HSCI 366 Cardiac Muscle + Cardiovascular System
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
Is cardiac muscle smaller, bigger, or the same size as skeletal muscle?
Smaller
smaller
Does cardiac muscle have higher, lower, or the same mitochondrial density as skeletal muscle?
Higher
Why does cardiac muscle have a high mitochondrial density than skeletal muscle?
Cardiac muscle must contract all the time so it needs a lot of ATP and therefore higher mitochondrial density
Does cardiac muscle have more, less, or the same amount of t-tubules as skeletal muscle?
Less
What are intercalated disks?
Gaps between cardiac muscle cells
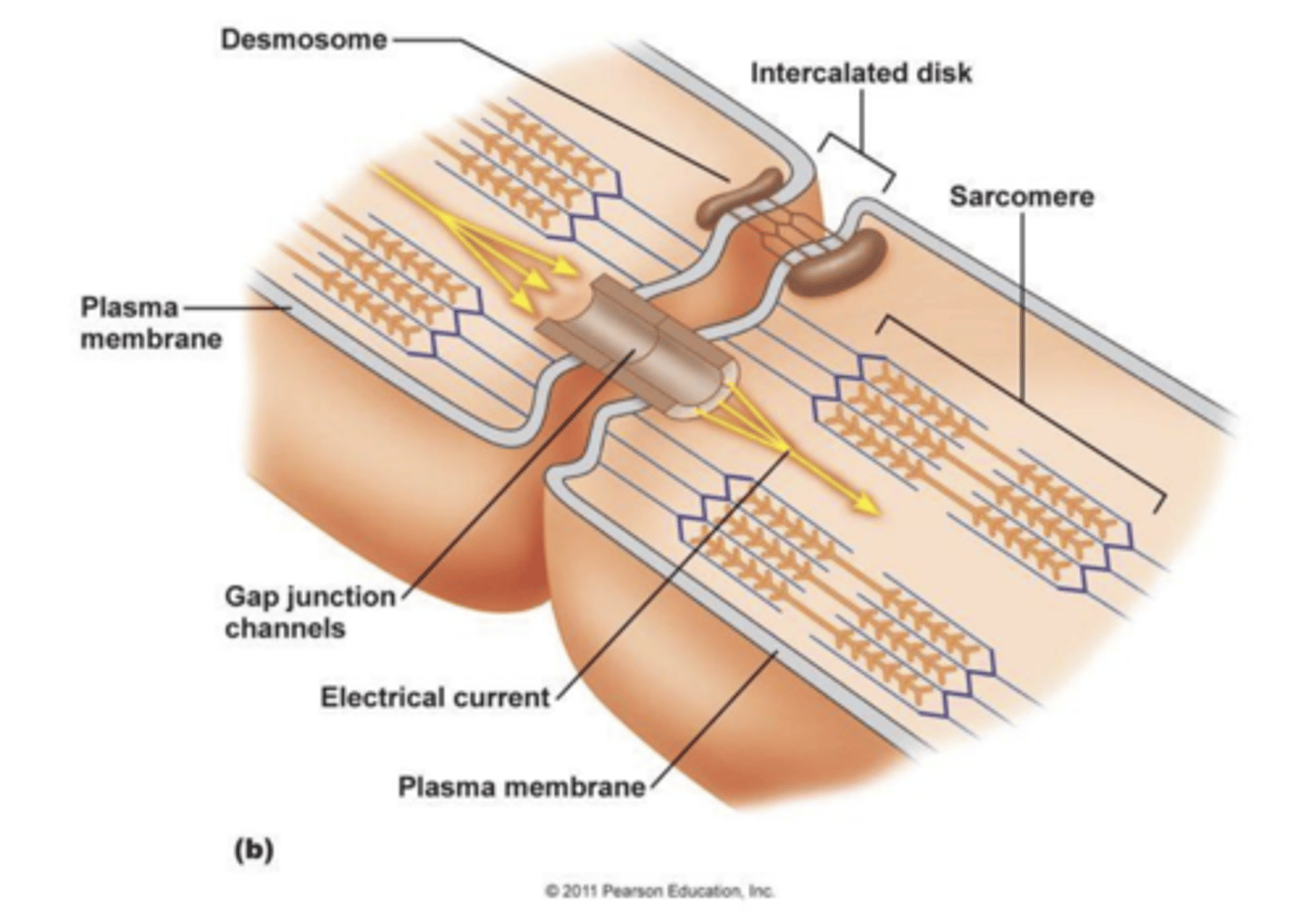
What are desmosomes?
