoms/signs of head lice?
nits are empty white egg-shell, stick very strongly to hair (not a sign of current infection and not removed by treatment)
eggs laid close to scalp and found farther from scalp as hair grows
itchy scalp sometimes, due to allergic response to saliva of lice, not biting of scalp.
often takes three months for an itch to develop.
do not wash off with normal shampoo.
itch can persist after eradication.
not everyone has itching (takes thousands of bites).
Questions to ask when patient presents with potential head lice?
age.
signs of infection - live lice (usually less than 20 lice=hard to see), checking for infection, nits, scalp itching (especially behind ears).
previous infection.
medication - treatments used?
Detection of head lice?
Wet hair method is more effective - immobilise lice with hair conditioner - able to see lice on the comb.
Wet hair method:
wash hair as normal - put lots of conditioner - comb out tangles.
using detection comb into roots of hair touching scalp draw down to tips of hair.
2 types of detection comb - plastic comb + metal fine tooth comb - normally recommend metal.
comb all parts of scalp - section hair.
check for lice after each stroke (wipe/rinse if seen).
rinse out conditioner.
repeat procedure.
Dry hair method:
straighten untangle hair with comb - switch to detection comb - comb each section 3/4x.
look for lice each time - hold white sheet of paper underneath for lice to fall on - good for detection.
trap lice with thumb, avoids risk of lice being repelled by static electricity as comb withdrawn from hair.
continue until full head covered.
Treatment for headlice?
Do NOT need to treat family and friends - unless they have it to.
Physical insecticides:
Dimeticone 4% lotion/gel/spray (Hedrin).
Isopropyl myristate and cyclomethicone solution (Full Marks Solution).
Isopropyl myristate and isopropyl alcohol aerosol (Vamousse).
Chemical insecticides:
Malathion 0.5% aqueous liquid (Derbac-M).
Alternative methods:
Wet combing using the Bug Buster kit.
Other nit combs - Nitty Gritty Nit Free comb, Nitcomb-S1 + Nitcomb-M2.
Nitview Ledcomb – uses ultraviolet light.
louse and nits glow under the UV light so aids easy detection and ability to remove.
can be used to checking clothing, bedding, etc.
Advantages and disadvantages of the different headlice treatment options?
Bug Buster kit - wet combing:
no chemicals = no resistance.
removes head lice without using lotion to kill them.
no contraindications, precautions or side effects.
inexpensive plus kits are reusable.
similar to wet detection, need to repeat process several times.
need to do this on every family member.
takes 30 min to 2 hours to do properly - repetitive + time consuming = reduced cure rate.
need correct comb.
do every 3 or 4 days for 2 to 3 weeks and continue until no further lice found on 3 consecutive sessions.
Dimeticone 4% lotion/gel/spray (Hedrin) - 6 months plus
silicone based product - blocks tubes lice use to breathe and pass out water.
use: apply to dry hair and leave overnight (min. 8 hrs) - 1 hour preparation available now.
does not kill unhatched eggs - therefore two applications needed (7 days apart).
odourless
Full Marks Solution - 2 years plus
dissolves wax coating on louse exoskeleton = dehydration + death
use: apply to dry hair and leave for 5-10 mins - comb hair to remove lice - wash with shampoo to remove solution.
repeat process after 7 days.
must be over 2 years.
suitable for asthmatics.
odourless.
Vamousse - 2 years plus
contains alcohol - do not recommend for eczema + asthma patients.
15 minute application on dry hair.
no need to reapply.
Malathion 0.5% aqueous liquid (Derbac-M).
poisons lice by chemical means.
re-apply after 1 week.
no alcohol.
ADRs – irritation + erythema of scalp, hands.
Advise/management of headlice?
Ensure reapplication for preparations requiring it.
Ensure adequate quantity of insecticide used.
1 small bottle for short/shoulder length hair.
1 large bottle or 2 small bottles for longer, thick hair.
Children can go to school.
Treat all affected family on same day.
Not associated with a lack of hygiene.
Unnecessary to clean bedding or clothing.
Short hair can be infected as well as long hair.
Symptoms e.g., persistent itch not due to treatment failure.
Not possible to prevent.
Examine children’s hair regularly for early identification.
What is scabies?
An skin infection - extremely itchy, especially at night. Accompanied by a rash.
mite transmitted by close physical contact e.g., holding hands, hugging, or sexual contact.
possible but rare to catch from bed linen, clothes, towels.
mite survives away from host for ~24-36 hours.
cannot jump or fly.
classical (most common) - transmitted only via direct skin contact.
crusted - transmitted via bedding, towels, clothes + furniture.