Structure that connects intercalated disks
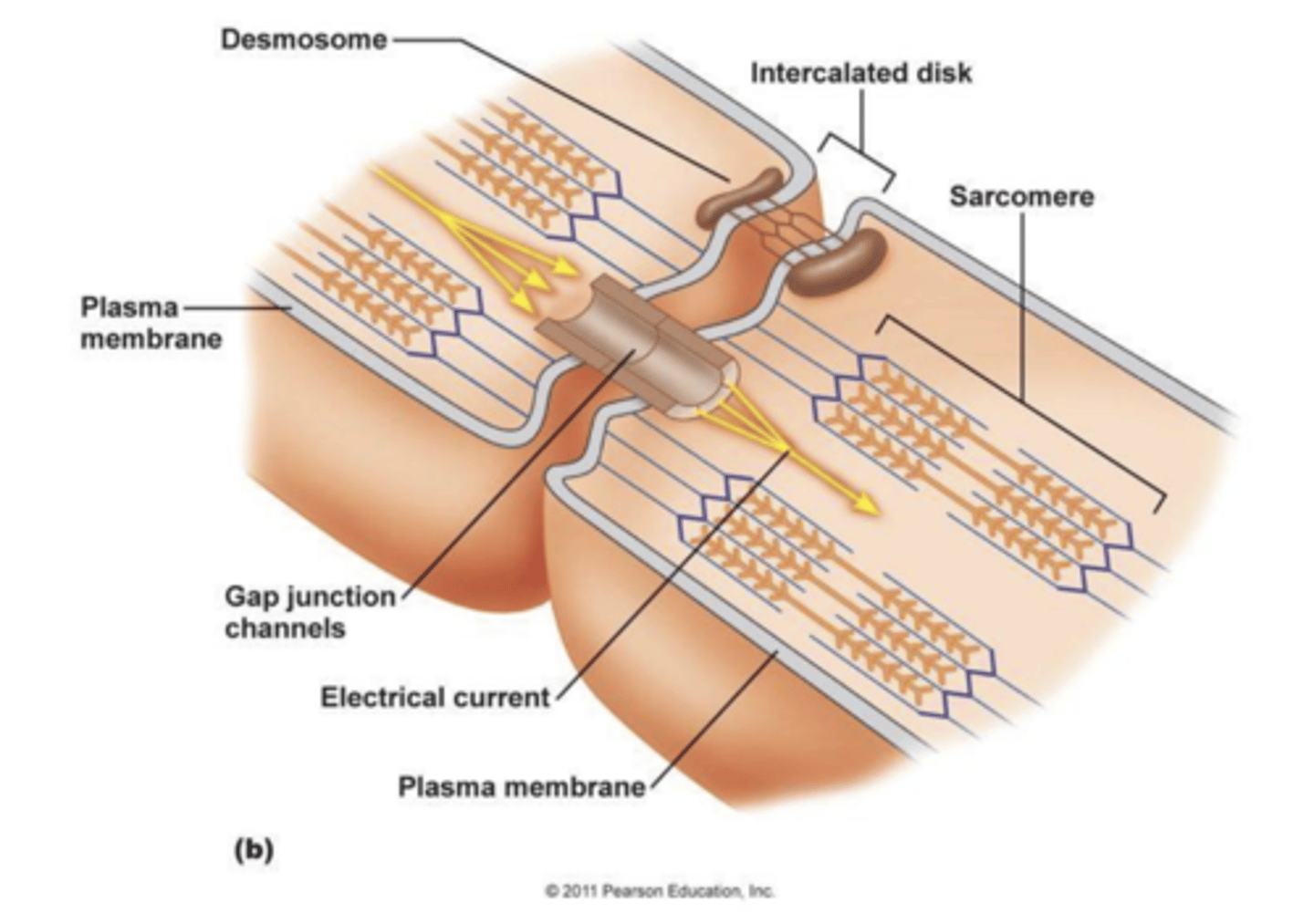
What are gap junctions?