Questions to ask individual presenting with scabies?
itching or rash?
itching occurs weeks after infection + post-eradication.
papular rash.
pruritus - sudden onset, severe + worse at night - night is when mites release faecal pellets.
presence of burrows?
tracks made by mite burrowing through skin.
small grey/silvery curved lines in skin (≤1 cm).
difficult to see due to scratching.
location?
finger webs, palms, wrists, elbows, abdomen, genitalia, + buttocks.
who the patient is?
history? - common in care workers.
signs of infection?
medication?
Symptoms of scabies?
can take 6 weeks, but normally ~2 weeks.
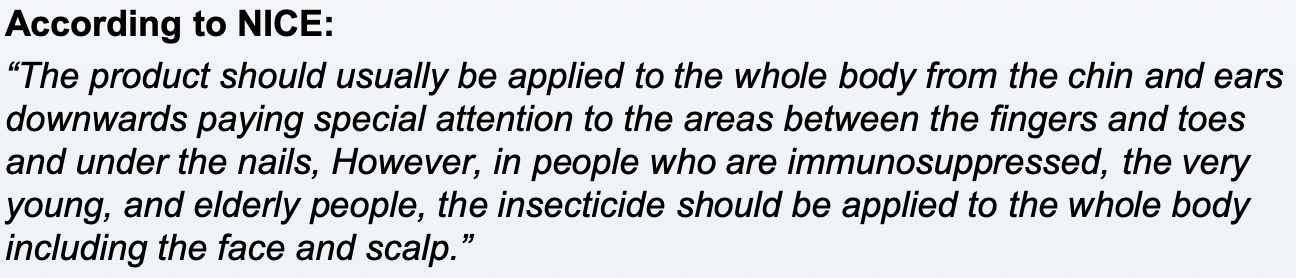
Treatment for scabies?
if untreated, can last for months-years.
Lyclear Dermal Cream - contains Permethrin 5% w/w - 1st line
adults & babies >2months but <2 years should be ideally be prescribed.
over 12 year olds - use a full tube as a single application (some patients 2 tubes).
use: apply to whole body (ex. head – manufacturer)
wash body after 8-12 hours - reapply if e.g., wash hands.
repeat after 1 week.
s/e: skin irritation.
How to apply: clean, cool, dry skin. Apply preparation all over body with cotton wool or sponge. If wash hands, reapply.
Derbac M - contains Malathion.
0.5% non-alcoholic liquid (same prep used in head lice).
apply to whole body.
leave on for 24h.
repeat after 1 week.
Ascabiol - contains benzyl benzoate.
???
Treatment for symptomatic relief of itching of scabies:
Calamine lotion - apply with cotton wool to affected skin PRN.
Crotamiton 10% cream (Eurax):
rubbed into entire body daily for 3-5 days OD-TDS.
may cause irritation.
Antihistamines:
sedating oral antihistamines for night time itching e.g., chlorphenamine (Piriton).
for piriton - adults: 1 tablet 4-6 hourly. Max 6 tabs in 24 hours.
Hydrocortisone 1% cream:
only if scabies definitely eradicated.
Advice for scabies?
itching can last for weeks or worsen - allergen from dead mite.
clean all bed linen at high temps (50o or over) after first treatment (mites lives for 1 day after).
if unable to wash, place in plastic bag for at least 72 hours. After this time, scabies mites will have died.
NO evidence for hot baths opening burrows
scabicide penetrates skin to kill mite and eggs in basal layer of epidermis.
current recommendations - treat whole body including head + neck.
different to some manufacturers’ advice about excluding head and neck.
remember to apply to toes, under nails etc.
treat all members of family/partners preferably on the same day (several weeks for itch to develop - may be asymptomatic but infected).
avoid close body contact until everyone treated.
children and adults can return to school or work after the first treatment has been completed
When to refer scabies?
babies + children (<2 years).
infected skin.
treatment failure.
unclear diagnosis.
genital scabies.
crusted scabies - thick, crusted skin containing living mites.
What is threadworm?
A small, white, thread-like worm, which lives in the upper part of the colon.
causes incontinence + embarrassment rather than morbidity.
social stigma - lack of hygiene.
Transmission - mostly via faecal-oral route (eggs lodged under nails which are ingested) but also retro-infection or inhalation.
Signs/symptoms of threadworms? Diagnosis?
night time perianal itching - can lead to sleep disturbances (eggs laid on perianal area).
threadworms look like thin, white cotton threads (2-12 mm long) in nappy, possibly clothing + bed sheets, sometimes protruding from anus.
sticky tape test (am), before wiping or bathing - tape under microscope.
in severe cases - diarrhoea.
Diagnosis: by observing worms in stool.
Treatment of threadworms?
adult worms live for approx. 6 weeks so Tx not always necessary (use strict hygiene measures) e.g., if pregnant
drug Tx - kills/paralyses worms.
1st line mebendazole OTC - 2 years plus
inhibits worms uptake of glucose.
Ovex (OTC) or Vermox (POM).
100mg tabs or suspension
6month-2year can be prescribed (unlicensed)
all household members treated at same time
repeat after 14 days if infection persists
avoid in pregnancy/bf
Advise/management of threadworms?
need hygiene measures to ensure eggs removed + to prevent re-infection.
at least 2 weeks if taken anthelminthic.
at least 6 weeks if using hygiene measures alone.
aim to clear eggs from body and home + prevent eggs being swallowed (re-infection).
wash sleep wear, bed linen, towels, toys (eggs can survive up to 2 weeks away from body).
vacuum and damp dust home (throw out cloth)
wear close fitting underpants/knickers at night.
shower every morning (rather than bath).
wash hands and scrub under nails first thing in morning + after using loo each time and eating.
avoid biting nails and hands in mouth.
cut fingernails short.
possibly wear gloves at nights if very itchy.
avoid sharing towels, flannels.
cover food in the home
rinse toothbrushes well before use and store in closed cupboard.
What is eczema?
Condition that causes the skin to become itchy, dry + cracked – skin can’t retain moisture.
Most common form of eczema + more common in children- often occurs in people with allergies – atopic means sensitivity to allergens.
Often develops alongside asthma + hay fever.
Symptoms of eczema?
Itchiness – can interfere with sleep, cause tiredness + irritability.
Red, dry skin + can leak fluid in flare=up.
Goes through phases – severe to less severe to worse.
More common – creases around joints e.g., behind knees or inner elbow, also can be wrists + neck (flexural pattern)
Treatment of eczema?
Not cure but helpful:
Moisturisers – emollients – use on daily basis – reduce water loss + cover skin with protective film:
Complete emollient therapy – regular application (many times a day) – are soap substitutes.
Depending on how dry skin is – ointment for severe, then cream, then lotion
Use large amount – smooth into skin in same direction as hair growth.
After shower/bath, gently pat the skin dry + apply emollient while skin is still moist to lock in moisture.
Topical steroids – e.g., Eurax HC cream – max 7 days:
Reduce swelling, redness + itching during flare-ups.
NOT long-term use – steroid withdrawal
Do not use if skin is open.
S/E’s = thinning of skin (usually w/ long-term use), changes in skin colour, acne, increased hair growth. If given steroid + emollient – emollient first + wait 30 mins at least before steroid
Advice for eczema?
Not contagious.
Can catch fire – avoid naked flames.
Treat early – easier to control.
Moisturise skin often
Wash with moisturizer instead of soap.
Don’t itch/scratch skin – keep nails short. Anti-scratch mittens for babies.
Wear comfortable clothes e.g.,
Avoid detergents, chemicals + soaps.
Rinse well after swimming + moisturize well.
Find out if have food allergy? – go to GP/dietician
Refer to dermatologist if unsure.
When to refer eczema?
Bacterial infection: weeping, crusted, pustules, fever, malaise.
May need antibiotics (flucloxacillin 1st line).
Eczema herpeticum - immediate hospital admission.
Rapidly worsening, painful eczema, clustered blisters, punched out erosions.
What is psoriasis?
Chronic inflammatory disorder causing flaky patches of skin which form scales.
Cause = triggers e.g., infections, stress alcohol, skin damage, direct sunlight, diabetes, obesity + medication.
Periods of no/mild symptoms, then periods of severe symptoms.
Not contagious.
People with psoriasis have an increased production of skin cells. Normally skin cells made + replaced every 3-4 weeks. In psoriasis, only takes about 3-7 days. Result= build-up of skin cells creating patches associated with psoriasis.
Symptoms of psoriasis?
Affects nails, joints + skin.
Cracks painful + can bleed.
Well-defined + slightly raised pink/red plaques.
Areas with silvery white scales.
Painful + lifted/pitted nails.
Swelling + stiffness in joint.
Patches normally on elbows, knees, scalp + lower back but can be anywhere.
Treatment for psoriasis?
Aim: induce remission as there is no cure.
1st line = emollient + topical treatment.
With emollients (soften scaling and reduce skin irritation):
apply liberally + frequently even when skin looks better.
If given topical corticosteroid (short-term use e.g., 7 days) – wait 15-30 mins after emollient use.
E45 psoriasis cream or dermalex psoriasis treatment.
Advice for psoriasis?
Lifestyle - weight loss, smoking cessation, alcohol reduction.
Management of stress/anxiety/depression.
Apply emollients/creams - keep skin hydrated and avoid itching.