Channels that help share action potentials between muscle cells
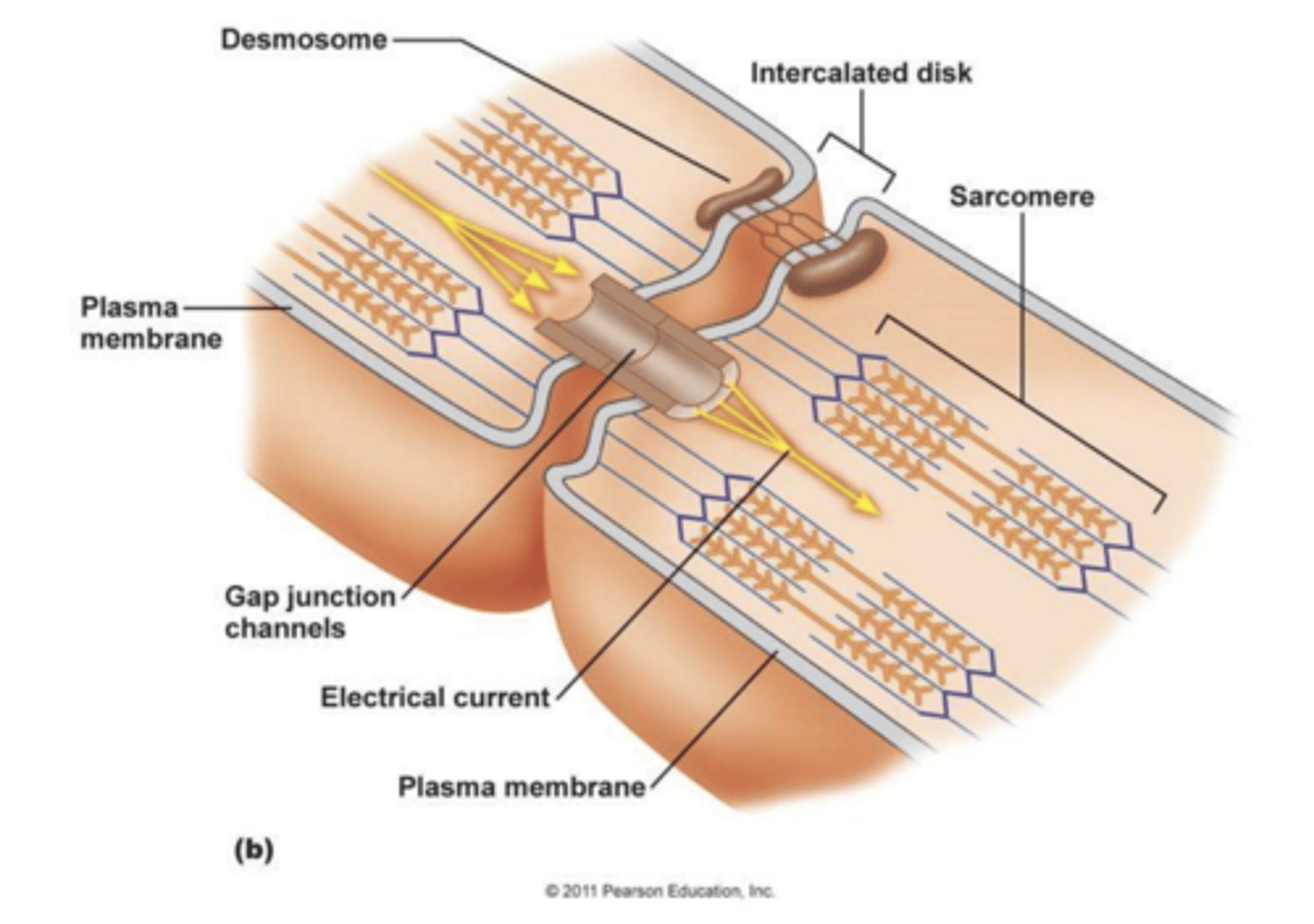
What is the importance of intercalated disks and gap junctions?
They make sure all cells function in sync
How does contraction in the heart occur?
(Same as skeletal muscle) Calcium released from sarcoplasmic reticulum → calcium binds to troponin → troponin moves tropomyosin → tropomyosin moves and exposes myosin → myosin binds to actin → contraction occurs
How is the DHP receptor different in cardiac muscle compared to skeletal muscle?
In cardiac muscle DHP is a voltage gated CHANNEL, in skeletal muscle DHP is a voltage gated SENSOR
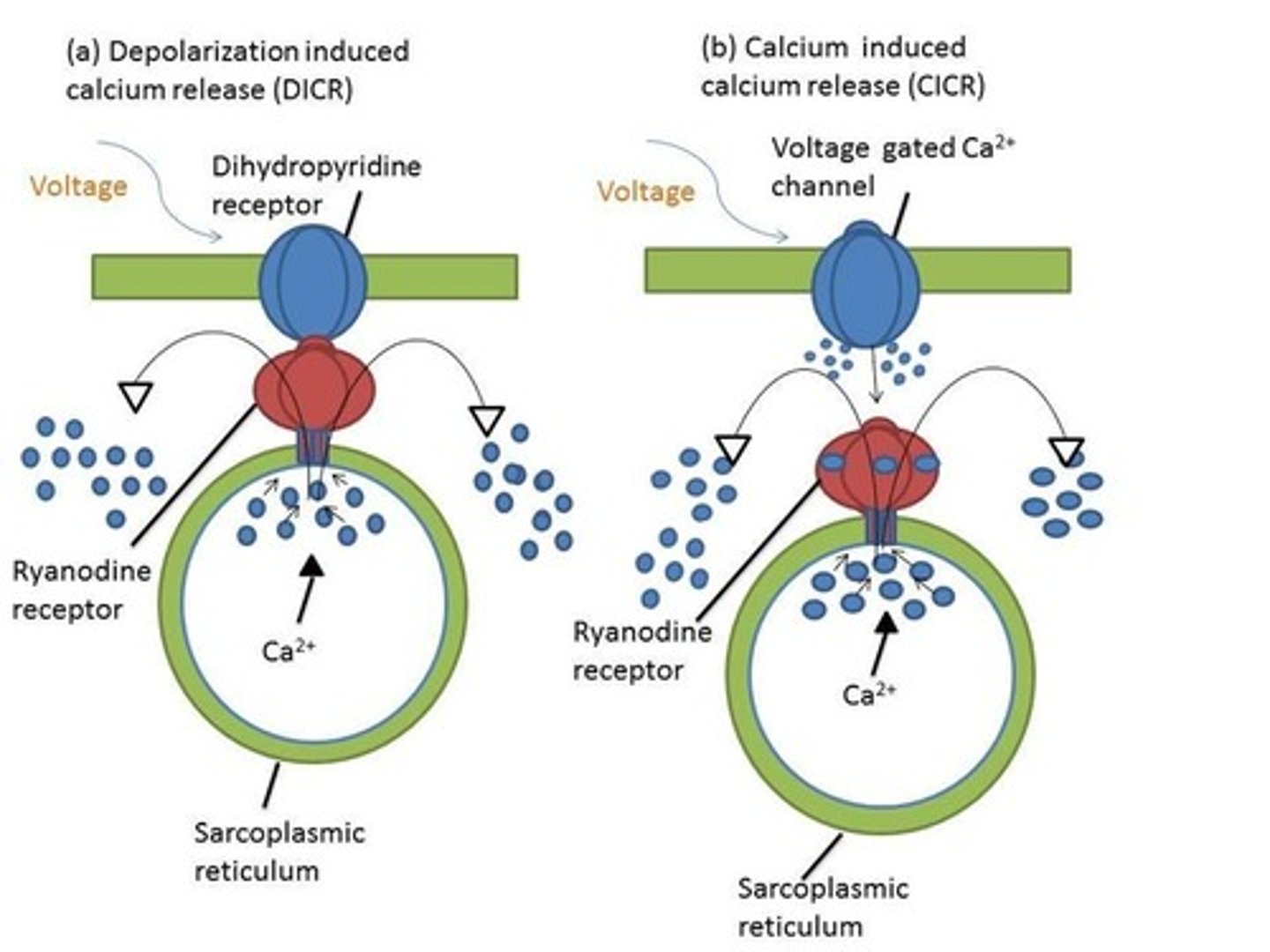
What is calcium induced calcium release (CICR)?
the DHP channel is opened by an action potential → DHP channel lets in calcium → calcium opens the sarcoplasmic reticulum → calcium is released
Why would you want the cardiac muscle to relax?