Avoid bathing in hot water/harsh soaps. Use soap substitutes.
Avoid triggers/irritant.
Wear gloves and other protective clothing.
Support groups – Psoriasis Association.
Stop smoking, cut down on alcohol, lose weight if overweight/obese.
Don’t itch skin.
When to refer psoriasis?
Unexplained joint pain or swelling (psoriatic arthritis) - rheumatology referral.
What is contact dermatitis?
Inflammatory skin condition due to exposure to an external irritant or allergen.
Allergic contact dermatitis - type IV (delayed) hypersensitivity reaction - occurs after sensitisation and subsequent re-exposure to an allergen.
E.g., cosmetics, metals, topical meds, certain plants.
Irritant contact dermatitis - non-immunological inflammatory reaction - due to direct physical or toxic effects of an irritating substance on the skin - prior sensitisation not required.
E.g., repeated exposure to water, detergents, cleaning agents, certain plants.
Symptoms of contact dermatitis?
Treatment of contact dermatitis?
Acute:
Avoid stimulus/minimise contact e.g., wash off after contact, wear gloves.
Emollient (liberally) - maintains hydration + improves barrier
Consider topical corticosteroids
Treat secondary skin infection if present
Avoid aqueous cream - can cause skin reactions.
Advise for contact dermatitis?
When to refer contact dermatitis?
Contact dermatitis associated with occupation - employers have legal duty to report to Health and Safety Executive and assess health risks at work + prevent/control exposure to hazards.
Secondary skin infection
Unresponsive/severe/chronic/recurrent - especially of hands and face.
Previously stable - now uncontrolled.
What is seborrhoeic dermatitis?
Common inflammatory skin condition affecting areas rich in sebaceous gland e.g.., scalp, nasolabial folds, eyebrows and chest.
Exact cause not fully known - presence of Malassezia yeasts and host immune response.
Symptoms of seborrhoeic dermatitis?
red, sharply marginated lesions with greasy looking scales.
on scalp or eyebrows - appears as dry, flaking or yellow, greasy scaly with redness.
Treatment of seborrhoeic dermatitis?
Scalp and beard:
Ketoconazole 2% shampoo (e.g., nizoral)
once every 3 days??
OTC anti-dandruff shampoo e.g., containing coal tar or salicylic acid.
once or twice weeklyy??
Face and body:
Ketoconazole 2% cream or other topical imidazole and an antifungal shampoo e.g., ketoconazole 2% as a body wash.
Consider short course mild topical corticosteroid cream.
Advise for seborrhoeic dermatitis?
Use gently, soap-free wash on skin plus light moisturiser after washing.
Avoid makeup that blocks pores and are non-comedogenic.
When to refer seborrhoeic dermatitis?
Uncertain diagnosis, failure to response.
Severe or widespread.
Eyelid involvement - if eyelid hygiene measures unsuccessful.
What is acne vulgaris?
Causes spots, oily skin + skin that can be painful to touch.
Cause = hair follicles blocked by excess sebum + dead skin, hormonal changes (increased testosterone), makeup/cosmetics, medication, sugary diet.
May flare up before period, during pregnancy, if have PCOS.
Common skin conditions affects most people at some point.
Symptoms of acne?
Comedones – blackheads
Pus-filled spots
Scaring
Affects face, neck, back, shoulders + chest.
Treatment for acne?
Likely need referral to GP, then potentially to dermatology??
Topical retinoids e.g., Roaccutane.
Topical antibiotics.
Combined oral contraceptive pill.
Gel, creams, lotions – benzyl peroxide – acnecide 5% w/w gel
After cleaning + drying skin, apply a thin layer 1-2x a day to affected areas. If sensitive skin, apply 1x a day before bed.
Makes face more sensitive to sun – avoid direct sun + wear spf.
Can have bleaching effect – avoid on hair or clothes.
S/E’s = dry + tense skin, burning, itching or stinging, redness + peeling – mild + usually pass. Usually, 6 weeks of treatment needed to clear skin – then less frequent treatment to prevent recurrence.
Advice for acne?
No scratching/picking/squeezing spots/blackheads.
Use treatment regularly – give it time to work.
Cleanse skin – oil free substitute.
Do not scrub face when washing + pat dry.
Avoid direct sunlight – use sunscreen.
Tretinoin prescription valid for 1 week after doing pregnancy test.
Don’t wash affected area more than twice a day – can irritate skin.
Wash with mild soap/cleanser + lukewarm water.
Completely remove makeup before sleep.
Regular exercise – can help with mood + self-esteem.
Drink plenty of water.
Wash hair regularly.
Avoid oil-based comedogenic skin care, make-up, sunscreens.