So that the heart can fill with blood and then contract to pump it out
Why do we pump calcium into the cell?
To trigger calcium release from the sarcoplasmic reticulum, causing contraction
Why do we pump calcium out of the cell?
To get calcium to flow into the sarcoplasmic reticulum, causing muscle relaxation
How do we pump calcium in and out of the cell's cytosol to control contraction?
A Na+ and Ca2+ exchanger can pump and change the concentration in both directions, depending on whether the muscle is contracting or relaxing
What is the flow of de-oxygenated blood?
rest of body → vena cava → right atrium → tricuspid valve → right ventricle → pulmonary valve → lungs
What is the flow of oxygenated blood?
lungs → pulmonary veins → left atrium → bicuspid/mitral valve → left ventricle → aortic valve → aorta → rest of body
What is the wall that separates left and right chambers of the heart?
Septum
What are congenital heart defects?
defect of the heart or great vessels that is present at birth
What is an atrial septal defect?
A hole in the septum between the right and left atria
What is the effect of an atrial septal defect?
oxygenated and de-oxygenated blood will mix, decreasing the efficiency of the heart to pump blood properly
What is a ventricular septal defect?
A hole in the septum between the right and left ventricles
What is the effect of a ventricular septal defect?
oxygenated and de-oxygenated blood will mix, decreasing the efficiency of the heart to pump blood properly
What is transposition of the great vessels?
Aorta and pulmonary artery are switched
What are the effects of transposition of the great vessels?
It causes two closed systems, one with only oxygenated blood and one with only de-oxygenated blood. the affected individual will die
What may prevent death if someone has transposition of the great vessels?
A septal defect may prevent death in someone with transposed great vessels as it will allow blood to be circulated properly, even if it is inefficient
What are the two types of valve defects?
Stenotic and prolapsed
What is a stenotic valve defect?
A valve in the heart does not open all the way
What is a prolapsed valve defect?
A valve in the heart does not close all the way
What happens to the blood flow if someone has a stenotic valve defect?
The valve won't open all the way to let blood through and blood will begin to pool in the chamber it is coming from
(i.e. a stenotic tricuspid valve will cause blood traveling to the right ventricle to pool in the right atrium)
What happens to blood flow if someone has a prolapsed valve defect?
The valve won't close all the way and blood will regurgitate into the chamber it came from (i.e. a prolapsed aortic valve will cause blood traveling to the aorta to regurgitate into the left ventricle)
How does conduction work in the heart?
Sinoatrial node (SA) sends an electrical signal → conduction fibers in the right and left atrium will contract both atria → atria pushes blood down into ventricles → SA signal to the AV junction will delay contraction of the ventricles so they can fill with blood → AV junction will send signal when ventricles are full → purkinje fibers stimulate ventricle contraction → blood is pushed out of ventricles
What is the AV junction and why is it important?
AV junction includes the AV node and Bindle of His; the junction is important as it delays electrical signals to the ventricles, allowing them to stay relaxed and fill with blood before the action potential reaches them, causing them to push blood out via contraction
What valves are open during atrial contraction?
Tricuspid and Bicuspid/Mitral valves
What valves are open during ventricular contraction?
Pulmonary and Aortic Valves
What is Mitral Valve Prolapse (MVP)?
Mitral valve does not close all the way and blood will regurgitate
What happens in the left ventricle during systole?
Atrioventricular valves close → ventricular pressure goes up and isovolumic contraction begins → Aortic valve opens → rapid ejection of blood occurs as ventricle contracts → volume of blood begins to decrease → slow ejection follows rapid ejection → Aortic valve closes
What happens in the left ventricle during diastole?
Aortic valve closes → ventricular pressure goes down as isovolumic relaxation occurs → atrioventricular valves open → blood will flow into ventricle → blood flow into ventricle will increase when atria contract → atrioventricular valves close
What is considered a healthy adult blood pressure?
120/80
What does a high blood pressure indicate?
hypertension, which can cause heart disease
What is the ejection fraction? (EF)
The percentage of oxygen-rich blood being pumped out of the heart
What is stroke volume? (SV)
the volume of blood pumped from the left ventricle per contraction
What is end diastolic volume? (EDV)
The amount of blood in the ventricle before contraction
What is end systolic volume? (ESV)
The amount of blood remaining in a ventricle after contraction
What is the formula for ejection fraction?
EF = SV/EDV * 100
How can stroke volume be elevated?
Either increase EDV or decrease ESV (Your body will do both whenever your heart rate increases)
What happens to the ejection fraction if someone has MVP?
The EF will decrease because the stroke volume (amount of oxygenated blood being pumped out of heart) will go down (EDV may go up)
What is considered a normal ejection fraction?
50%
What is the recommended treatment for people who have stroke volume lower than 50%?
A valve replacement may be recommended
Is atrial contraction necessary to push blood down into the ventricles?
No, the blood will flow into the ventricles anyway because of gravity. However, atrial contraction helps get the most blood out of the atrium and into the ventricle.
What factor may impact blood pressure?
Gender. Women typically have smaller stature and hearts than men, so their hearts do not have to push as much and therefore they tend to have lower blood pressure.
What is the outer most layer of the heart?
epicardium
What is the middle layer of the heart?
myocardium
What is the inner most layer of the heart?
endocardium
Which layer of the heart is the first to depolarize?
endocardium
Which layer of the heart is last to depolarize?
epicardium
Which layer of the heart is the first to repolarize?
epicardium
Which layer of the heart is the last to repolarize?
endocardium
True or False: The wave of action potential in the endocardium and epicardium cancel each other out
True
2 multiple choice options
What are the channels involved in SA node action potential?
Funny (HCN) channel, T-type channel, L-type channel
What happens when the funny channel depolarizes?
It lets Na into the cell and opens the T-type channel
What happens when the T-type channel opens?
Calcium enters the cell, making the cell more positive, and opens the L-type channel
What happens when the L-type channel opens?
More calcium enters, making the cell more positive
What happens after the L-type channel lets in calcium?
The cell becomes depolarized until potassium is slowly released from the cell
How does the cell repolarize after the Funny channel, t-type channel, and l-type channel depolarized it?
The cell begins to hyperpolarize by using Na/K pump, Ca pump, and the Na/K exchanger
How many phases does ventricular action potential have?
5 phases
3 multiple choice options
What happens in the ventricular cells during phase 0?
Sodium rushes in rapidly
What happens in the ventricular cells during phase 2?
Potassium exits the cell and calcium enters to trigger calcium induced calcium release
What happens in the ventricular cells during phase 3?
Potassium exits the cell rapidly
What happens in the ventricular cells during phase 4?
Concentration gradients re-establish to prepare for another action potential
What is the importance of calcium induced calcium released in cardiac muscle specifically?
Allows cardiac muscle to come to rest which is how it is able to pump blood
What is the Frank-Starling law of the heart?
Basically, the more blood returned to the heart (the more EDV), the more blood will be ejected with each beat, this is based on the relationship of the stretch of the sarcomeres and the ability of actin and myosin to form cross-bridges.
What happens to the heart during sympathetic activation at a physiological level?
Epinephrine and norepinephrine bind to B1 receptor → B1 receptor triggers G-protein → G-protein stimulates Adenylyl ayclase →Adenylyl cyclase turns ATP into cAMP → cAMP opens calcium channels into the SA node and ventricles → Calcium induced calcium release occurs → Heart rate goes up due to increased calcium levels
What happens to the heart during parasympathetic activation at a physiological level?
Acetylcholine binds to muscarinic receptors → potassium leaks out of the cell and Adenylyl cyclase turns off → ATP is no longer turned into cAMP → calcium channels are not opened → cell is too far from threshold to send action potentials → slower heart rate
In patients with high blood pressure, is it better to first prescribe a Beta blocker or a vasodilator?
Presribe a beta blocker (i.e. better to turn down the flow intensity than change the entire hose)
What chamber of the heart is responsible for heart rate?
Left ventricle
What is an ideal blood pressure?
120/80
Is 120 systolic or diastolic?
Systolic
Is 80 systolic or diastolic?
Diastolic